1. Introduction
The patient with multiple injuries is a unique challenge for the trauma care team, even more so in association with spinal fractures. Traumatic spinal injuries in multiple-injured patients are less common in comparison to extremity injuries but present with an increasing incidence over the last decades [
1,
2]. Most of these injuries are located within the thoracic and lumbar spine and are accompanied by lung contusion and/or abdominal trauma [
3,
4]. Beside worse outcomes, a cost analysis showed that apart from injuries of the head, associated spinal lesions in multiple-injured patients result in higher hospitalisation costs and prolonged length of stay (LOS) [
5].
Controversy still arises concerning the optimal timing for spinal surgery in the multiple-injured patient. In the literature, the discussion has ultimately focused on the question of early versus late surgical treatment and its consequences on mortality and the patients’ outcome [
6,
7]. Recent register studies generally advocate that early spinal stabilization is beneficial for multiple-injured patients, mainly due to the increased possibility of early patient mobilisation in the ICU [
8]; however, these register studies do not differentiate the wide variety of different spinal injuries. For example, although AOSpine A-type fractures are managed surgically in some countries to maintain sagittal spinal balance, they are—from a biomechanical viewpoint—stable enough to tolerate early mobilisation in the ICU without the risk of neurological compromise. Therefore, a general recommendation to perform early spinal stabilization, which is definitely a surgical burden and second hit in this scenario, may not be justified, and may even jeopardize multiple-injured patients with biomechanically stable spinal injuries.
For this reason, the aim of the present study is to analyse the impact of the timing of spinal surgery in multiple-injured patients both in general and in respect to spinal injury severity.
2. Methods
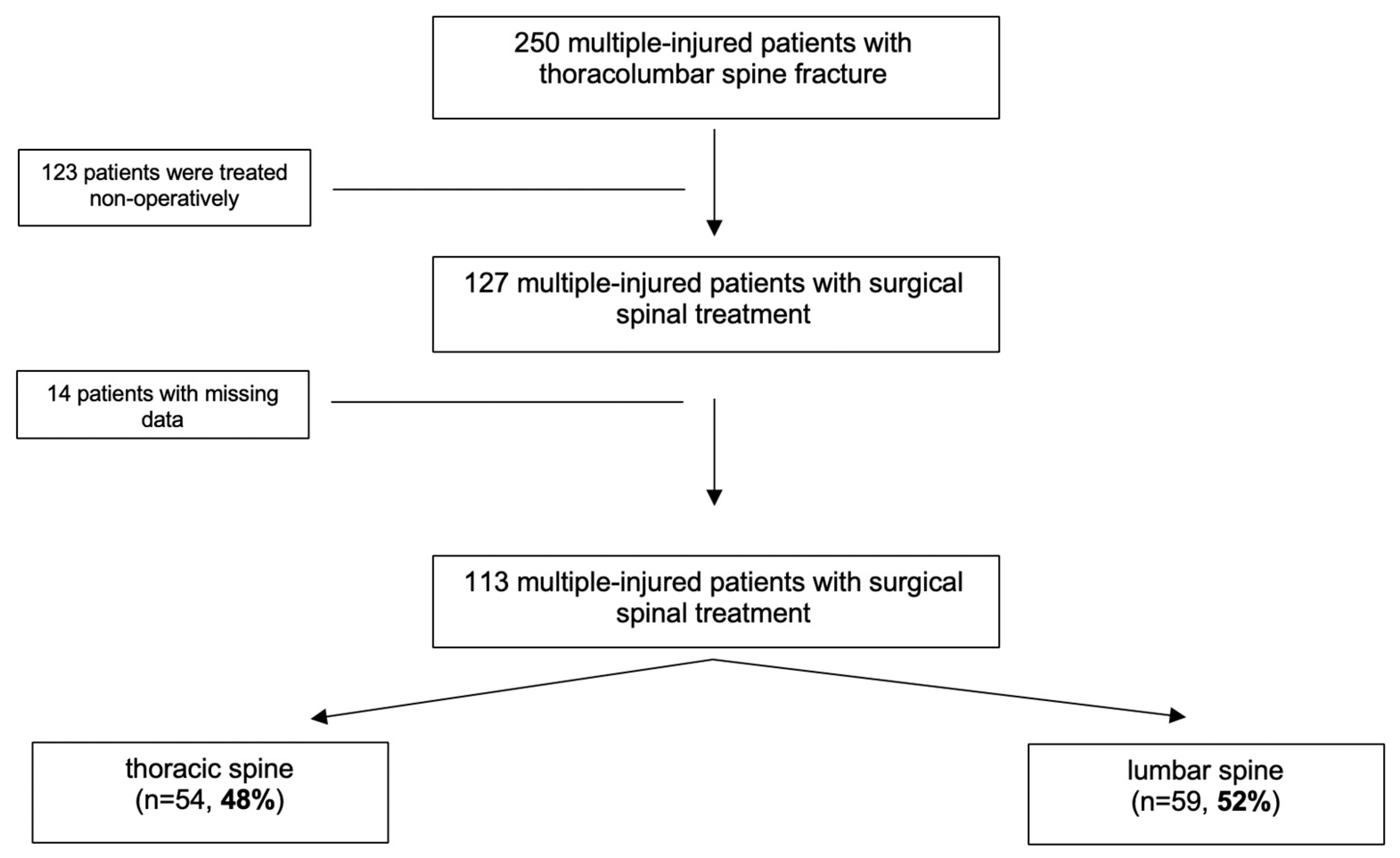
This retrospective two-centre study was conducted on all multiple-injured patients with spinal injuries who were admitted to one of the two level I trauma hospitals between January 2012 and December 2016. Patients were eligible for further analysis if they met the following inclusion criteria: age >16 years; injury severity score (ISS) >16; associated spinal injury within the thoracic or lumbar spine; and a fully available computed tomography scan for spinal injury classification, according to the established AOSpine Classification [
9]. Demographic data, circumstances of the accident, overall injury severity score (ISS), and time to spinal surgery (24, 72, and 96 h) were documented. Measured outcome parameters were duration of mechanical ventilation, intensive care unit (ICU) length of stay (iLOS), length of hospital stay (LOS), development of sepsis or multiple organ dysfunction syndrome (MODS), and death. Organ failure was defined according to the sequential organ failure assessment (SOFA) score: a value in one or more organ systems of ≥3 points was defined as single or multiple organ failure. Sepsis was defined as systemic inflammatory response syndrome (SIRS) combined with bacteraemia.
Data were collected from the inhouse clinical documentation system. Counts and frequencies were used to describe the sample. Correlation analysis (Spearman) was used to determine any dependence between the variables. For evaluation of influencing factors on the timing of surgery, a chi-square test and a one-way ANOVA was performed. Fisher’s exact test was used for categorical variables. Multivariable logistic regression analysis was performed using time to surgery, LOS, iLOS, and sepsis as dependent variables. Results are presented as odds ratios (ORs) with 95% confidence intervals. Significance was set at p < 0.05 for all statistical tests. A power analysis was carried out with G * Power (3.1.9.3, IBM) and resulted in the following statistical power for each statistical test: 0.998 for the ANOVA, 0.963 for the t-test, and 0.999 for both the correlation analysis and the regression analysis.
All testing procedures were performed exploratively, so no adjustment for multiple testing has been made. Statistical analyses were performed with IBM SPSS software (version 23; IBM Corp., Armonk, New York, NY, USA). The study complies with the principles of the Declaration of Helsinki (2013) and was approved by the local ethical committee (#EK056/17).
4. Discussion
The clinical course for multiple-injured patients is determined by the initial trauma (first hit), the initial surgical burden (second hit), and the resulting systemic inflammatory response [
10]. In contrast to the established damage control orthopedics (DCO) concept for long-bone fractures, which recommends performing a definite long-bone fracture stabilization later in the course of treatment, early definite spinal stabilization in multiple-injured patients is gaining increasing popularity in recent years [
11,
12]. This “spine damage control” concept advocates immediate posterior spinal stabilization in multiple-injured patients, with delayed anterior spinal stabilization, if required, later in the course [
11,
13]. Support of this concept is provided by several studies showing that early spinal stabilization in multiple-injured patients appears to be associated with a beneficial medical and socioeconomic outcome [
5,
8,
14,
15].
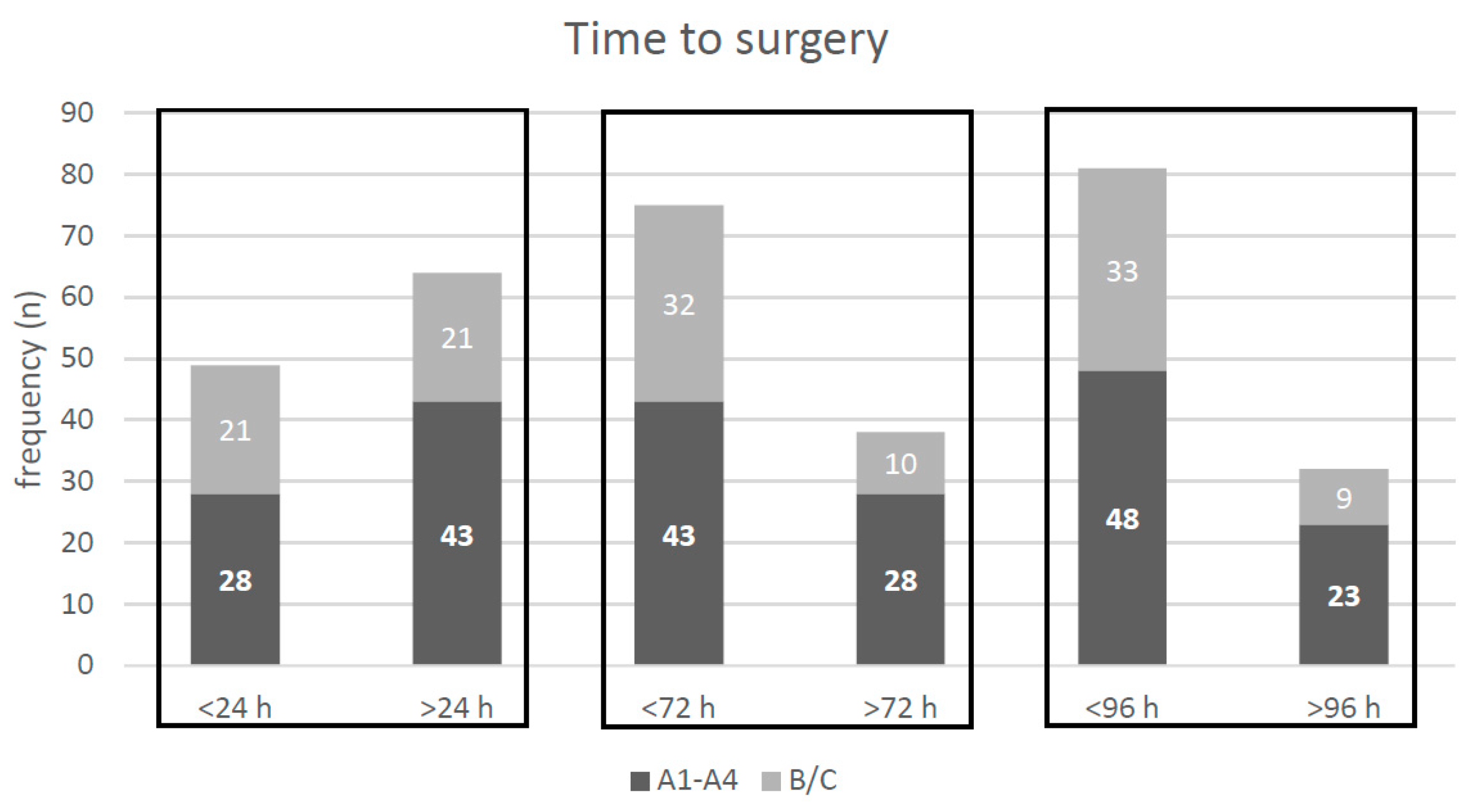
In general, our data support the concept of early posterior spinal stabilization in multiple-injured patients. Our data show that increasing time to spinal surgery in multiple-injured patients is an independent risk factor for an increased ICU and hospital stay, and that spinal stabilization later than 72 h is an independent risk factor for the development of sepsis. We consider immediate spinal stabilization, as advocated above, as spinal surgery within 24 h after trauma. Applying a 24 h cutoff to our patient population, we are able to show that multiple-injured patients with their spinal stabilization later than 24 h had, on average, a significantly longer stay of 7 days in the ICU, and a significantly longer length of hospital stay of 10 days, while having a comparable overall injury severity, as defined by the ISS, compared to those multiple-injured patients with spinal surgery within 24 h. Furthermore, the duration of mechanical ventilation was increased by approximately 30 h, and the prevalence of sepsis was significantly increased in the case of spinal stabilization later than 24 h. These adverse effects were even more pronounced for 72 h or 96 h as time cutoffs for spinal surgery. Several studies have attributed the beneficial effect of early spinal stabilization mainly to a better patient handling in the ICU, which allows, for example, for prone positioning for the improvement of pulmonary function, or even earlier in- or out-of-bed mobilization [
8]. Most of these studies, however, do not consider spinal injury severity from a biomechanical point of view. Thus, the above-mentioned reasons for a beneficial effect of early spinal stabilization may only be true for instable spinal injuries (AOSpine B-/C-type), because stable spinal injuries (AOSpine A-type) may be considered for early mobilization anyway.
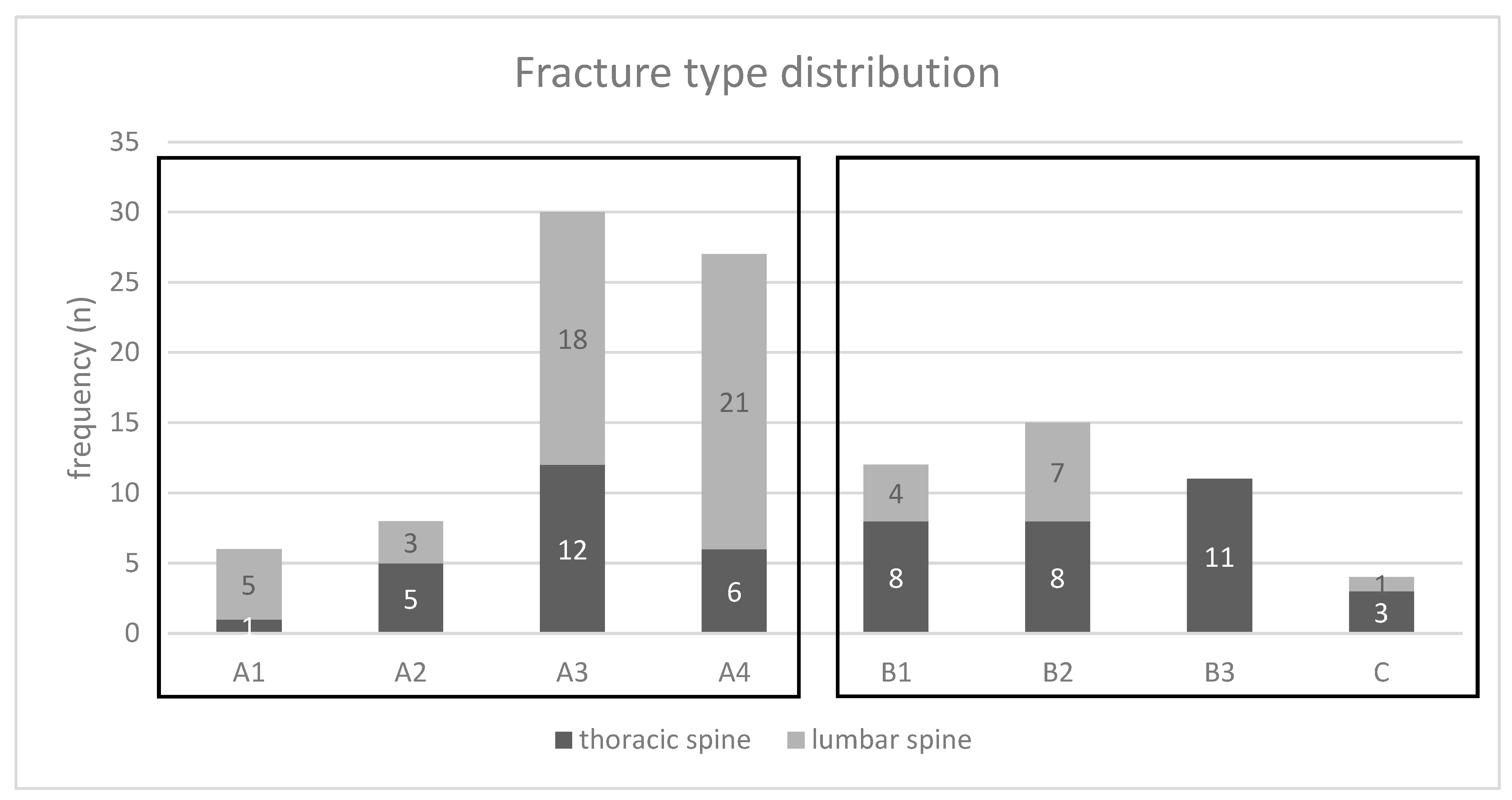
Therefore, the “spine damage control” concept has to be interpreted with caution and should not result in the recommendation that in multiple-injured patients, every spinal injury requiring surgery should be stabilized as early as possible at almost any cost. Further subgroup analyzation of our patient population supports a more individualized treatment concept, taking into account the degree of spinal injury stability, as described with the AOSpine classification. In multiple-injured patients with AOSpine B-/C-type spinal injuries, which from a biomechanical view are unstable spinal injuries, stabilization as early as possible appears to be beneficial. In these patients, prolonged time to spinal surgery is an independent risk factor for increased length of stay in the ICU and in hospital, as well as for the development of sepsis. In contrast to these findings, the benefit of an early spinal stabilization for multiple-injured patients with AOSpine A-type spinal injuries appears to be less pronounced. In these biomechanically stable spinal injuries, a prolonged time to spinal stabilization is only an independent risk factor for an increased length of hospital stay. Although we could not observe an adverse effect of the stabilization of AOSpine A-type spinal injuries in our multiple-injured patients, this observation reduces the pressure on the trauma team to deal with AOSpine A-type spinal injuries in the acute phase. Since AOSpine A-type injuries are the predominant spinal injury pattern in our multiple-injured patient population, this may have an important impact on trauma care in the future. Although a differentiation of the spinal injury, according to the AOSpine classification, is important for decisions with regard to surgical timing, the injury type in and of itself is not an independent risk factor for adverse outcomes.
Thoracic spinal injury location has been identified by other studies to adversely influence patients’ outcome [
16,
17]. Our data reveals that thoracic spinal injury location is an independent risk factor for prolonged ICU stay. This may be explained by two considerations. First, thoracic spinal injury location in our population is associated with delayed spinal stabilization, probably due to a higher grade of required surgical expertise. Secondly, thoracic spinal injuries are probably associated with a higher rate of thoracic injury (for example, lung contusions). In our population, multiple-injured patients with thoracic spinal injuries on average required 90 h more of mechanical ventilation than those multiple-injured patients with lumbar spinal injuries.
Our data show that in our patient population, almost half of the patients (47.8%) were surgically treated for their spinal injury within 24 h, and almost ¾ of the patients (71.7%) within 72 h. Within 24 h, 50% (21/42 patients) of the total AOSpine B-/C-type spinal injuries and 39% (28/71) of the total AOSpine A-type spinal injuries were surgically addressed; thus, the surgeons already recognized the higher surgical urgency of AOSpine B-/C-type injuries. Reasons for a delayed spinal stabilization appear to be multifactorial. Regression analysis identified, in particular, a higher ISS, thoracic spine injury location, A-type injuries, and the absence of an evident neurological deficit as independent risk factors for a delay in spinal surgery.
In our population, 31% of the multiple-injured patients (
n = 35) presented with neurological impairment due to their spinal trauma. In the literature, urgent surgical spinal treatment is widely accepted in the event of any neurological impairment focusing on isolated spine trauma. The main target is the decompression of the affected nerve structures and the restoration of the correct spinal alignment. The analysis of the STASCI (Surgical Timing in Acute Spinal Cord Injury) study showed that a general improvement of at least two ASIA (American Spinal Injury Association) grades is observable after early decompression within 24 h [
18,
19]. Our data show that even in multiple-injured patients with different priority surgeries, neurological impairment resulted in an earlier spinal surgery; however, we were not able to assess whether this had a beneficial impact on neurological outcome.
There are some limitations of our study, which merit further comments. Endpoint selection may not be meticulous enough to identify further differences between the treatment groups, and no in-depth information concerning patients’ comorbidities were available for analysis. The clinical course and outcome of multiple-injured patients are influenced by several factors, which might not all be included in our analysis. In particular, spinal trauma with neurological compromise might have a severe impact on outcome parameters of these multiple-injured patients, which might not be valued enough in our data due to early out-of-hospital transfer to neurological rehabilitation units.
Furthermore, the population size is limited as compared to register studies. However, this is the first study to consider spinal injury severity, according to the AOSpine classification, and to correlate this to the impact of surgical timing of spinal injuries. There are several existing fracture classification systems to evaluate the fracture pattern of spinal fractures. Advantages of the AOSpine fracture classification are better reliability and feasibility in clinical practice, in comparison to the thoracolumbar injury classification and severity score (TLICS). Several studies confirmed that the AOSpine classification is superior to the TLICS with regard to reliability for the identification of fracture morphology [
20,
21].
In conclusion, our data support the concept of early spinal stabilization within 24 h in multiple-injured patients with AOSpine B-/C-type injuries, especially of the thoracic spine. However, in multiple-injured patients with AOSpine A-type injuries, the beneficial impact of early spinal stabilization has been overemphasized in former studies, and the benefit should be weighed against the risk of patients’ deterioration, due to the unneglectable surgical burden of spinal surgery.