Reduced Recovery Capacity After Major Trauma in the Elderly: Results of a Prospective Multicenter Registry-Based Cohort Study
Abstract
1. Introduction
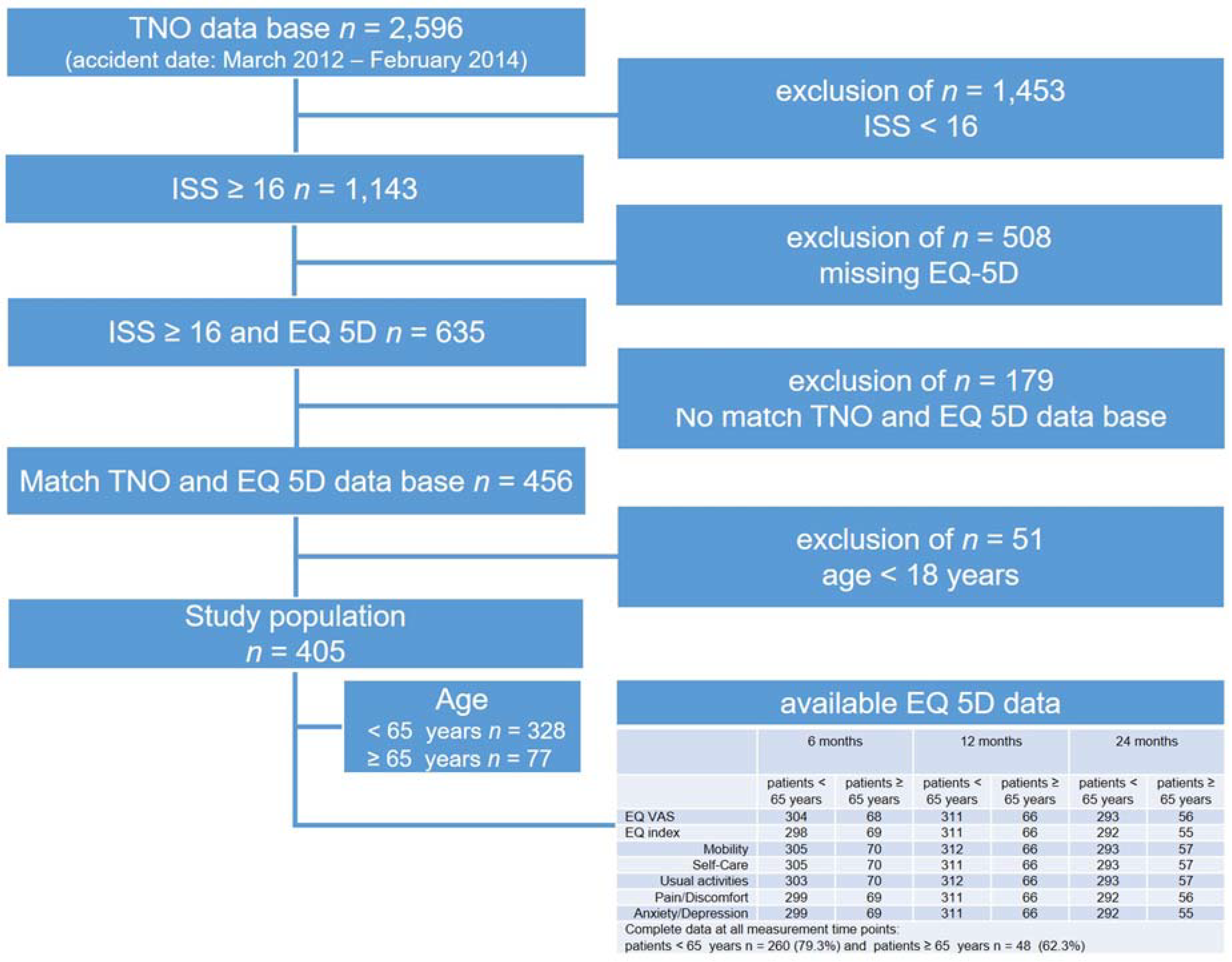
2. Methods
3. Statistics
4. Results
4.1. Baseline Characteristics
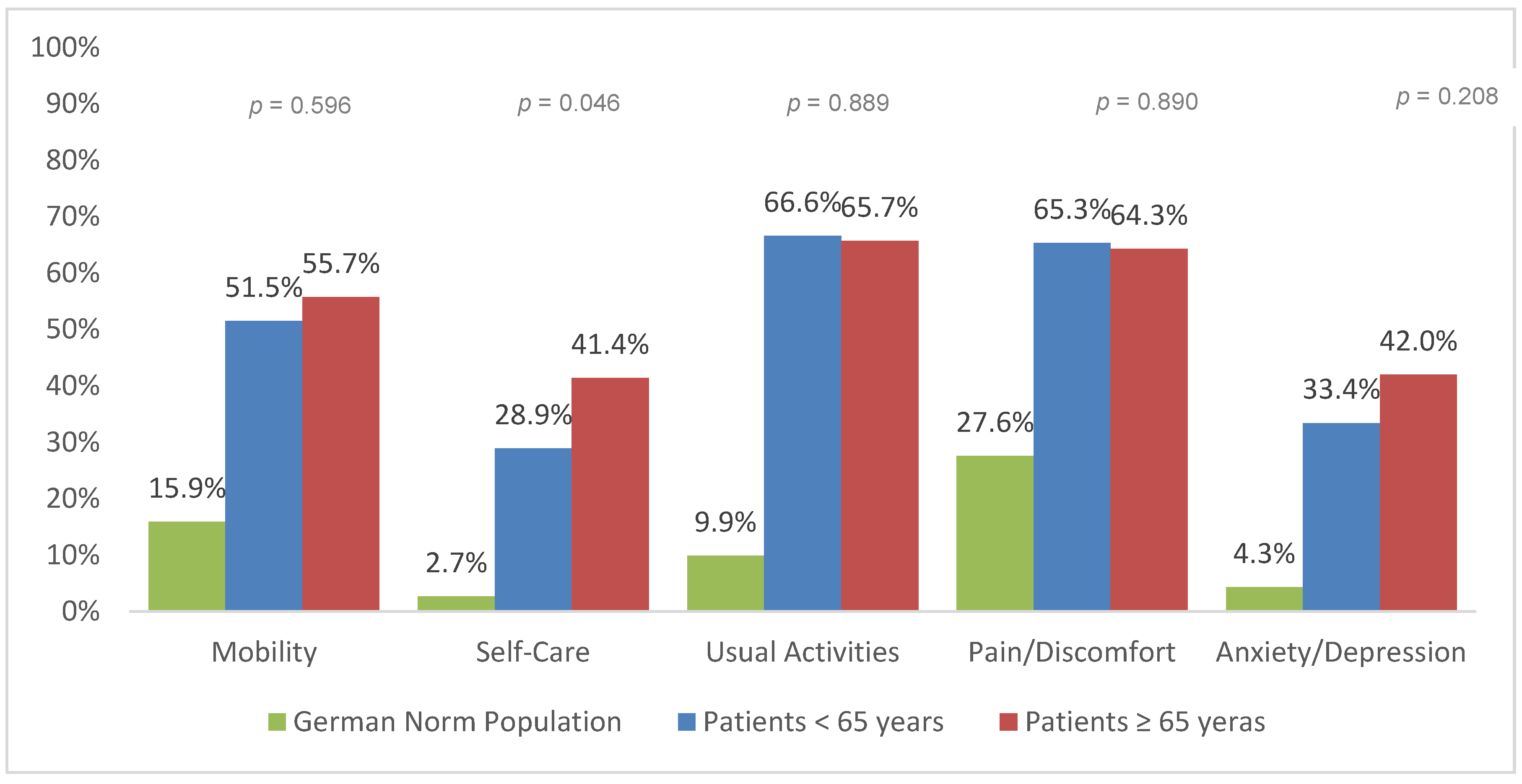
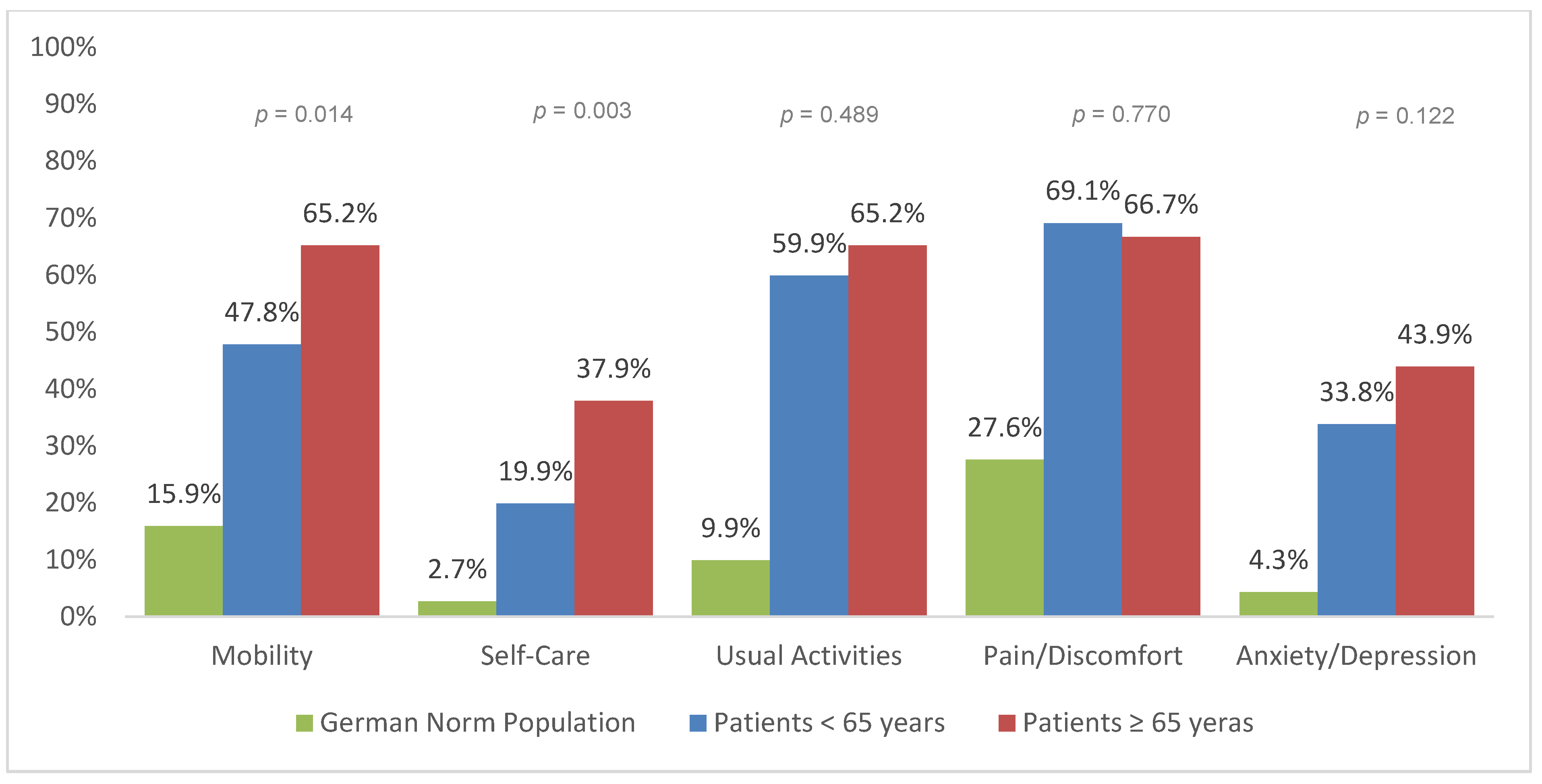
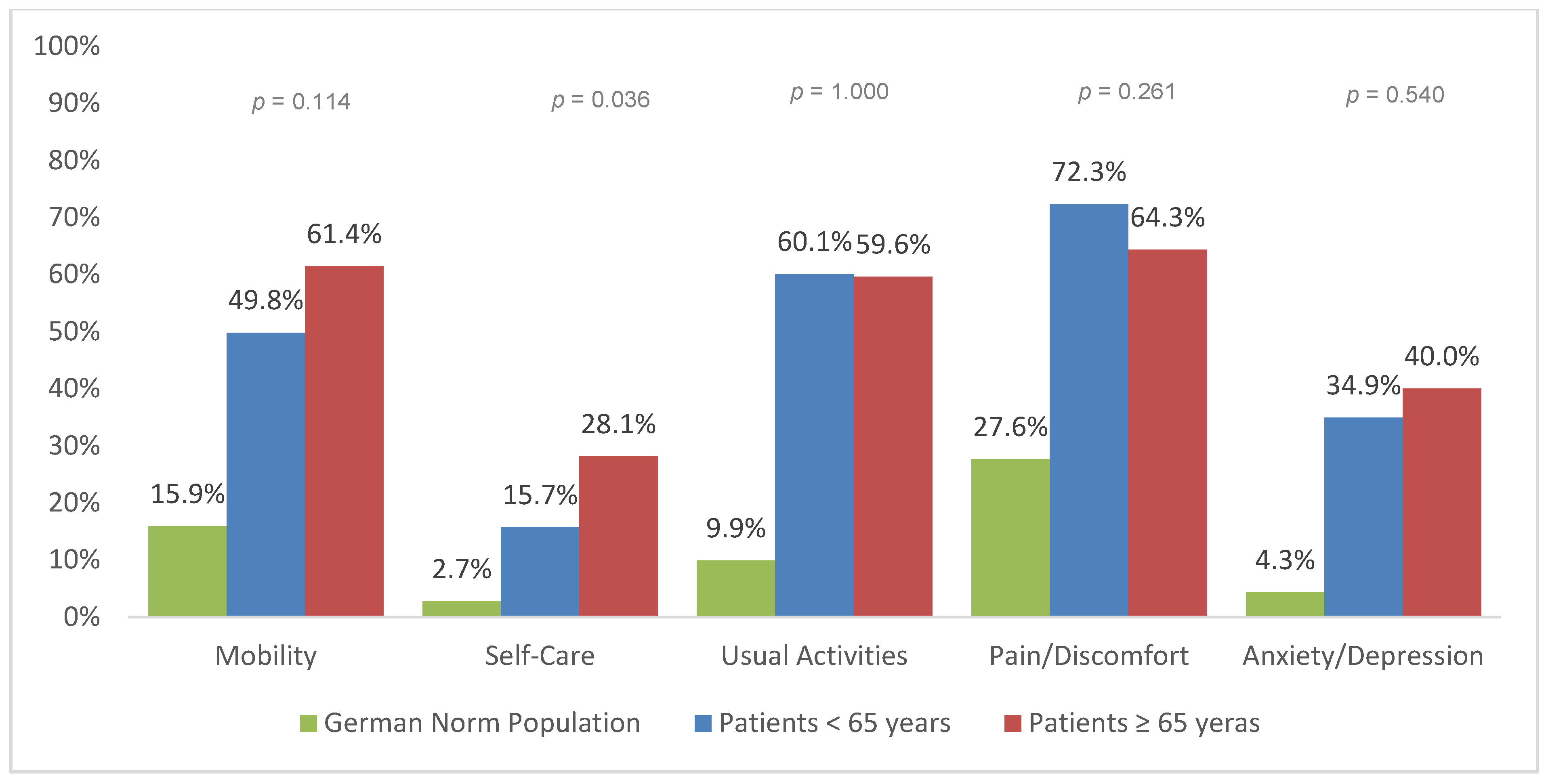
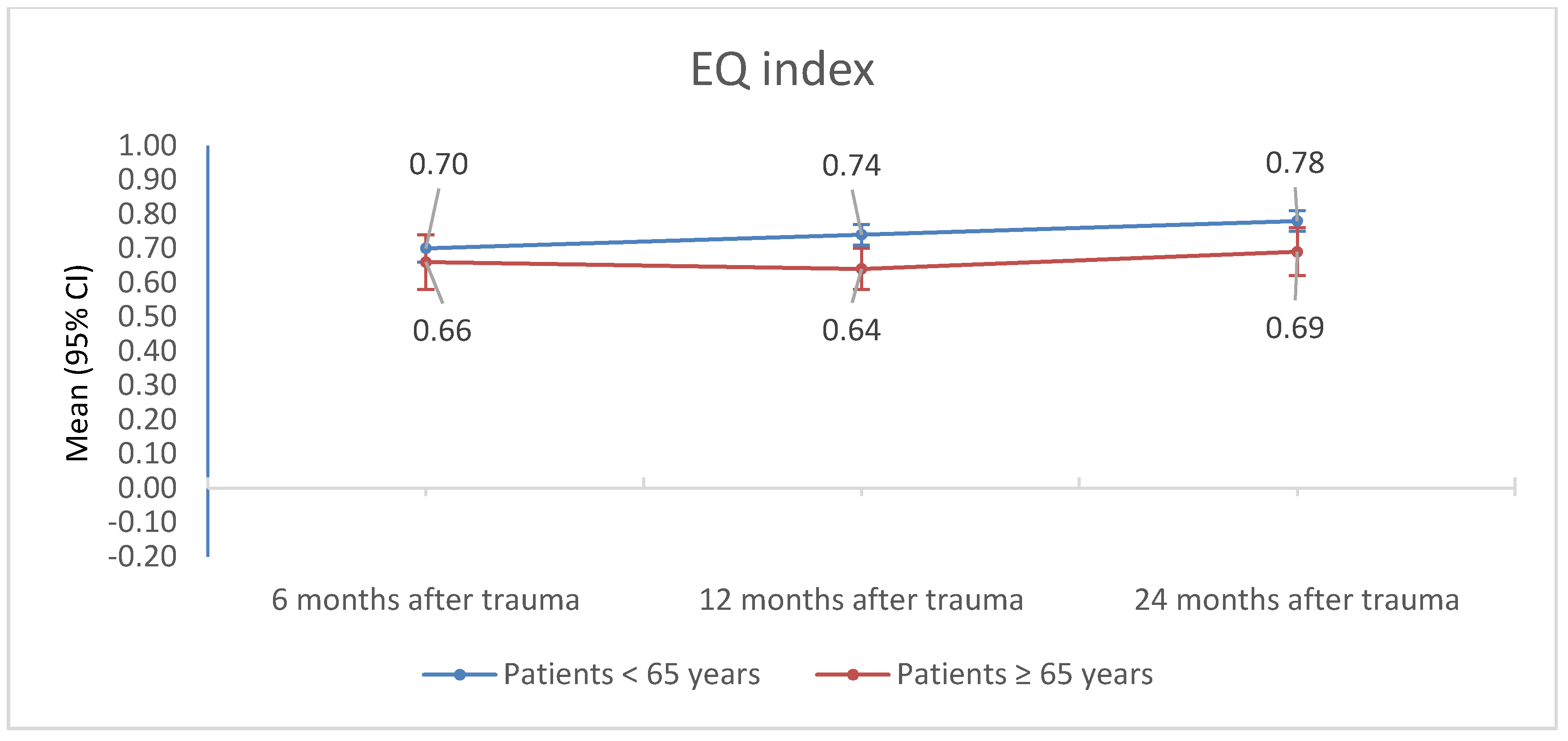
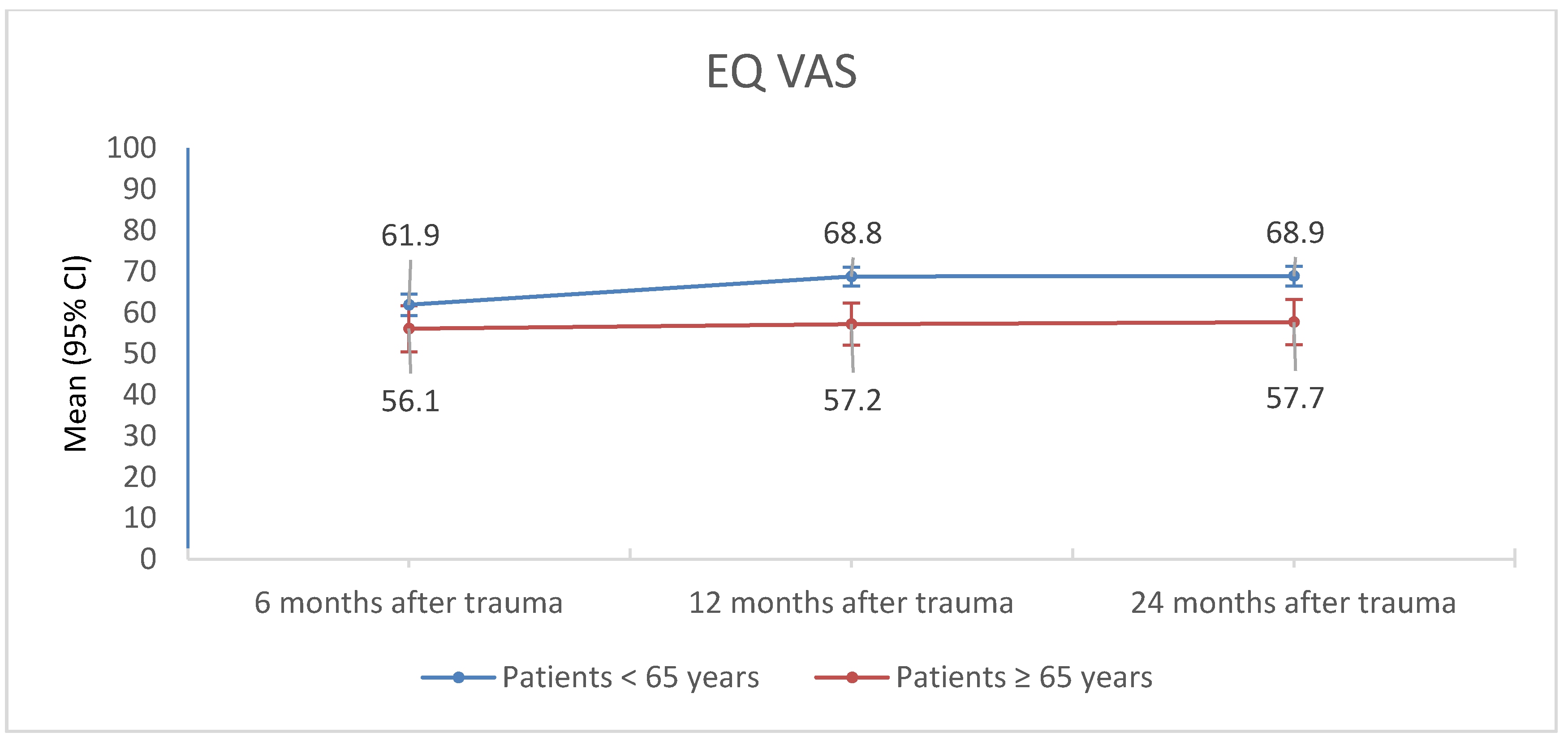
4.2. Quality of Life
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Statistisches Bundesamt (Destatis). Bevölkerung im Wandel Annahmen und Ergebnisse der 14. koordinierten Bevölkerungsvorausberechnung. 2019. Available online: https://www.destatis.de/DE/Presse/Pressekonferenzen/2019/Bevoelkerung/pressebroschuere-bevoelkerung.pdf?__blob=publicationFile (accessed on 1 February 2020).
- Gather, A.; Grützner, P.A.; Münzberg, M. Polytrauma in old Age-Knowledge from the TraumaRegister DGU®. Chirurg 2019, 90, 791–794. [Google Scholar] [CrossRef]
- Shankar, K.N.; Liu, S.W.; Ganz, D.A. Trends and Characteristics of Emergency Department Visits for Fall-Related Injuries in Older Adults, 2003–2010. West J. Emerg. Med. 2017, 18, 785–793. [Google Scholar] [CrossRef]
- Kirshenbom, D.; Ben-Zaken, Z.; Albilya, N.; Niyibizi, E.; Bala, M. Older Age, Comorbid Illnesses, and Injury Severity Affect Immediate Outcome in Elderly Trauma Patients. J. Emerg. Trauma Shock 2017, 10, 146–150. [Google Scholar]
- Bala, M.; Willner, D.; Klauzn, D.; Bdolah-Abram, T.; Rivkind, A.; Abu Gazala, M.; Elazary, R.; Almogy, G. Pre-hospital and admission parameters predict in-hospital mortality among patients 60 years and older following severe trauma. Scand. J. Trauma Resusc. Emerg. Med. 2013, 21, 91. [Google Scholar] [CrossRef]
- Crawford, S.M. Changing the System-Major Trauma Patients and Their Outcomes in the NHS (England) 2008-17. Eclinicalmedicine 2018, 4, 3. [Google Scholar] [CrossRef]
- Wang, M.C.; Bellows, J. Quality of Life and Patient-Centered Outcomes. In Chronic Illness Care: Principles and Practice; Daaleman, T.P., Helton, M.R., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 95–107. [Google Scholar] [CrossRef]
- Ernstberger, A.; Koller, M.; Nerlich, M. Quality circle in a trauma network of the German Association for Trauma Surgery. Upgrading patient care. Unfallchirurg 2011, 114, 172–181. [Google Scholar] [CrossRef]
- Koller, M.; Ernstberger, A.; Zeman, F.; Loss, J.; Nerlich, M. Trauma Network Eastern Bavaria (TNO). Outcome after polytrauma in a certified trauma network: Comparing standard vs. maximum care facilities concept of the study and study protocol (POLYQUALY). BMC Health Serv. Res. 2016, 16, 242. [Google Scholar] [CrossRef]
- Rabin, R.; de Charro, F. EQ-5D: A measure of health status from the EuroQol Group. Ann. Med. 2001, 33, 337–343. [Google Scholar] [CrossRef]
- Greiner, W.; Claes, C.; Busschbach, J.J.V.; von der Schulenburg, J.-M.G. Validating the EQ-5D with time trade off for the German population. Eur. J. Health Econ. 2005, 6, 124–130. [Google Scholar] [CrossRef]
- Baker, S.P.; O’Neill, B.; Haddon, W.; Long, W.B. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J. Trauma 1974, 14, 187–196. [Google Scholar] [CrossRef]
- Lefering, R.; Huber-Wagner, S.; Nienaber, U.; Maegele, M.; Bouillon, B. Update of the trauma risk adjustment model of the TraumaRegister DGUTM: The Revised Injury Severity Classification, version II. Crit. Care 2014, 18, 476. [Google Scholar] [CrossRef] [PubMed]
- MacKenzie, E.J.; Damiano, A.; Miller, T.; Luchter, S. The development of the Functional Capacity Index. J. Trauma 1996, 41, 799–807. [Google Scholar] [CrossRef]
- Demetriades, D.; Sava, J.; Alo, K.; Newton, E.; Velmahos, G.C.; Murray, J.A.; Belzberg, H.; Asensio, J.A.; Berne, T.V. Old age as a criterion for trauma team activation. J. Trauma 2001, 51, 754–756, discussion 756–757. [Google Scholar] [CrossRef] [PubMed]
- Kuhne, C.A.; Ruchholtz, S.; Kaiser, G.M.; Nast-Kolb, D.; Working Group on Multiple Trauma of the German Society of Trauma. Mortality in severely injured elderly trauma patients-when does age become a risk factor? World J. Surg. 2005, 29, 1476–1482. [Google Scholar] [CrossRef] [PubMed]
- Bergeron, E.; Clement, J.; Lavoie, A.; Ratte, S.; Bamvita, J.-M.; Aumont, F.; Clas, D. A simple fall in the elderly: Not so simple. J. Trauma 2006, 60, 268–273. [Google Scholar] [CrossRef]
- Grossman, M.D.; Miller, D.; Scaff, D.W.; Arcona, S. When is an elder old? Effect of preexisting conditions on mortality in geriatric trauma. J. Trauma 2002, 52, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Sterling, D.A.; O’Connor, J.A.; Bonadies, J. Geriatric falls: Injury severity is high and disproportionate to mechanism. J. Trauma 2001, 50, 116–119. [Google Scholar] [CrossRef]
- Puac-Polanco, V.; Keyes, K.M.; Li, G. Mortality from motorcycle crashes: The baby-boomer cohort effect. Inj. Epidemiol. 2016, 3, 19. [Google Scholar] [CrossRef]
- Arendt, E.A.; DiNubile, N.D. Toward optimal health: The experts discuss fitness among baby boomers. Interview by Jodi Godfrey Meisler. J. Womens Health 2003, 12, 219–225. [Google Scholar]
- Skaga, N.O.; Eken, T.; Søvik, S.; Jones, J.M.; Steen, P.A. Pre-injury ASA physical status classification is an independent predictor of mortality after trauma. J. Trauma 2007, 63, 972–978. [Google Scholar] [CrossRef]
- Ringdal, K.G.; Skaga, N.O.; Steen, P.A.; Hestnes, M.; Laake, P.; Jones, J.M.; Lossius, H.M. Classification of comorbidity in trauma: The reliability of pre-injury ASA physical status classification. Injury 2013, 44, 29–35. [Google Scholar] [CrossRef]
- Sammy, I.; Lecky, F.; Sutton, A.; Leaviss, J.; O’Cathain, A. Factors affecting mortality in older trauma patients-A systematic review and meta-analysis. Injury 2016, 47, 1170–1183. [Google Scholar] [CrossRef]
- Zhu, Z.; Shang, X.; Qi, P.; Ma, S. Sex-based differences in outcomes after severe injury: An analysis of blunt trauma patients in China. Scand. J. Trauma Resusc. Emerg. Med. 2017, 25, 47. [Google Scholar] [CrossRef] [PubMed]
- Angele, M.K.; Frantz, M.C.; Chaudry, I.H. Gender and sex hormones influence the response to trauma and sepsis: Potential therapeutic approaches. Clinics 2006, 61, 479–488. [Google Scholar] [CrossRef]
- Sperry, J.L.; Nathens, A.B.; Frankel, H.L.; Vanek, S.L.; Moore, E.E.; Maier, R.V.; Minei, J.P. Characterization of the gender dimorphism after injury and hemorrhagic shock: Are hormonal differences responsible? Crit. Care Med. 2008, 36, 1838–1845. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.V.R.; Rix, K.; Klein, A.L.; Ford, B.; Teixeira, P.G.R.; Aydelotte, J.; Coopwood, B.; Ali, S. A Comprehensive Investigation of Comorbidities, Mechanisms, Injury Patterns, and Outcomes in Geriatric Blunt Trauma Patients. Am. Surg. 2016, 82, 1055–1062. [Google Scholar] [CrossRef] [PubMed]
- DiMaggio, C.; Ayoung-Chee, P.; Shinseki, M.; Wilson, C.; Marshall, G.; Lee, D.C.; Wall, S.; Maulana, S.; Pachter, H.L.; Frangos, S. Traumatic injury in the United States: In-patient epidemiology 2000–2011. Injury 2016, 47, 1393–1403. [Google Scholar] [CrossRef] [PubMed]
- Fagerström, C.; Borglin, G. Mobility, functional ability and health-related quality of life among people of 60 years or older. Aging Clin. Exp. Res. 2010, 22, 387–394. [Google Scholar] [CrossRef]
- Patel, A.V.; Bernstein, L.; Deka, A.; Spencer Feigelson, H.; Campbell, P.T.; Gapstur, S.M.; Colditz, G.A.; Thun, M.J. Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. Am. J. Epidemiol. 2010, 172, 419–429. [Google Scholar] [CrossRef] [PubMed]
- Hirvensalo, M.; Rantanen, T.; Heikkinen, E. Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older population. J. Am. Geriatr. Soc. 2000, 48, 493–498. [Google Scholar] [CrossRef]
- Kaye, A.D.; Baluch, A.; Scott, J.T. Pain management in the elderly population: A review. Ochsner J. 2010, 10, 179–187. [Google Scholar]
- Sofaer, B.; Moore, A.P.; Holloway, I.; Lamberty, J.M.; Thorp, T.A.; O’Dwyer, J. Chronic pain as perceived by older people: A qualitative study. Age Ageing. 2005, 34, 462–466. [Google Scholar] [CrossRef] [PubMed]
- McCleane, G.; Smith, H. Clinical Management of the Elderly Patient in Pain; CRC Press: Boca Raton, FL, USA, 2006. [Google Scholar]
- Noroozian, M.; Raeesi, S.; Hashemi, R.; Khedmat, L.; Vahabi, Z. Pain: The Neglect Issue in Old People’s Life. Open Access Maced. J. Med. Sci. 2018, 6, 1773–1778. [Google Scholar] [CrossRef] [PubMed]
- Wioletta, M.-D.; Sebastian, D.; Andrzej, B. Perception of barriers to postoperative pain management in elderly patients in Polish hospitals—A multicentre study. J. Nurs. Manag. 2016, 24, 1049–1059. [Google Scholar] [CrossRef] [PubMed]
- Kozar, R.A.; Arbabi, S.; Stein, D.M.; Shackford, S.R.; Barraco, R.D.; Biffl, W.L.; Brasel, K.J.; Cooper, Z.; Fakhry, S.M.; Livingston, D.; et al. Injury in the aged: Geriatric trauma care at the crossroads. J. Trauma Acute Care Surg. 2015, 78, 1197–1209. [Google Scholar] [CrossRef]
- Fares, A. Pharmacological and Non-Pharmacological Means for Prevention of Fractures among Elderly. Int. J. Prev. Med. 2018, 9, 78. [Google Scholar] [CrossRef] [PubMed]
- Verhoeff, K.; Glen, P.; Taheri, A.; Min, B.; Tsang, B.; Fawcett, V.; Widder, S. Implementation and adoption of advanced care planning in the elderly trauma patient. World J. Emerg. Surg. 2018, 13, 40. [Google Scholar] [CrossRef]
- Wong, T.H.; Wong, Y.J.; Lau, Z.Y.; Nadkarni, N.; Lim, G.H.; Seow, D.C.; Ong, M.E.; Tan, K.B.; Nguyen, H.V.; Wong, C.H. Not All Falls Are Equal: Risk Factors for Unplanned Readmission in Older Patients After Moderate and Severe Injury-A National Cohort Study. J. Am. Med. Dir. Assoc. 2019, 20, 201–207.e3. [Google Scholar] [CrossRef]
- Southern, A.P.; Lopez, R.A.; Jwayyed, S. Geriatric Trauma. In StatPearls; StatPearls Publishing: Bethesda, MD, USA, 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK442020/ (accessed on 1 February 2020).
- Gage, A.M.; Traven, N.; Rivara, F.P.; Jurkovich, G.J.; Arbabi, S. Compliance with Centers for Disease Control and Prevention field triage guidelines in an established trauma system. J. Am. Coll. Surg. 2012, 215, 148–154; discussion 154–156. [Google Scholar] [CrossRef]
- Chang, D.C.; Bass, R.R.; Cornwell, E.E.; Mackenzie, E.J. Undertriage of elderly trauma patients to state-designated trauma centers. Arch Surg. 2008, 143, 776–781; discussion 782. [Google Scholar] [CrossRef]
- Ruchholtz, S.; Lefering, R.; Paffrath, T.; Oestern, H.J.; Neugebauer, E.; Nast-Kolb, D.; Pape, H.C.; Bouillon, B. Reduction in mortality of severely injured patients in Germany. Dtsch Arztebl Int. 2008, 105, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Von Oelreich, E.; Eriksson, M.; Brattström, O.; Discacciati, A.; Strömmer, L.; Oldner, A.; Larsson, E. Post-trauma morbidity, measured as sick leave, is substantial and influenced by factors unrelated to injury: A retrospective matched observational cohort study. Scand. J. Trauma Resusc. Emerg. Med. 2017, 25, 100. [Google Scholar] [CrossRef] [PubMed]
- Hays, R.D. Measurement and Modeling of Health-Related Quality of Life. In Epidemiology and Demography in Public Health; Killewo, J., Heggenhougen, H.K., Quah, S.R., Eds.; Academic Press: Cambridge, MA, USA, 2010; pp. 195–205. [Google Scholar]
- Hinz, A.; Klaiberg, A.; Brähler, E.; König, H.-H. The Quality of Life Questionnaire EQ-5D: Modelling and norm values for the general population. Psychother. Psychosom. Med. Psychol. 2006, 56, 42–48. [Google Scholar] [CrossRef] [PubMed]
| Patients < 65 years n = 328 | Patients ≥ 65 years n = 77 | p Value | ||||
|---|---|---|---|---|---|---|
| Age (in years) | 43.0 | (24.3/53.0) | 73.0 | (70.0/78.0) | <0.001 | |
| Sex | ||||||
| male | 245 | (74.7%) | 45 | (58.4%) | 0.007 | |
| female | 83 | (25.3%) | 32 | (41.6%) | ||
| Level of Trauma Center Facility | ||||||
| Level I | 131 | (39.9%) | 21 | (27.3%) | 0.001 | |
| Level II | 186 | (56.7%) | 46 | (59.7%) | ||
| Level III | 11 | (3.4%) | 10 | (13.0%) | ||
| ISS | 22.0 | (18.0/30.0) | 20.0 | (17.0/27.5) | 0.018 | |
| AIS head | 2.0 | (0/3.0) | 2.0 | (0/4.0) | 0.513 | |
| AIS face | 0 | (0/0) | 0 | (0/0) | 0.251 | |
| AIS thorax | 3.0 | (2.0/4.0) | 3.0 | (0/4.0) | 0.937 | |
| AIS abdomen | 0 | (0/2.00) | 0 | (0/2.0) | 0.186 | |
| AIS extremities | 2.0 | (0/3.0) | 2.0 | (0/2.5) | 0.020 | |
| AIS soft tissue | 0 | (0/1.0) | 0 | (0/1.0) | 0.995 | |
| RISC II 1 | 1.2 | (0.7/3.9) | 6.3 | (2.2/16.5) | <0.001 | |
| FCI 2 | 4.0 | (2.0/5.0) | 5.0 | (3.0/5.0) | 0.073 | |
| ASA physical status 3 | 1.0 | (1.0/1.0) | 2.0 | (2.0/3.0) | <0.001 | |
| GCS 4 | 15.0 | (12.0/15.0) | 15.0 | (13.8/15.0) | 0.266 | |
| Type of injury | ||||||
| blunt | 309 | (96.3%) | 73 | (97.3%) | 1.000 | |
| penetrating | 12 | (3.7%) | 2 | (2.7%) | ||
| In hospital stay (in days) | 15.6 | (9.8/24.5) | 17.0 | (11.1/26.9) | 0.215 | |
| Emergency surgery | ||||||
| no | 215 | (70.0%) | 55 | (80.9%) | 0.075 | |
| yes | 92 | (30.0%) | 13 | (19.1%) | ||
| Time between accident and emergency surgery (in hours) 5 | 3.0 | (2.4/4.5) | 3.6 | (1.9/6.4) | 0.599 | |
| stabbing | 33.8% | 27.0% | ||||
| 22.8% | 4.1% | |||||
| 6.5% | 9.5% | |||||
| 4.0% | 10.8% | |||||
| 16% | 13.5% | |||||
| 8.6% | 20.3% | |||||
| 1.2% | 0.0% | |||||
| 3.2% | 5.4% | |||||
| 0.6% | 0.0% | |||||
| Estimate | 95% CI | p Value | |||
|---|---|---|---|---|---|
| EQ index | |||||
| FCI | 0.04 | 0.02 | 0.06 | <0.001 | |
| RISC II | −0.003 | −0.005 | −0.001 | 0.001 | |
| AIS head | −0.01 | −0.02 | 0.01 | 0.315 | |
| AIS face | 0.03 | 0.00 | 0.06 | 0.026 | |
| AIS thorax | −0.01 | −0.03 | 0.01 | 0.198 | |
| AIS abdomen | 0.01 | −0.01 | 0.03 | 0.178 | |
| AIS extremities | −0.02 | −0.04 | 0.00 | 0.016 | |
| AIS soft tissue | −0.01 | −0.04 | 0.03 | 0.742 | |
| ASA physical status | −0.08 | −0.12 | −0.03 | <0.001 | |
| EQ VAS | |||||
| FCI | 2.50 | 0.98 | 4.02 | 0.001 | |
| RISC II | −0.23 | −0.38 | −0.09 | 0.001 | |
| AIS head | −0.25 | −1.60 | 1.09 | 0.712 | |
| AIS face | 1.86 | −0.46 | 4.18 | 0.116 | |
| AIS thorax | 0.18 | −1.16 | 1.52 | 0.789 | |
| AIS abdomen | 1.20 | −0.24 | 2.64 | 0.101 | |
| AIS extremities | −2.01 | −3.49 | −0.53 | 0.008 | |
| AIS soft tissue | 0.26 | −2.41 | 2.93 | 0.847 | |
| ASA physical status | −7.20 | −10.63 | −3.77 | <0.001 | |
| 6 Months Post Trauma | 12 Months Post Trauma | 24 Months Post Trauma | p Value 2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | m | 95% CI | n | m | 95% CI | n | m | 95% CI | |||||
| EQ Index | |||||||||||||
| <65 years | 256 | 0.70 | 0.66 | 0.74 | 268 | 0.74 | 0.70 | 0.77 | 247 | 0.77 | 0.74 | 0.81 | 0.004 |
| ≥65 years | 55 | 0.69 | 0.61 | 0.77 | 55 | 0.69 | 0.61 | 0.76 | 44 | 0.73 | 0.64 | 0.81 | 0.558 |
| p value 1 | 0.755 | 0.232 | 0.304 | ||||||||||
| EQ VAS | |||||||||||||
| <65 years | 262 | 61.2 | 58.2 | 64.2 | 268 | 69.3 | 66.6 | 72.1 | 248 | 68.8 | 65.9 | 71.6 | <0.001 |
| ≥65 years | 55 | 59.4 | 53.2 | 65.6 | 55 | 62.7 | 57.0 | 68.5 | 45 | 63.8 | 57.3 | 70.3 | 0.262 |
| p value 1 | 0.618 | 0.051 | 0.177 | ||||||||||
| 6 Months Post Trauma | 12 Months Post Trauma | 24 Months Post Trauma | p Value 2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | m | 95% CI | n | m | 95% CI | n | m | 95% CI | |||||
| EQ Index | |||||||||||||
| male | 220 | 0.72 | 0.67 | 0.78 | 232 | 0.72 | 0.68 | 0.77 | 212 | 0.76 | 0.72 | 0.81 | 0.193 |
| female | 91 | 0.67 | 0.60 | 0.74 | 91 | 0.70 | 0.64 | 0.76 | 79 | 0.74 | 0.67 | 0.81 | 0.242 |
| p value 1 | 0.209 | 0.546 | 0.548 | ||||||||||
| EQ VAS | |||||||||||||
| male | 226 | 63.8 | 59.8 | 67.8 | 232 | 65.8 | 62.1 | 69.5 | 213 | 65.4 | 61.6 | 69.3 | 0.413 |
| female | 91 | 56.8 | 51.6 | 62.1 | 91 | 66.3 | 61.4 | 71.1 | 80 | 67.1 | 61.5 | 72.7 | <0.001 |
| p value 1 | 0.036 | 0.883 | 0.614 | ||||||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Freigang, V.; Müller, K.; Ernstberger, A.; Kaltenstadler, M.; Bode, L.; Pfeifer, C.; Alt, V.; Baumann, F. Reduced Recovery Capacity After Major Trauma in the Elderly: Results of a Prospective Multicenter Registry-Based Cohort Study. J. Clin. Med. 2020, 9, 2356. https://doi.org/10.3390/jcm9082356
Freigang V, Müller K, Ernstberger A, Kaltenstadler M, Bode L, Pfeifer C, Alt V, Baumann F. Reduced Recovery Capacity After Major Trauma in the Elderly: Results of a Prospective Multicenter Registry-Based Cohort Study. Journal of Clinical Medicine. 2020; 9(8):2356. https://doi.org/10.3390/jcm9082356
Chicago/Turabian StyleFreigang, Viola, Karolina Müller, Antonio Ernstberger, Marlene Kaltenstadler, Lisa Bode, Christian Pfeifer, Volker Alt, and Florian Baumann. 2020. "Reduced Recovery Capacity After Major Trauma in the Elderly: Results of a Prospective Multicenter Registry-Based Cohort Study" Journal of Clinical Medicine 9, no. 8: 2356. https://doi.org/10.3390/jcm9082356
APA StyleFreigang, V., Müller, K., Ernstberger, A., Kaltenstadler, M., Bode, L., Pfeifer, C., Alt, V., & Baumann, F. (2020). Reduced Recovery Capacity After Major Trauma in the Elderly: Results of a Prospective Multicenter Registry-Based Cohort Study. Journal of Clinical Medicine, 9(8), 2356. https://doi.org/10.3390/jcm9082356







