Inter-Hospital Transfer after Return of Spontaneous Circulation Shows no Correlation with Neurological Outcomes in Cardiac Arrest Patients Undergoing Targeted Temperature Management in Cardiac Arrest Centers
Abstract
:1. Introduction
2. Methods
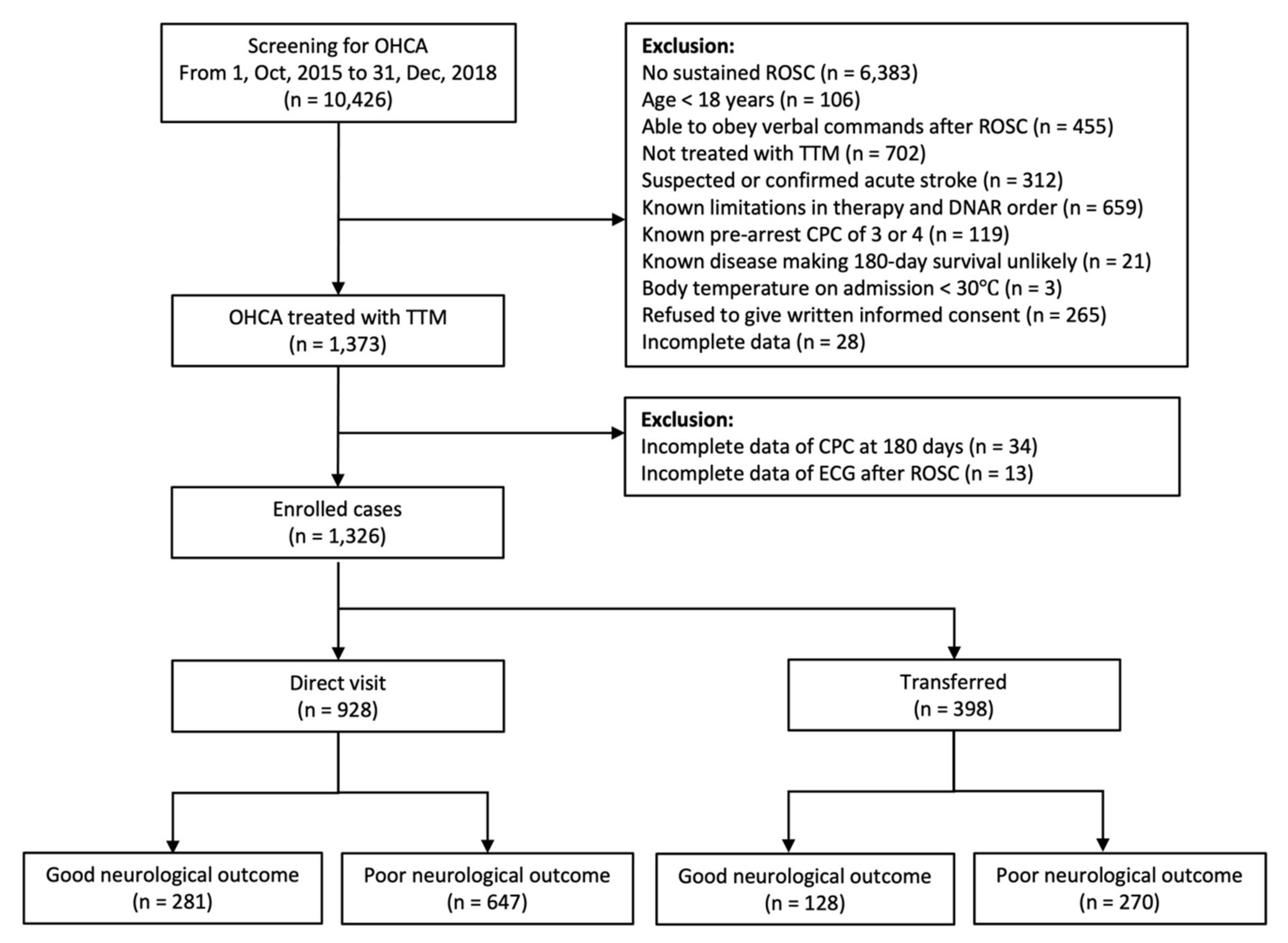
2.1. Study Design and Population
2.2. Variables
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics of the Patients
3.2. Independent Prognostic Factors for Poor Neurological Outcomes
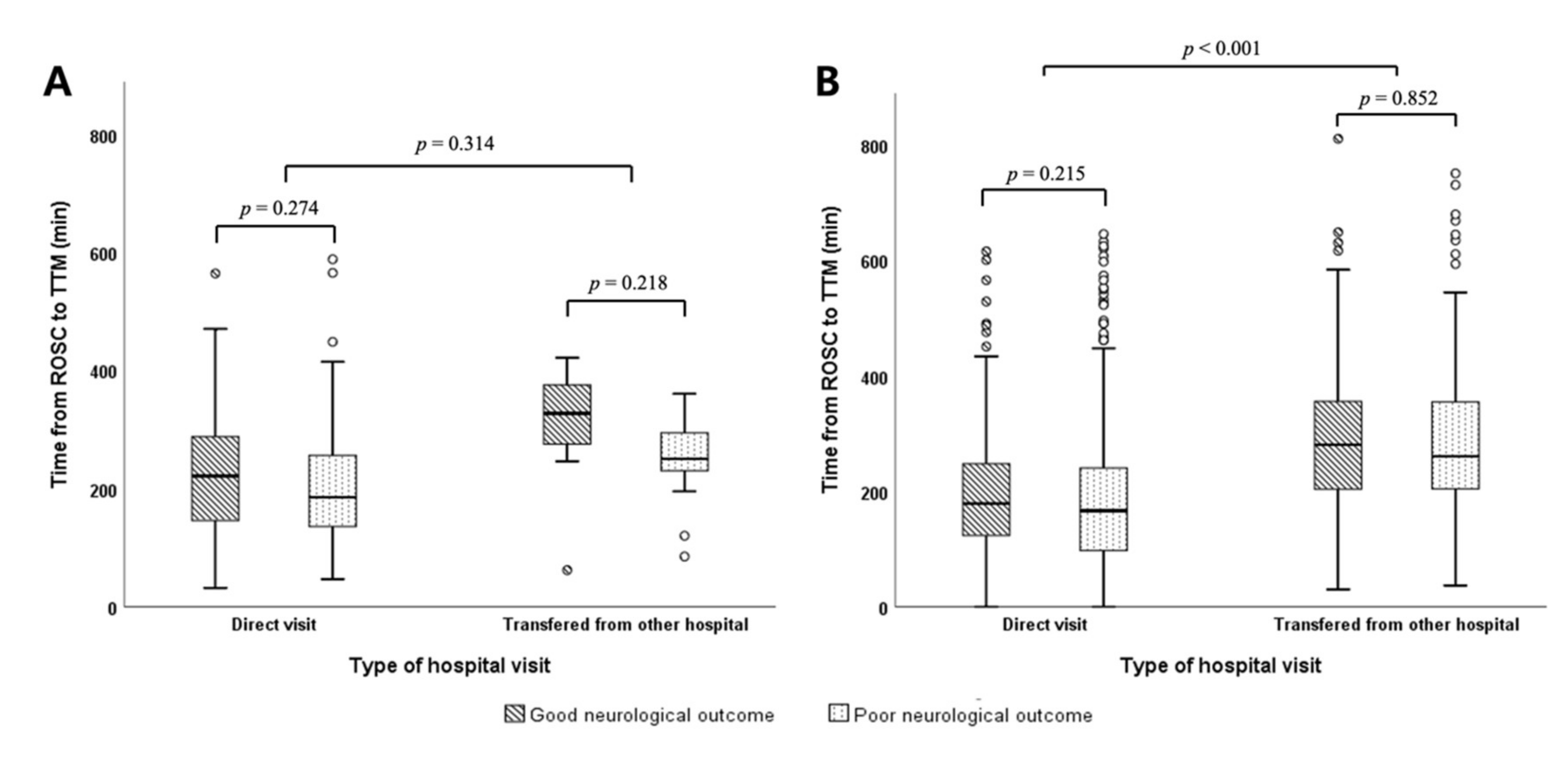
3.3. Time from ROSC to the Induction of TTM According to the Type of Hospital Visit and Neurological Outcomes
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Callaway, C.W.; Donnino, M.W.; Fink, E.L.; Geocadin, R.G.; Golan, E.; Kern, K.B.; Leary, M.; Meurer, W.J.; Peberdy, M.A.; Thompson, T.M.; et al. Part 8: Post-Cardiac Arrest Care: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015, 132 (Suppl. 2), S465–S482. [Google Scholar] [CrossRef] [Green Version]
- Elmer, J.; Rittenberger, J.C.; Coppler, P.J.; Guyette, F.X.; Doshi, A.A.; Callaway, C.W.; Pittsburgh Post-Cardiac Arrest Service. Long-term survival benefit from treatment at a specialty center after cardiac arrest. Resuscitation 2016, 108, 48–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patterson, T.; Perkins, A.; Perkins, G.D.; Clayton, T.; Evans, R.; Nguyen, H.; Wilson, K.; Whitbread, M.; Hughes, J.; Fothergill, R.T.; et al. Rationale and design of: A Randomized tRial of Expedited transfer to a cardiac arrest center for non-ST elevation out-of-hospital cardiac arrest: The ARREST randomized controlled trial. Am. Heart J. 2018, 204, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Patterson, T.; Perkins, G.D.; Joseph, J.; Wilson, K.; Van Dyck, L.; Robertson, S.; Nguyen, H.; McConkey, H.; Whitbread, M.; Fothergill, R.; et al. A Randomised tRial of Expedited transfer to a cardiac arrest centre for non-ST elevation ventricular fibrillation out-of-hospital cardiac arrest: The ARREST pilot randomised trial. Resuscitation 2017, 115, 185–191. [Google Scholar] [CrossRef] [Green Version]
- Peberdy, M.A.; Callaway, C.W.; Neumar, R.W.; Geocadin, R.G.; Zimmerman, J.L.; Donnino, M.; Gabrielli, A.; Silvers, S.M.; Zaritsky, A.L.; Merchant, R.; et al. Part 9: Post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010, 122 (Suppl. 3), S768–S786. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kronick, S.L.; Kurz, M.C.; Lin, S.; Edelson, D.P.; Berg, R.A.; Billi, J.E.; Cabanas, J.G.; Cone, D.C.; Diercks, D.B.; Foster, J.J.; et al. Part 4: Systems of Care and Continuous Quality Improvement: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015, 132 (Suppl. 2), S397–S413. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.H.; Lee, S.C.; Shin, S.D.; Song, K.J.; Hong, K.J.; Ro, Y.S. Interhospital transfer in low-volume and high-volume emergency departments and survival outcomes after out-of-hospital cardiac arrest: A nationwide observational study and propensity score-matched analysis. Resuscitation 2019, 139, 41–48. [Google Scholar] [CrossRef]
- Perkins, G.D.; Jacobs, I.G.; Nadkarni, V.M.; Berg, R.A.; Bhanji, F.; Biarent, D.; Bossaert, L.L.; Brett, S.J.; Chamberlain, D.; de Caen, A.R.; et al. Cardiac Arrest and Cardiopulmonary Resuscitation Outcome Reports: Update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: A Statement for Healthcare Professionals from a Task Force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Resuscitation 2015, 96, 328–340. [Google Scholar]
- Hill, A.D.; Vingilis, E.; Martin, C.M.; Hartford, K.; Speechley, K.N. Interhospital transfer of critically ill patients: Demographic and outcomes comparison with nontransferred intensive care unit patients. J. Crit. Care 2007, 22, 290–295. [Google Scholar] [CrossRef]
- Salcido, D.D.; Stephenson, A.M.; Condle, J.P.; Callaway, C.W.; Menegazzi, J.J. Incidence of rearrest after return of spontaneous circulation in out-of-hospital cardiac arrest. Prehosp. Emerg. Care 2010, 14, 413–418. [Google Scholar] [CrossRef] [Green Version]
- Bosson, N.; Kaji, A.H.; Niemann, J.T.; Eckstein, M.; Rashi, P.; Tadeo, R.; Gorospe, D.; Sung, G.; French, W.J.; Shavelle, D.; et al. Survival and neurologic outcome after out-of-hospital cardiac arrest: Results one year after regionalization of post-cardiac arrest care in a large metropolitan area. Prehosp. Emerg. Care 2014, 18, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Kajino, K.; Iwami, T.; Daya, M.; Nishiuchi, T.; Hayashi, Y.; Kitamura, T.; Irisawa, T.; Sakai, T.; Kuwagata, Y.; Hiraide, A.; et al. Impact of transport to critical care medical centers on outcomes after out-of-hospital cardiac arrest. Resuscitation 2010, 81, 549–554. [Google Scholar] [CrossRef] [PubMed]
- Kern, K.B. Cardiac receiving centers: Beyond hypothermia. Curr. Opin. Crit. Care 2012, 18, 246–250. [Google Scholar] [CrossRef] [PubMed]
- Noc, M.; Radsel, P. Urgent invasive coronary strategy in patients with sudden cardiac arrest. Curr. Opin. Crit. Care 2008, 14, 287–291. [Google Scholar] [CrossRef] [PubMed]
- Ting, H.H.; Rihal, C.S.; Gersh, B.J.; Haro, L.H.; Bjerke, C.M.; Lennon, R.J.; Lim, C.C.; Bresnahan, J.F.; Jaffe, A.S.; Holmes, D.R.; et al. Regional systems of care to optimize timeliness of reperfusion therapy for ST-elevation myocardial infarction: The Mayo Clinic STEMI Protocol. Circulation 2007, 116, 729–736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Acker, J.E., 3rd; Pancioli, A.M.; Crocco, T.J.; Eckstein, M.K.; Jauch, E.C.; Larrabee, H.; Meltzer, N.M.; Mergendahl, W.C.; Munn, J.W.; Prentiss, S.M.; et al. Implementation strategies for emergency medical services within stroke systems of care: A policy statement from the American Heart Association/American Stroke Association Expert Panel on Emergency Medical Services Systems and the Stroke Council. Stroke 2007, 38, 3097–3115. [Google Scholar] [CrossRef]
- Nolan, J.P.; Lyon, R.M.; Sasson, C.; Rossetti, A.O.; Lansky, A.J.; Fox, K.A.; Meier, P. Advances in the hospital management of patients following an out of hospital cardiac arrest. Heart 2012, 98, 1201–1206. [Google Scholar] [CrossRef]
- Sunde, K.; Pytte, M.; Jacobsen, D.; Mangschau, A.; Jensen, L.P.; Smedsrud, C.; Draegni, T.; Steen, P.A. Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation 2007, 73, 29–39. [Google Scholar] [CrossRef]
- Spaite, D.W.; Bobrow, B.J.; Stolz, U.; Berg, R.A.; Sanders, A.B.; Kern, K.B.; Chikani, V.; Humble, W.; Mullins, T.; Stapczynski, J.S.; et al. Statewide regionalization of postarrest care for out-of-hospital cardiac arrest: Association with survival and neurologic outcome. Ann. Emerg. Med. 2014, 64, 496–506. [Google Scholar] [CrossRef]
- Gorjup, V.; Noc, M.; Radsel, P. Invasive strategy in patients with resuscitated cardiac arrest and ST elevation myocardial infarction. World J. Cardiol. 2014, 6, 444–448. [Google Scholar] [CrossRef]
- Noc, M.; Fajadet, J.; Lassen, J.F.; Kala, P.; MacCarthy, P.; Olivecrona, G.K.; Windecker, S.; Spaulding, C.; European association of Percutaneous Cardiovascular Interventions; Stent for Life Initiative. Invasive coronary treatment strategies for out-of-hospital cardiac arrest: A consensus statement from the European association for percutaneous cardiovascular interventions (EAPCI)/stent for life (SFL) groups. EuroIntervention 2014, 10, 31–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Direct Visit (n = 928) | Transferred (n = 398) | p-Value | |
|---|---|---|---|
| Sex | 0.996 | ||
| Male | 660 (71.7) | 283 (71.1) | |
| Female | 268 (28.9) | 115 (28.9) | |
| Age (year) | 58.02 ± 15.81 | 57.78 ± 15.57 | 0.797 |
| Pre-arrest CPC | 0.678 | ||
| CPC1 | 818 (88.1) | 354 (88.9) | |
| CPC2 | 110 (11.9) | 44 (11.1) | |
| Cause of arrest | 0.007 | ||
| Cardiac origin | 597 (64.3) | 225 (56.5) | |
| Non-cardiac origin | 331 (35.7) | 173 (43.5) | |
| Witness | 0.001 | ||
| Yes | 670 (72.2) | 248 (62.3) | |
| No | 251 (27.0) | 144 (36.2) | |
| Unknown | 7 (0.8) | 6 (1.5) | |
| Bystander CPR | 0.001 | ||
| Yes | 577 (62.2) | 239 (60.1) | |
| No | 346 (37.3) | 147 (36.9) | |
| Unknown | 5 (0.5) | 12 (3.0) | |
| ECG rhythm in EMS | < 0.001 | ||
| Shockable | 334 (36.0) | 110 (27.6) | |
| Non-shockable | 523 (56.4) | 194 (48.7) | |
| Unknown | 71 (7.7) | 94 (23.6) | |
| EMS defibrillation | < 0.001 | ||
| Yes | 364 (39.2) | 117 (29.4) | |
| No | 411 (44.3) | 223 (56.0) | |
| Unknown | 153 (16.5) | 58 (14.6) | |
| Down time (min) | 32.59 ± 20.95 | 32.45 ± 19.19 | 0.908 |
| ECG rhythm in the ED | < 0.001 | ||
| Shockable | 79 (8.5) | 34 (8.5) | |
| Non-shockable | 545 (58.7) | 213 (53.5) | |
| Prehospital ROSC | 293 (31.6) | 118 (29.6) | |
| Unknown | 11 (1.2) | 33 (8.3) | |
| ED defibrillation | 0.81 | ||
| Yes | 166 (17.9) | 69 (17.3) | |
| No | 762 (82.1) | 329 (82.7) | |
| GCS score after ROSC | 0.035 | ||
| ≤8 | 901 (97.1) | 376 (94.5) | |
| >8 | 7 (0.8) | 3 (0.8) | |
| Unknown | 20 (2.2) | 19 (4.8) | |
| Pupillary light reflex | 0.115 | ||
| Yes | 422 (45.5) | 203 (51.0) | |
| No | 499 (53.8) | 194 (48.7) | |
| Unknown | 7 (0.8) | 1 (0.3) | |
| Corneal reflex | 0.238 | ||
| Yes | 230 (24.8) | 85 (21.4) | |
| No | 591 (63.7) | 257 (64.6) | |
| Unknown | 107 (11.5) | 56 (14.1) | |
| ECG result after ROSC | < 0.001 | ||
| ST elevation | 123 (13.3) | 29 (6.5) | |
| Non-ST elevation | 805 (86.7) | 372 (93.5) | |
| CAG within 24 h | 0.003 | ||
| Yes | 200 (21.6) | 116 (29.1) | |
| No | 728 (78.4) | 282 (70.9) | |
| Lactate (mmol/L) | 10.47 ± 4.94 | 8.10 ± 5.34 | < 0.001 |
| MAP after ROSC (mmHg) | 93.61 ± 31.74 | 88.70 ± 30.41 | 0.011 |
| Time from ROSC to TTM induction (min) | 205.24 ± 158.56 | 298.42 ± 157.44 | < 0.001 |
| Target of TTM (°C) | 0.594 | ||
| ≤34 | 727 (78.3) | 317 (79.6) | |
| >34 | 201 (21.7) | 81 (20.4) | |
| Time from ROSC to the achievement of the target temperature (min) | 423.65 ± 301.33 | 481.10 ± 245.19 | < 0.001 |
| Highest SOFA score in 7 days | 12.40 ± 3.68 | 12.36 ± 3.56 | 0.863 |
| Neurological outcome after 6 months | 0.497 | ||
| Good (CPC 1-2) | 281 (30.3) | 128 (32.2) | |
| Poor (CPC 3-5) | 647 (69.7) | 270 (67.8) |
| Good Neurological Outcomes | Poor Neurological Outcomes | p-Value | |
|---|---|---|---|
| (n = 409) | (n = 917) | ||
| Sex | < 0.001 | ||
| Male | 318 (77.8) | 625 (68.2) | |
| Female | 91 (22.2) | 292 (31.8) | |
| Age (year) | 52.75 ± 14.60 | 60.26 ± 15.68 | < 0.001 |
| Pre-arrest CPC | < 0.001 | ||
| CPC1 | 397 (97.1) | 775 (84.5) | |
| CPC2 | 12 (2.9) | 142 (15.5) | |
| Cause of arrest | < 0.001 | ||
| Cardiac origin | 360 (88.0) | 462 (50.4) | |
| Non-cardiac origin | 49 (12.0) | 455 (49.6) | |
| Type of ED visit | 0.497 | ||
| Direct visit | 281 (68.7) | 647 (70.6) | |
| Transferred | 128 (31.3) | 270 (29.4) | |
| Witness | < 0.001 | ||
| Yes | 343 (83.9) | 575 (62.7) | |
| No | 65 (15.9) | 330 (36.0) | |
| Unknown | 1 (0.2) | 12 (1.3) | |
| Bystander CPR | 0.004 | ||
| Yes | 278 (68.0) | 538 (58.7) | |
| No | 125 (30.6) | 368 (40.1) | |
| Unknown | 6 (1.5) | 11 (1.2) | |
| ECG rhythm in EMS | < 0.001 | ||
| Shockable | 286 (69.9) | 158 (17.2) | |
| Non-shockable | 74 (18.1) | 643 (70.1) | |
| Unknown | 49 (12.0) | 116 (12.6) | |
| EMS defibrillation | < 0.001 | ||
| Yes | 284 (69.4) | 197 (21.5) | |
| No | 76 (18.6) | 558 (60.9) | |
| Unknown | 49 (12.0) | 162 (17.7) | |
| Down time (min) | 21.73 ± 16.86 | 37.37 ± 20.04 | < 0.001 |
| ECG rhythm in the ED | < 0.001 | ||
| Shockable | 57 (13.9) | 56 (6.1) | |
| Non-shockable | 64 (15.6) | 694 (75.7) | |
| Prehospital ROSC | 279 (68.2) | 132 (14.4) | |
| Unknown | 9 (2.2) | 35 (3.8) | |
| ED defibrillation | 0.482 | ||
| Yes | 77 (18.8) | 158 (17.2) | |
| No | 332 (81.2) | 759 (82.8) | |
| GCS score after ROSC | < 0.001 | ||
| ≤8 | 383 (93.6) | 894 (97.5) | |
| >8 | 9 (2.2) | 1 (0.1) | |
| Unknown | 17 (4.2) | 22 (2.4) | |
| Pupillary light reflex | < 0.001 | ||
| Yes | 334 (81.7) | 291 (31.7) | |
| No | 74 (18.1) | 619 (67.5) | |
| Unknown | 1 (0.2) | 7 (0.8) | |
| Corneal reflex | < 0.001 | ||
| Yes | 204 (49.9) | 111 (12.1) | |
| No | 130 (31.8) | 718 (78.3) | |
| Unknown | 75 (18.3) | 88 (9.6) | |
| ECG result after ROSC | < 0.001 | ||
| ST elevation | 159 (38.9) | 157 (17.1) | |
| Non-ST elevation | 250 (61.1) | 760 (82.9) | |
| CAG within 24 h | < 0.001 | ||
| Yes | 159 (38.9) | 157 (17.1) | |
| No | 250 (61.1) | 760 (82.9) | |
| Lactate (mmol/L) | 7.92 ± 5.29 | 10.56 ± 4.92 | < 0.001 |
| MAP after ROSC (mmHg) | 100.95 ± 30.84 | 88.30 ± 30.91 | < 0.001 |
| Time from ROSC to TTM induction (min) | 241.04 ± 150.45 | 229.72 ± 169.42 | 0.245 |
| Target of TTM (°C) | 0.882 | ||
| ≤34 | 321 (78.55) | 723 (78.8) | |
| >34 | 88 (21.5) | 194 (21.2) | |
| Time from ROSC to the achievement of the target temperature (min) | 510.83 ± 290.96 | 409.47 ± 279.06 | < 0.001 |
| Highest SOFA score in 7 days | 9.86 ± 3.05 | 13.52 ± 3.30 | < 0.001 |
| Odds Ratio | 95% CI | p-Value | |
|---|---|---|---|
| Age (year) | 1.044 | 1.028–1.061 | < 0.001 |
| Transferred (vs. direct visit) | 0.85 | 0.508–1.422 | 0.536 |
| Non-cardiac origin (vs. cardiac origin) | 3.297 | 1.792–6.068 | < 0.001 |
| Non-shockable rhythm in EMS (vs. shockable) | 6.098 | 2.569–14.472 | < 0.001 |
| Down time (min) | 1.042 | 1.025–1.059 | 0.001 |
| Non-shockable rhythm in the ED (vs. shockable) | 3.082 | 1.452–6.544 | 0.003 |
| No pupillary reflex | 1.95 | 1.186–3.206 | 0.008 |
| No corneal reflex | 3.442 | 2.067–5.733 | < 0.001 |
| CAG within 24 h | 1.135 | 0.677–1.903 | 0.63 |
| MAP after ROSC (mmHg) | 0.987 | 0.980–0.994 | < 0.001 |
| Highest SOFA score in 7 days | 1.192 | 1.111–1.278 | < 0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, Y.H.; Lee, D.H.; Oh, J.H.; Min, J.H.; Jang, T.C.; Kim, W.Y.; Jeong, W.J.; You, J.S., on behalf of the Korean Hypothermia Network Investigators. Inter-Hospital Transfer after Return of Spontaneous Circulation Shows no Correlation with Neurological Outcomes in Cardiac Arrest Patients Undergoing Targeted Temperature Management in Cardiac Arrest Centers. J. Clin. Med. 2020, 9, 1979. https://doi.org/10.3390/jcm9061979
Choi YH, Lee DH, Oh JH, Min JH, Jang TC, Kim WY, Jeong WJ, You JS on behalf of the Korean Hypothermia Network Investigators. Inter-Hospital Transfer after Return of Spontaneous Circulation Shows no Correlation with Neurological Outcomes in Cardiac Arrest Patients Undergoing Targeted Temperature Management in Cardiac Arrest Centers. Journal of Clinical Medicine. 2020; 9(6):1979. https://doi.org/10.3390/jcm9061979
Chicago/Turabian StyleChoi, Yoon Hee, Dong Hoon Lee, Je Hyeok Oh, Jin Hong Min, Tae Chang Jang, Won Young Kim, Won Jung Jeong, and Je Sung You on behalf of the Korean Hypothermia Network Investigators. 2020. "Inter-Hospital Transfer after Return of Spontaneous Circulation Shows no Correlation with Neurological Outcomes in Cardiac Arrest Patients Undergoing Targeted Temperature Management in Cardiac Arrest Centers" Journal of Clinical Medicine 9, no. 6: 1979. https://doi.org/10.3390/jcm9061979
APA StyleChoi, Y. H., Lee, D. H., Oh, J. H., Min, J. H., Jang, T. C., Kim, W. Y., Jeong, W. J., & You, J. S., on behalf of the Korean Hypothermia Network Investigators. (2020). Inter-Hospital Transfer after Return of Spontaneous Circulation Shows no Correlation with Neurological Outcomes in Cardiac Arrest Patients Undergoing Targeted Temperature Management in Cardiac Arrest Centers. Journal of Clinical Medicine, 9(6), 1979. https://doi.org/10.3390/jcm9061979






