Leveraging Fitness Tracker and Personalized Exercise Prescription to Promote Breast Cancer Survivors’ Health Outcomes: A Feasibility Study
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Study Design and Procedure
2.3. Measurements
2.4. Statistical Analysis
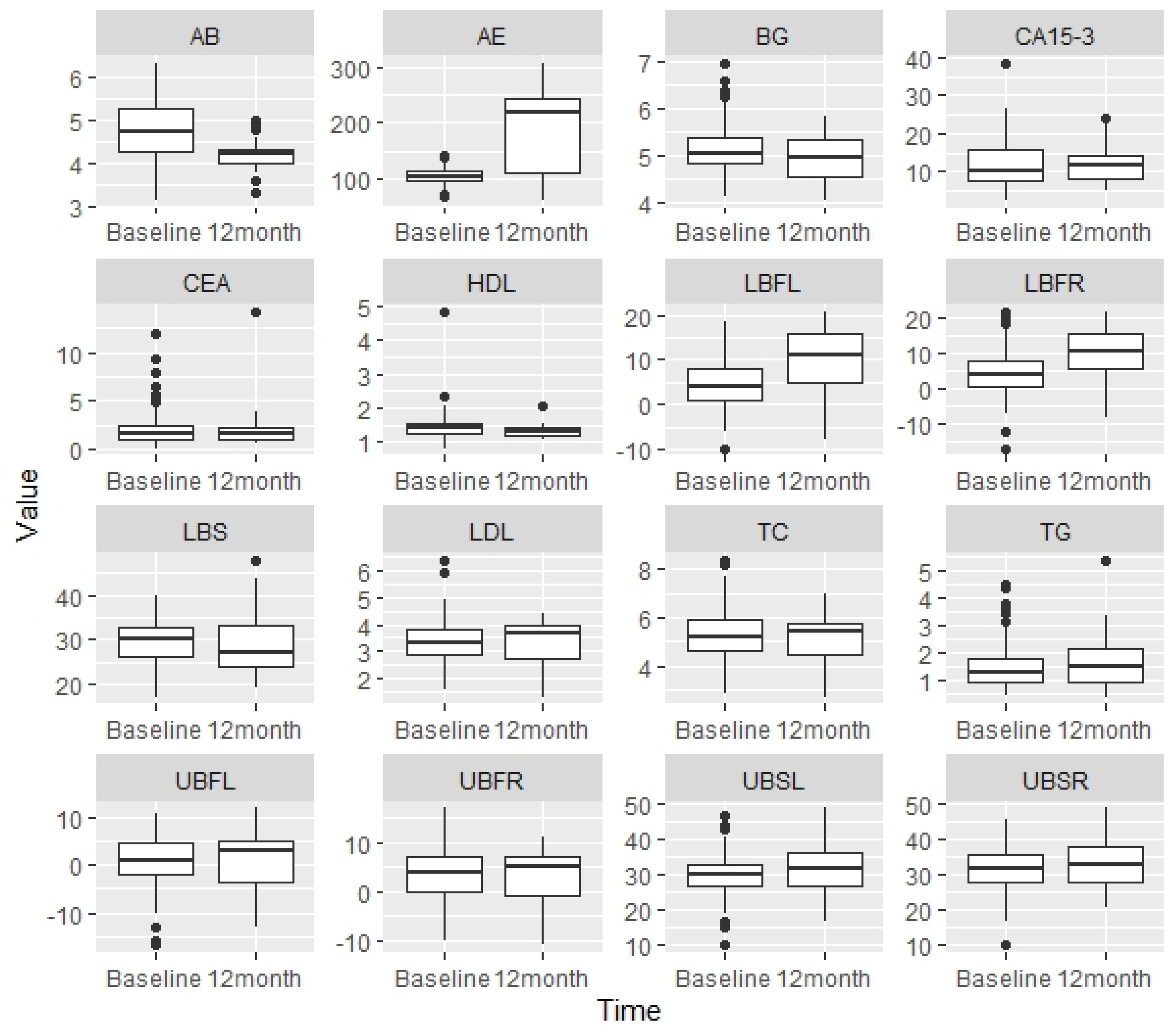
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A.
Appendix A.1. Week 1
- Strength Workout
- ○
- Dumbbell Lunges (count every other leg): 3 sets × 10–12 repetitions
- ■
- Alternative: Walking Lunges without Dumbbells (still counts every other leg)
- ○
- Hamstring Curls: 3 sets × 10–12 repetitions
- ■
- Alternative: Glute Kickbacks
- ○
- Calf Raises: 3 sets × 50 repetitions
- ■
- Alternative: Seated Heel Lifts
- ○
- Bicycle Crunches: 2 sets × 50 revolutions
- ■
- Alternative: Standard Crunches
- Cardio Workout
- ○
- 30-min selected cardio exercise at moderate pace: rating of perceived exertion (RPE) Scale: 4–6
- Strength Workout
- ○
- Dumbbell Bench Press: 3 sets × 10–12 repetitions
- ■
- Alternative: Push-Ups on Knees (only go down as far as your mobility will allow)
- ○
- Tricep Kickbacks: 3 sets × 10–12 repetitions
- ■
- Alternative: Tricep Dips on a Chair (only go down as far as your mobility will allow)
- ○
- Dumbbell Chest Flies (go light and pretend to “hug a tree”): 3 sets × 10–12 repetitions
- ■
- Alternative: Wide-Grip Wall Push-Ups
- ○
- Bicycle Crunches: 2 sets × 50 revolutions
- ■
- Alternative: Standard Crunches
- Cardio Workout
- ○
- 30-min selected cardio exercise at high-intensity intervals: These intervals will be comprised of 1 min easy (RPE Scale: 2–3) and 1 min hard (RPE Scale: 7–8) and will be repeated until time is up.
- Strength Workout
- ○
- Upright Rows: 3 sets × 10–12 repetitions
- ■
- Alternative: Forward Arm Raises
- ○
- One-Arm Rows (pretend you are “starting a lawnmower”): 3 sets × 10–12 repetitions
- ■
- Alternative: Single Arm Circles
- ○
- Lat Pulldowns: 3 sets × 10–12 repetitions
- ■
- Alternative: Seated Reaching Exercise (count every other side)
- ○
- Dumbbell Shrugs: 2 sets × 10–12 repetitions
- ■
- Alternative: Shoulders to Ears
- ○
- Sit-ups: 2 sets × 25 repetitions
- ■
- Alternative: Standard Crunches
- Cardio Workout
- ○
- 30-min selected cardio exercise at moderate pace: RPE Scale: 4–6
- Cardio Workout Only
- ○
- 60-min selected cardio at light/moderate pace: RPE Scale: 3–6
Appendix A.2. Week 2
- Strength Workout
- ○
- Goblet Squats with Dumbbell: 3 sets × 10–12 repetitions
- ■
- Alternative: Air Squats
- ○
- Hamstring Curls: 3 sets × 10–12 repetitions
- ■
- Alternative: Glute Kickbacks
- ○
- Calf Raises: 3 sets × 50 repetitions
- ■
- Alternative: Seated Heel Lifts
- ○
- Leg Raises: 2 sets × 25 raises
- ■
- Alternative: Seated Leg Lifts
- Cardio Workout
- ○
- 30-min selected cardio exercise at moderate pace: RPE Scale: 4–6
- Strength Workout
- ○
- Incline Dumbbell Bench Press: 3 sets × 10–12 repetitions
- ■
- Alternative: Push-Ups on Knees (only go down as far as your mobility will allow)
- ○
- Diamond Push-Ups: 3 sets × 10–12 repetitions
- ■
- Alternative: Close-Grip Wall Push-Ups
- ○
- Dumbbell Chest Flies (go light and pretend to “hug a tree”): 3 sets × 10–12 repetitions
- ■
- Alternative: Wide-Grip Wall Push-Ups
- ○
- Jack Knives: 2 sets × 20 repetitions
- ■
- Alternative: Standard Crunches
- Cardio Workout
- ○
- 30-min selected cardio exercise at high-intensity intervals: These intervals will be comprised of 1 min easy (RPE Scale: 2–3) and 1 min hard (RPE Scale: 7–8) and will be repeated until time is up.
- Strength Workout
- ○
- Upright Rows: 3 sets × 10–12 repetitions
- ■
- Alternative: Forward Arm Raises
- ○
- One-Arm Rows (pretend you are “starting a lawnmower”): 3 sets × 10–12 repetitions
- ■
- Alternative: Single Arm Circles
- ○
- Lat Pulldowns: 3 sets × 10–12 repetitions
- ■
- Alternative: Seated Reaching Exercise (count every other side)
- ○
- Seated Cable Row: 2 sets × 10–12 repetitions
- ■
- Alternative: Single Arm Circles
- ○
- Sit-ups: 2 sets × 25 repetitions
- ■
- Alternative: Standard Crunches
- Cardio Workout
- ○
- 30-min selected cardio exercise at moderate pace: RPE Scale: 4–6
- Cardio Workout ONLY
- ○
- 60-min selected cardio at light/moderate pace: RPE Scale: 3–6
Appendix A.3. Week 1
- Strength Workout
- ○
- Dumbbell Lunges (count every other leg): 3 sets × 10–12 repetitions
- ■
- Alternative: Walking Lunges without Dumbbells (still count every other leg)
- ○
- Hamstring Curls: 3 sets × 10–12 repetitions
- ■
- Alternative: Glute Kickbacks
- ○
- Calf Raises: 3 sets × 50 repetitions
- ■
- Alternative: Seated Heel Lifts
- ○
- Bicycle Crunches: 2 sets × 50 revolutions
- ■
- Alternative: Standard Crunches
- Cardio Workout
- ○
- 30-min selected cardio exercise at moderate pace: RPE Scale: 4–6
- Cardio Workout Only
- ○
- 30-min selected cardio at light/moderate pace: RPE Scale: 3–6
- Strength Workout
- ○
- Dumbbell Bench Press: 3 sets × 10–12 repetitions
- ■
- Alternative: Push-Ups on Knees or on Toes (only go as far down as your mobility will allow)
- ○
- Tricep Kickbacks: 3 sets × 10–12 repetitions
- ■
- Alternative: Tricep Dips on Chair (only go as far down as your mobility will allow)
- ○
- Dumbbell Chest Flies (go light and pretend to “hug a tree”): 3 sets × 10–12 repetitions
- ■
- Alternative: Wide-Grip Wall Push-Ups
- ○
- Bicycle Crunches: 2 sets × 50 revolutions
- ■
- Alternative: Sit-Ups
- Cardio Workout
- ○
- 30-min selected cardio exercise at high-intensity intervals: These intervals will be comprised of 1 min easy (RPE Scale: 2–3) and 1 min hard (RPE Scale: 7–8) and will be repeated until time is up.
- Cardio Workout Only
- ○
- 30-min selected cardio at light/moderate pace: RPE Scale: 3–6
- Strength Workout
- ○
- Upright Rows: 3 sets × 10–12 repetitions
- ■
- Alternative: Forward Arm Raises
- ○
- One-Arm Rows (pretend you are “starting a lawnmower”): 3 sets × 10–12 repetitions
- ■
- Alternative: Single Arm Circles
- ○
- Lat Pulldowns: 3 sets × 10–12 repetitions
- ■
- Alternative: Seated Reaching Exercise (count every other side)
- ○
- Dumbbell Shrugs: 2 sets × 10–12 repetitions
- ■
- Alternative: Shoulders to Ears
- ○
- Sit-ups: 2 sets × 25 repetitions
- ■
- Alternative: Bicycle Crunches or Standard Crunches
- Cardio Workout
- ○
- 30-min selected cardio exercise at moderate pace: RPE Scale: 4–6
Appendix A.4. Week 2
- Strength Workout
- ○
- Goblet Squats with Dumbbell: 3 sets × 10–12 repetitions
- ■
- Alternative: Air Squats
- ○
- Hamstring Curls: 3 sets × 10–12 repetitions
- ■
- Alternative: Glute Kickbacks
- ○
- Split Jumps: 3 sets × 16 repetitions
- ■
- Alternative: Walking Lunges without Dumbbells (count every other leg)
- ○
- Leg Raises: 2 sets × 25 raises
- ■
- Alternative: Standing Leg Raises (count every other leg)
- Cardio Workout
- ○
- 30-min selected cardio exercise at moderate pace: RPE Scale: 4–6
- Cardio Workout Only
- ○
- 30-min selected cardio at light/moderate pace: RPE Scale: 3–6
- Strength Workout
- ○
- Incline Dumbbell Bench Press: 3 sets × 10–12 repetitions
- ■
- Alternative: Push-Ups on Knees or Toes (only go as far down as your mobility will allow)
- ○
- Diamond Push-Ups: 3 sets × 10–12 repetitions
- ■
- Alternative: Close-Grip Wall Push-Ups
- ○
- Dumbbell Chest Flies (go light and pretend to “hug a tree”): 3 sets × 10–12 repetitions
- ■
- Alternative: Wide-Grip Wall Push-Ups
- ○
- Jack Knives: 2 sets × 20 repetitions
- ■
- Alternative: Sit-Ups or Standard Crunches
- Cardio Workout
- ○
- 30-min selected cardio exercise at high-intensity intervals: These intervals will be comprised of 1 min easy (RPE Scale: 2–3) and 1 min hard (RPE Scale: 7–8) and will be repeated until time is up.
- Cardio Workout Only
- ○
- 30-min selected cardio at light/moderate pace: RPE Scale: 3–6
- Strength Workout
- ○
- Upright Rows: 3 sets × 10–12 repetitions
- ■
- Alternative: Forward Arm Raises
- ○
- Back Extension: 3 sets × 10–12 repetitions
- ■
- Alternative: Good Morning Exercise (keep back straight through range of motion)
- ○
- Lat Pulldowns: 3 sets × 10–12 repetitions
- ■
- Alternative: Seated Reaching Exercise
- ○
- Seated Cable Row: 2 sets × 10–12 repetitions
- ■
- Alternative: Single Arm Circles
- ○
- Sit-ups: 2 sets × 25 repetitions
- ■
- Alternative: Bicycle Crunches or Standard Crunches
- Cardio Workout
- ○
- 30-min selected cardio exercise at moderate pace: RPE Scale: 4–6
References
- Torre, L.A.; Siegel, R.L.; Ward, E.M.; Jemal, A. Global cancer incidence and mortality rates and trends—An Update. Cancer Epidemiol. Biomark. Prev. 2016, 25, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Burnham, T.R.; Wilcox, A. Effects of exercise on physiological and psychological variables in cancer survivors. Med. Sci. Sports Exerc. 2002, 34, 1863–1867. [Google Scholar] [CrossRef] [PubMed]
- American Cancer Society. Cancer Facts & Figures 2019. Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf (accessed on 26 October 2019).
- Government of Canada. Canada Cancer Statistics. Available online: https://www.canada.ca/en/public-health/services/chronic-diseases/cancer/canadian-cancer-statistics.html (accessed on 26 October 2019).
- Xinhua English News. Xinhuanet Survival rate for Breast Cancer Rises in China. Available online: http://www.xinhuanet.com/english/2019-04/21/c_137995095.htm (accessed on 26 October 2019).
- Runowicz, C.D.; Leach, C.R.; Henry, N.L.; Henry, K.S.; Mackey, H.T.; Cowens-Alvarado, R.L.; Cannady, R.S.; Pratt-Chapman, M.L.; Edge, S.B.; Jacobs, L.A.; et al. American cancer society/American society of clinical oncology breast cancer survivorship care guideline. CA Cancer J. Clin. 2016, 66, 43–73. [Google Scholar] [CrossRef] [PubMed]
- Luan, X.; Tian, X.; Zhang, H.; Huang, R.; Li, N.; Chen, P.; Wang, R. Exercise as a prescription for patients with various diseases. J. Sport Health Sci. 2019, 8, 422–441. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Macera, C.A. Promoting physical activity in a public health context. J. Sport Health Sci. 2018, 7, 1–2. [Google Scholar] [CrossRef]
- Schmitz, K.H.; Courneya, K.S.; Matthews, C.; Demark-Wahnefried, W.; Galvão, D.A.; Pinto, B.M.; Irwin, M.L.; Wolin, K.Y.; Segal, R.J.; Lucia, A.; et al. American college of sports medicine roundtable on exercise guidelines for cancer survivors. Med. Sci. Sports Exerc. 2010, 42, 1409–1426. [Google Scholar] [CrossRef]
- DiPietro, L.; Buchner, D.M.; Marquez, D.X.; Pate, R.R.; Pescatello, L.S.; Whitt-Glover, M.C. New scientific basis for the 2018 U.S. physical activity guidelines. J. Sport Health Sci. 2019, 8, 197–200. [Google Scholar] [CrossRef]
- Meneses-Echávez, J.F.; González-Jiménez, E.; Ramírez-Vélez, R. Effects of supervised exercise on cancer-related fatigue in breast cancer survivors: A systematic review and meta-analysis. BMC Cancer 2015, 15, 77. [Google Scholar] [CrossRef]
- McNeely, M.L.; Campbell, K.; Ospina, M.; Rowe, B.H.; Dabbs, K.; Klassen, T.P.; Mackey, J.; Courneya, K. Exercise interventions for upper-limb dysfunction due to breast cancer treatment. Cochrane Database Syst. Rev. 2010, 005211. [Google Scholar] [CrossRef]
- Speck, R.M.; Courneya, K.S.; Mâsse, L.C.; Duval, S.; Schmitz, K.H. An update of controlled physical activity trials in cancer survivors: A systematic review and meta-analysis. J. Cancer Surviv. 2010, 4, 87–100. [Google Scholar] [CrossRef]
- Cormie, P.; Zopf, E.M.; Zhang, X.; Schmitz, K.H. The impact of exercise on cancer mortality, recurrence, and treatment-related adverse effects. Epidemiol. Rev. 2017, 39, 71–92. [Google Scholar] [CrossRef]
- Irwin, M.L.; McTiernan, A.; Bernstein, L.; Gilliland, F.D.; Baumgartner, R.; Baumgartner, K.; Ballard-Barbash, R. Physical activity levels among breast cancer survivors. Med. Sci. Sports Exerc. 2004, 36, 1484–1491. [Google Scholar]
- Irwin, M.L.; Crumley, D.; McTiernan, A.; Bernstein, L.; Baumgartner, R.; Gilliland, F.D.; Kriska, A.; Ballard-Barbash, R. Physical activity levels before and after a diagnosis of breast carcinoma: The health, eating, activity, and lifestyle (HEAL) study. Cancer 2003, 97, 1746–1757. [Google Scholar] [CrossRef] [PubMed]
- Wood, W.; Neal, D.T. Healthy through habit: Interventions for initiating & maintaining health behavior change. Behav. Sci. Policy 2016, 2, 71–83. [Google Scholar]
- Galvão, D.A.; Newton, R.U. Review of exercise intervention studies in cancer patients. JCO 2005, 23, 899–909. [Google Scholar] [CrossRef] [PubMed]
- McNeely, M.L.; Campbell, K.L.; Rowe, B.H.; Klassen, T.P.; Mackey, J.R.; Courneya, K.S. Effects of exercise on breast cancer patients and survivors: A systematic review and meta-analysis. CMAJ 2006, 175, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Campbell, K.L.; Neil, S.E.; Winters-Stone, K.M. Review of exercise studies in breast cancer survivors: Attention to principles of exercise training. Br. J. Sports Med. 2012, 46, 909–916. [Google Scholar] [CrossRef]
- Neil-Sztramko, S.E.; Winters-Stone, K.M.; Bland, K.A.; Campbell, K.L. Updated systematic review of exercise studies in breast cancer survivors: Attention to the principles of exercise training. Br. J. Sports Med. 2019, 53, 504–512. [Google Scholar] [CrossRef]
- Zeng, N.; Pope, Z.; Lee, J.; Gao, Z. Virtual reality exercise for anxiety and depression: A preliminary review of current research in an emerging field. J. Clin. Med. 2018, 7, 42. [Google Scholar] [CrossRef]
- Pope, Z.; Lee, J.E.; Zeng, N.; Lee, H.Y.; Gao, Z. Feasibility of smartphone application and social media intervention on breast cancer survivors’ health outcomes. Transl. Behav. Med. 2019, 9, 11–22. [Google Scholar] [CrossRef]
- Nguyen, N.H.; Hadgraft, N.T.; Moore, M.M.; Rosenberg, D.E.; Lynch, C.; Reeves, M.M.; Lynch, B.M. A qualitative evaluation of breast cancer survivors’ acceptance of and preferences for consumer wearable technology activity trackers. Support. Care Cancer 2017, 25, 3375–3384. [Google Scholar] [CrossRef] [PubMed]
- Quintiliani, L.M.; Mann, D.M.; Puputti, M.; Quinn, E.; Bowen, D.J. Pilot and feasibility test of a mobile health-supported behavioral counseling intervention for weight management among breast cancer survivors. JMIR Cancer 2016, 2, 4. [Google Scholar] [CrossRef] [PubMed]
- Pope, Z.C.; Zeng, N.; Zhang, R.; Lee, H.Y.; Gao, Z. Effectiveness of combined smartwatch and social media intervention on breast cancer survivor health outcomes: A 10-week pilot randomized trial. J. Clin. Med. 2018, 7, 140. [Google Scholar] [CrossRef] [PubMed]
- Nierkens, V.; Hartman, M.A.; Nicolaou, M.; Vissenberg, C.; Beune, E.J.A.J.; Hosper, K.; van Valkengoed, I.G.; Stronks, K. Effectiveness of cultural adaptations of interventions aimed at smoking cessation, diet, and/or physical activity in ethnic minorities. A systematic review. PLoS ONE 2013, 8, e73373. [Google Scholar] [CrossRef] [PubMed]
- Wilde, B.E.; Sidman, C.L.; Corbin, C.B. A 10,000-step count as a physical activity target for sedentary women. Res. Q. Exerc. Sport 2001, 72, 411–414. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Locke, C.; Craig, C.L.; Brown, W.J.; Clemes, S.A.; De Cocker, K.; Giles-Corti, B.; Hatano, Y.; Inoue, S.; Matsudo, S.M.; Mutrie, N.; et al. How many steps/day are enough? For adults. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 79. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association declaration of helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Rikli, R.E.; Jones, C.J. Development and validation of a functional fitness test for community-residing older adults. J. Aging Phys. Act. 1999, 7, 129–161. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 2013, 53, 255–267. [Google Scholar] [CrossRef]
- Damush, T.M.; Perkins, A.; Miller, K. The implementation of an oncologist referred, exercise self-management program for older breast cancer survivors. Psycho-Oncolology 2006, 15, 884–890. [Google Scholar] [CrossRef]
- Bates, D.; Maechler, M.; Bolker, B. lme4: Linear Mixed-Effects Models Using S4 Classes. R package Version 0.999375-42. 2011. Available online: http://CRAN.R-project.org/package=lme4 (accessed on 5 March 2020).
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear mixed-effects models using lme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Kuznetsova, A.; Brockhoff, P.B.; Christensen, R.H.B. lmerTest Package: Tests in linear mixed effects models. J. Stat. Softw. 2017, 82, 1–26. [Google Scholar] [CrossRef]
- Phillips, S.M.; Dodd, K.W.; Steeves, J.; McClain, J.; Alfano, C.M.; McAuley, E. Physical activity and sedentary behavior in breast cancer survivors: New insight into activity patterns and potential intervention targets. Gynecol. Oncol. 2015, 138, 398–404. [Google Scholar] [CrossRef]
- Holmes, M.D.; Chen, W.Y.; Feskanich, D.; Kroenke, C.H.; Colditz, G.A. physical activity and survival after breast cancer diagnosis. JAMA 2005, 293, 2479–2486. [Google Scholar] [CrossRef]
- Demark-Wahnefried, W.; Clipp, E.C.; Lipkus, I.M.; Lobach, D.; Snyder, D.C.; Sloane, R.; Peterson, B.; Macri, J.M.; Rock, C.L.; McBride, C.M.; et al. Main outcomes of the FRESH START trial: A sequentially tailored, diet and exercise mailed print intervention among breast and prostate cancer survivors. J. Clin. Oncol. 2007, 25, 2709–2718. [Google Scholar] [CrossRef]
- Duffy, M.J.; Harbeck, N.; Nap, M.; Molina, R.; Nicolini, A.; Senkus, E.; Cardoso, F. Clinical use of biomarkers in breast cancer: Updated guidelines from the European Group on Tumor Markers (EGTM). Eur. J. Cancer 2017, 75, 284–298. [Google Scholar] [CrossRef] [PubMed]
- Ballard-Barbash, R.; Friedenreich, C.M.; Courneya, K.S.; Siddiqi, S.M.; McTiernan, A.; Alfano, C.M. Physical activity, biomarkers, and disease outcomes in cancer survivors: A systematic review. J. Natl. Cancer Inst. 2012, 104, 815–840. [Google Scholar] [CrossRef] [PubMed]
- Löf, M.; Bergström, K.; Weiderpass, E. Physical activity and biomarkers in breast cancer survivors: A systematic review. ScienceDirect 2012, 73, 134–142. Available online: https://www.sciencedirect.com/science/article/pii/S0378512212002356 (accessed on 1 November 2019). [CrossRef] [PubMed]
- Kim, T.H.; Chang, J.S.; Kong, I.D. Effects of exercise training on physical fitness and biomarker levels in breast cancer survivors. J. Lifestyle Med. 2017, 7, 55–62. [Google Scholar] [CrossRef][Green Version]
- Friedenreich, C.M.; Wang, Q.; Yasui, Y.; Stanczyk, F.Z.; Duha, A.; Brenner, D.R.; Courneya, K.S. Long-term effects of moderate versus high durations of aerobic exercise on biomarkers of breast cancer risk: Follow-up to a randomized controlled trial. Cancer Epidemiol. Biomark. Prev. 2019, 28, 1725–1734. [Google Scholar] [CrossRef]
- Irwin, M.L.; Varma, K.; Alvarez-Reeves, M.; Cadmus, L.; Wiley, A.; Chung, G.G.; Dipietro, L.; Mayne, S.T.; Yu, H. Randomized controlled trial of aerobic exercise on insulin and insulin-like growth factors in breast cancer survivors: The Yale Exercise and Survivorship study. Cancer Epidemiol. Biomark. Prev. 2009, 18, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Braithwaite, D.; Satariano, W.A.; Sternfeld, B.; Hiatt, R.A.; Ganz, P.A.; Kerlikowske, K.; Moore, D.H.; Slattery, M.L.; Tammemagi, M.; Castillo, A.; et al. Long-term prognostic role of functional limitations among women with breast cancer. J. Natl. Cancer Inst. 2010, 102, 1468–1477. [Google Scholar] [CrossRef] [PubMed]
- Sehl, M.; Lu, X.; Silliman, R.; Ganz, P.A. Decline in physical functioning in first 2 years after breast cancer diagnosis predicts 10 year survival in older women. J. Cancer Surviv. 2013, 7, 20–31. [Google Scholar] [CrossRef]
- The American Cancer Society Exercises after Breast Cancer Surgery. Available online: https://www.cancer.org/cancer/breast-cancer/treatment/surgery-for-breast-cancer/exercises-after-breast-cancer-surgery.html (accessed on 3 November 2019).
- Milne, H.M.; Wallman, K.E.; Gordon, S.; Courneya, K.S. Effects of a combined aerobic and resistance exercise program in breast cancer survivors: A randomized controlled trial. Breast Cancer Res. Treat. 2008, 108, 279–288. [Google Scholar] [CrossRef]
- Winters-Stone, K.M.; Dobek, J.; Bennett, J.A.; Nail, L.M.; Leo, M.C.; Schwartz, A. The effect of resistance training on muscle strength and physical function in older, postmenopausal breast cancer survivors: A randomized controlled trial. J. Cancer Surviv. 2012, 6, 189–199. [Google Scholar] [CrossRef] [PubMed]
- Foley, M.P.; Hasson, S.M. Effects of a community-based multimodal exercise program on health-related physical fitness and physical function in breast cancer survivors: A pilot study. Integr. Cancer 2016, 15, 446–454. [Google Scholar] [CrossRef] [PubMed]
- Kagawa-Singer, M. A socio-cultural perspective on cancer control issues for Asian Americans. Asian Am. Pac. Isl. J. Health 2000, 8, 12–17. [Google Scholar] [PubMed]
- Vainshelboim, B.; Lima, R.M.; Myers, J. Cardiorespiratory fitness and cancer in women: A prospective pilot study. J. Sport Health Sci. 2019, 8, 457–462. [Google Scholar] [CrossRef] [PubMed]
| Category | Average Steps/Day | Exercise Prescription |
|---|---|---|
| ≤7999 steps/day | ≤2499 steps/day | Level 1.1 |
| 2500–2999 steps/day | Level 1.2 | |
| 3000–3499 steps/day | Level 1.3 | |
| 3500–3999 steps/day | Level 1.4 | |
| 4000–4499 steps/day | Level 1.5 | |
| 4500–4999 steps/day | Level 1.6 | |
| 5000–5499 steps/day | Level 1.7 | |
| 5500–5999 steps/day | Level 1.8 | |
| 6000–6499 steps/day | Level 1.9 | |
| 6500–6999 steps/day | Level 1.10 | |
| 7000–7499 steps/day | Level 1.11 | |
| 7500–7999 steps/day | Level 1.12 | |
| 8000–12,799 steps/day | 8000–8399 steps/day | Level 2.1 |
| 8400–8799 steps/day | Level 2.2 | |
| 8800–9199 steps/day | Level 2.3 | |
| 9200–9599 steps/day | Level 2.4 | |
| 9600–9999 steps/day | Level 2.5 | |
| 10,000–10,399 steps/day | Level 2.6 | |
| 10,400–10,799 steps/day | Level 2.7 | |
| 10,800–11,199 steps/day | Level 2.8 | |
| 11,200–11,599 steps/day | Level 2.9 | |
| 11,600–11,999 steps/day | Level 2.10 | |
| 12,000–12,399 steps/day | Level 2.11 | |
| 12,400–12,799 steps/day | Level 2.12 | |
| ≥12,800 steps/day | 12,800–13,099 steps/day | Level 3.1 |
| 13,100–13,399 steps/day | Level 3.2 | |
| 13,400–13,699 steps/day | Level 3.3 | |
| 13,700–13,999 steps/day | Level 3.4 | |
| 14,000–14,299 steps/day | Level 3.5 | |
| 14,300–14,599 steps/day | Level 3.6 | |
| 14,600–14,899 steps/day | Level 3.7 | |
| 14,900–15,199 steps/day | Level 3.8 | |
| 15,200–15,499 steps/day | Level 3.9 | |
| 15,500–15,799 steps/day | Level 3.10 | |
| 15,800–16,099 steps/day | Level 3.11 | |
| ≥16,100 steps/day | Level 3.12 |
| Item | Description |
|---|---|
| Chair Stand | The number of full stands with arms folded across the chest completed in 30 s was used to represent lower-body strength. |
| Arm Curl | The number of 5-pound (2.28 kg) dumbbell biceps curls completed in 30 s were used to represent upper-body strength. |
| Chair Sit-and-Reach | From a sitting position at the front of chair with leg extended and hands reaching toward toes, the number of centimeters between extended fingers and tip of toe (+/−) was used to represent lower-body flexibility. |
| Back Scratch | With one hand reaching over the shoulder and one up the middle of the back, the number of centimeters between extended middle fingers (+/−) was used to represent upper-body flexibility. |
| 8-Foot Up-and-Go | The number of seconds required to get up from a seated position, to walk 8 feet (2.44 m), to turn, and to return to a seated position were used to represent agility and balance. |
| 2-Minute Step | The number of times that the right knee reaches the tape level (midway between the patella and iliac crest in 2 min were used to represent aerobic endurance. |
| Characteristics | Initial Sample (N = 95) | Nonadherence (N = 62) | Adherence (N = 33) |
|---|---|---|---|
| a Age (year) | 44.81 ± 7.94 | 44.98 ± 8.48 | 44.48 ± 6.93 |
| a Height (cm) | 158.18 ± 4.39 | 158.14 ± 4.74 | 158.27 ± 3.74 |
| a Weight (kg) | 55.21 ± 7.69 | 55.22 ± 8.28 | 55.19 ± 6.59 |
| a Body Mass Index (kg/m2) | 22.18 ± 3.48 | 22.27 ± 3.84 | 21.99 ± 2.73 |
| a Waist Circumference (cm) | 77.68 ± 9.26 | 77.17 ± 10.06 | 78.64 ± 7.57 |
| a Hip Circumference (cm) | 93.47 ± 6.57 | 93.77 ± 6.54 | 92.91 ± 6.70 |
| b Diagnosed breast cancer stage | |||
| Stage 0 | 5 | 3 | 2 |
| Stage I | 26 | 17 | 9 |
| Stage IIa | 38 | 26 | 12 |
| Stage IIb | 14 | 11 | 3 |
| Stage IIIa | 10 | 3 | 7 |
| Stage IIIc | 2 | 2 | 0 |
| b Menstrual status | |||
| Postmenopause | 52 | 32 | 20 |
| Premenopause | 43 | 27 | 16 |
| Health Outcomes | Baseline (N = 95) | 12-Month (N = 33) | Estimate (95% CI) | p Value |
|---|---|---|---|---|
| Blood Glucose (mmol/L) | 5.14 ± 0.47 | 4.92 ± 0.52 | −0.22 (−0.41–−0.03) | 0.028 * |
| Cancer Antigen 15-3 (U/mL) | 11.94 ± 5.71 | 12.01 ± 5.19 | 0.006 (−1.394–1.406) | 0.993 |
| Carcinoembryonic Antigen (ng/mL) | 2.15 ± 1.88 | 2.26 ± 2.57 | 0.13 (−0.12–0.38) | 0.759 |
| High-Density Lipoprotein (mmol/L) | 1.46 ± 0.45 | 1.33 ± 0.21 | −0.05 (−0.14–0.04) | 0.362 |
| Low-Density Lipoprotein (mmol/L) | 3.35 ± 0.90 | 3.35 ± 0.85 | −0.03 (−0.10–0.04) | 0.820 |
| Total Cholesterol (mmol/L) | 5.29 ± 1.07 | 5.19 ± 1.05 | −0.14 (−0.42–0.14) | 0.456 |
| Triglyceride (mmol/L) | 1.51 ± 0.85 | 1.71 ± 1.11 | 0.18 (−0.18–0.54) | 0.364 |
| Functional Fitness | ||||
| Agility and Balance (seconds) | 4.76 ± 0.07 | 4.22 ± 0.34 | −0.47 (−0.68–−0.26) | <0.001 * |
| Aerobic Endurance (times) | 105.39 ± 14.20 | 194.64 ± 70.25 | 89.25 (73.82–104.68) | <0.001 * |
| Left Lower-Body Flexibility (cm) | 4.93 ± 5.59 | 10.37 ± 6.96 | 4.58 (−4.4–13.56) | <0.001 * |
| Right Lower-Body Flexibility (cm) | 4.98 ± 6.83 | 10.73 ± 6.62 | 4.84 (−4.65–14.33) | <0.001* |
| Lower-Body Strength (times) | 28.98 ± 5.08 | 28.58 ± 6.88 | −0.47 (−1.39–0.45) | 0.629 |
| Left Upper-Body Flexibility (cm) | 0.61 ± 5.68 | 1.11 ± 5.92 | 1.40 (−1.34–4.41) | 0.110 |
| Right Upper-Body Flexibility (cm) | 3.05 ± 5.38 | 3.10 ± 5.92 | 0.43 (−0.41–1.27) | 0.439 |
| Left Upper-Body Strength (times) | 29.44 ± 6.67 | 31.84 ± 7.11 | 2.31 (−2.21–6.83) | 0.053 |
| Right Upper-Body Strength (times) | 31.93 ± 6.45 | 34.00 ± 6.87 | 1.70 (−1.64–5.04) | 0.151 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zeng, N.; Liao, N.; Han, C.; Liu, W.; Gao, Z. Leveraging Fitness Tracker and Personalized Exercise Prescription to Promote Breast Cancer Survivors’ Health Outcomes: A Feasibility Study. J. Clin. Med. 2020, 9, 1775. https://doi.org/10.3390/jcm9061775
Zeng N, Liao N, Han C, Liu W, Gao Z. Leveraging Fitness Tracker and Personalized Exercise Prescription to Promote Breast Cancer Survivors’ Health Outcomes: A Feasibility Study. Journal of Clinical Medicine. 2020; 9(6):1775. https://doi.org/10.3390/jcm9061775
Chicago/Turabian StyleZeng, Nan, Ning Liao, Chunyuan Han, Wenxi Liu, and Zan Gao. 2020. "Leveraging Fitness Tracker and Personalized Exercise Prescription to Promote Breast Cancer Survivors’ Health Outcomes: A Feasibility Study" Journal of Clinical Medicine 9, no. 6: 1775. https://doi.org/10.3390/jcm9061775
APA StyleZeng, N., Liao, N., Han, C., Liu, W., & Gao, Z. (2020). Leveraging Fitness Tracker and Personalized Exercise Prescription to Promote Breast Cancer Survivors’ Health Outcomes: A Feasibility Study. Journal of Clinical Medicine, 9(6), 1775. https://doi.org/10.3390/jcm9061775






