Trends and between-Physician Variation in Laboratory Testing: A Retrospective Longitudinal Study in General Practice
Abstract
1. Introduction
2. Experimental Section
2.1. Study Design, Setting, and Participants
2.2. Data Preparation and Selection
2.3. Objectives
2.4. Statistical Analysis
3. Results
3.1. Selection Process
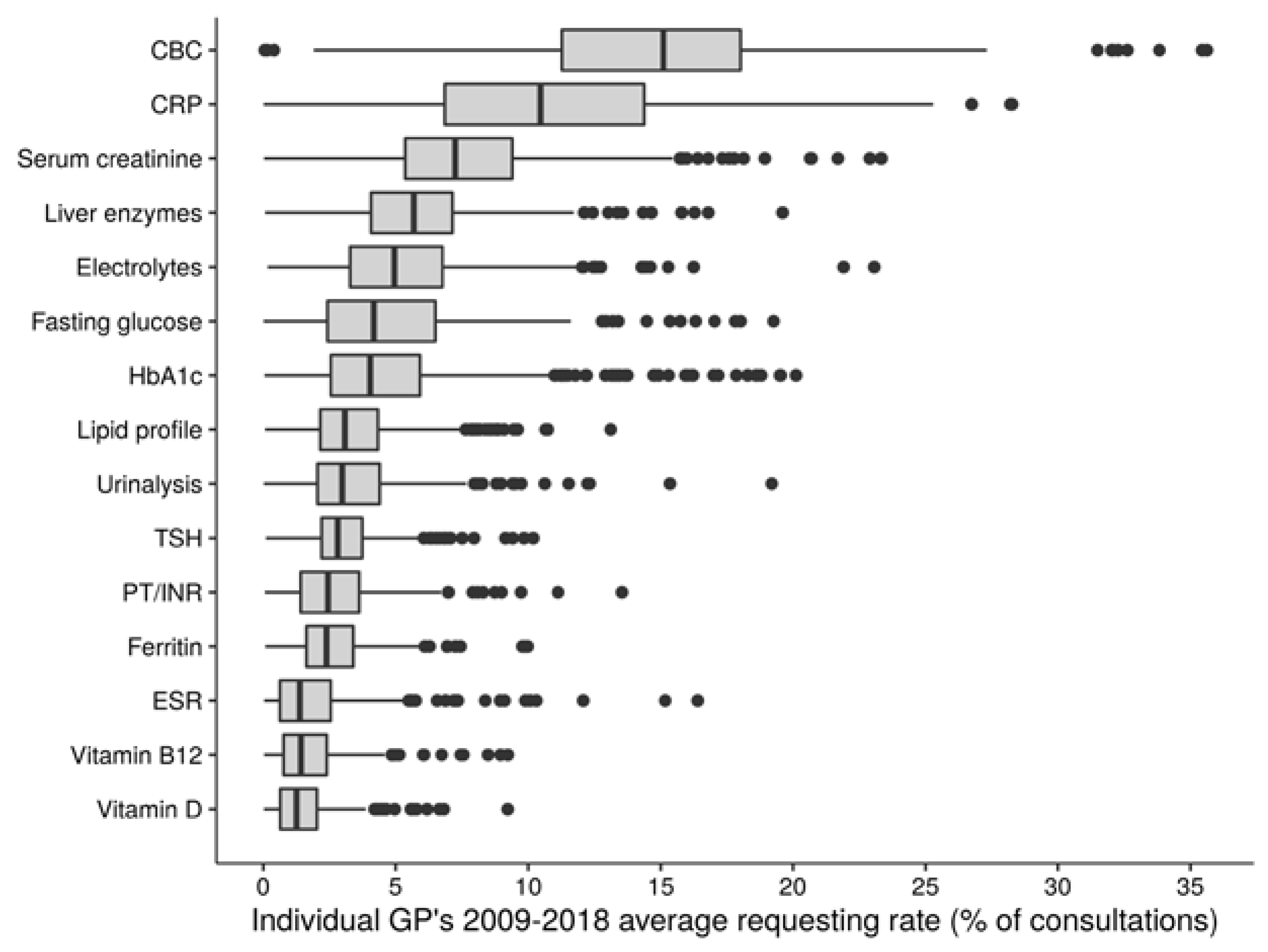
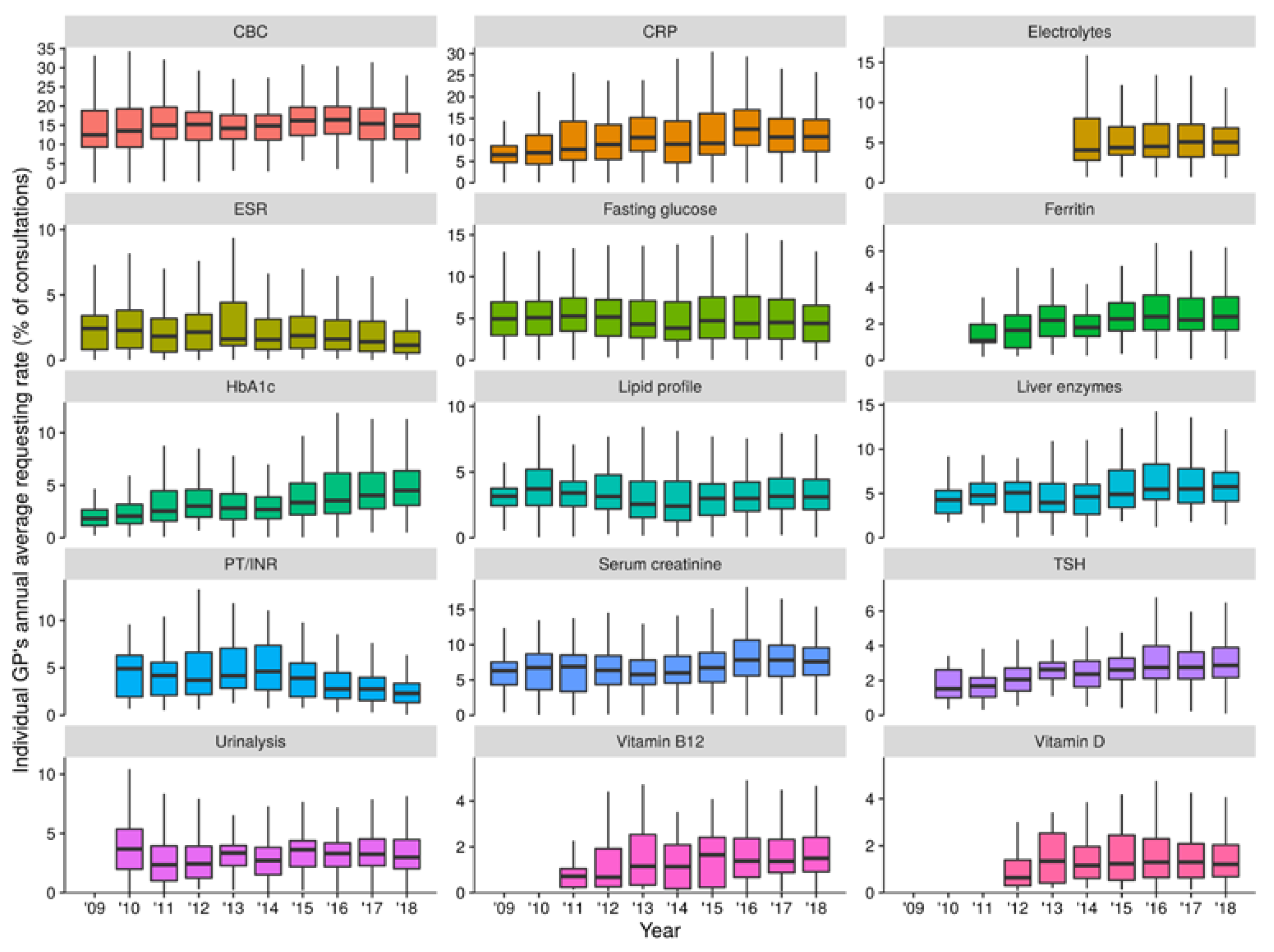
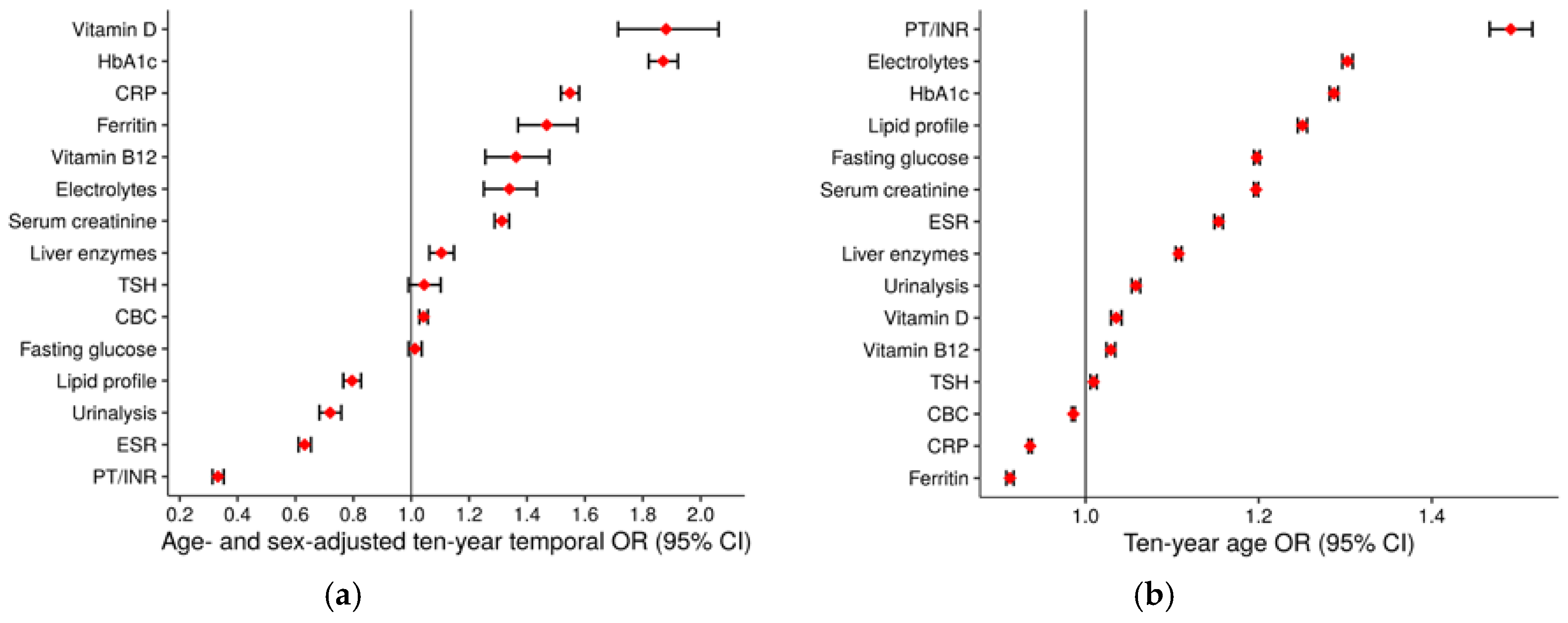
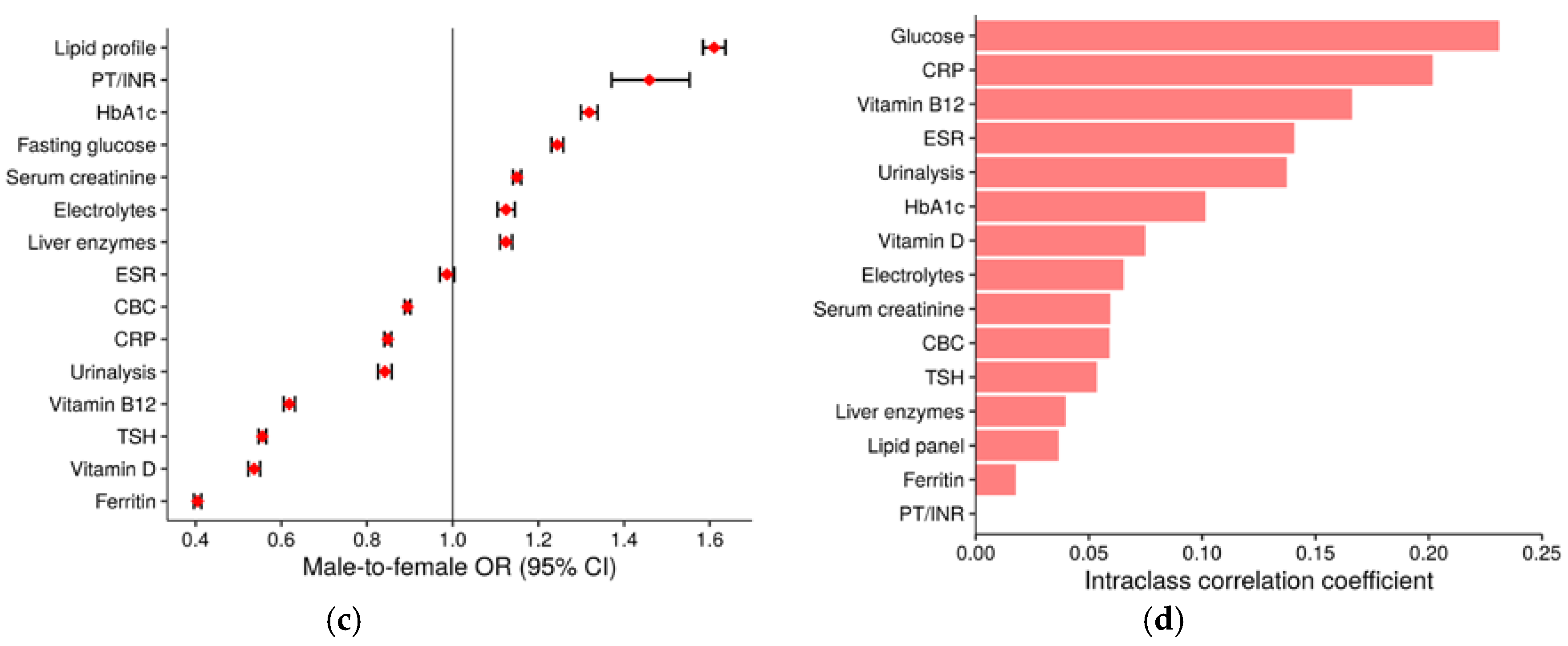
3.2. Test Type-Specific Use of Laboratory Tests
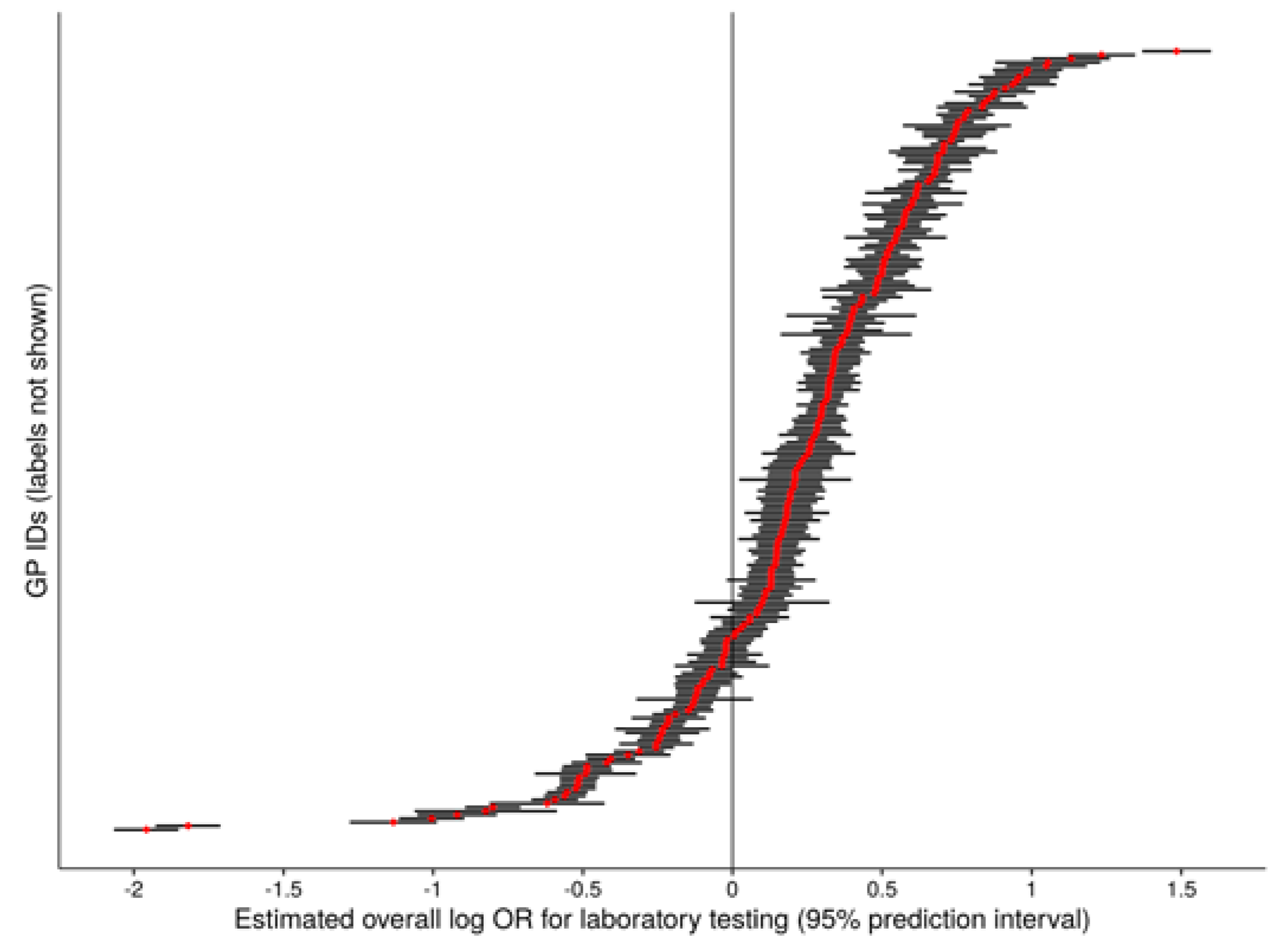
3.3. Overall Use of Laboratory Tests
4. Discussion
Stengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Forsman, R.W. Why is the laboratory an afterthought for managed care organizations? Clin. Chem. 1996, 42, 813–816. [Google Scholar] [CrossRef] [PubMed]
- Vinker, S.; Kvint, I.; Erez, R.; Elhayany, A.; Kahan, E. Effect of the characteristics of family physicians on their utilisation of laboratory tests. Br. J. Gen. Pract. J. R. College Gen. Pract. 2007, 57, 377–382. [Google Scholar]
- Birtwhistle, R.V. Diagnostic testing in family practice. Can. Fam. Phys. Med. Fam. Can. 1988, 34, 327–331. [Google Scholar]
- O’Sullivan, J.W.; Stevens, S.; Hobbs, F.D.R.; Salisbury, C.; Little, P.; Goldacre, B.; Bankhead, C.; Aronson, J.K.; Perera, R.; Heneghan, C. Temporal trends in use of tests in UK primary care, 2000–2015: Retrospective analysis of 250 million tests. BMJ 2018, 363, k4666. [Google Scholar] [CrossRef] [PubMed]
- Hickner, J.; Thompson, P.J.; Wilkinson, T.; Epner, P.; Sheehan, M.; Pollock, A.M.; Lee, J.; Duke, C.C.; Jackson, B.R.; Taylor, J.R. Primary care physicians’ challenges in ordering clinical laboratory tests and interpreting results. J. Am. Board Fam. Med. JABFM 2014, 27, 268–274. [Google Scholar] [CrossRef]
- Naugler, C. A perspective on laboratory utilization management from Canada. Clin. Chim. Acta Int. J. Clin. Chem. 2014, 427, 142–144. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, J.W.; Albasri, A.; Nicholson, B.D.; Perera, R.; Aronson, J.K.; Roberts, N.; Heneghan, C. Overtesting and undertesting in primary care: A systematic review and meta-analysis. BMJ Open 2018, 8, e018557. [Google Scholar] [CrossRef]
- Ganguli, I.; Simpkin, A.L.; Lupo, C.; Weissman, A.; Mainor, A.J.; Orav, E.J.; Rosenthal, M.B.; Colla, C.H.; Sequist, T.D. Cascades of Care After Incidental Findings in a US National Survey of Physicians. JAMA Netw. Open 2019, 2, e1913325. [Google Scholar] [CrossRef]
- Van der Weijden, T.; van Bokhoven, M.A.; Dinant, G.J.; van Hasselt, C.M.; Grol, R.P. Understanding laboratory testing in diagnostic uncertainty: A qualitative study in general practice. Br. J. Gen. Pract. J. R. Coll. Gen. Pract. 2002, 52, 974–980. [Google Scholar]
- Naugler, C. Laboratory test use and primary care physician supply. Can. Fam. Phys. Med. Fam. Can. 2013, 59, e240–e245. [Google Scholar]
- Eisenberg, J.M.; Nicklin, D. Use of diagnostic services by physicians in community practice. Med. Care 1981, 19, 297–309. [Google Scholar] [CrossRef] [PubMed]
- DeKay, M.L.; Asch, D.A. Is the defensive use of diagnostic tests good for patients, or bad? Med. Decis. Mak. Int. J. Soc. Med. Decis. Mak. 1998, 18, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Kristiansen, I.S.; Hjortdahl, P. The general practitioner and laboratory utilization: Why does it vary? Fam. Pract. 1992, 9, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Djalali, S.; Ursprung, N.; Rosemann, T.; Senn, O.; Tandjung, R. Undirected health IT implementation in ambulatory care favors paper-based workarounds and limits health data exchange. Int. J. Med. Inform. 2015, 84, 920–932. [Google Scholar] [CrossRef]
- Swiss Federal Office of Public Health. Federal Analysis List (Status as of 30 April 2020); Swiss Federal Office of Public Health: Bern, Switzerland, 2020.
- Wennberg, J.E. Time to tackle unwarranted variations in practice. BMJ 2011, 342, d1513. [Google Scholar] [CrossRef]
- Swiss Federal Office of Public Health. Monitoring der Analysenliste 2013–2015; Swiss Federal Office of Public Health: Bern, Switzerland, 2019.
- Federal Act on Research Involving Human Beings of 30 September 2011 (Status as of 1 January 2020). Available online: https://www.admin.ch/opc/en/classified-compilation/20061313/index.html (accessed on 15 May 2020).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Using lme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 2009, 32, 1327–1334. [CrossRef]
- Rodd, C.; Sokoro, A.; Lix, L.M.; Thorlacius, L.; Moffatt, M.; Slater, J.; Bohm, E. Increased rates of 25-hydroxy vitamin D testing: Dissecting a modern epidemic. Clin. Biochem. 2018, 59, 56–61. [Google Scholar] [CrossRef]
- Granado-Lorencio, F.; Blanco-Navarro, I.; Pérez-Sacristán, B. Criteria of adequacy for vitamin D testing and prevalence of deficiency in clinical practice. Clin. Chem. Lab. Med. 2016, 54, 791–798. [Google Scholar] [CrossRef]
- Woodford, H.J.; Barrett, S.; Pattman, S. Vitamin D: Too much testing and treating? Clin. Med. 2018, 18, 196–200. [Google Scholar] [CrossRef]
- Zhao, S.; Gardner, K.; Taylor, W.; Marks, E.; Goodson, N. Vitamin D assessment in primary care: Changing patterns of testing. Lond. J. Prim. Care 2015, 7, 15–22. [Google Scholar] [CrossRef] [PubMed]
- McCoy, R.G.; Van Houten, H.K.; Ross, J.S.; Montori, V.M.; Shah, N.D. HbA1c overtesting and overtreatment among US adults with controlled type 2 diabetes, 2001–2013: Observational population based study. BMJ 2015, 351, h6138. [Google Scholar] [CrossRef] [PubMed]
- Adams, G.; Gulliford, M.C.; Ukoumunne, O.C.; Eldridge, S.; Chinn, S.; Campbell, M.J. Patterns of intra-cluster correlation from primary care research to inform study design and analysis. J. Clin. Epidemiol. 2004, 57, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.T.; Guo, M.; Hemmelgarn, B.; Quan, H.; Clement, F.; Sajobi, T.; Thomas, R.; Turin, T.C.; Naugler, C. Evaluating practice variance among family physicians to identify targets for laboratory utilization management. Clin. Chim. Acta Int. J. Clin. Chem. 2019, 497, 1–5. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, J.W.; Stevens, S.; Oke, J.; Hobbs, F.D.R.; Salisbury, C.; Little, P.; Goldacre, B.; Bankhead, C.; Aronson, J.K.; Heneghan, C.; et al. Practice variation in the use of tests in UK primary care: A retrospective analysis of 16 million tests performed over 3.3 million patient years in 2015/16. BMC Med. 2018, 16, 229. [Google Scholar] [CrossRef]
- Barnett, K.; Mercer, S.W.; Norbury, M.; Watt, G.; Wyke, S.; Guthrie, B. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet 2012, 380, 37–43. [Google Scholar] [CrossRef]
- Thompson, A.E.; Anisimowicz, Y.; Miedema, B.; Hogg, W.; Wodchis, W.P.; Aubrey-Bassler, K. The influence of gender and other patient characteristics on health care-seeking behaviour: A QUALICOPC study. BMC Fam. Pract. 2016, 17, 38. [Google Scholar] [CrossRef]
- Nabalamba, A.; Millar, W.J. Going to the doctor. Health Rep. 2007, 18, 23–35. [Google Scholar]
- Mosca, L.; Barrett-Connor, E.; Wenger, N.K. Sex/gender differences in cardiovascular disease prevention: What a difference a decade makes. Circulation 2011, 124, 2145–2154. [Google Scholar] [CrossRef]
- Puymirat, E.; Simon, T.; Steg, P.G.; Schiele, F.; Gueret, P.; Blanchard, D.; Khalife, K.; Goldstein, P.; Cattan, S.; Vaur, L.; et al. Association of changes in clinical characteristics and management with improvement in survival among patients with ST-elevation myocardial infarction. JAMA 2012, 308, 998–1006. [Google Scholar] [CrossRef]
- Mosca, L.; Linfante, A.H.; Benjamin, E.J.; Berra, K.; Hayes, S.N.; Walsh, B.W.; Fabunmi, R.P.; Kwan, J.; Mills, T.; Simpson, S.L. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation 2005, 111, 499–510. [Google Scholar] [CrossRef] [PubMed]
- Cawthon, P.M. Gender differences in osteoporosis and fractures. Clin. Orthop. Relat. Res. 2011, 469, 1900–1905. [Google Scholar] [CrossRef] [PubMed]
- Levi, M.; Rosselli, M.; Simonetti, M.; Brignoli, O.; Cancian, M.; Masotti, A.; Pegoraro, V.; Cataldo, N.; Heiman, F.; Chelo, M.; et al. Epidemiology of iron deficiency anaemia in four European countries: A population-based study in primary care. Eur. J. Haematol. 2016, 97, 583–593. [Google Scholar] [CrossRef] [PubMed]
- Vanderpump, M.P. The epidemiology of thyroid disease. Br. Med. Bull. 2011, 99, 39–51. [Google Scholar] [CrossRef]
- Paslakis, G.; Richardson, C.; Nohre, M.; Brahler, E.; Holzapfel, C.; Hilbert, A.; de Zwaan, M. Prevalence and psychopathology of vegetarians and vegans-Results from a representative survey in Germany. Sci. Rep. 2020, 10, 6840. [Google Scholar] [CrossRef]
- Rachamin, Y.; Meier, R.; Grischott, T.; Rosemann, T.; Markun, S. General practitioners’ consultation counts and associated factors in Swiss primary care–A retrospective observational study. PLoS ONE 2020, 14, e0227280. [Google Scholar] [CrossRef]
| Characteristic | At Least One Laboratory Test Reported (n = 315,807) | No Laboratory Tests Reported (n = 258,996) |
|---|---|---|
| Male sex, n (%) | 172,810 (54.7) | 132,062 (51.0) |
| Female sex, n (%) | 142,997 (45.3) | 126,934 (49.0) |
| Median age at observation start, years (IQR) | 48 (32–64) | 39 (25–56) |
| Median follow-up time, days (IQR) | 406 (134–1152) | 8 (1–227) |
| Median consultations per patient, n (IQR) | 9 (1–19) | 2 (1–4) |
| Full Model | ||||
| Consultations, n | 1,608,613 | |||
| Fixed effects | β(SE) | OR (95% CI) | Wald’s χ2 | p-Value |
| Intercept | −1.95 (0.03) | 0.14 (0.13–0.15) | −60 | <0.001 |
| Male sex | −0.143 (0.009) | 0.87 (0.86–0.88) | −16 | <0.001 |
| Age (10 years) | 0.058 (0.002) | 1.060 (1.056–1.065) | 27 | <0.001 |
| Random effects | Variance estimate | Group members, n | ||
| Patient ID | 3.16 | 234,931 | ||
| GP ID | 0.22 | 210 | ||
| Null model | ||||
| Fixed effects | β(SE) | OR (95% CI) | Wald’s χ2 | p-Value |
| Intercept | −2.04 (0.03) | 0.13 (0.12–0.14) | −72 | <0.001 |
| Random effects | Variance estimate | ICC | ||
| Patient ID | 3.17 | |||
| GP ID | 0.21 | 0.032 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schumacher, L.D.; Jäger, L.; Meier, R.; Rachamin, Y.; Senn, O.; Rosemann, T.; Markun, S. Trends and between-Physician Variation in Laboratory Testing: A Retrospective Longitudinal Study in General Practice. J. Clin. Med. 2020, 9, 1787. https://doi.org/10.3390/jcm9061787
Schumacher LD, Jäger L, Meier R, Rachamin Y, Senn O, Rosemann T, Markun S. Trends and between-Physician Variation in Laboratory Testing: A Retrospective Longitudinal Study in General Practice. Journal of Clinical Medicine. 2020; 9(6):1787. https://doi.org/10.3390/jcm9061787
Chicago/Turabian StyleSchumacher, Lisa D., Levy Jäger, Rahel Meier, Yael Rachamin, Oliver Senn, Thomas Rosemann, and Stefan Markun. 2020. "Trends and between-Physician Variation in Laboratory Testing: A Retrospective Longitudinal Study in General Practice" Journal of Clinical Medicine 9, no. 6: 1787. https://doi.org/10.3390/jcm9061787
APA StyleSchumacher, L. D., Jäger, L., Meier, R., Rachamin, Y., Senn, O., Rosemann, T., & Markun, S. (2020). Trends and between-Physician Variation in Laboratory Testing: A Retrospective Longitudinal Study in General Practice. Journal of Clinical Medicine, 9(6), 1787. https://doi.org/10.3390/jcm9061787






