Clinical and Imaging Characteristics in Patients with SARS-CoV-2 Infection and Acute Intracranial Hemorrhage
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Image Acquisitions
2.3. Image Analysis
2.4. Statistics
3. Results
3.1. Demographic and Clinical Characteristics
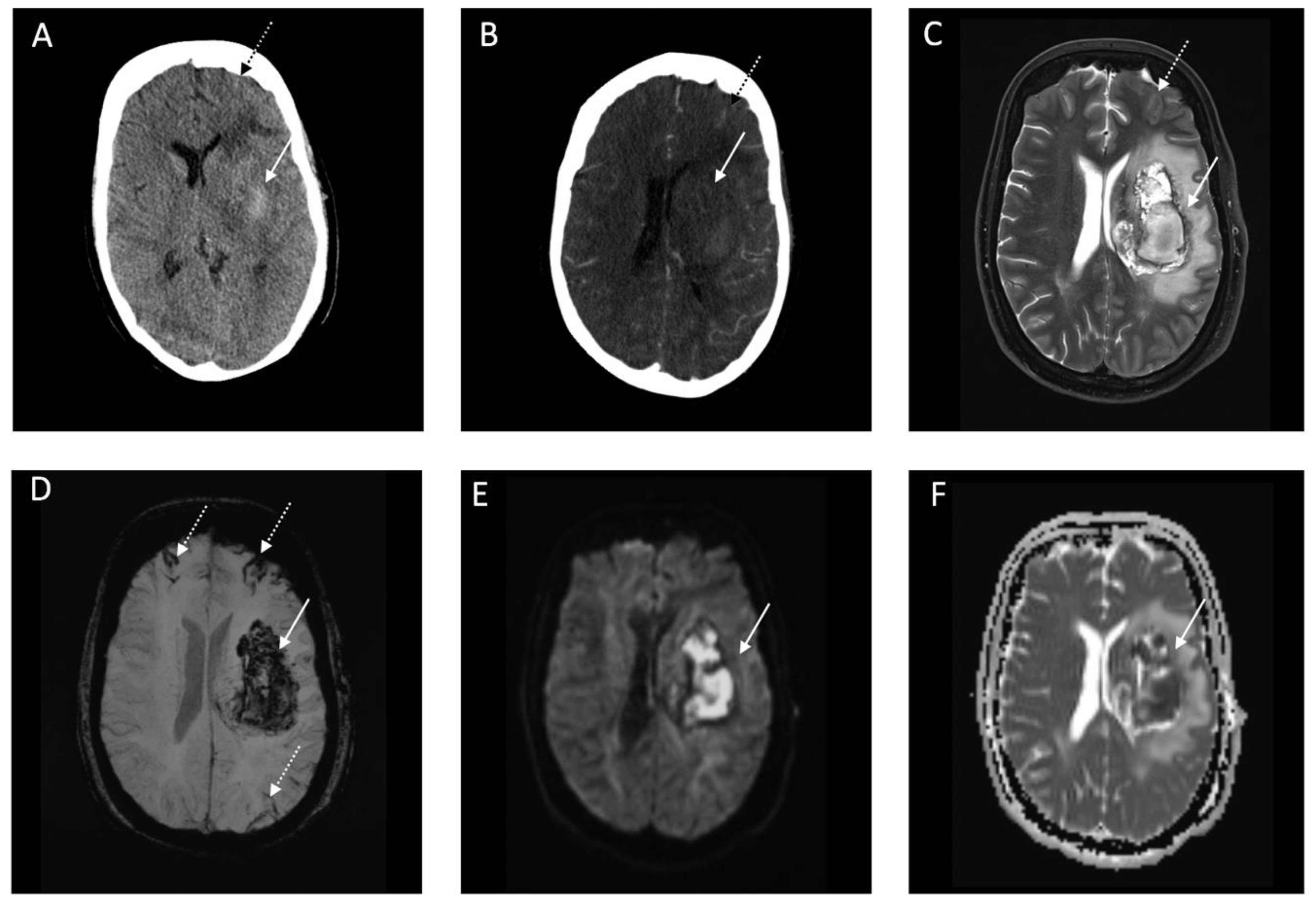
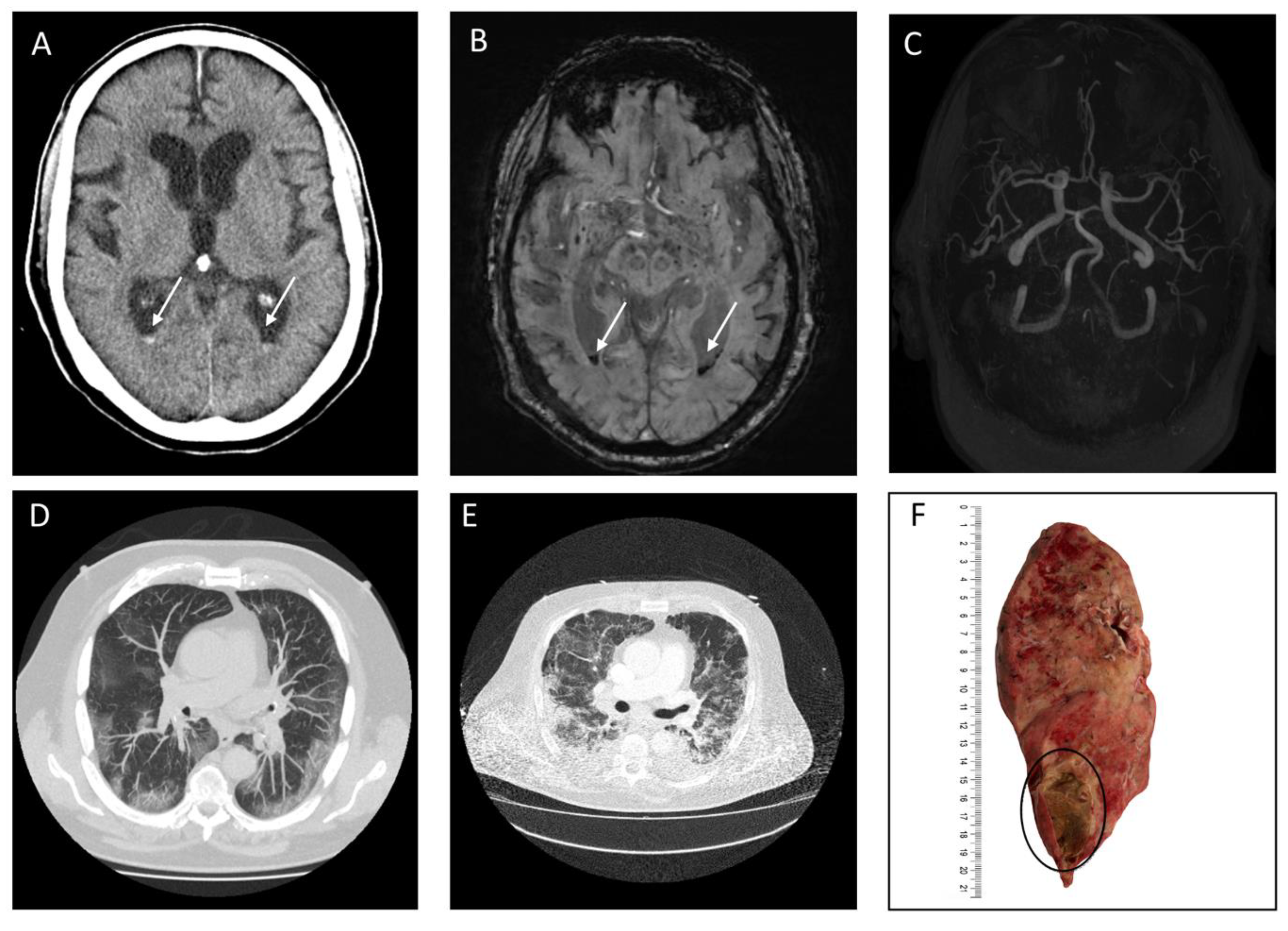
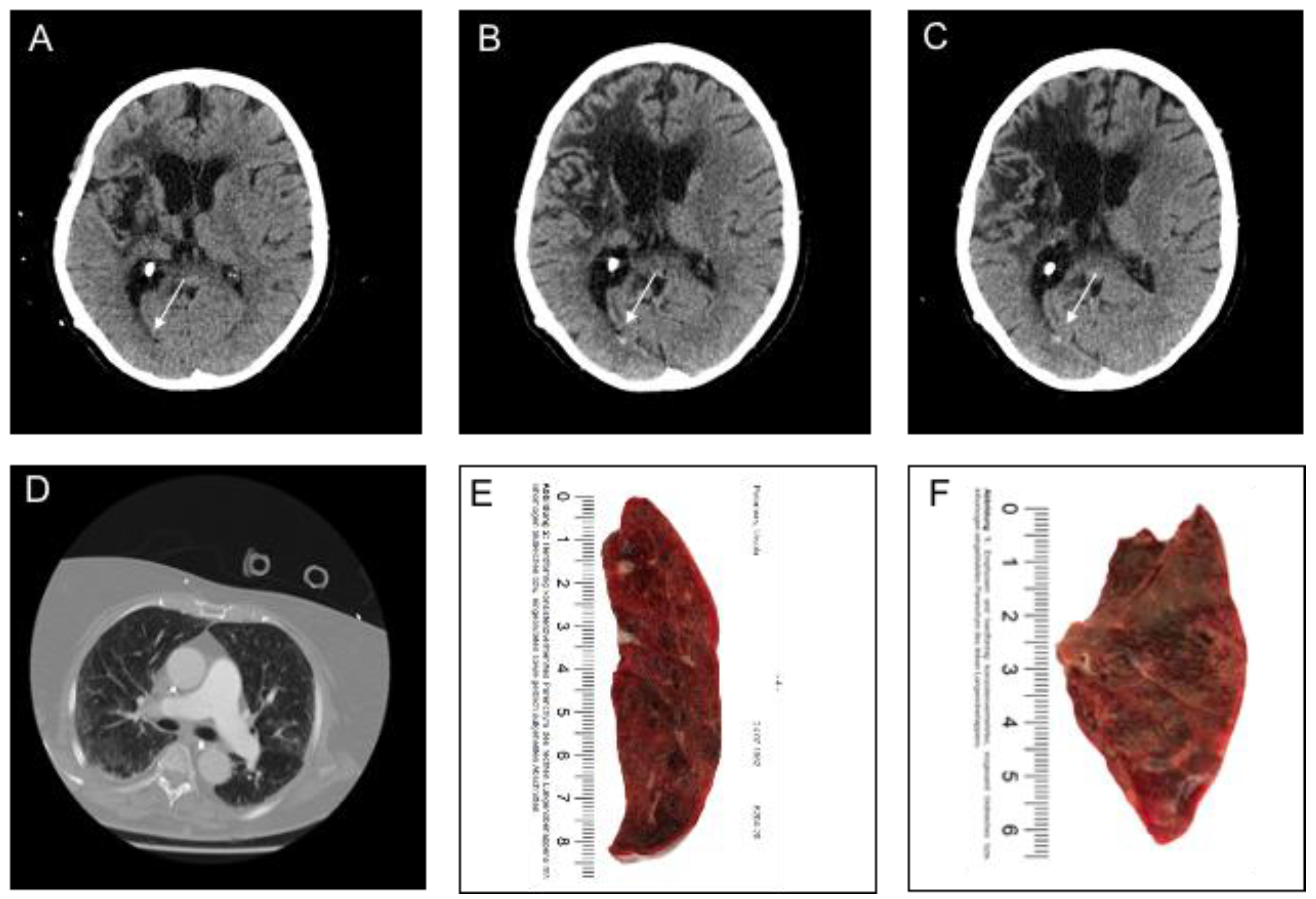
3.2. Imaging and Clinical Findings
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 1 June 2020).
- Fu, L.; Wang, B.; Yuan, T.; Chen, X.; Ao, Y.; Fitzpatrick, T.; Li, P.; Zhou, Y.; Lin, Y.F.; Duan, Q.; et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis. J. Infect. 2020, 80, 656–665. [Google Scholar] [CrossRef] [PubMed]
- Mao, L.; Jin, H.; Wang, M.; Hu, Y.; Chen, S.; He, Q.; Chang, J.; Hong, C.; Zhou, Y.; Wang, D.; et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020, 77, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Pinna, P.; Grewal, P.; Hall, J.P.; Tavarez, T.; Dafer, R.M.; Garg, R.; Osteraas, N.D.; Pellack, D.R.; Asthana, A.; Fegan, K.; et al. Neurological manifestations and COVID-19: Experiences from a tertiary care center at the Frontline. J. Neurol. Sci. 2020, 415, 116969. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Favaloro, E.J. D-dimer is associated with severity of coronavirus disease 2019: A pooled analysis. Thromb. Haemost. 2020, 120, 876–878. [Google Scholar] [CrossRef]
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S.; Mehra, M.R.; Schuepbach, R.A.; Ruschitzka, F.; Moch, H. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- Mahammedi, A.; Saba, L.; Vagal, A.; Leali, M.; Rossi, A.; Gaskill, M.; Sengupta, S.; Zhang, B.; Carriero, A.; Bachir, S.; et al. Imaging in neurological disease of hospitalized COVID-19 patients: An Italian multicenter retrospective observational study. Radiology 2020, 201933. [Google Scholar] [CrossRef]
- Kerleroux, B.; Fabacher, T.; Bricout, N.; Moïse, M.; Testud, B.; Vingadassalom, S.; Ifergan, H.; Janot, K.; Consoli, A.; Ben Hassen, W.; et al. Mechanical thrombectomy for acute ischemic stroke amid the COVID-19 outbreak. Stroke 2020, 51, 2012–2017. [Google Scholar] [CrossRef]
- Merkler, A.E.; Parikh, N.S.; Mir, S.; Gupta, A.; Kamel, H.; Lin, E.; Lantos, J.; Schenck, E.J.; Goyal, P.; Bruce, S.S.; et al. Risk of ischemic stroke in patients with COVID-19 versus patients with influenza. JAMA Neurol. 2020. [Google Scholar] [CrossRef]
- Novel Coronavirus Pneumonia Diagnosis and Treatment Plan (Provisional 7th Edition). Available online: https://www.chinalawtranslate.com/coronavirus-treatment-plan-7/ (accessed on 7 July 2020).
- Broderick, J.P.; Adeoye, O.; Elm, J. Evolution of the modified rankin scale and its use in future stroke trials. Stroke 2017, 48, 2007–2012. [Google Scholar] [CrossRef]
- Zulfiqar, A.-A.; Lorenzo-Villalba, N.; Hassler, P.; Andrès, E. Immune thrombocytopenic purpura in a patient with COVID-19. N. Engl. J. Med. 2020, 382, e43. [Google Scholar] [CrossRef]
- Akute Zerebrovaskuläre Ereignisse Bei COVID-19. Available online: https://www.dgn.org/rubrik-themen/3961-akute-zerebrovaskulaere-ereignisse-bei-covid-20 (accessed on 5 May 2020).
- Cuvinciuc, V.; Viguier, A.; Calviere, L.; Raposo, N.; Larrue, V.; Cognard, C.; Bonneville, F. Isolated acute nontraumatic cortical subarachnoid hemorrhage. Am. J. Neuroradiol. 2010, 31, 1355–1362. [Google Scholar] [CrossRef] [PubMed]
- Princiotta Cariddi, L.; Tabaee Damavandi, P.; Carimati, F.; Banfi, P.; Clemenzi, A.; Marelli, M.; Giorgianni, A.; Vinacci, G.; Mauri, M.; Versino, M. Reversible encephalopathy syndrome (PRES) in a COVID-19 patient. J. Neurol. 2020, 1, 3. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, A.M.; Ahmed, O.; Giliberto, L.; Castillo, M. Hemorrhagic posterior reversible encephalopathy syndrome as a manifestation of COVID-19 infection. Am. J. Neuroradiol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Forman, R.; Harris, J.; Lee, V.; Garg, R.; John, S.; Conners, J. Reversible cerebral vasoconstriction syndrome presenting as convexity subarachnoid hemorrhage (P2.286). Neurology 2017, 88, 286. [Google Scholar]
- Barboza, M.A.; Maud, A.; Rodriguez, G.J. Reversible Cerebral Vasoconstriction Syndrome and Nonaneurysmal Subarachnoid Hemorrhage. J. Vasc. Int. Neurol. 2014, 7, 17–20. [Google Scholar]
- Peeyush Kumar, T.; McBride, D.W.; Dash, P.K.; Matsumura, K.; Rubi, A.; Blackburn, S.L. Endothelial cell dysfunction and injury in subarachnoid hemorrhage. Mol. Neurobiol. 2019, 56, 1992–2006. [Google Scholar] [CrossRef] [PubMed]
- Bonetti, P.O.; Lerman, L.O.; Lerman, A. Endothelial dysfunction: A marker of atherosclerotic risk. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 168–175. [Google Scholar] [CrossRef]
- Fogarty, H.; Townsend, L.; Cheallaigh, C.N.; Bergin, C.; Martin-Loeches, I.; Browne, P.; Bacon, C.L.; Gaule, R.; Gillett, A.; Byrne, M.; et al. COVID-19 coagulopathy in caucasian patients. Br. J. Haematol. 2020. [Google Scholar] [CrossRef]
- Jones, V.G.; Mills, M.; Suarez, D.; Hogan, C.A.; Yeh, D.; Segal, J.B.; Nguyen, E.L.; Barsh, G.R.; Maskatia, S.; Mathew, R. COVID-19 and kawasaki disease: Novel virus and novel case. Hosp. Pediatrics 2020. [Google Scholar] [CrossRef]
- Verdoni, L.; Mazza, A.; Gervasoni, A.; Martelli, L.; Ruggeri, M.; Ciuffreda, M.; Bonanomi, E.; D’Antiga, L. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: An observational cohort study. Lancet 2020, 395, 1771–1778. [Google Scholar] [CrossRef]
- Sharlala, H.; Adebajo, A. Virus-induced vasculitis. Curr. Rheumatol. Rep. 2008, 10, 449–452. [Google Scholar] [CrossRef]
- Salvarani, C.; Brown, R.D.; Calamia, K.T.; Christianson, T.J.H.; Huston, J.; Meschia, J.F.; Giannini, C.; Miller, D.V.; Hunder, G.G. Primary central nervous system vasculitis presenting with intracranial hemorrhage. Arthritis Rheum. 2011, 63, 3598–3606. [Google Scholar] [CrossRef] [PubMed]
- Boulouis, G.; De Boysson, H.; Zuber, M.; Guillevin, L.; Meary, E.; Costalat, V.; Pagnoux, C.; Naggara, O. Primary angiitis of the central nervous system: Magnetic resonance imaging spectrum of parenchymal, meningeal, and vascular lesions at baseline. Stroke 2017, 48, 1248–1255. [Google Scholar] [CrossRef] [PubMed]
- Younger, D.S.; Coyle, P.K. Central nervous system vasculitis due to infection. Neurol. Clin. 2019, 37, 441–463. [Google Scholar] [CrossRef] [PubMed]
- Jain, R.; Deveikis, J.; Hickenbottom, S.; Mukherji, S.K. Varicella-zoster vasculitis presenting with intracranial hemorrhage. Am. J. Neuroradiol. 2003, 24, 971–974. [Google Scholar] [PubMed]
- Salvarani, C.; Brown, R.D.; Hunder, G.G. Adult primary central nervous system vasculitis. Curr. Opin. Rheumatol. 2012, 24, 46–52. [Google Scholar] [CrossRef]
- Greenan, T.J.; Grossman, R.I.; Goldberg, H.I. Cerebral vasculitis: MR imaging and angiographic correlation. Radiology 1992, 182, 65–72. [Google Scholar] [CrossRef]
- Marsh, E.B.; Zeiler, S.R.; Levy, M.; Llinas, R.H.; Urrutia, V.C. Diagnosing CNS vasculitis. Neurologist 2012, 18, 233–238. [Google Scholar] [CrossRef]
- Hamming, I.; Timens, W.; Bulthuis, M.L.C.; Lely, A.T.; Navis, G.J.; van Goor, H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. 2004, 203, 631–637. [Google Scholar] [CrossRef]
- Sharma, R.; Dearaugo, S.; Infeld, B.; O’Sullivan, R.; Gerraty, R.P. Cerebral amyloid angiopathy: Review of clinico-radiological features and mimics. J. Med. Imaging Radiat. Oncol. 2018, 62, 451–463. [Google Scholar] [CrossRef]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.C.; et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Oudit, G.Y.; Kassiri, Z.; Jiang, C.; Liu, P.P.; Poutanen, S.M.; Penninger, J.M.; Butany, J. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur. J. Clin. Investig. 2009, 39, 618–625. [Google Scholar] [CrossRef] [PubMed]
- Cavayas, Y.A.; del Sorbo, L.; Fan, E. Intracranial hemorrhage in adults on ECMO. Perfusion 2018, 33, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Fanou, E.M.; Coutinho, J.M.; Shannon, P.; Kiehl, T.R.; Levi, M.M.; Wilcox, M.E.; Aviv, R.I.; Mandell, D.M. Critical illness-associated cerebral microbleeds. Stroke 2017, 48, 1085–1087. [Google Scholar] [CrossRef] [PubMed]
- Mavragani, A. Tracking COVID-19 in Europe: Infodemiology approach. JMIR Public Health Surveill. 2020, 6, e18941. [Google Scholar] [CrossRef]
- Jin, H.; Hong, C.; Chen, S.; Zhou, Y.; Wang, Y.; Mao, L.; Li, Y.; He, Q.; Li, M.; Su, Y.; et al. Consensus for prevention and management of coronavirus disease 2019 (COVID-19) for neurologists. Stroke Vasc. Neurol. 2020. [Google Scholar] [CrossRef]
- Hemphill, J.C.; Greenberg, S.M.; Anderson, C.S.; Becker, K.; Bendok, B.R.; Cushman, M.; Fung, G.L.; Goldstein, J.N.; MacDonald, R.L.; Mitchell, P.H.; et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals from the American Heart Association. Stroke 2015, 46, 2032–2060. [Google Scholar] [CrossRef]
- Sweidan, A.J.; Singh, N.K.; Conovaloff, J.L.; Bower, M.; Groysman, L.I.; Shafie, M.; Yu, W. Coagulopathy reversal in intracerebral haemorrhage. Stroke Vasc. Neurol. 2020, 5, 29–33. [Google Scholar] [CrossRef]
- Ropper, A.H.; King, R.B. Intracranial pressure monitoring in comatose patients with cerebral hemorrhage. Arch. Neurol. 1984, 41, 725–728. [Google Scholar] [CrossRef]


| Baseline Characteristics | COVID-19 Patients with Acute Intracranial Hemorrhage (n = 18) |
|---|---|
| Clinical Parameters | |
| Age (years), median (IQR) | 49.50 (39.25–62.75) |
| Female, n (%) | 9 (50.0) |
| Hypertension, n (%) | 10 (55.6) |
| Diabetes mellitus, n (%) | 4 (22.2) |
| Comorbidities | |
| • cardiovascular, n (%) | 6 (33.3) |
| • neurovascular, n (%) | 1 (5.6) |
| • oncological, n (%) | 4 (22.2) |
| GCS score, median (IQR) | 9 (3–7) |
| Anticoagulation Treatment, n (%) | 8 (44.4) |
| Antiplatelet Treatment, n (%) | 1 (5.6) |
| Time difference between symptom onset to imaging, (days), median (IQR) | 1.5 (0–3) |
| Time difference between admission to imaging, (days), median (IQR) | 11 (9–29.4) |
| Laboratory Parameters | |
| Lactate dehydrogenase, median (U/L), median (IQR) | 483.50 (278–738.5) |
| Creatinine (mg/dL), median (IQR) | 2.06 (1.45–2.81) |
| C-reactive protein (mg/L), median (IQR) | 239.8 (145–377.14) |
| Platelet (103/µL), median (IQR) | 218.0 (108.5–445.25) |
| White blood cells [×109/L], median (IQR) | 8.5 (2.9–28.2) |
| D-dimer (µg/L), median (IQR) | 8.8 (7.0–11.5) |
| COVID-19 Symptoms | |
| Neurological symptoms first, n (%) | 2 (11.1) |
| Respiratory symptoms first, n (%) | 16 (88.9) |
| COVID-19 Classification | |
| Mild lung infection, n (%) | 1 (5.6) |
| Regular lung infection, n (%) | 1 (5.6) |
| Severe lung infection, n (%) | 1 (5.6) |
| Critical lung infection, n (%) | 15 (83.3) |
| Procedure Process and Results | |
| Craniectomy, n (%) | 1 (5.6) |
| EVD, n (%) | 1 (5.6) |
| ECMO, n (%) | 8 (44.4) |
| Ventilation, n (%) | 13 (72.2) |
| Sepsis, n (%) | 8 (44.4) |
| mRS, n (%) | |
| • 0–3 | 0 (0) |
| • 4–6 | 18 (100) |
| Parenchymal Hemorrhage (n = 6) | |
| Location | |
| • Lobar, n (%) | 4 (66.7) |
| • Deep, n (%) | 1 (16.7) |
| • Infratentorial, n (%) | 1 (16.7) |
| Ventricular extension, n (%) | 1 (16.7) |
| SAH extension, n (%) | 1 (0) |
| Subarachnoid Hemorrhage (n = 11) | |
| Primary SAH, n (%) | 9 (81.8) |
| • Aneurysmal, n (%) | - |
| • Cortical, n (%) | 9 (81.8) |
| • Bilateral, n (%) | 4 (36.4) |
| • Ventricular extension, n (%) | - |
| Secondary SAH, n (%) | 2 (18.2) |
| Intraventricular Hemorrhage (n = 3) | |
| Isolated IVH | |
| • Supratentorial, n (%) | 3 (100) |
| • Infratentorial, n (%) | - |
| • SAH extension, n (%) | - |
| Secondary IVH *1, n (%) | 1 (33.3) |
| Subdural Hemorrhage (n = 1) | |
| Convexity, n (%) | 1 (100) |
| Bilateral, n (%) | - |
| SAH extension, n (%) | 1 (100) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nawabi, J.; Morotti, A.; Wildgruber, M.; Boulouis, G.; Kraehling, H.; Schlunk, F.; Can, E.; Kniep, H.; Thomalla, G.; Psychogios, M.; et al. Clinical and Imaging Characteristics in Patients with SARS-CoV-2 Infection and Acute Intracranial Hemorrhage. J. Clin. Med. 2020, 9, 2543. https://doi.org/10.3390/jcm9082543
Nawabi J, Morotti A, Wildgruber M, Boulouis G, Kraehling H, Schlunk F, Can E, Kniep H, Thomalla G, Psychogios M, et al. Clinical and Imaging Characteristics in Patients with SARS-CoV-2 Infection and Acute Intracranial Hemorrhage. Journal of Clinical Medicine. 2020; 9(8):2543. https://doi.org/10.3390/jcm9082543
Chicago/Turabian StyleNawabi, Jawed, Andrea Morotti, Moritz Wildgruber, Gregoire Boulouis, Hermann Kraehling, Frieder Schlunk, Elif Can, Helge Kniep, Götz Thomalla, Marios Psychogios, and et al. 2020. "Clinical and Imaging Characteristics in Patients with SARS-CoV-2 Infection and Acute Intracranial Hemorrhage" Journal of Clinical Medicine 9, no. 8: 2543. https://doi.org/10.3390/jcm9082543
APA StyleNawabi, J., Morotti, A., Wildgruber, M., Boulouis, G., Kraehling, H., Schlunk, F., Can, E., Kniep, H., Thomalla, G., Psychogios, M., Hamm, B., Fiehler, J., Hanning, U., & Sporns, P. (2020). Clinical and Imaging Characteristics in Patients with SARS-CoV-2 Infection and Acute Intracranial Hemorrhage. Journal of Clinical Medicine, 9(8), 2543. https://doi.org/10.3390/jcm9082543







