Long-Term Outcomes of Patients with Unprotected Left Main Coronary Artery Disease Treated with Percutaneous Angioplasty versus Bypass Grafting: A Meta-Analysis of Randomized Controlled Trials
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Data Extraction
2.4. Outcomes and Definitions
2.5. Quality Assessment
2.6. Statistical Analysis
3. Results
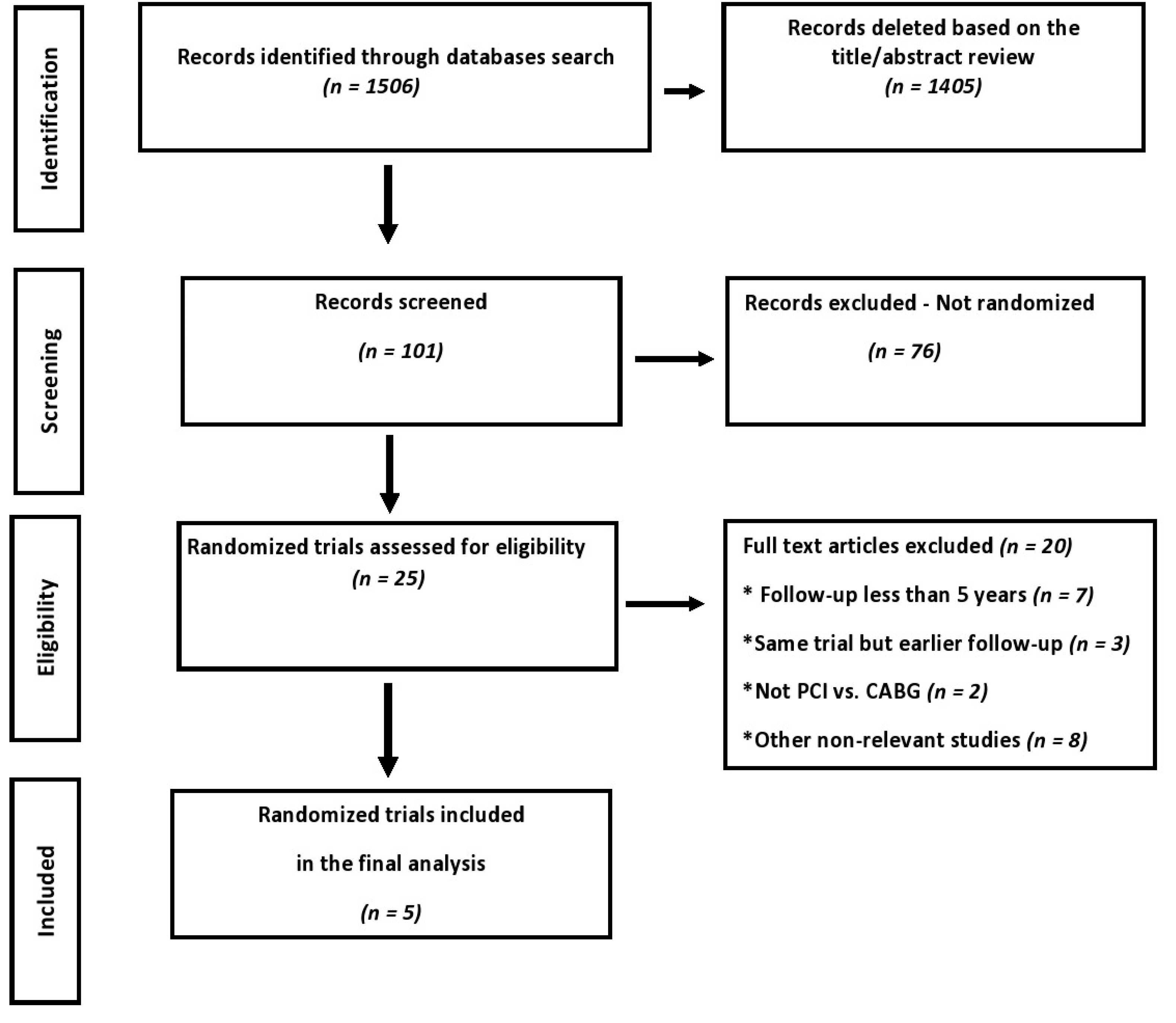
3.1. Search Results and Trial Flow
3.2. Characteristics of Included Studies
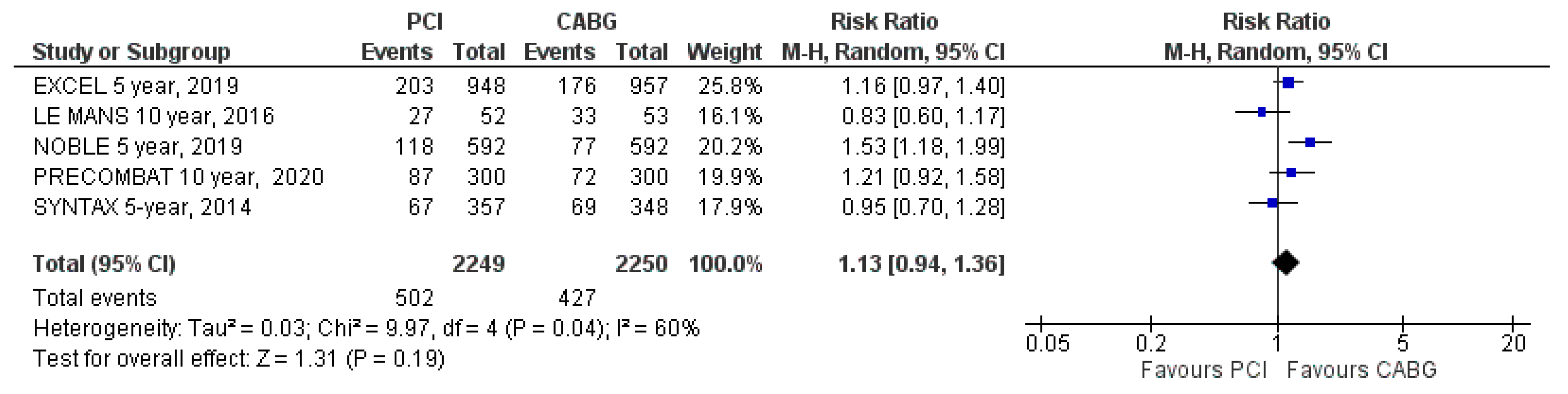
3.3. Primary Clinical Outcomes
MACE
3.4. Secondary Clinical Outcomes
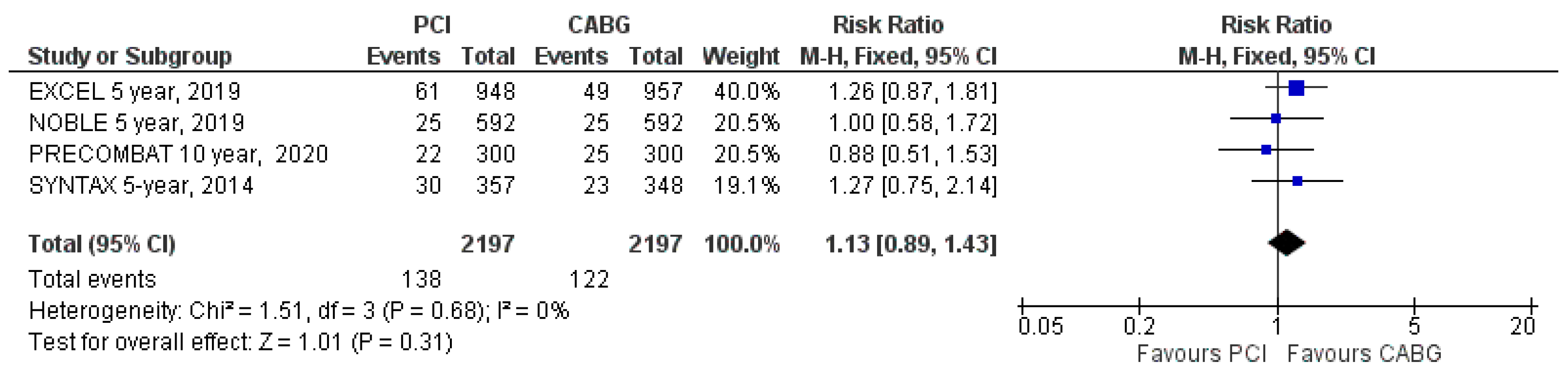
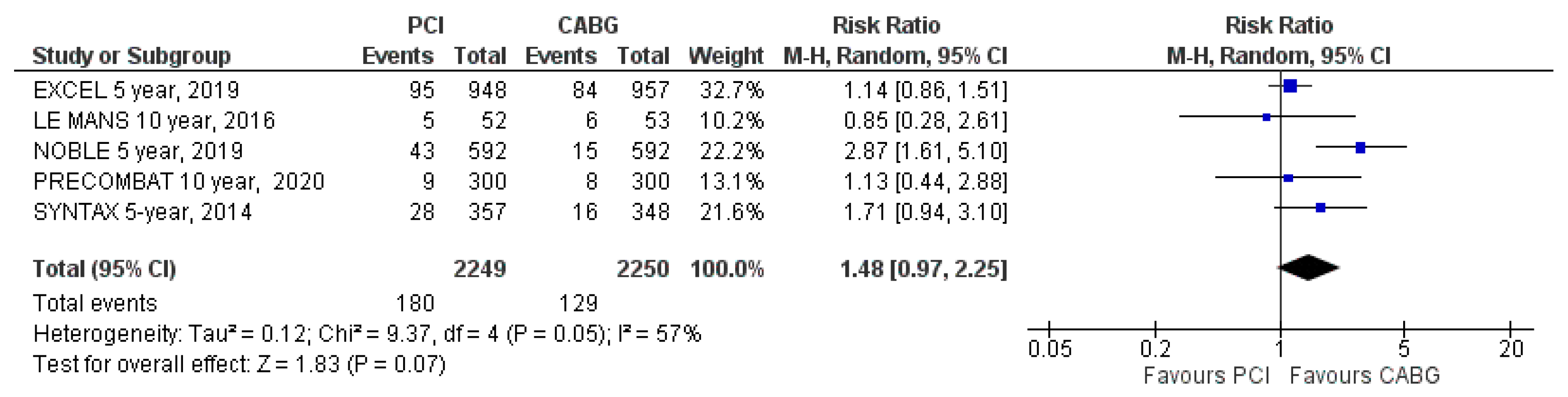
3.4.1. All-Cause Mortality
3.4.2. CV Mortality
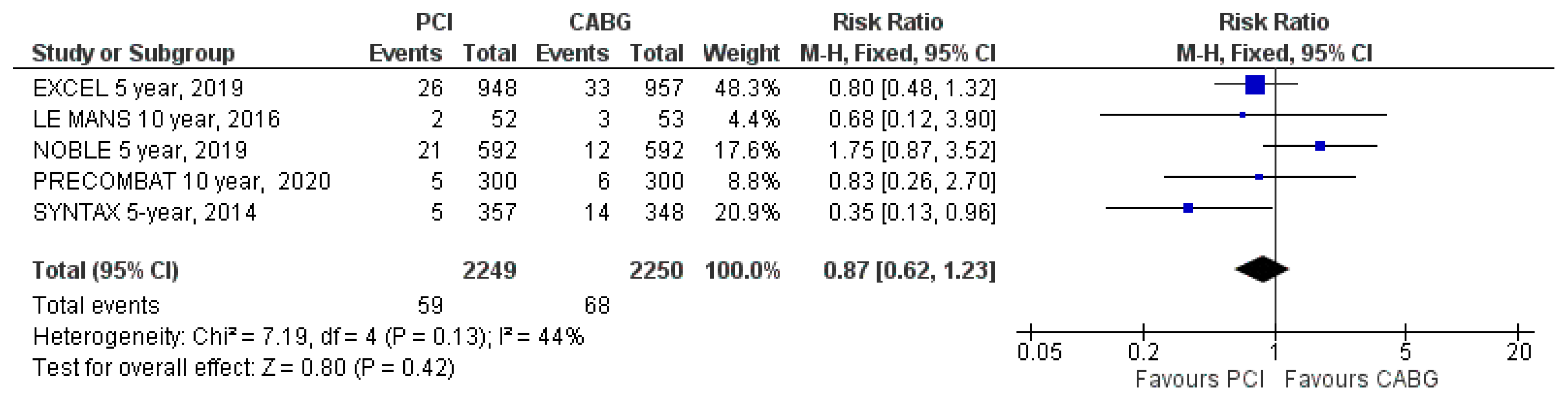
3.4.3. Stroke
3.4.4. Myocardial Infarction
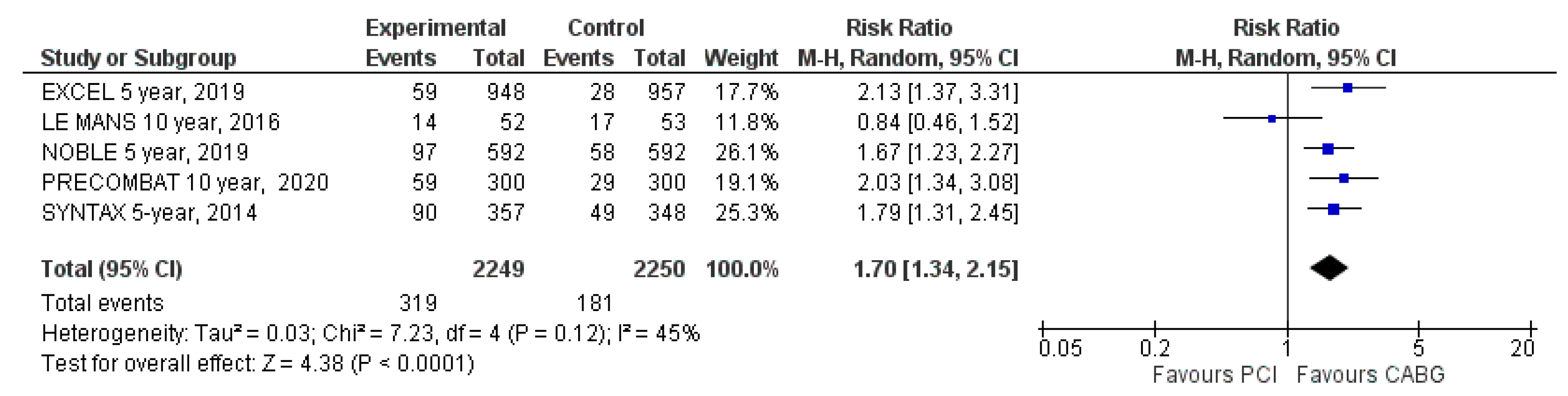
3.4.5. Unplanned Repeat Revascularization
3.4.6. Risk of Bias Assessment
4. Discussion
4.1. Findings
4.2. Data Interpretation
4.3. Clinical Implications
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.-P.; Falk, V.; ESC Scientific Document Group; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef]
- Patel, M.R.; Dehmer, G.J.; Hirshfeld, J.W.; Smith, P.K.; Spertus, J.A. ACCF/SCAI/STS/AATS/AHA/ASNC/HFSA/SCCT 2012 appropriate use criteria for coronary revascularization focused update: A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, American Society of Nuclear Cardiology, and the Society of Cardiovascular Computed Tomography. J. Am. Coll. Cardiol. 2012, 59, 857–881. [Google Scholar] [CrossRef] [PubMed]
- Holm, N.R.; Mäkikallio, T.; Lindsay, M.M.; Spence, M.S.; Erglis, A.; Menown, I.B.A.; Trovik, T.; Eskola, M.; Romppanen, H.; SYNTAX Extended Survival Investigators; et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in the treatment of unprotected left main stenosis: Updated 5-year outcomes from the randomised, non-inferiority NOBLE trial. Lancet 2020, 395, 191–199. [Google Scholar] [CrossRef]
- Thuijs, D.J.F.M.; Kappetein, A.P.; Serruys, P.W.; Mohr, F.-W.; Morice, M.-C.; Mack, M.J.; Holmes, D.R., Jr.; Curzen, N.; Davierwala, P.; SYNTAX Extended Survival Investigators; et al. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomised controlled SYNTAX trial. Lancet 2019, 394, 1325–1334. [Google Scholar] [CrossRef]
- Stone, G.W.; Kappetein, A.P.; Sabik, J.F.; Pocock, S.J.; Morice, M.C.; Puskas, J.; Kandzari, D.E.; Karmpaliotis, D.; Brown, W.M., II; EXCEL Trial Investigators; et al. Five-Year Outcomes after PCI or CABG for Left Main Coronary Disease. N. Engl. J. Med. 2019, 381, 1820–1830. [Google Scholar] [CrossRef] [PubMed]
- Park, D.W.; Ahn, J.M.; Park, H.; Yun, S.C.; Kang, D.Y.; Lee, P.H.; Kim, Y.-H.; Lim, D.-S.; Rha, S.-W.; PRECOMBAT Investigators; et al. Ten-Year Outcomes After Drug-Eluting Stents Versus Coronary Artery Bypass Grafting for Left Main Coronary Disease: Extended Follow-Up of the PRECOMBAT Trial. Circulation 2020, 141, 1437–1446. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- Green, S. Cochrane Handbook for Systematic Reviews of Interventions; The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- The Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions—10.4.3.1 Recommendations on Testing for Funnel Plot Asymmetry; The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- Cooper, H.M.; Hedges, L.V. The Handbook of Research Synthesis; Russell Sage Foundation: New York, NY, USA, 1994. [Google Scholar]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Abramson, J.; Abramsonm, Z. Making Sense of Data: A Self-Instruction Manual on the Interpretation of Epidemiological Data; Oxford University Press: Oxford, UK, 2001; ISBN 0-19-514525-9. [Google Scholar]
- Buszman, P.E.; Buszman, P.P.; Banasiewicz-Szkróbka, I.; Milewski, K.P.; Żurakowski, A.; Orlik, B.; Konkolewska, M.; Trela, B.; Janas, A.; Martin, J.L.; et al. Left Main Stenting in Comparison with Surgical Revascularization: 10-Year Outcomes of the (Left Main Coronary Artery Stenting) LE MANS Trial. JACC Cardiovasc. Interv. 2016, 9, 318–327. [Google Scholar] [CrossRef] [PubMed]
- Morice, M.C.; Serruys, P.W.; Kappetein, A.P.; Feldman, T.E.; Stahle, E.; Colombo, A.; Mack, M.J.; Holmes, D.R.; Choi, J.W.; Ruzyllo, W.; et al. Five-Year outcomes in patients with left main disease treated with either percutaneous coronary intervention or coronary artery bypass grafting in the synergy between percutaneous coronary intervention with taxus and cardiacsurgery trial. Circulation 2014, 129, 2388–2394. [Google Scholar] [CrossRef] [PubMed]
- El-Menyar, A.A.; Al Suwaidi, J.; Holmes, D.R., Jr. Left main coronary artery stenosis: State-of-the-Art. Curr. Probl. Cardiol. 2007, 32, 103–193. [Google Scholar] [CrossRef] [PubMed]
- Alfonso, F.; Antuña, P. New-Generation drug-eluting stents for unselected patients with left main coronary artery disease: Crossing a second Rubicon? Int. J. Cardiol. 2019, 280, 49–50. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, Y.; Howard, J.P.; Arnold, A.D.; Cook, C.M.; Prasad, M.; Ali, Z.A.; Parikh, M.A.; Kosmidou, I.; Francis, D.P.; Moses, J.W.; et al. Mortality after drug-eluting stents vs. coronary artery bypass grafting for left main coronary artery disease: A meta-analysis of randomized controlled trials. Eur. Heart J. 2020. [Google Scholar] [CrossRef] [PubMed]
- D’Ascenzo, F.; De Filippo, O.; Elia, E.; Doronzo, M.P.; Omedè, P.; Montefusco, A.; Pennone, M.; Salizzoni, S.; Conrotto, F.; Gallone, G.; et al. Percutaneous vs. surgical revascularization for patients with unprotected left main stenosis: A meta-analysis of 5 years follow-up RCTs. Eur. Heart J. Qual. Care Clin. Outcomes 2020. [Google Scholar] [CrossRef]
- Borhani, S.; Hassanajili, S.; Ahmadi Tafti, S.H.; Rabbani, S. Cardiovascular stents: Overview, evolution, and next generation. Prog. Biomater. 2018, 7, 175–205. [Google Scholar] [CrossRef] [PubMed]
- Shelton, M.E.; Forman, M.B.; Virmani, R.; Bajaj, A.; Stoney, W.S.; Atkinson, J.B. A comparison of morphologic and angiographic findings in long-term internal mammary artery and saphenous vein bypass grafts. J. Am. Coll. Cardiol. 1988, 11, 297–307. [Google Scholar] [CrossRef]
- Henein, M.Y.; Vancheri, S.; Bajraktari, G.; Vancheri, F. Coronary Atherosclerosis Imaging. Diagnostics 2020, 10, 65. [Google Scholar] [CrossRef] [PubMed]
- Yoon, H.C.; Emerick, A.M.; Hill, J.A.; Gjertson, D.W.; Goldin, J.G. Calcium begets calcium: Progression of coronary artery calcification in asymptomatic subjects. Radiology 2002, 224, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Alfonso, F.; Kastrati, A. Ten-Year Follow-Up of Left Main Coronary Artery Revascularization: Still Equipoise between Percutaneous Interventions and Surgery? Circulation 2020, 141, 1447–1451. [Google Scholar] [CrossRef] [PubMed]

| Excel | Le Mans | Noble | Precombat | Syntax | |
|---|---|---|---|---|---|
| Publication year | 2019 | 2016 | 2019 | 2020 | 2019 |
| Number of patients after 5-year follow-ups | 1905 (PCI n = 948; CABG n = 957) | 105 (PCI n = 52; CABG n = 53) | 1184 (PCI n = 592; CABG n = 592) | 600 (PCI n = 300; CABG n = 300) | 705 (PCI n = 357; CABG n = 348) |
| Major inclusion criteria | Unprotected LMCA stenosis >70% or >50% if hemodynamically significant | Symptomatic stenosis > 50% of unprotected LMCA | Unprotected LMCA stenosis > 50% or FFR ≤ 0.80 without more than three noncomplex lesions | Symptomatic or asymptomatic unprotected LMCA stenosis > 50% regardless of other significant lesions | Symptomatic stenosis > 50% of unprotected LMCA or with assessed myocardial ischemia |
| Major exclusion criteria | PCI or CABG of unprotected LMCA in the previous year, need of concomitant cardiac surgery, SYNTAX score ≥33 or life expectancy < 3 years | Previous MI, total occlusion of the left main, Euroscore surgical risk of 8 or more, stroke or transient ischemic attack within 3 months, renal dysfunction or contraindication to antiplatelet therapy | Patients considered too high-risk for PCI or CABG, STEMI < 24 h or life expectancy < 1 year | MI in the previous week, PCI in the previous year, LVEF < 30%, cardiogenic shock, stroke in the previous 6 months, CKD, severe hepatic dysfunction or life expectancy < 1 year | Previous PCI or CABG, acute MI or need for concomitant cardiac surgery |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bajraktari, G.; Zhubi-Bakija, F.; Ndrepepa, G.; Alfonso, F.; Elezi, S.; Rexhaj, Z.; Bytyçi, I.; Bajraktari, A.; Poniku, A.; Henein, M.Y. Long-Term Outcomes of Patients with Unprotected Left Main Coronary Artery Disease Treated with Percutaneous Angioplasty versus Bypass Grafting: A Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2020, 9, 2231. https://doi.org/10.3390/jcm9072231
Bajraktari G, Zhubi-Bakija F, Ndrepepa G, Alfonso F, Elezi S, Rexhaj Z, Bytyçi I, Bajraktari A, Poniku A, Henein MY. Long-Term Outcomes of Patients with Unprotected Left Main Coronary Artery Disease Treated with Percutaneous Angioplasty versus Bypass Grafting: A Meta-Analysis of Randomized Controlled Trials. Journal of Clinical Medicine. 2020; 9(7):2231. https://doi.org/10.3390/jcm9072231
Chicago/Turabian StyleBajraktari, Gani, Fjolla Zhubi-Bakija, Gjin Ndrepepa, Fernando Alfonso, Shpend Elezi, Zarife Rexhaj, Ibadete Bytyçi, Artan Bajraktari, Afrim Poniku, and Michael Y. Henein. 2020. "Long-Term Outcomes of Patients with Unprotected Left Main Coronary Artery Disease Treated with Percutaneous Angioplasty versus Bypass Grafting: A Meta-Analysis of Randomized Controlled Trials" Journal of Clinical Medicine 9, no. 7: 2231. https://doi.org/10.3390/jcm9072231
APA StyleBajraktari, G., Zhubi-Bakija, F., Ndrepepa, G., Alfonso, F., Elezi, S., Rexhaj, Z., Bytyçi, I., Bajraktari, A., Poniku, A., & Henein, M. Y. (2020). Long-Term Outcomes of Patients with Unprotected Left Main Coronary Artery Disease Treated with Percutaneous Angioplasty versus Bypass Grafting: A Meta-Analysis of Randomized Controlled Trials. Journal of Clinical Medicine, 9(7), 2231. https://doi.org/10.3390/jcm9072231








