Pain and Oral-Health-Related Quality of Life in Orthodontic Patients During Initial Therapy with Conventional, Low-Friction, and Lingual Brackets and Aligners (Invisalign): A Prospective Clinical Study
Abstract
1. Introduction
2. Experimental Section
2.1. Ethics Approval and Patient Consent
2.2. Sample Size Calculation and Participants
- Patients between 18 and 40 years of age and with permanent dentition;
- Without previous orthodontic treatment;
- No previous extractions except third molars;
- Dental bone discrepancy between –2 and –6 mm in both arches;
- Good oral health without caries or periodontal disease;
- Skeletal class I or mild classes II and III (ANB 0°–5°) [26].
- Patients with deciduous teeth or in the process of dental replacement;
- Patients in need of orthodontic surgical treatment or dental extractions due to treatment;
- Patients with systemic diseases;
- Patients with medication that influences pain perception (analgesics, antidepressants, and/or anticonvulsants);
- Severe malformations;
- Anatomy of the lingual side that would prevent lingual brackets being cemented in the lingual orthodontic group.
2.3. Study Design
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Participants
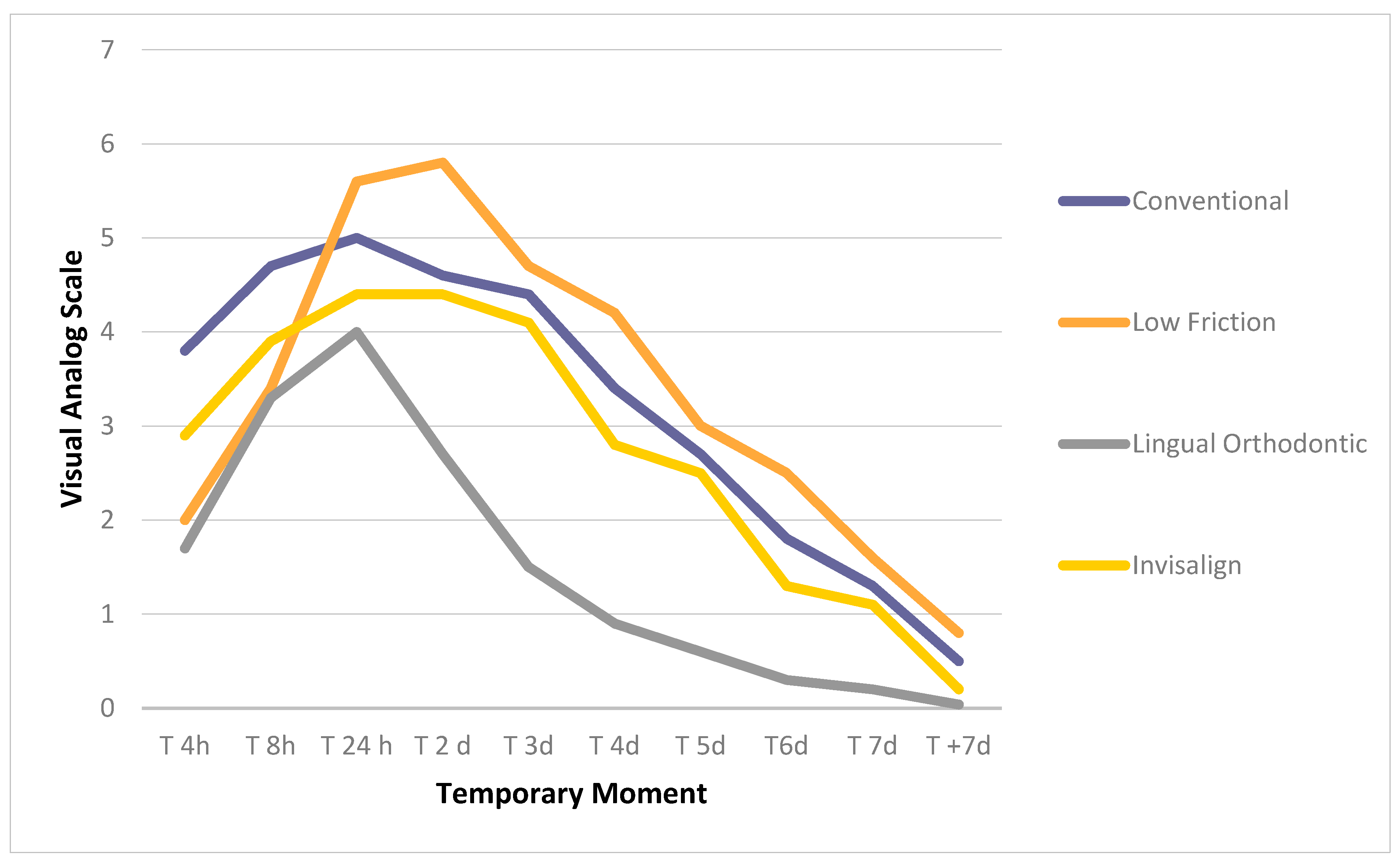
3.2. Pain Analysis
3.3. Analysis of the Quality of Life Related to Oral Health
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sawada, A.; Usui, N.; Shimazaki, K.; Taira, M.; Ono, T. The effects of cognitive behavioral therapy on experimental orthodontic pain. Orthod. Waves 2015, 74, 10–14. [Google Scholar] [CrossRef]
- Krishnan, V. Orthodontic pain: From causes to management--a review. Eur. J. Orthod. 2007, 29, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Bergius, M.; Berggren, U.; Kiliaridis, S. Experience of pain during an orthodontic procedure. Eur. J. Oral Sci. 2002, 110, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Rakhshan, H.; Rakhshan, V. Pain and discomfort perceived during the initial stage of active fixed orthodontic treatment. Saudi Dent. J. 2015, 27, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Lew, K.K. Attitudes and perceptions of adults towards orthodontic treatment in an Asian community. Community Dent. Oral Epidemiol. 1993, 21, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Polat-Ozsoy, O. Pain and Discomfort After Orthodontic Appointments. Semin. Orthod. 2007, 13, 292–300. [Google Scholar] [CrossRef]
- Alarcón, J.A.; Linde, D.; Barbieri, G.; Solano, P.; Caba, O.; Rios-Lugo, M.J.; Sanz, M.; Martin, C. Calcitonin gingival crevicular fluid levels and pain discomfort during early orthodontic tooth movement in young patients. Arch. Oral Boil. 2013, 58, 590–595. [Google Scholar] [CrossRef]
- Johal, A.; Ashari, A.B.; AlAmiri, N.; Fleming, P.S.; Qureshi, U.; Cox, S.; Pandis, N. Pain experience in adults undergoing treatment: A longitudinal evaluation. Angle Orthod. 2018, 88, 292–298. [Google Scholar] [CrossRef]
- Fujiyama, K.; Honjo, T.; Suzuki, M.; Matsuoka, S.; Deguchi, T. Analysis of pain level in cases treated with Invisalign aligner: Comparison with fixed edgewise appliance therapy. Prog. Orthod. 2014, 15, 64. [Google Scholar] [CrossRef]
- Shen, H.; Shao, S.; Zhang, J.; Wang, Z.; Lv, D.; Chen, W.; Svensson, P. Fixed orthodontic appliances cause pain and disturbance in somatosensory function. Eur. J. Oral Sci. 2015, 124, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, M.; Nakajima, R.; Kasai, K. Mechanoreceptors, Nociceptors, and Orthodontic Tooth Movement. Semin. Orthod. 2012, 18, 249–256. [Google Scholar] [CrossRef]
- Scott, P.; Sherriff, M.; DiBiase, A.T.; Cobourne, M.T. Perception of discomfort during initial orthodontic tooth alignment using a self-ligating or conventional bracket system: A randomized clinical trial. Eur. J. Orthod. 2008, 30, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.F.; Moerenhout, R.G. The pain experience and psychological adjustment to orthodontic treatment of preadolescents, adolescents, and adults. Am. J. Orthod. Dentofac. Orthop. 1991, 100, 349–356. [Google Scholar] [CrossRef]
- Miller, K.B.; McGorray, S.P.; Womack, R.; Quintero, J.C.; Perelmuter, M.; Gibson, J.; Dolan, T.A.; Wheeler, T.T. A comparison of treatment impacts between Invisalign aligner and fixed appliance therapy during the first week of treatment. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 302.e1–302.e9. [Google Scholar] [CrossRef]
- Johal, A.; Fleming, P.S.; Al Jawad, F.A. A prospective longitudinal controlled assessment of pain experience and oral health-related quality of life in adolescents undergoing fixed appliance treatment. Orthod. Craniofacial Res. 2014, 17, 178–186. [Google Scholar] [CrossRef]
- Cunningham, S.J.; Hunt, N.P. Quality of Life and Its Importance in Orthodontics. J. Orthod. 2001, 28, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Othman, S.A.; Mansor, N.; Saub, R. Randomized controlled clinical trial of oral health-related quality of life in patients wearing conventional and self-ligating brackets. Korean J. Orthod. 2014, 44, 168–176. [Google Scholar] [CrossRef]
- Zhou, Y.; Zheng, M.; Lin, J.; Wang, Y.; Ni, Z.Y. Self-Ligating Brackets and Their Impact on Oral Health-Related Quality of Life in Chinese Adolescence Patients: A Longitudinal Prospective Study. Sci. World J. 2014, 2014, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Rai, A.; Rozario, J.; Ganeshkar, S. Parametric and nonparametric assessment of speech changes in labial and lingual orthodontics: A prospective study. APOS Trends Orthod. 2013, 3, 99. [Google Scholar] [CrossRef]
- Khattab, T.Z.; Farah, H.; Al-Sabbagh, R.; Hajeer, M.Y.; Haj-Hamed, Y. Speech performance and oral impairments with lingual and labial orthodontic appliances in the first stage of fixed treatment. Angle Orthod. 2012, 83, 519–526. [Google Scholar] [CrossRef]
- Rai, A.K.; Rozario, J.E.; Ganeshkar, S.V. Comparison of speech performance in labial and lingual orthodontic patients: A prospective study. Dent. Res. J. 2014, 11, 663–675. [Google Scholar]
- Pacheco-Pereira, C.; Brandelli, J.; Flores-Mir, C. Patient satisfaction and quality of life changes after Invisalign treatment. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Tecco, S.; D’Attilio, M.; Tetè, S.; Festa, F. Prevalence and type of pain during conventional and self-ligating orthodontic treatment. Eur. J. Orthod. 2009, 31, 380–384. [Google Scholar] [CrossRef]
- Bertl, M.; Onodera, K.; Celar, A. A prospective randomized split-mouth study on pain experience during chairside archwire manipulation in self-ligating and conventional brackets. Angle Orthod. 2013, 83, 292–297. [Google Scholar] [CrossRef] [PubMed]
- Scuzzo, G.; Takemoto, K.; Takemoto, Y.; Takemoto, A.; Lombardo, L. A new lingual straight-wire techique. J. Clin. Orthod. 2010, 44, 114–123. [Google Scholar] [PubMed]
- Steiner, C.C. Cephalometrics for you and me. Am. J. Orthod. 1953, 39, 729–755. [Google Scholar] [CrossRef]
- Iwasaki, L.R.; Freytag, L.E.; Schumacher, C.A.; Walker, M.P.; Williams, K.B. Validation of a modified McGill Pain Questionnaire for orthodontic patients. Angle Orthod. 2013, 83, 906–912. [Google Scholar] [CrossRef]
- Dworkin, R.H.; Turk, D.C.; Trudeau, J.; Benson, C.; Biondi, D.M.; Katz, N.P.; Kim, M. Validation of the Short-Form McGill Pain Questionnaire-2 (SF-MPQ-2) in Acute Low Back Pain. J. Pain 2015, 16, 357–366. [Google Scholar] [CrossRef]
- Otasevic, M.; Naini, F.B.; Gill, D.S.; Lee, R.T. Prospective randomized clinical trial comparing the effects of a masticatory bite wafer and avoidance of hard food on pain associated with initial orthodontic tooth movement. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 6.e9–6.e15. [Google Scholar] [CrossRef]
- Kane, R.L.; Bershadsky, B.; Rockwood, T.; Saleh, K.; Islam, N.C. Visual Analog Scale pain reporting was standardized. J. Clin. Epidemiology 2005, 58, 618–623. [Google Scholar] [CrossRef]
- Slade, G.D. Derivation and validation of a short-form oral health impact profile. Community Dent. Oral Epidemiol. 1997, 25, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Montero-Martín, J.; Bravo-Pérez, M.; Albaladejo-Martínez, A.; Hernández-Martín, L.A.; Rosel-Gallardo, E.M. Validation the Oral Health Impact Profile (OHIP-14sp) for adults in Spain. Med. Oral Patol. Oral Cir. Bucal 2009, 14, 1–7. [Google Scholar]
- Othman, S.A.; Saub, R.; Mansor, N. Changes in the oral health-related quality of life 24 h following insertion of fixed orthodontic appliances. J. Orthod. Sci. 2012, 1, 98–102. [Google Scholar] [CrossRef]
- Chen, M.; Wang, D.-W.; Wu, L.-P. Fixed Orthodontic Appliance Therapy and Its Impact on Oral Health-Related Quality of Life in Chinese Patients. Angle Orthod. 2010, 80, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Abdelrahman, R.S.; Al-Nimri, K.S.; Al Maaitah, E.F. Pain experience during initial alignment with three types of nickel-titanium archwires: A prospective clinical trial. Angle Orthod. 2015, 85, 1021–1026. [Google Scholar] [CrossRef] [PubMed]
- Ambekar, A. Pain and Discomfort Associated With Initial Alignment with Three Different Archwires—A Clinical Study. IOSR J. Dent. Med. Sci. 2014, 13, 47–50. [Google Scholar] [CrossRef]
- Mandall, N.; Lowe, C.; Worthington, H.V.; Sandler, J.; Derwent, S.; Abdi-Oskouei, M.; Ward, S. Which orthodontic archwire sequence? A randomized clinical trial. Eur. J. Orthod. 2006, 28, 561–566. [Google Scholar] [CrossRef]
- Fleming, P.S.; DiBiase, A.T.; Sarri, G.; Lee, R.T. Pain Experience during Initial Alignment with a Self-Ligating and a Conventional Fixed Orthodontic Appliance System. Angle Orthod. 2009, 79, 46–50. [Google Scholar] [CrossRef]
- Lai, T.-T.; Chiou, J.-Y.; Lai, T.-C.; Chen, T.; Wang, H.-Y.; Li, C.-H.; Chen, M.-H. Perceived pain for orthodontic patients with conventional brackets or self-ligating brackets over 1 month period: A single-center, randomized controlled clinical trial. J. Formos. Med. Assoc. 2019, 119, 282–289. [Google Scholar] [CrossRef]
- Revill, S.I.; Robinson, J.O.; Rosén, M.; Hogg, M.I.J. The reliability of a linear analogue for evaluating pain. Anaesthesia 1976, 31, 1191–1198. [Google Scholar] [CrossRef]
- Aitken, R.C. Measurement of feelings using visual analogue scales. Proc. R. Soc. Med. 1969, 62, 989–993. [Google Scholar] [PubMed]
- Wu, A.K.Y.; McGrath, C.P.J.; Wong, R.; Wiechmann, D.; Rabie, A.B.M. A comparison of pain experienced by patients treated with labial and lingual orthodontic appliances. Eur. J. Orthod. 2009, 32, 403–407. [Google Scholar] [CrossRef] [PubMed]
- Long, H.; Zhou, Y.; Pyakurel, U.; Liao, L.; Jian, F.; Xue, J.; Ye, N.; Yang, X.; Wang, Y.; Lai, W. Comparison of adverse effects between lingual and labial orthodontic treatment: A systematic review. Angle Orthod. 2013, 83, 1066–1073. [Google Scholar] [CrossRef] [PubMed]
- Ata-Ali, F.; Ata-Ali, J.; Ferrer-Molina, M.; Cobo, T.; Villafra, F.D.C.; Cobo, J. Adverse effects of lingual and buccal orthodontic techniques: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 820–829. [Google Scholar] [CrossRef]
- Shalish, M.; Cooper-Kazaz, R.; Ivgi, I.; Canetti, L.; Tsur, B.; Bachar, E.; Chaushu, S. Adult Patients’ Adjustability to Orthodontic Appliances. Part I: A Comparison Between Labial, Lingual, and Invisalign™. Eur. J. Orthod. 2012, 34, 724–730. [Google Scholar] [CrossRef]
- Caniklioglu, C.; Oztürk, Y. Patient discomfort: A comparison between lingual and labial fixed appliances. Angle Orthod. 2005, 75, 86–91. [Google Scholar]
- White, D.W.; Julien, K.C.; Jacob, H.; Campbell, P.M.; Buschang, P.H. Discomfort associated with Invisalign and traditional brackets: A randomized, prospective trial. Angle Orthod. 2017, 87, 801–808. [Google Scholar] [CrossRef]
- Cioffi, I.; Piccolo, A.; Tagliaferri, R.; Paduano, S.; Galeotti, A.; Martina, R. Pain perception following first orthodontic archwire placement--thermoelastic vs. superelastic alloys: A randomized controlled trial. Quintessence Int. 2012, 43, 61–69. [Google Scholar]
- Jian, F.; Lai, W.; Furness, S.; McIntyre, G.; Millett, D.T.; Hickman, J.; Wang, Y. Initial arch wires for tooth alignment during orthodontic treatment with fixed appliances. Cochrane Database Syst. Rev. 2013, 2013, CD007859. [Google Scholar] [CrossRef]
- Ong, E.; Ho, C.; Miles, P.E.; Lloyd, T.A.; Drage, N.; Cronin, A.J. Alignment efficiency and discomfort of three orthodontic archwire sequences: A randomized clinical trial. J. Orthod. 2011, 38, 32–39. [Google Scholar] [CrossRef]
- Lai, T.-T.; Chiou, J.-Y.; Lai, T.-C.; Chen, T.; Chen, M.-H. Oral health-related quality of life in orthodontic patients during initial therapy with conventional brackets or self-ligating brackets. J. Dent. Sci. 2017, 12, 161–172. [Google Scholar] [CrossRef] [PubMed]
- Curto, A.; Albaladejo, A.; Montero, J.; Alvarado, A. Influence of a Lubricating Gel (Orthospeed®) on Pain and Oral Health-Related Quality of Life in Orthodontic Patients during Initial Therapy with Conventional and Low-Friction Brackets: A Prospective Randomized Clinical Trial. J. Clin. Med. 2020, 9, 1474. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, S.N.; Gölz, L.; Jäger, A.; Eliades, T.; Bourauel, C. Lingual vs. labial fixed orthodontic appliances: Systematic review and meta-analysis of treatment effects. Eur. J. Oral Sci. 2016, 124, 105–118. [Google Scholar] [CrossRef] [PubMed]
- Azaripour, A.; Weusmann, J.; Mahmoodi, B.; Peppas, D.; Gerhold-Ay, A.; Van Noorden, C.J.F.; Willershausen, B. Braces versus Invisalign®: Gingival parameters and patients’ satisfaction during treatment: A cross-sectional study. BMC Oral Health 2015, 15, 69. [Google Scholar] [CrossRef] [PubMed]
- Diddige, R.; Negi, G.; Kiran, K.; Chitra, P. Comparision of pain levels in patients treated with 3 different orthodontic appliances – a randomized trial. Med. Pharm. Rep. 2020, 93, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Slater, R.D. Speech and discomfort during lingual orthodontic treatment. J. Orthod. 2013, 40, 34–37. [Google Scholar] [CrossRef]
| Conventional Brackets (n = 30) | Low-Friction Brackets (n = 30) | Lingual Brackets (n = 30) | Invisalign (n = 30) | |||
|---|---|---|---|---|---|---|
| Age (Years) | Mean | 24.7 | 28 | 33.8 | 33.4 | |
| SD | 4.1 | 9.7 | 8.2 | 5.1 | ||
| Sex | Men | N | 13 | 12 | 13 | 16 |
| % | 43.3 | 40 | 43.3 | 53.3 | ||
| Women | N | 17 | 18 | 17 | 14 | |
| % | 56.7 | 60 | 56.7 | 46.6 | ||
| Dental Bone Discrepancy | Upper | Mean | −3.1 | −3.1 | −3.0 | −2.6 |
| SD. | 1.0 | 0.7 | 1.6 | 1.6 | ||
| Lower | Mean | −3.3 | −2.7 | −3.4 | −2.6 | |
| SD. | 1.3 | 1.2 | 1.5 | 1.7 | ||
| Time | Conventional Brackets (n = 30) | Low-Friction Brackets (n = 30) | Lingual Brackets (n = 30) | Invisalign (n = 30) | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| 4 h (T4h) ** | 3.8 A | 2.3 | 2.0 B,C | 1.9 | 1.7 C | 2.3 | 2.9 A,B,C | 2.5 |
| 8 h (T8h) | 4.7 | 2.3 | 3.4 | 2.2 | 3.3 | 1.9 | 3.9 | 2.3 |
| 24 h (T1) * | 5.0 a,c | 2.7 | 5.6 a | 2.0 | 4 c | 1.9 | 4.4 a,c | 2.1 |
| 2 days (T2) ** | 4.6 A | 2.5 | 5.8 A | 1.9 | 2.7 C | 2.1 | 4.4 A | 2.4 |
| 3 days (T3) ** | 4.4 A | 3.0 | 4.7 A | 2.3 | 1.5 C | 1.7 | 4.1 A | 2.5 |
| 4 days (T4) ** | 3.4 A | 2.7 | 4.2 A | 2.4 | 0.9 C | 1.3 | 2.8 B | 2.1 |
| 5 days (T5) ** | 2.7 A | 2.4 | 3.0 A | 2.5 | 0.6 C | 1.2 | 2.5 A | 1.9 |
| 6 days (T6) ** | 1.8 A | 1.9 | 2.5 A | 2.2 | 0.3 C | 0.9 | 1.3 B | 1.7 |
| 7 days (T7) ** | 1.3 A,B | 1.6 | 1.6 B | 2.1 | 0.2 A | 0.8 | 1.1 A,B | 1.6 |
| Domains | Conventional Brackets (n = 30) | Low-Friction Brackets (n = 30) | Lingual Brackets (n = 30) | Invisalign (n = 30) | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Functional limitation | 0.4 | 0.6 | 0.6 | 0.8 | 0.3 | 0.5 | 0.5 | 0.7 |
| ANOVA F: 1.5; fd: 3; p-value: 0.22 | ||||||||
| Physical pain ** | 1.6 A | 0.6 | 1.3 A,C | 0.8 | 0.8 C | 0.8 | 0.9 A,C | 0.7 |
| ANOVA F: 7.7; fd: 3; p-value: 0.00 | ||||||||
| Psychological discomfort ** | 0.8 A | 0.9 | 1.3 B | 0.8 | 0.0 C | 0.2 | 0.2 C,D | 0.4 |
| ANOVA F: 24.4; fd: 3; p-value: 0.00 | ||||||||
| Physical disability ** | 0.6 A | 0.7 | 2 B | 0.5 | 0.1 B | 0.4 | 0.0 B | 0.2 |
| ANOVA F: 9.7; fd: 3; p-value: 0.00 | ||||||||
| Psychological disability ** | 0.3 A,C | 0.5 | 0.8 B | 0.9 | 0.0 C | 0.0 | 0.1 A,C,D | 0.4 |
| ANOVA F: 12.5; fd: 3; p-value: 0.00 | ||||||||
| Social disability * | 0.1 a,c | 0.4 | 3 a | 0.5 | 0.0 c | 0.0 | 0.1 a,c | 0.7 |
| ANOVA F: 3.1; fd: 3; p-value: 0.03 | ||||||||
| Handicap | 0.0 | 0.0 | 0.1 | 0.2 | 0.0 | 0.0 | 0.1 | 0.4 |
| ANOVA F: 0.7; fd: 3; p-value: 0.53 | ||||||||
| Total OHIP ** | 3.8 A | 2.1 | 4.5 A,B | 2.8 | 1.3 C | 1.2 | 1.7 C,D | 1.9 |
| ANOVA F: 16; fd: 3; p-value: 0.00 | ||||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antonio-Zancajo, L.; Montero, J.; Albaladejo, A.; Oteo-Calatayud, M.D.; Alvarado-Lorenzo, A. Pain and Oral-Health-Related Quality of Life in Orthodontic Patients During Initial Therapy with Conventional, Low-Friction, and Lingual Brackets and Aligners (Invisalign): A Prospective Clinical Study. J. Clin. Med. 2020, 9, 2088. https://doi.org/10.3390/jcm9072088
Antonio-Zancajo L, Montero J, Albaladejo A, Oteo-Calatayud MD, Alvarado-Lorenzo A. Pain and Oral-Health-Related Quality of Life in Orthodontic Patients During Initial Therapy with Conventional, Low-Friction, and Lingual Brackets and Aligners (Invisalign): A Prospective Clinical Study. Journal of Clinical Medicine. 2020; 9(7):2088. https://doi.org/10.3390/jcm9072088
Chicago/Turabian StyleAntonio-Zancajo, Laura, Javier Montero, Alberto Albaladejo, Maria Dolores Oteo-Calatayud, and Alfonso Alvarado-Lorenzo. 2020. "Pain and Oral-Health-Related Quality of Life in Orthodontic Patients During Initial Therapy with Conventional, Low-Friction, and Lingual Brackets and Aligners (Invisalign): A Prospective Clinical Study" Journal of Clinical Medicine 9, no. 7: 2088. https://doi.org/10.3390/jcm9072088
APA StyleAntonio-Zancajo, L., Montero, J., Albaladejo, A., Oteo-Calatayud, M. D., & Alvarado-Lorenzo, A. (2020). Pain and Oral-Health-Related Quality of Life in Orthodontic Patients During Initial Therapy with Conventional, Low-Friction, and Lingual Brackets and Aligners (Invisalign): A Prospective Clinical Study. Journal of Clinical Medicine, 9(7), 2088. https://doi.org/10.3390/jcm9072088







