Narrow-Margin Excision for Invasive Acral Melanoma: Is It Acceptable?
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Patients
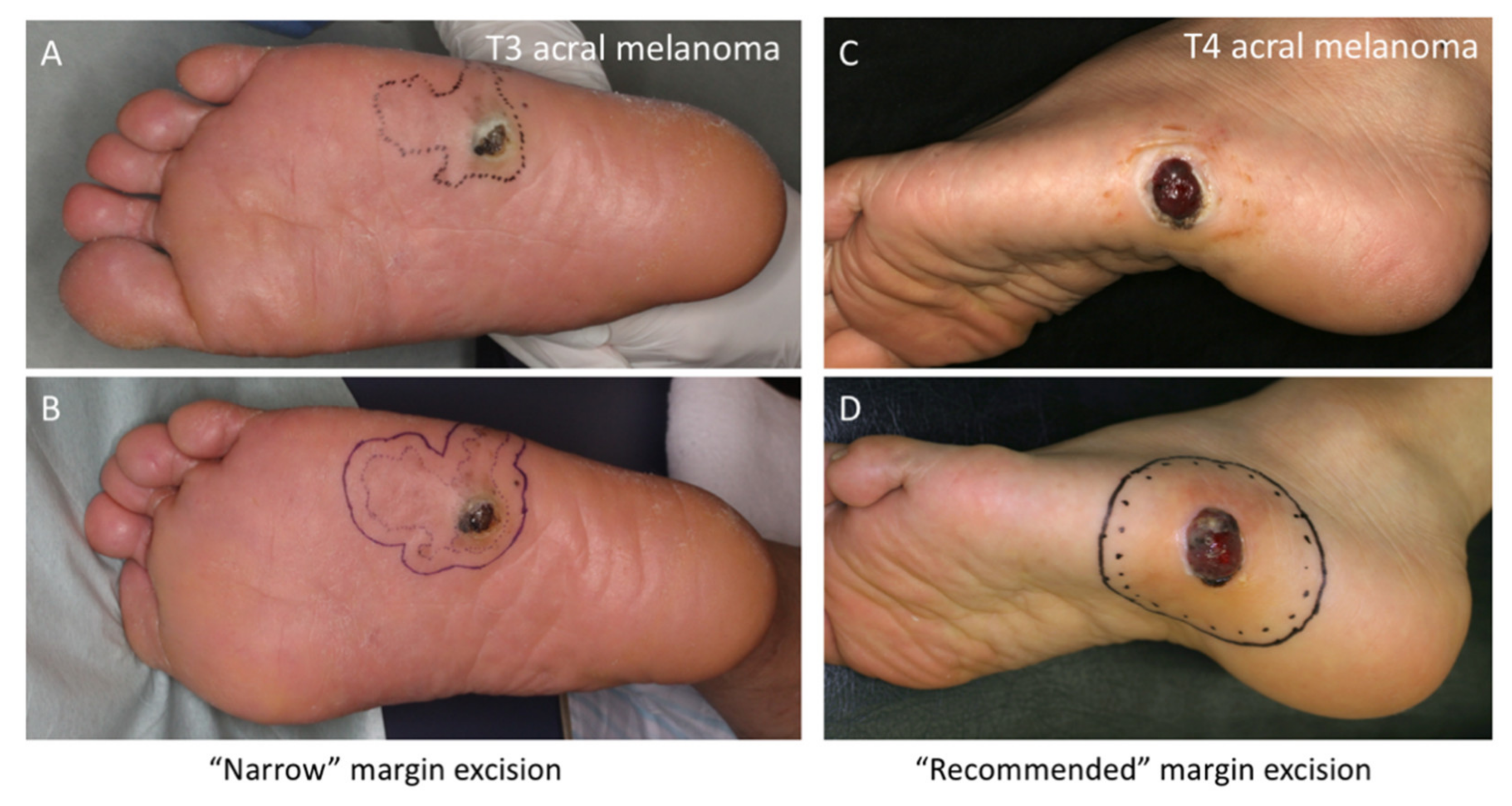
2.3. Surgical Margins
2.4. Statistical Analysis
3. Results
3.1. Patient Data
3.2. Surgical Margins for Invasive Acral Melanomas
3.3. Patient Outcomes at the End of the Follow-Up Periods
3.4. Kaplan-Meier Analysis for MSS and DFS
3.5. Comparison between Narrow and Recommended Margins
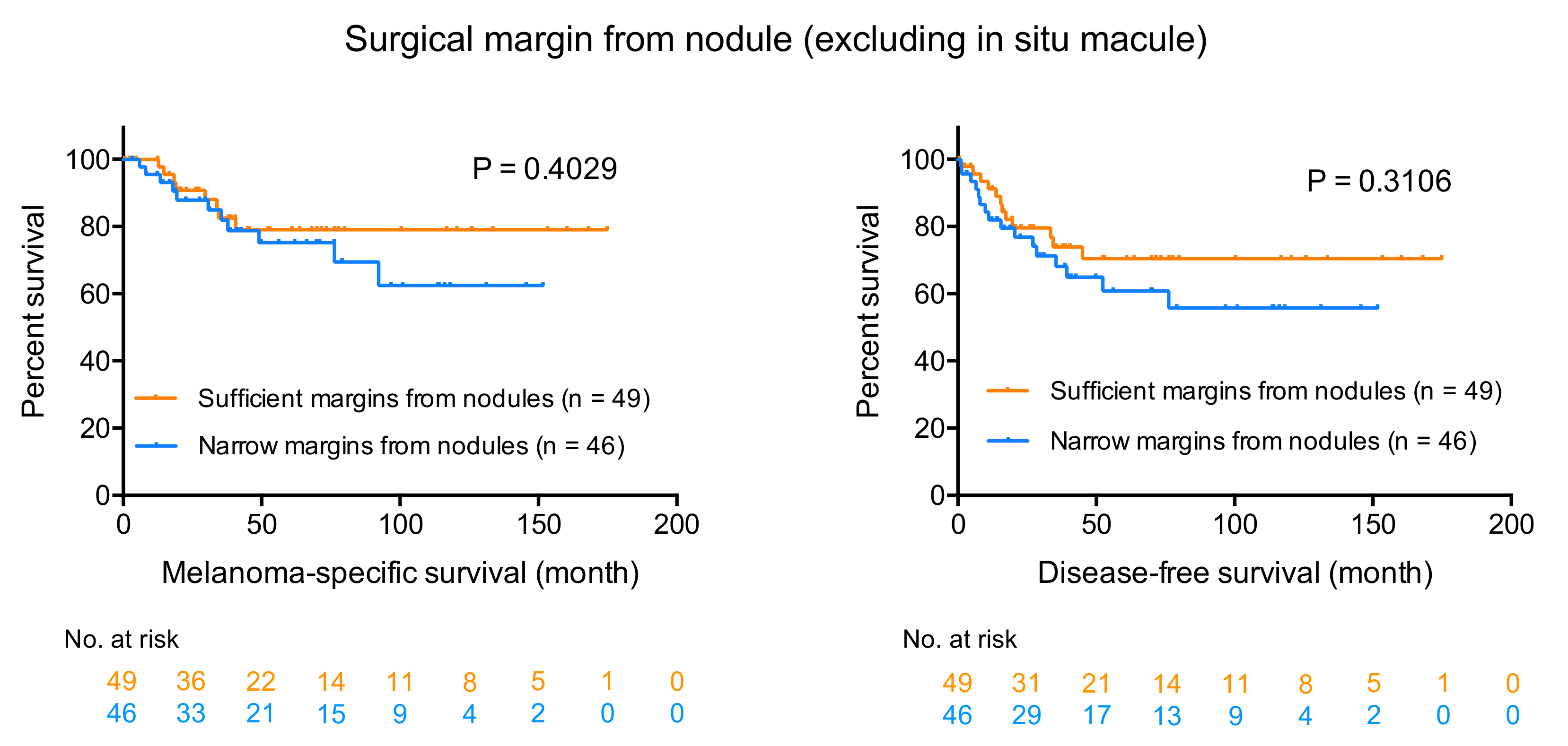
3.6. Prognostic Impact of Surgical Margin from Nodule
3.7. Comparison between Narrow and Sufficient Margins from Nodules
3.8. Cox Multivariate Analyses for MSS and DFS: Surgical Margins from Lateral Borders
3.9. Cox Multivariate Analyses for MSS and DFS: Surgical Margins from Nodules
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, N.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 2014, 136. [Google Scholar] [CrossRef] [PubMed]
- Kohler, B.A.; Ward, E.; McCarthy, B.J.; Schymura, M.J.; Ries, L.A.G.; Eheman, C.; Jemal, A.; Anderson, R.N.; Ajani, U.A.; Edwards, B.K. Annual Report to the Nation on the Status of Cancer, 1975-2007, Featuring Tumors of the Brain and Other Nervous System. J. Natl. Cancer Inst. 2011, 103, 714–736. [Google Scholar] [CrossRef] [PubMed]
- NCCN Guidelines Version 3.2020 Cutaneous Melanoma. Available online: https://www.nccn.org/professionals/physician_gls/pdf/cutaneous_melanoma.pdf. (accessed on 16 June 2020).
- Furue, M.; Ito, T.; Wada, N.; Wada-Ohno, M.; Kadono, T.; Uchi, H. Melanoma and Immune Checkpoint Inhibitors. Curr. Oncol. Rep. 2018, 20, 29. [Google Scholar] [CrossRef] [PubMed]
- Cohn-Cedermark, G.; Rutqvist, L.E.; Andersson, R.; Breivald, M.; Ingvar, C.; Johansson, H.; Jönsson, P.E.; Krysander, L.; Lindholm, C.; Ringborg, U. Long term results of a randomized study by the Swedish Melanoma Study Group on 2-cm versus 5-cm resection margins for patients with cutaneous melanoma with a tumor thickness of 0.8-2.0 mm. Cancer 2000, 89, 1495–1501. [Google Scholar] [CrossRef]
- Mocellin, S.; Pasquali, S.; Nitti, D. The Impact of Surgery on Survival of Patients With Cutaneous Melanoma. Ann. Surg. 2011, 253, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Lens, M.B.; Dawes, M.; Goodacre, T.; Bishop, J.A.N. Excision Margins in the Treatment of Primary Cutaneous Melanoma. Arch. Surg. 2002, 137, 1101–1105. [Google Scholar] [CrossRef] [PubMed]
- Cascinelli, N. Margin of resection in the management of primary melanoma. Semin. Surg. Oncol. 1998, 14, 272–275. [Google Scholar] [CrossRef]
- Balch, C.M.; Soong, S.-J.; Smith, T.; Ross, M.I.; Urist, M.M.; Karakousis, C.P.; Temple, W.J.; Mihm, M.C.; Barnhill, R.L.; Jewell, W.R.; et al. Long-Term Results of a Prospective Surgical Trial Comparing 2 cm vs. 4 cm Excision Margins for 740 Patients With 1?4 mm Melanomas. Ann. Surg. Oncol. 2001, 8, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Khayat, D.; Rixe, O.; Martin, G.; Soubrane, C.; Banzet, M.; Bazex, J.-A.; Lauret, P.; Verola, O.; Auclerc, G.; Harper, P.; et al. Surgical margins in cutaneous melanoma (2 cm versus 5 cm for lesions measuring less than 2.1-mm thick). Cancer 2003, 97, 1941–1946. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.M.; Newton-Bishop, J.; A’Hern, R.; Coombes, G.; Timmons, M.; Evans, J.; Cook, M.; Theaker, J.; Fallowfield, M.; O’Neill, T.; et al. Excision Margins in High-Risk Malignant Melanoma. N. Engl. J. Med. 2004, 350, 757–766. [Google Scholar] [CrossRef] [PubMed]
- Gillgren, P.; Drzewiecki, K.T.; Niin, M.; Gullestad, H.P.; Hellborg, H.; Månsson-Brahme, E.; Ingvar, C.; Ringborg, U. 2-cm versus 4-cm surgical excision margins for primary cutaneous melanoma thicker than 2 mm: A randomised, multicentre trial. Lancet 2011, 378, 1635–1642. [Google Scholar] [CrossRef]
- Curtin, J.; Fridlyand, J.; Kageshita, T.; Patel, H.N.; Busam, K.J.; Kutzner, H.; Cho, K.-H.; Aiba, S.; Bröcker, E.-B.; LeBoit, P.E.; et al. Distinct Sets of Genetic Alterations in Melanoma. N. Engl. J. Med. 2005, 353, 2135–2147. [Google Scholar] [CrossRef] [PubMed]
- Rabbie, R.; Ferguson, P.; Molina-Aguilar, C.; Adams, D.J.; Robles-Espinoza, C.D. Melanoma subtypes: Genomic profiles, prognostic molecular markers and therapeutic possibilities. J. Pathol. 2019, 247, 539–551. [Google Scholar] [CrossRef] [PubMed]
- Ito, T.; Kaku-Ito, Y.; Murata, M.; Ichiki, T.; Kuma, Y.; Tanaka, Y.; Ide, T.; Ohno, F.; Wada-Ohno, M.; Yamada, Y.; et al. Intra- and Inter-Tumor BRAF Heterogeneity in Acral Melanoma: An Immunohistochemical Analysis. Int. J. Mol. Sci. 2019, 20, 6191. [Google Scholar] [CrossRef] [PubMed]
- Ito, T.; Kaku-Ito, Y.; Murata, M.; Furue, K.; Shen, C.-H.; Oda, Y.; Furue, M. Immunohistochemical BRAF V600E Expression and Intratumor BRAF V600E Heterogeneity in Acral Melanoma: Implication in Melanoma-Specific Survival. J. Clin. Med. 2020, 9, 690. [Google Scholar] [CrossRef] [PubMed]
- Ito, T.; Wada-Ohno, M.; Nagae, K.; Nakano-Nakamura, M.; Nakahara, T.; Hagihara, A.; Furue, M.; Uchi, H. Acral lentiginous melanoma: Who benefits from sentinel lymph node biopsy? J. Am. Acad. Dermatol. 2015, 72, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Ito, T.; Wada, M.; Nagae, K.; Nakano-Nakamura, M.; Nakahara, T.; Hagihara, A.; Furue, M.; Uchi, H. Triple-marker PCR assay of sentinel lymph node as a prognostic factor in melanoma. J. Eur. Acad. Dermatol. Venereol. 2014, 29, 912–918. [Google Scholar] [CrossRef] [PubMed]
- Wada-Ohno, M.; Ito, T.; Tsuji, G.; Nakahara, T.; Hagihara, A.; Furue, M.; Uchi, H. Acral lentiginous melanoma versus other melanoma: A single-center analysis in Japan. J. Dermatol. 2017, 61, 212–938. [Google Scholar] [CrossRef]
- Bajaj, S.; Donnelly, D.; Call, M.; Johannet, P.; Moran, U.; Polsky, D.; Shapiro, R.; Berman, R.; Pavlick, A.; Weber, J.; et al. Melanoma Prognosis: Accuracy of the American Joint Committee on Cancer Staging Manual Eighth Edition. J. Natl. Cancer Inst. 2020. [Google Scholar] [CrossRef] [PubMed]
- Wheatley, K.; Wilson, J.S.; Gaunt, P.; Marsden, J.R. Surgical excision margins in primary cutaneous melanoma: A meta-analysis and Bayesian probability evaluation. Cancer Treat. Rev. 2016, 42, 73–81. [Google Scholar] [CrossRef] [PubMed]


| Parameter | Number (%) |
|---|---|
| Age in years | |
| Range (mean ± SD) | 16–89 (67.0 ± 15.7) |
| Sex | |
| Male | 42 (42.0) |
| Female | 58 (58.0) |
| Histopathological subtype | |
| Acral lentiginous | 100 (100) |
| Primary tumor site | |
| Palm | 15 (15.0) |
| Sole | 65 (65.0) |
| Nail bed | 20 (20.0) |
| Ulceration | |
| Present | 49 (49.0) |
| Absent | 51 (51.0) |
| T category | |
| T1 | 31 (31.0) |
| T2 | 15 (15.0) |
| T3 | 16 (16.0) |
| T4 | 38 (38.0) |
| American Joint Committee on Cancer stage | |
| I | 42 (42.0) |
| II | 30 (30.0) |
| III | 23 (23.0) |
| IV | 5 (5.0) |
| Melanoma-specific survival in months | |
| Range (mean ± SD) | 1–175 (54.3 ± 43.9) |
| Disease-free survival in months | |
| Range (mean ± SD) | 0–175 (48.4 ± 46.3) |
| Total | 100 (100.0) |
| T Category (NCCN Recommendation) | Surgical Margin from Tumor Border | Patients (n) | Positive Margin (n) |
|---|---|---|---|
| T1 | 5 mm | 16 | 1 a |
| (10 mm) | ≥10 mm | 15 | 1 b |
| T2 | 5 mm | 3 | 0 |
| (10–20 mm) | 10 mm | 8 | 1 c |
| 20 mm | 4 | 0 | |
| T3 | 10 mm | 11 | 0 |
| (20 mm) | 15 mm | 2 | 0 |
| 20 mm | 3 | 0 | |
| T4 | 5 mm | 7 | 0 |
| (20 mm) | 10 mm | 20 | 0 |
| 15 mm | 6 | 0 | |
| ≥20 mm | 5 | 0 |
| T Category | Surgical Margin (n) | Local Recurrence | In Transit Metastasis | Death Due to Melanoma | Follow-Up (Person-Years) |
|---|---|---|---|---|---|
| T1 | Narrow (16) | 1 (6.3%) | 0 | 2 (12.5%) | 72.6 |
| Recommended (15) | 0 | 0 | 0 | 72.3 | |
| T2 | Narrow (3) | 0 | 0 | 0 | 7.3 |
| Recommended (12) | 0 | 0 | 1 (8.3%) | 68.6 | |
| T3 | Narrow (12) | 0 | 3 (25.0%) | 0 | 67.3 |
| Recommended (3) | 0 | 1 (33.1%) | 1 (33.3%) | 15.1 | |
| T4 | Narrow (29) | 1 (3.4%) | 4 (13.8%) | 14 (48.3%) | 122.4 |
| Recommended (5) | 0 | 0 | 1 (20.0%) | 19.9 |
| Parameter | Narrow | Recommended | p |
|---|---|---|---|
| Age in years | |||
| Mean ± SD | 67.3 ± 15.8 | 66.3 ± 16.8 | 0.9220 |
| Breslow thickness (mm) | |||
| Mean ± SD | 4.21 ± 2.96 | 2.03 ± 2.20 | 0.0013 * |
| Sex | |||
| Male | 25 | 12 | 0.5194 |
| Female | 35 | 23 | |
| Primary tumor site | |||
| Palm | 9 | 6 | 0.9540 |
| Sole | 38 | 22 | |
| Nail bed | 13 | 7 | |
| Ulceration | |||
| Present | 31 | 14 | 0.2947 |
| Absent | 29 | 21 | |
| American Joint Committee on Cancer stage | |||
| I or II | 42 | 30 | 0.1351 |
| III | 18 | 5 | |
| Total | 60 | 35 | |
| Parameter | Narrow | Sufficient | p |
|---|---|---|---|
| Age in years | |||
| Mean ± SD | 65.1 ± 16.6 | 68.7 ± 15.5 | 0.2264 |
| Breslow thickness (mm) | |||
| Mean ± SD | 3.86 ± 3.11 | 2.62 ± 2.55 | 0.0633 |
| Sex | |||
| Male | 17 | 20 | 0.8336 |
| Female | 29 | 29 | |
| Primary tumor site | |||
| Palm | 9 | 6 | 0.4120 |
| Sole | 26 | 34 | |
| Nail bed | 11 | 9 | |
| Ulceration | |||
| Present | 21 | 24 | 0.8379 |
| Absent | 25 | 25 | |
| American Joint Committee on Cancer stage | |||
| I or II | 33 | 39 | 0.4736 |
| III | 13 | 10 | |
| Total | 46 | 49 | |
| MSS | DFS | |||||
|---|---|---|---|---|---|---|
| Variable | HR | 95% CI | p | HR | 95% CI | p |
| Age † | 1.05 | 1.01–1.10 | 0.0286 * | 1.03 | 0.99–1.06 | 0.0892 |
| Sex, male | 1.87 | 0.75–4.65 | 0.1806 | 1.73 | 0.82–3.66 | 0.1528 |
| Breslow thickness † | 1.20 | 1.02–1.40 | 0.0226 * | 1.19 | 1.05–1.34 | 0.0045 * |
| Surgical margin, narrow | 1.83 | 0.47–7.14 | 0.3836 | 1.73 | 0.60–4.99 | 0.3092 |
| MSS | DFS | |||||
|---|---|---|---|---|---|---|
| Variable | HR | 95% CI | p | HR | 95% CI | p |
| Age † | 1.05 | 1.01–1.10 | 0.0265 * | 1.03 | 0.99–1.06 | 0.0797 |
| Sex, male | 1.99 | 0.79–5.03 | 0.1459 | 1.84 | 0.86–3.93 | 0.1169 |
| Breslow thickness † | 1.23 | 1.06–1.42 | 0.0045 * | 1.22 | 1.08–1.36 | 0.0006 * |
| Margin from nodule, narrow | 1.29 | 0.50–3.33 | 0.5962 | 1.23 | 0.56–2.70 | 0.6087 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ito, T.; Kaku-Ito, Y.; Wada-Ohno, M.; Furue, M. Narrow-Margin Excision for Invasive Acral Melanoma: Is It Acceptable? J. Clin. Med. 2020, 9, 2266. https://doi.org/10.3390/jcm9072266
Ito T, Kaku-Ito Y, Wada-Ohno M, Furue M. Narrow-Margin Excision for Invasive Acral Melanoma: Is It Acceptable? Journal of Clinical Medicine. 2020; 9(7):2266. https://doi.org/10.3390/jcm9072266
Chicago/Turabian StyleIto, Takamichi, Yumiko Kaku-Ito, Maiko Wada-Ohno, and Masutaka Furue. 2020. "Narrow-Margin Excision for Invasive Acral Melanoma: Is It Acceptable?" Journal of Clinical Medicine 9, no. 7: 2266. https://doi.org/10.3390/jcm9072266
APA StyleIto, T., Kaku-Ito, Y., Wada-Ohno, M., & Furue, M. (2020). Narrow-Margin Excision for Invasive Acral Melanoma: Is It Acceptable? Journal of Clinical Medicine, 9(7), 2266. https://doi.org/10.3390/jcm9072266





