Impact of Improvement in Walking Speed on Hospitalization and Mortality in Females with Cardiovascular Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Clinical Follow-Up
2.3. Data Analysis
3. Results
3.1. Baseline Characteristics
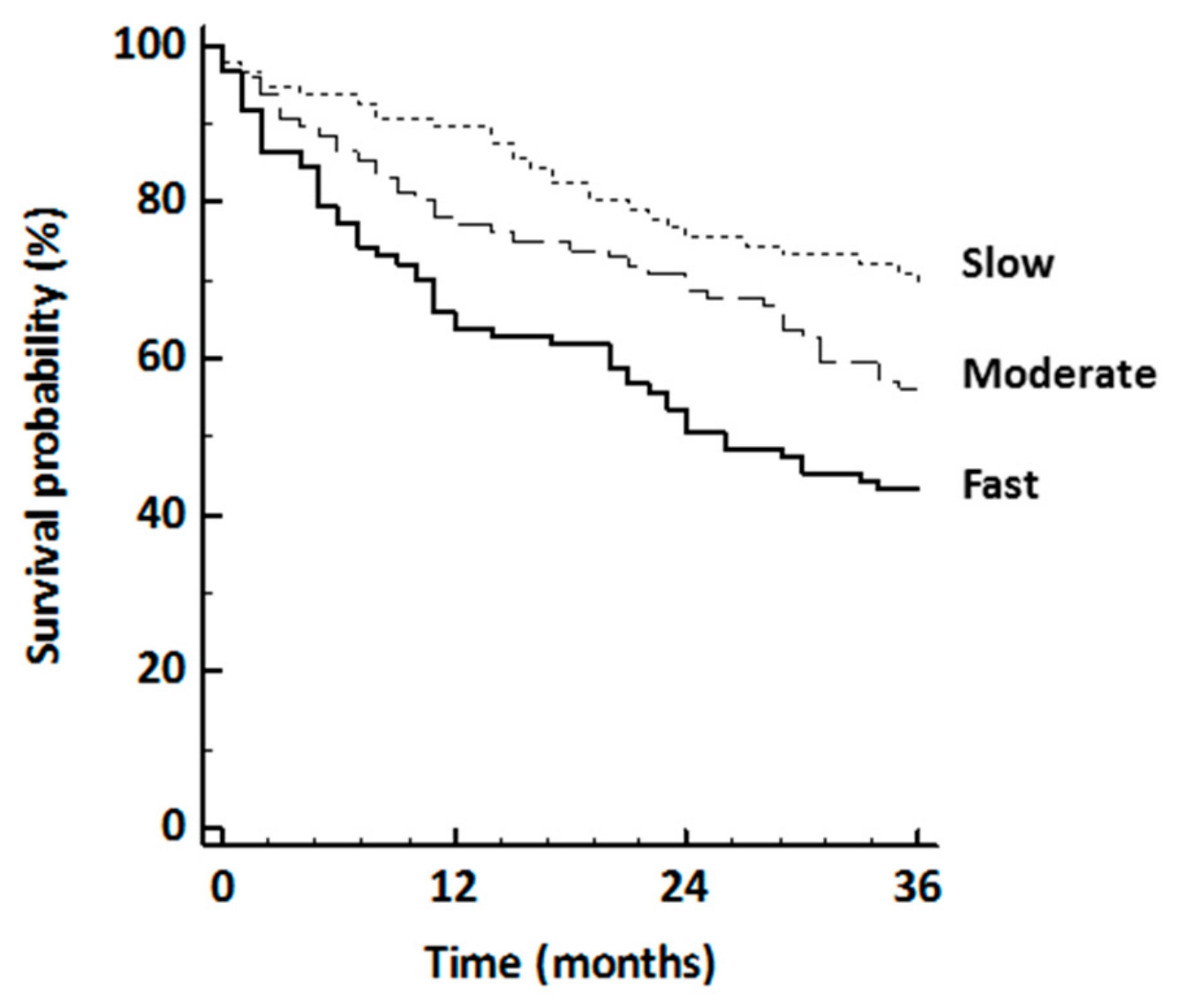
3.2. Baseline Walking Speed and 3-Year Hospitalization and Death
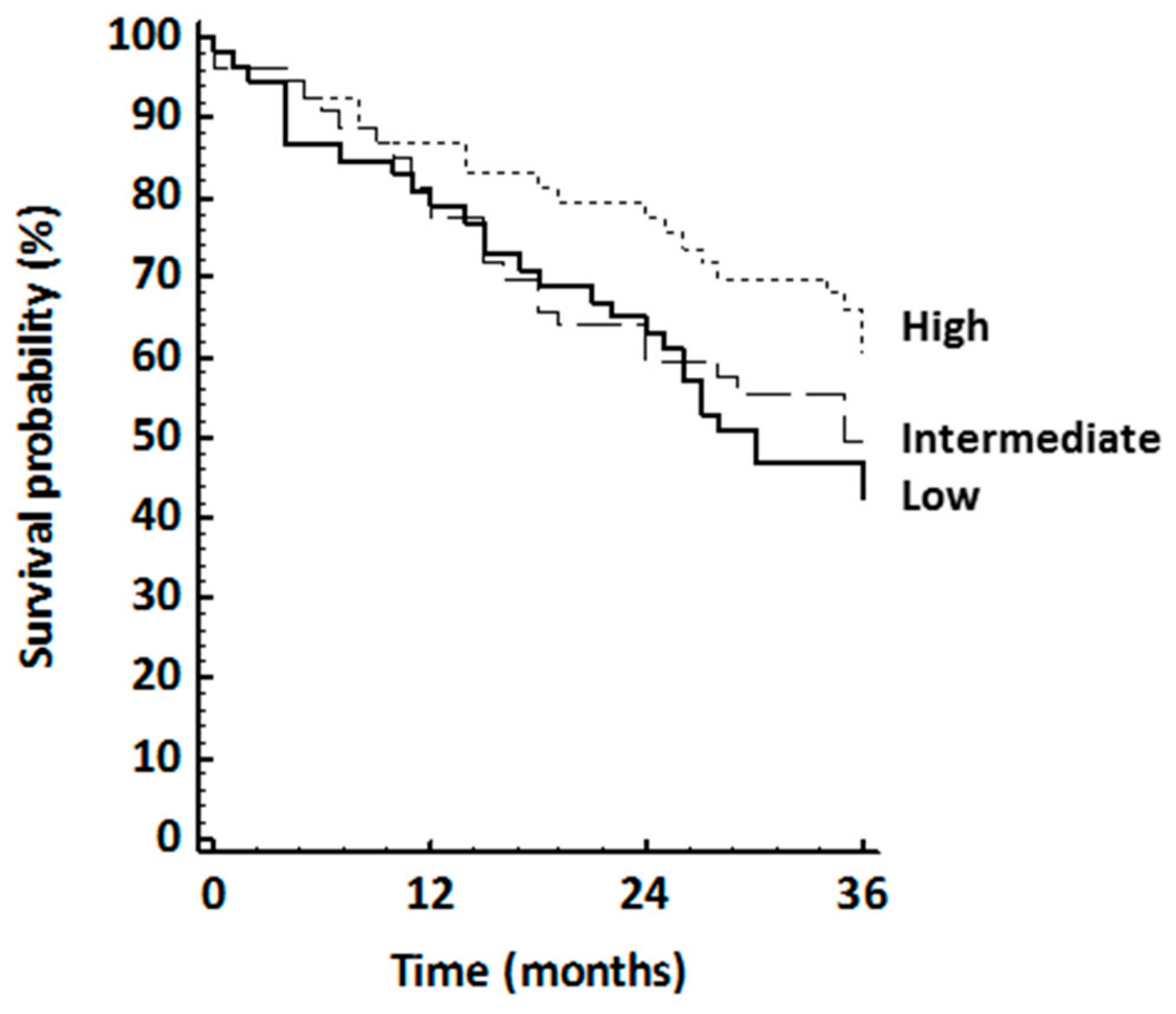
3.3. Walking Speed Changes and 4–6 Years’ Hospitalization or Death
4. Discussion
4.1. Strengths of the Study
4.2. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gulati, M. Improving the Cardiovascular Health of Women in the Nation. Moving Beyond the Bikini Boundaries. Circulation 2017, 135, 495–498. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Murphy, S.L.; Kochanek, K.D.; Bastian, B.A. Deaths: Final Data for 2013. Natl. Vital. Stat. Rep. 2016, 64(2), 1–119. [Google Scholar] [PubMed]
- Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. In American Association of Cardiovascular and Pulmonary Rehabilitation, 5th ed.; Human Kinetics: Champaign, IL, USA, 2013.
- Audelin, M.C.; Savage, P.D.; Ades, P.A. Changing clinical profile of patients entering cardiac rehabilitation/secondary prevention programs: 1996 to 2006. J. Cardiopulm. Rehabil. Prev. 2008, 28, 299–306. [Google Scholar] [CrossRef]
- Roger, V.L.; Go, A.S.; Lloyd-Jones, D.M.; Adams, R.J.; Berry, J.D.; Brown, T.M.; Carnethon, M.R.; Dai, S.; De Simone, G.; Ford, E.S.; et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2011 update: A report from the American Heart Association. Circulation 2011, 123, 18–209. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; De Ferranti, S.; Desprès, J.P.; Fullerton, H.J.; Howard, V.J.; et al. On behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics—2015 Update. A Report From the American Heart Association. Circulation 2015, 131, 29–322. [Google Scholar]
- Balady, G.J.; Williams, M.A.; Ades, P.A.; Bittner, V.; Comoss, P.; Foody, J.M.; Franklin, B.; Sanderson, B.; Southard, D.; American Heart Association Exercise; et al. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: A scientific statement from the American Heart Association and the American Association of Cardiovascular and Pulmonary Rehabilitation. J. Cardiopulm. Rehabil. Prev. 2007, 27, 21–129. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Corrà, U.; Benzer, W.; Bjarnason-Wehrens, B.; Dendale, P.; Gaita, G.; McGee, H.; Mendes, M.; Niebauer, J.; Zwisler, A.D.; et al. Secondary prevention through cardiac rehabilitation: From knowledge to implementation. A position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur. J. Cardiovasc. Prev. Rehabil. 2010, 17, 1–17. [Google Scholar] [CrossRef]
- Balady, G.J.; Ades, P.A.; Bittner, V.A.; Franklin, B.A.; Gordon, N.F.; Thomas, R.J.; Tomaselli, G.F.; Yancy, C.W.; American Heart Association Science Advisory and Coordinating Committee. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: A presidential advisory from the American Heart Association. Circulation 2011, 124, 2951–2960. [Google Scholar] [CrossRef]
- Gulati, M.; Black, H.R.; Shaw, L.J.; Arnsdorf, M.F.; Merz, C.N.; Lauer, M.S.; Marwick, T.H.; Pandey, D.K.; Wicklund, R.H.; Thisted, R.A. The prognostic value of a nomogram for exercise capacity in women. N. Engl. J. Med. 2005, 353, 468–475. [Google Scholar] [CrossRef]
- Myers, J.; Prakash, M.; Froelicher, V.; Do, D.; Partington, S.; Atwood, J.E. Exercise capacity and mortality among men referred for exercise testing. N. Engl. J. Med. 2002, 346, 793–801. [Google Scholar] [CrossRef]
- Simonsick, E.M.; Fan, E.; Fleg, J.L. Estimating cardiorespiratory fitness in well-functioning older adults: Treadmill validation of the long distance corridor walk. J. Am. Geriatr. Soc. 2006, 54, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Pober, D.M.; Freedson, P.S.; Kline, G.M.; McInnis, K.J.; Rippe, J.M. Development and validation of a one-mile treadmill walk test to predict peak oxygen uptake in healthy adults ages 40 to 79 years. Can. J. Appl. Physiol. 2002, 27, 575–588. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chaudhry, S.I.; McAvay, G.; Chen, S.; Whitson, H.; Newman, A.B.; Krumholz, H.M.; Gill, T.M. Risk factors for hospital admission among older persons with newly diagnosed heart failure: Findings from the Cardiovascular Health study. J. Am. Coll. Cardiol. 2013, 61, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Afilalo, J.; Eisenberg, M.J.; Morin, J.F.; Bergman, H.; Monette, J.; Noiseux, N.; Perrault, L.P.; Alexander, K.P.; Langlois, Y.; Dendukuri, N.; et al. Gait speed as an incremental predictor of mortality and major morbidity in elderly patients undergoing cardiac surgery. J. Am. Coll. Cardiol. 2010, 56, 1668–1676. [Google Scholar] [CrossRef] [PubMed]
- Sergi, G.; Veronese, N.; Fontana, L.; De Rui, M.; Bolzetta, F.; Zambon, S.; Corti, M.C.; Baggio, G.; Toffanello, E.D.; Crepaldi, G.; et al. Pre-frailty and risk of cardiovascular disease in elderly men and women: The prova. Study. J. Am. Coll. Cardiol. 2015, 65, 976–983. [Google Scholar] [CrossRef]
- Rolland, Y.; Lauwers-Cances, V.; Cesari, M.; Vellas, B.; Pahor, M.; Grandjean, H. Physical performance measures as predictors of mortality in a cohort of community-dwelling older French women. Eur. J. Epidemiol. 2006, 21, 113–122. [Google Scholar] [CrossRef]
- More People Walk to Better Health. In CDC Vital Signs; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2012. Available online: http://www.cdc.gov/vitalsigns/pdf/2012-08-vitalsigns.pdf.
- Booth, M.L.; Bauman, A.; Owen, N.; Gore, C.J. Physical Activity Preferences, Preferred Sources of Assistance, and Perceived Barriers to Increased Activity among Physically Inactive Australians. Prev. Med. 1997, 26, 131–137. [Google Scholar] [CrossRef]
- Chiaranda, G.; Myers, J.; Mazzoni, G.; Terranova, F.; Bernardi, E.; Grossi, G.; Codecà, L.; Conconi, F.; Grazzi, G. Peak oxygen uptake prediction from a moderate, perceptually regulated, 1-km treadmill walk in Male cardiac patients. J. Cardiopulm. Rehabil. Prev. 2012, 32, 262–269. [Google Scholar] [CrossRef]
- Grazzi, G.; Chiaranda, G.; Myers, J.; Pasanisi, G.; Lordi, R.; Conconi, F.; Mazzoni, G. Outdoor reproducibility of a 1-km treadmill-walking test to predict peak oxygen consumption in cardiac outpatients. J. Cardiopulm. Rehab. Prev. 2017, 37, 347–349. [Google Scholar] [CrossRef]
- Chiaranda, G.; Bernardi, E.; Codecà, L.; Conconi, F.; Myers, J.; Terranova, F.; Volpato, S.; Mazzoni, G.; Grazzi, G. Treadmill walking speed and survival prediction in men with cardiovascular disease: A 10-year follow-up study. BMJ Open 2013, 3. [Google Scholar] [CrossRef]
- Grazzi, G.; Myers, J.; Bernardi, E.; Terranova, F.; Grossi, G.; Codecà, L.; Volpato, S.; Conconi, F.; Mazzoni, G.; Chiaranda, G. Association between VO2peak estimated by a 1-km treadmill walk and mortality. A 10-year follow-up study in patients with cardiovascular disease. Int. J. Cardiol. 2014, 173, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Sorino, N.; Merlo, C.; Myers, J.; Sassone, B.; Pasanisi, G.; Mandini, S.; Mazzoni, G.; Chiaranda, G.; Grazzi, G. Inverse association between mortality and estimated functional capacity in hypertensive male outpatients with established coronary artery disease. G. Ital. Cardiol. 2018, 19, 648–654. [Google Scholar]
- Steffen-Batey, L.; Nichaman, M.Z.; Goff, D.C., Jr.; Frankowski, R.F.; Hanis, C.L.; Ramsey, D.J.; Labarthe, D.R. Change in level of physical activity and risk of all-cause mortality or reinfarction: The corpus christi heart project. Circulation 2000, 102, 2204–2209. [Google Scholar] [CrossRef] [PubMed]
- Martin, B.J.; Arena, R.; Haykowsky, M.; Hauer, T.; Austford, L.D.; Knudtson, M.; Aggarwal, S.; Stone, J.A.; APPROACH Investigators. Cardiovascular fitness and mortality after contemporary cardiac rehabilitation. Mayo. Clin. Proc. 2013, 88, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Sherman, S.E.; Reuben, D. Measures of functional status in community-dwelling elders. J. Gen. Intern. Med. 1998, 13, 817–823. [Google Scholar] [CrossRef][Green Version]
- Matsuzawa, Y.; Konishi, M.; Akiyama, E.; Suzuki, H.; Nakayama, N.; Kiyokuni, M.; Sumita, S.; Ebina, T.; Kosuge, M.; Hibi, K.; et al. Association between gait speed as a measure of frailty and risk of cardiovascular events after myocardial infarction. J. Am. Coll. Cardiol. 2013, 61, 1964–1972. [Google Scholar] [CrossRef] [PubMed]
- Beatty, A.L.; Schiller, N.B.; Whooley, M.A. Six-Minute Walk Test as a Prognostic Tool in Stable Coronary Heart Disease. Arch. Int. Med. 2012, 172, 1096–1102. [Google Scholar] [CrossRef]
- Shah, M.R.; Hasselblad, V.; Gheorghiade, M.; Adams, K.F., Jr.; Swedberg, K.; Califf, R.M.; O’Connor, C.M. Prognostic usefulness of the six-minute walk in patients with advanced congestive heart failure secondary to ischemic or non-ischemic cardiomyopathy. Am. J. Cardiol. 2001, 88, 987–993. [Google Scholar] [CrossRef]
- Zaccardi, F.; Franks, P.W.; Dudbridge, F.; Davies, M.J.; Khunti, K.; Yates, T. Mortality risk comparing walking pace to handgrip strength and a healthy lifestyle: A UK Biobank study. Eur. J. Prev. Cardiol. 2019, 12. [Google Scholar] [CrossRef]
- Fritz, S.; Lusardi, M. White paper: ‘Walking speed: The sixth vital sign’. J. Geriatr. Phys. Ther. 2009, 32, 46–49. [Google Scholar] [CrossRef]
- Fletcher, G.F.; Landolfo, C.; Niebauer, J.; Ozemek, C.; Arena, R.; Lavie, C.J. Promoting physical activity and exercise: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 1622–1639. [Google Scholar] [CrossRef]
- Hermansen, R.; Jacobsen, B.K.; Lochen, M.L.; Morseth, B. Leisure time and occupational physical activity, resting heart rate and mortality in the Arctic region of Norway: The Finnmark Study. Eur. J. Prev. Cardiol. 2019, 26, 1636–1644. [Google Scholar] [CrossRef] [PubMed]
- Verhoog, S.; Saner, H. Walking pace: Don’t hurry, be active. Eur. J. Prev. Cardiol. 2019. [CrossRef] [PubMed]
- Veronese, N.; Stubbs, B.; Volpato, S.; Zuliani, G.; Maggi, S.; Cesari, M.; Lipnicki, D.M.; Smith, L.; Schoefield, P.; Firth, J.; et al. Association between gait speed with mortality, cardiovascular disease and cancer: A systematic review and meta-analysis of prospective cohort studies. J. Am. Med. Dir. Assoc. 2018, 19, 981–988. [Google Scholar] [CrossRef] [PubMed]
- Corrà, U.; Piepoli, F.M.; Carré, F.; Heuschmann, P.; Hoffmann, U.; Verschuren, M.; Halcox, J.; Giannuzzi, P.; Saner, H.; Wood, D.; et al. Secondary prevention through cardiac rehabilitation: Physical activity counselling and exercise training: Key components of the position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur. Heart J. 2010, 31, 1967–1974. [Google Scholar]
- Wilson, M.G.; Ellison, G.M.; Cable, N.T. Basic science behind the cardiovascular benefits of exercise. Heart 2015, 101, 758–765. [Google Scholar] [CrossRef]
- Rosano, C.; Brach, J.; Studenski, S.; Longstreth, W.T.; Newman, A.B. Gait variability is associated with subclinical brain vascular abnormalities in high-functioning older adults. Neuroepidemiology 2007, 29, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Heald, C.L.; Fowkes, F.G.; Murray, G.D.; Price, J.F.; Ankle Brachial Index Collaboration. Risk of mortality and cardiovascular disease associated with the ankle-brachial index: Systematic review. Atherosclerosis 2006, 189, 61–69. [Google Scholar] [CrossRef]
- Onen, F.; Henry-Feugeas, M.C.; Roy, C.; Baron, G.; Ravaud, P. Mobility decline of unknown origin in mild cognitive impairment: An MRI-based clinical study of the pathogenesis. Brain Res. 2008, 1222, 79–86. [Google Scholar] [CrossRef]
| All Subjects | Slow | Moderate | Fast | p Value | |
|---|---|---|---|---|---|
| n | 290 | 97 | 96 | 97 | |
| Walking speed (km/h) | 3.1 (0.9) | 2.1 (0.4) | 3.1 (0.3) | 4.3 (0.6) | - |
| Demographics | |||||
| Age | 65 (10) | 71 (7) | 65 (10) | 60 (10) | <0.001 |
| BMI | 26.4 (4.1) | 27.2 (5.1) | 26.4 (3.9) | 25.7 (3.1) | 0.06 |
| LV ejection fraction (%) | 59 (9) | 59 (9) | 59 (10) | 59 (9) | 0.9 |
| Risk factor | |||||
| Current smoking (%) | 9 | 1 | 8 | 9 | 0.2 |
| Hypertension (%) | 72 | 75 | 77 | 64 | 0.09 |
| Family history (%) | 46 | 44 | 38 | 55 | 0.06 |
| Fasting glucose (mg/dL) | 104 (27) | 105 (32) | 107 (29) | 99 (20) | 0.3 |
| Total cholesterol (mg/dL) | 211 (49) | 214 (58) | 216 (49) | 204 (39) | 0.3 |
| HDL cholesterol (mg/dL) | 51 (14) | 56 (14) | 56 (14) | 57 (15) | 0.8 |
| Triglycerides (mg/dL) | 135 (76) | 134 (69) | 155 (99) | 121 (57) | 0.04 |
| Serum creatinine (mg/dL) | 0.98 (0.33) | 1.01 (0.25) | 0.99 (0.46) | 0.93 (0.23) | 0.4 |
| Medical history (%) | |||||
| CABG | 40 | 46 | 46 | 26 | 0.03 |
| Myocardial infarction | 18 | 6 | 14 | 34 | <0.0001 |
| PTCA | 9 | 6 | 10 | 9 | 0.5 |
| Valvular repair/replacement | 29 | 37 | 27 | 22 | 0.06 |
| Other | 2 | 2 | 1 | 4 | 0.4 |
| Medications (%) | |||||
| ACE inhibitor or ARB | 53 | 58 | 60 | 40 | 0.006 |
| Aspirin | 63 | 57 | 65 | 68 | 0.2 |
| β-blockers | 52 | 44 | 56 | 57 | 0.2 |
| Calcium antagonists | 15 | 17 | 14 | 12 | 0.3 |
| Diuretics | 28 | 45 | 28 | 11 | <0.0001 |
| Statins | 46 | 41 | 45 | 51 | 0.4 |
| All (n = 176) | Low Improvement (n = 59) | Moderate Improvement (n = 60) | High Improvement (n = 57) | p Value | |
|---|---|---|---|---|---|
| Walking speed improvement from baseline (km/h) | 0.7 (0.6) | 0.1 (0.3) | 0.7 (0.2) | 1.5 (0.4) | - |
| General | |||||
| Age | 65 (9) | 66 (10) | 65 (8) | 63 (9) | 0.18 |
| BMI | 26.6 (3.8) | 27.7 (3.6) | 26.4 (4.1) | 26.8 (3.8) | 0.85 |
| LV ejection fraction (%) | 59 (9) | 60 (11) | 59 (8) | 59 (10) | 0.88 |
| Risk factor | |||||
| Current smoking (%) | 4 | 5 | 5 | 2 | 0.71 |
| Hypertension (%) | 76 | 80 | 74 | 72 | 0.52 |
| Family history (%) | 45 | 38 | 53 | 45 | 0.29 |
| Fasting glucose (mg/dL) | 104 (24) | 99 (20) | 103 (22) | 109 (28) | 0.28 |
| Total cholesterol (mg/dL) | 213 (50) | 207 (40) | 219 (60) | 214 (49) | 0.53 |
| HDL cholesterol (mg/dL) | 57 (13) | 59 (13) | 54 (12) | 57 (14) | 0.32 |
| Triglycerides (mg/dL) | 125 (57) | 117 (44) | 127 (58) | 130 (66) | 0.62 |
| Serum creatinine (mg/dL) | 0.97 (0.3) | 0.99 (0.2) | 0.95 (0.3) | 0.97 (0.3) | 0.81 |
| Medical history | |||||
| CABG (%) | 48 | 51 | 42 | 53 | 0.46 |
| Myocardial infarction (%) | 15 | 15 | 19 | 9 | 0.39 |
| PTCA (%) | 6 | 6 | 8 | 4 | 0.69 |
| Valvular replacement (%) | 29 | 28 | 30 | 28 | 0.06 |
| Other (%) | 1 | 0 | 0 | 2 | 0.41 |
| Medications | |||||
| ACE inhibitor or ARB (%) | 52 | 51 | 47 | 58 | 0.48 |
| Aspirin (%) | 63 | 62 | 66 | 60 | 0.77 |
| β-blockers (%) | 52 | 42 | 57 | 57 | 0.21 |
| Calcium antagonists (%) | 18 | 21 | 21 | 11 | 0.34 |
| Diuretics (%) | 24 | 25 | 21 | 26 | 0.39 |
| Statins (%) | 50 | 49 | 51 | 49 | 0.98 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grazzi, G.; Mazzoni, G.; Myers, J.; Caruso, L.; Sassone, B.; Pasanisi, G.; Guerzoni, F.; Napoli, N.; Pizzolato, M.; Zerbini, V.; et al. Impact of Improvement in Walking Speed on Hospitalization and Mortality in Females with Cardiovascular Disease. J. Clin. Med. 2020, 9, 1755. https://doi.org/10.3390/jcm9061755
Grazzi G, Mazzoni G, Myers J, Caruso L, Sassone B, Pasanisi G, Guerzoni F, Napoli N, Pizzolato M, Zerbini V, et al. Impact of Improvement in Walking Speed on Hospitalization and Mortality in Females with Cardiovascular Disease. Journal of Clinical Medicine. 2020; 9(6):1755. https://doi.org/10.3390/jcm9061755
Chicago/Turabian StyleGrazzi, Giovanni, Gianni Mazzoni, Jonathan Myers, Lorenzo Caruso, Biagio Sassone, Giovanni Pasanisi, Franco Guerzoni, Nicola Napoli, Matteo Pizzolato, Valentina Zerbini, and et al. 2020. "Impact of Improvement in Walking Speed on Hospitalization and Mortality in Females with Cardiovascular Disease" Journal of Clinical Medicine 9, no. 6: 1755. https://doi.org/10.3390/jcm9061755
APA StyleGrazzi, G., Mazzoni, G., Myers, J., Caruso, L., Sassone, B., Pasanisi, G., Guerzoni, F., Napoli, N., Pizzolato, M., Zerbini, V., Franchi, M., Masotti, S., Mandini, S., Raisi, A., & Chiaranda, G. (2020). Impact of Improvement in Walking Speed on Hospitalization and Mortality in Females with Cardiovascular Disease. Journal of Clinical Medicine, 9(6), 1755. https://doi.org/10.3390/jcm9061755





