Return to Sport Activity in the Elderly Patients after Unicompartmental Knee Arthroplasty: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Criteria for Considering Studies for This Review
2.2. Primary Outcome Measures
2.3. Secondary Outcome Measures
2.4. Search Strategy for Study Identification
2.5. Data Collection and Analysis
2.6. Risk of Bias Assessment
2.7. Quantitative Analysis
3. Results
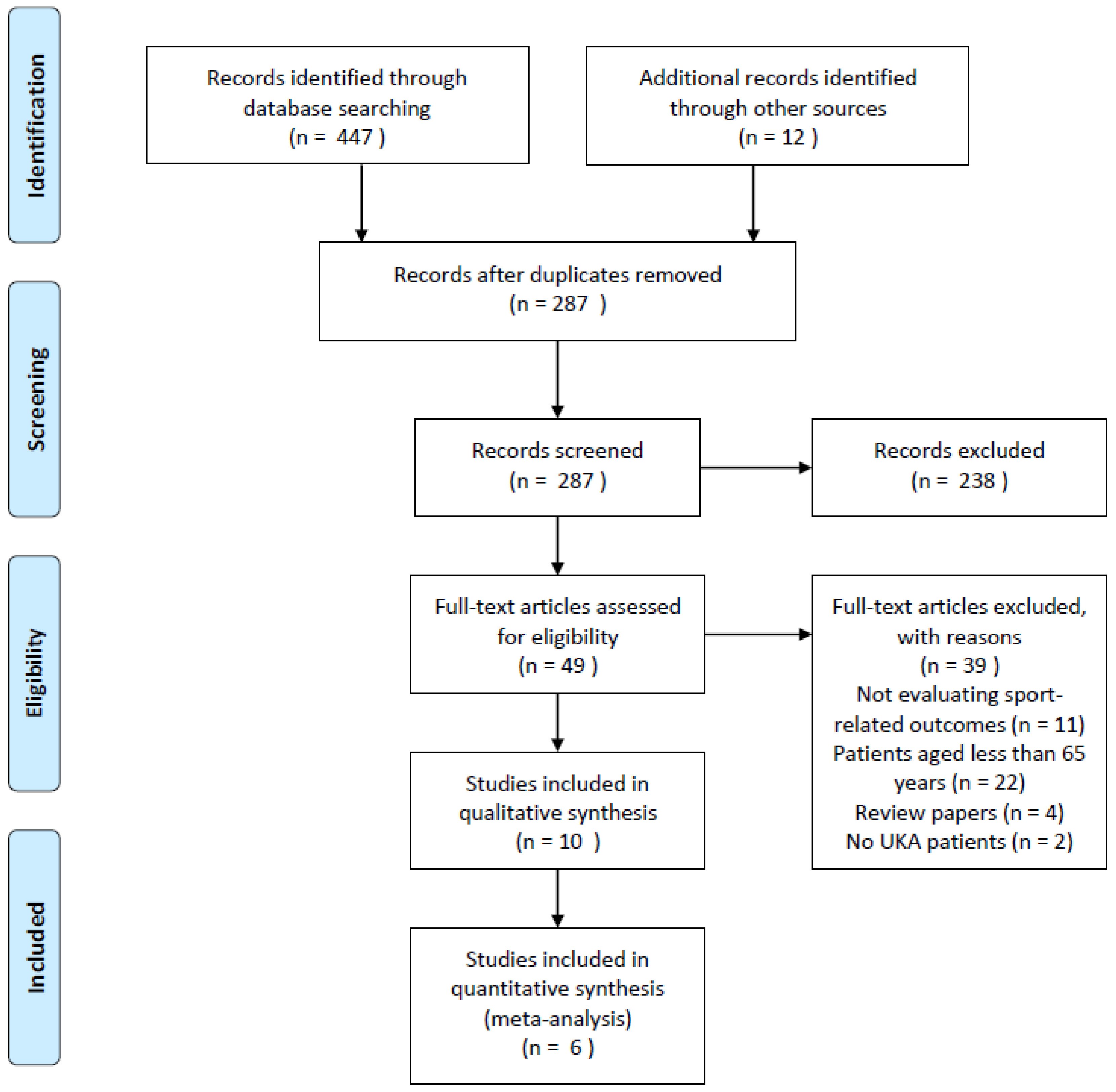
3.1. Research Results
3.2. Included and Excluded Studies
3.3. Demographic Results
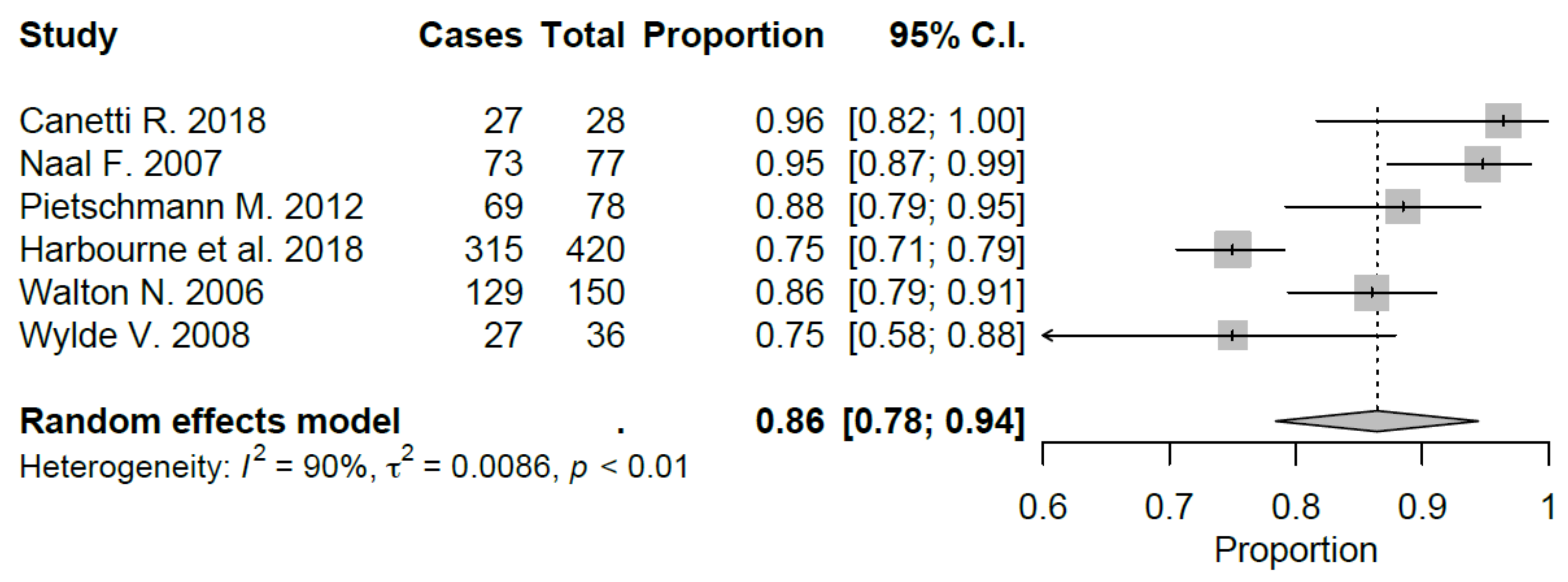
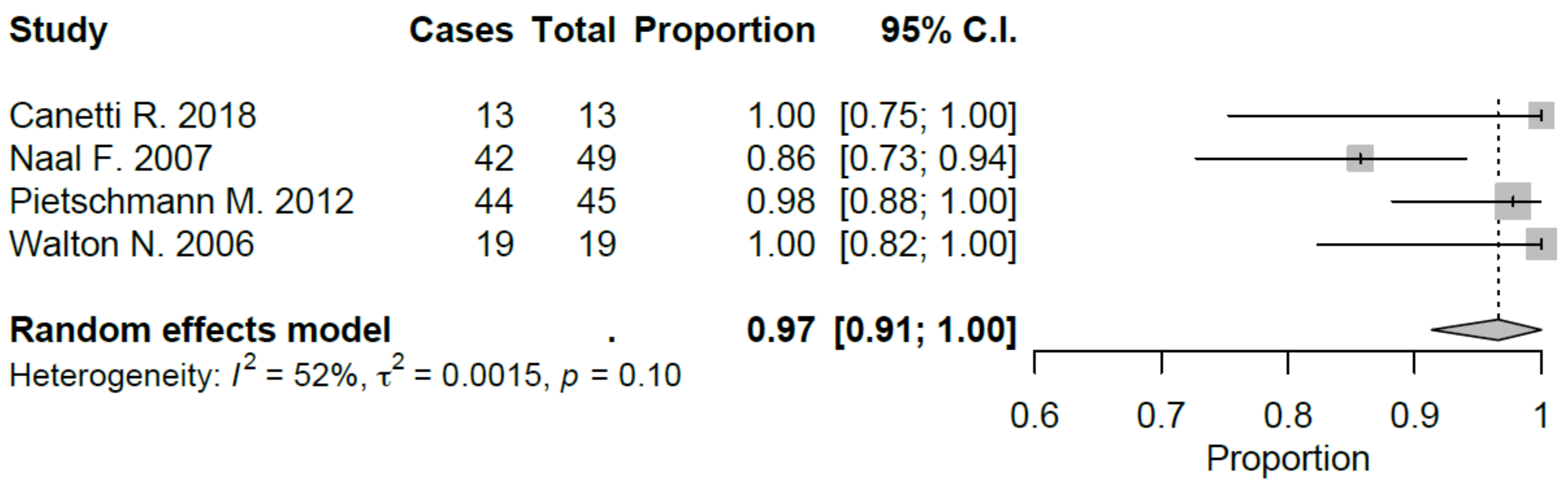
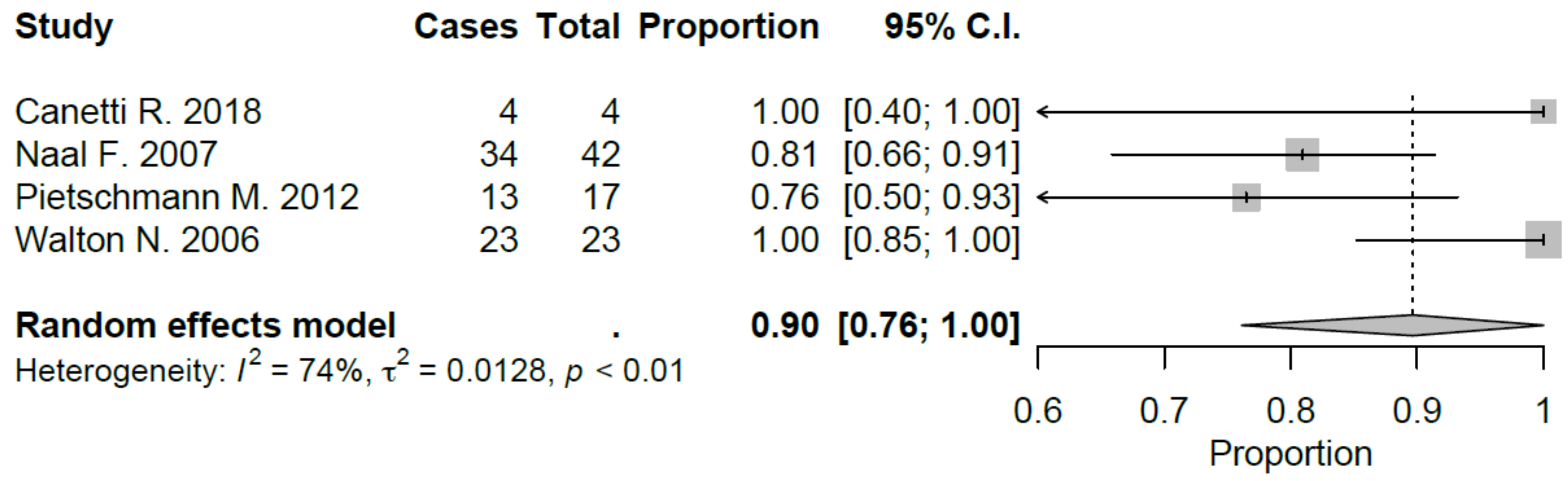
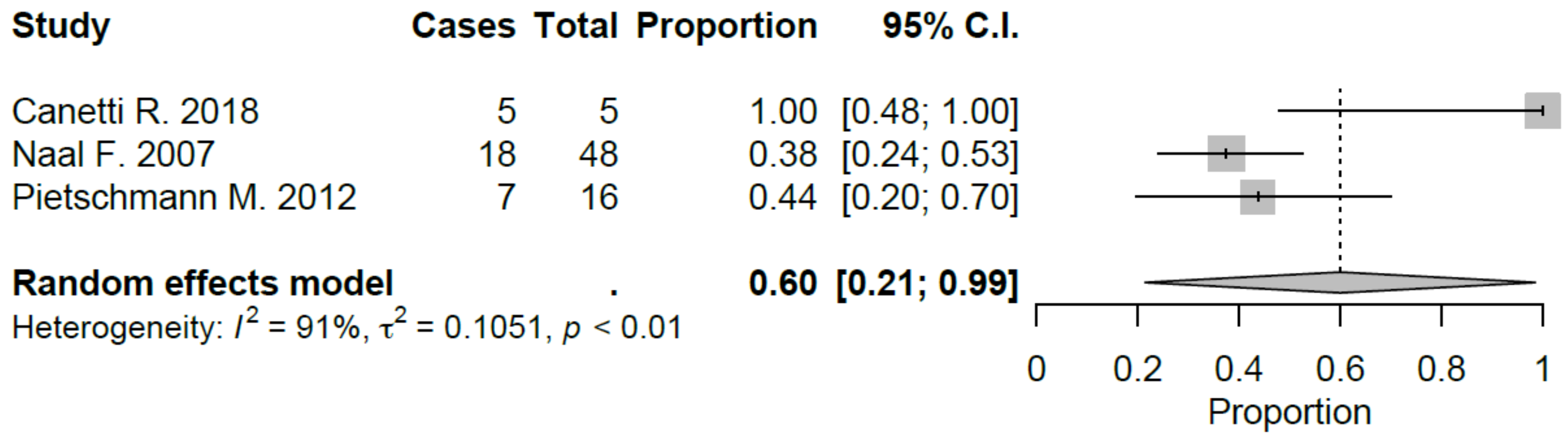
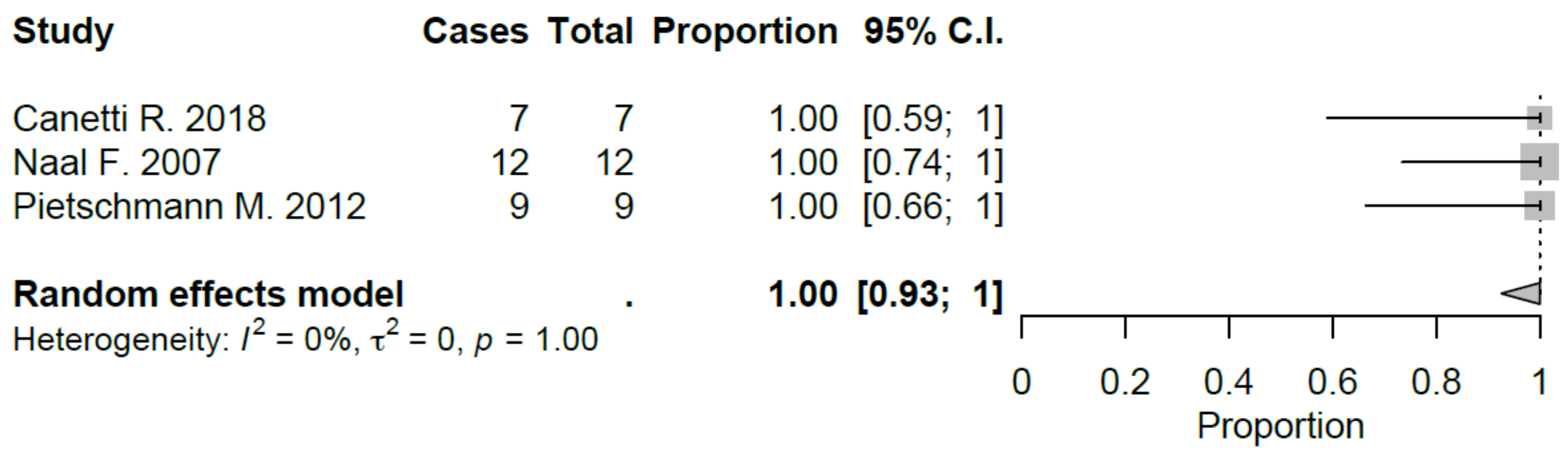
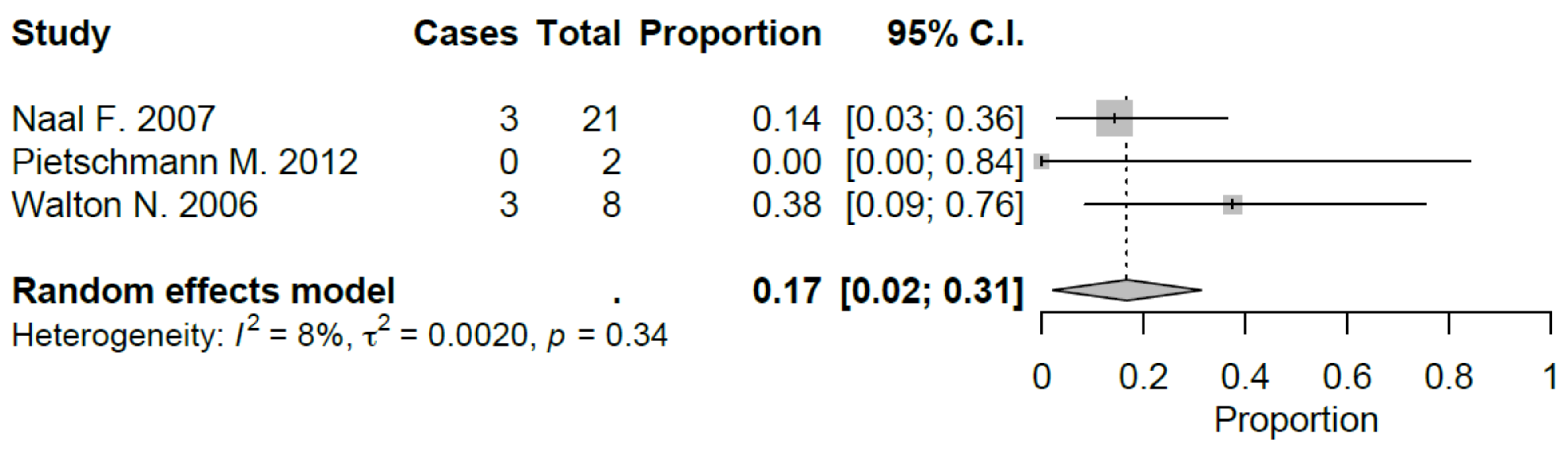
3.4. Return to Sport Activity
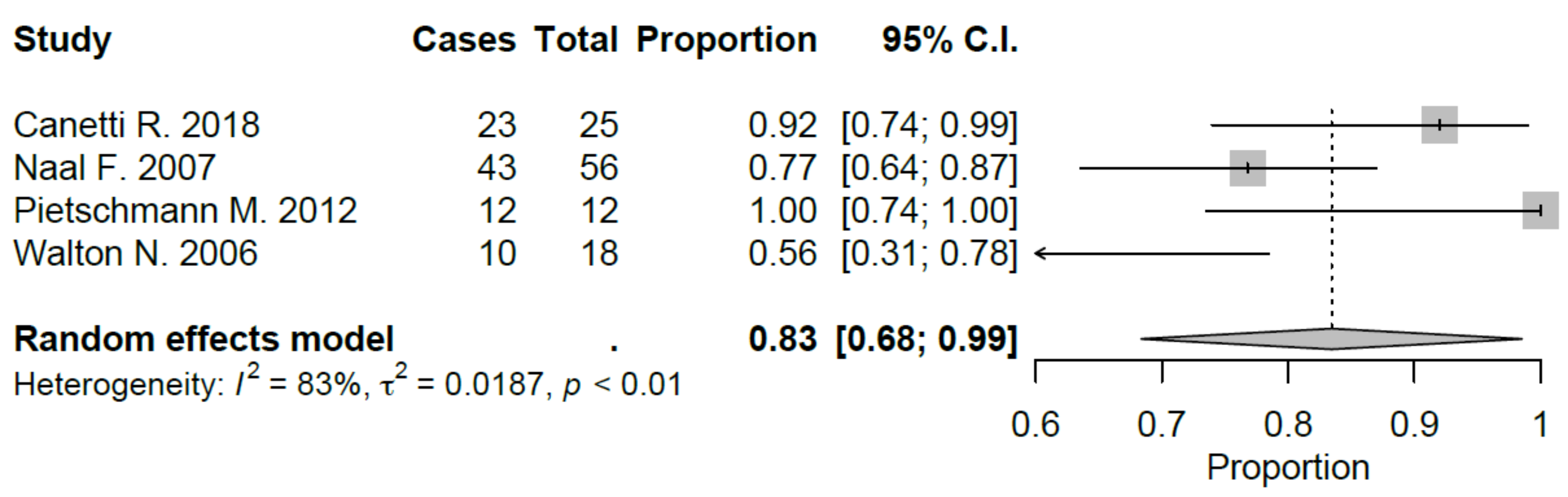
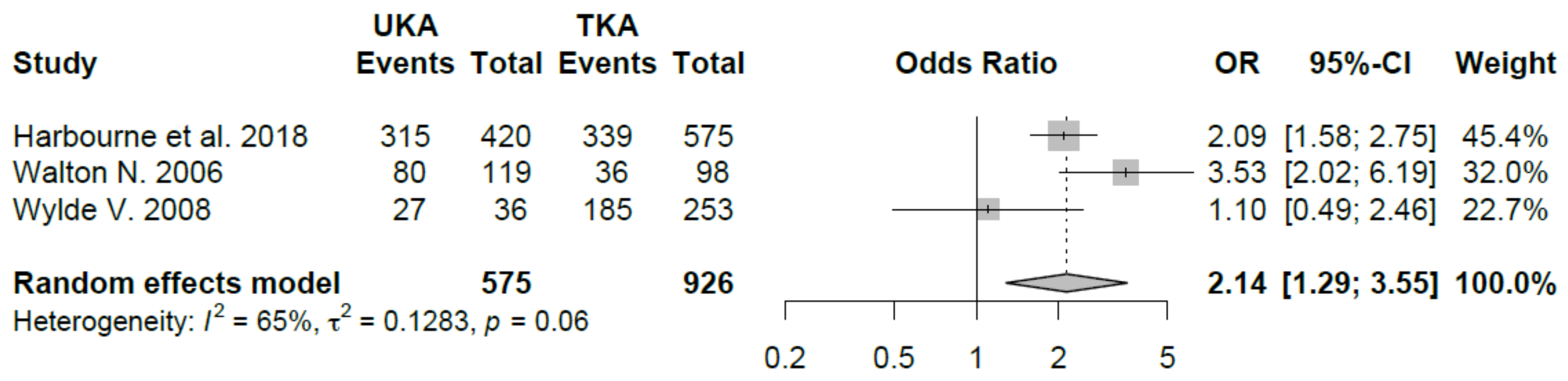
3.5. Comparison with TKA
3.6. Clinical Outcome Data
3.7. Clinical Outcome Data UKA vs. TKA
3.8. Quality Assessment (MINORS)
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dieppe, P.; Basler, H.; Chard, J.; Croft, P.; Dixon, J.; Hurley, M.; Lohmander, S.; Raspe, H. Knee replacement surgery for osteoarthritis: Effectiveness, practice variations, indications and possible determinants of utilization. Rheumatology (Oxf. Engl.) 1999, 38, 73–83. [Google Scholar] [CrossRef]
- Felson, D.T.; Naimark, A.; Anderson, J.; Kazis, L.; Castelli, W.; Meenan, R.F. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. Off. J. Am. Coll. Rheumatol. 1987, 30, 914–918. [Google Scholar] [CrossRef] [PubMed]
- Hunter, D.J.; Bierma-zeinstra, S. Osteoarthritis. Lancet 2019, 393, 1745–1759. [Google Scholar] [CrossRef]
- Dunlop, D.D.; Song, J.; Semanik, P.A.; Chang, R.W.; Sharma, L.; Bathon, J.M.; Eaton, C.B.; Hochberg, M.C.; Jackson, R.D.; Kwoh, C.K. Objective physical activity measurement in the osteoarthritis initiative: Are guidelines being met? Arthritis Rheum. 2011, 63, 3372–3382. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.; Ettinger, W.; Neuhaus, J.; Mallon, K. Knee osteoarthritis and physical functioning: Evidence from the NHANES I Epidemiologic Followup Study. J. Rheumatol. 1991, 18, 591–598. [Google Scholar] [PubMed]
- Ettinger, W.H., Jr.; Fried, L.P.; Harris, T.; Shemanski, L.; Schulz, R.; Robbins, J.; Group, C.C.R. Self-reported causes of physical disability in older people: The Cardiovascular Health Study. J. Am. Geriatr. Soc. 1994, 42, 1035–1044. [Google Scholar] [CrossRef] [PubMed]
- Ethgen, O.; Bruyère, O.; Richy, F.; Dardennes, C.; Reginster, J.-Y. Health-related quality of life in total hip and total knee arthroplasty: A qualitative and systematic review of the literature. JBJS 2004, 86, 963–974. [Google Scholar] [CrossRef] [PubMed]
- Cartier, P.; Khefacha, A.; Sanouiller, J.-L.; Frederick, K. Unicondylar knee arthroplasty in middle-aged patients: A minimum 5-year follow-up. Orthopedics 2007, 30, 62. [Google Scholar]
- Pandit, H.; Gulati, A.; Jenkins, C.; Barker, K.; Price, A.; Dodd, C.; Murray, D. Unicompartmental knee replacement for patients with partial thickness cartilage loss in the affected compartment. Knee 2011, 18, 168–171. [Google Scholar] [CrossRef]
- Naal, F.D.; Fischer, M.; Preuss, A.; Goldhahn, J.; von Knoch, F.; Preiss, S.; Munzinger, U.; Drobny, T. Return to sports and recreational activity after unicompartmental knee arthroplasty. Am. J. Sports Med. 2007, 35, 1688–1695. [Google Scholar] [CrossRef]
- Papalia, R.; Del Buono, A.; Zampogna, B.; Maffulli, N.; Denaro, V. Sport activity following joint arthroplasty: A systematic review. Br. Med Bull. 2012, 101, 81. [Google Scholar] [CrossRef] [PubMed]
- Blair, S.; Sallis, R.; Hutber, A.; Archer, E. Exercise therapy–the public health message. Scand. J. Med. Sci. Sports 2012, 22, e24–e28. [Google Scholar] [CrossRef] [PubMed]
- Kohl, H.W., 3rd; Craig, C.L.; Lambert, E.V.; Inoue, S.; Alkandari, J.R.; Leetongin, G.; Kahlmeier, S.; Group, L.P.A.S.W. The pandemic of physical inactivity: Global action for public health. Lancet 2012, 380, 294–305. [Google Scholar] [CrossRef]
- Haskell, W.L.; Lee, I.-M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Macera, C.A.; Heath, G.W.; Thompson, P.D.; Bauman, A. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007, 39, 1423–1434. [Google Scholar] [CrossRef] [PubMed]
- Seyler, T.M.; Mont, M.A.; Ragland, P.S.; Kachwala, M.M.; Delanois, R.E. Sports activity after total hip and knee arthroplasty. Sports Med. 2006, 36, 571–583. [Google Scholar] [CrossRef]
- Chatterji, U.; Ashworth, M.J.; Lewis, P.L.; Dobson, P.J. Effect of total knee arthroplasty on recreational and sporting activity. Anz J. Surg. 2005, 75, 405–408. [Google Scholar] [CrossRef]
- McGrory, B.J.; Stuart, M.J.; Sim, F.H. Participation in sports after hip and knee arthroplasty: Review of literature and survey of surgeon preferences. Mayo Clin. Proc. 1995, 70, 342–348. [Google Scholar] [CrossRef]
- Swanson, E.A.; Schmalzried, T.P.; Dorey, F.J. Activity recommendations after total hip and knee arthroplasty: A survey of the American Association for Hip and Knee Surgeons. J. Arthroplast. 2009, 24, 120–126. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (MINORS): Development and validation of a new instrument. Anz J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Canetti, R.; Batailler, C.; Bankhead, C.; Neyret, P.; Servien, E.; Lustig, S. Faster return to sport after robotic-assisted lateral unicompartmental knee arthroplasty: A comparative study. Arch. Orthop. Trauma Surg. 2018, 138, 1765–1771. [Google Scholar] [CrossRef]
- Harbourne, A.D.; Sanchez-Santos, M.T.; Arden, N.K.; Filbay, S.R. Predictors of return to desired activity 12 months following unicompartmental and total knee arthroplasty. Acta Orthop. 2019, 90, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Lygre, S.H.L.; Espehaug, B.; Havelin, L.I.; Furnes, O.; Vollset, S.E. Pain and function in patients after primary unicompartmental and total knee arthroplasty. JBJS 2010, 92, 2890–2897. [Google Scholar] [CrossRef] [PubMed]
- Matthews, D.J.; Hossain, F.S.; Patel, S.; Haddad, F.S. A cohort study predicts better functional outcomes and equivalent patient satisfaction following UKR compared with TKR. HSS J. 2013, 9, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Pandit, H.; Campi, S.; Hamilton, T.; Dada, O.; Pollalis, S.; Jenkins, C.; Dodd, C.; Murray, D. Five-year experience of cementless Oxford unicompartmental knee replacement. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Pandit, H.; Jenkins, C.; Gill, H.; Barker, K.; Dodd, C.; Murray, D. Minimally invasive Oxford phase 3 unicompartmental knee replacement: Results of 1000 cases. J. Bone Jt. Surgery. Br. Vol. 2011, 93, 198–204. [Google Scholar] [CrossRef] [PubMed]
- Pietschmann, M.F.; Wohlleb, L.; Weber, P.; Schmidutz, F.; Ficklscherer, A.; Gülecyüz, M.F.; Safi, E.; Niethammer, T.R.; Jansson, V.; Müller, P.E. Sports activities after medial unicompartmental knee arthroplasty Oxford III—what can we expect? Int. Orthop. 2013, 37, 31–37. [Google Scholar] [CrossRef]
- Walton, N.P.; Jahromi, I.; Lewis, P.L.; Dobson, P.J.; Angel, K.R.; Campbell, D.G. Patient-perceived outcomes and return to sport and work: TKA versus mini-incision unicompartmental knee arthroplasty. J. Knee Surg. 2006, 19, 112–116. [Google Scholar] [CrossRef]
- Wylde, V.; Blom, A.; Dieppe, P.; Hewlett, S.; Learmonth, I. Return to sport after joint replacement. The Journal of bone and joint surgery. Br. Vol. 2008, 90, 920–923. [Google Scholar]
- Witjes, S.; Gouttebarge, V.; Kuijer, P.P.F.; van Geenen, R.C.; Poolman, R.W.; Kerkhoffs, G.M. Return to sports and physical activity after total and unicondylar knee arthroplasty: A systematic review and meta-analysis. Sports Med. 2016, 46, 269–292. [Google Scholar] [CrossRef]
- Kuster, M.S. Exercise recommendations after total joint replacement. Sports Med. 2002, 32, 433–445. [Google Scholar] [CrossRef] [PubMed]
- Vasta, S.; Papalia, R.; Torre, G.; Vorini, F.; Papalia, G.; Zampogna, B.; Fossati, C.; Bravi, M.; Campi, S.; Denaro, V. The Influence of Preoperative Physical Activity on Postoperative Outcomes of Knee and Hip Arthroplasty Surgery in the Elderly: A Systematic Review. J. Clin. Med. 2020, 9, 969. [Google Scholar] [CrossRef] [PubMed]
- Zampogna, B.; Papalia, R.; Papalia, G.F.; Campi, S.; Vasta, S.; Vorini, F.; Fossati, C.; Torre, G.; Denaro, V. The Role of Physical Activity as Conservative Treatment for Hip and Knee Osteoarthritis in Older People: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 1167. [Google Scholar] [CrossRef] [PubMed]
- Ho, J.C.; Stitzlein, R.N.; Green, C.J.; Stoner, T.; Froimson, M.I. Return to sports activity following UKA and TKA. J. Knee Surg. 2016, 29, 254–259. [Google Scholar]
- Kleeblad, L.J.; van der List, J.P.; Zuiderbaan, H.A.; Pearle, A.D. Larger range of motion and increased return to activity, but higher revision rates following unicompartmental versus total knee arthroplasty in patients under 65: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1811–1822. [Google Scholar] [CrossRef]
- Mont, M.A.; Rajadhyaksha, A.D.; Marxen, J.L.; Silberstein, C.E.; Hungerford, D.S. Tennis after total knee arthroplasty. Am. J. Sports Med. 2002, 30, 163–166. [Google Scholar] [CrossRef]
- Lefevre, N.; Rousseau, D.; Bohu, Y.; Klouche, S.; Herman, S. Return to judo after joint replacement. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2889–2894. [Google Scholar] [CrossRef]
| Author and Year | LOE | N.er of Patients | M | F | Type of Arthroplasty | Type of Implant | Bearing and Fixation | Mean Age at Surgery | Mean Follow-up (Months) | MINORS Score |
|---|---|---|---|---|---|---|---|---|---|---|
| Canetti et al. 2018 | 3 | 25 (28 knees) | 9 | 21 | Robotic UKA 11 | Resurfacing Uni Evolution, Tornier; BlueBelt Navio robotic surgical system. | Fixed bearing and cemented. | 66.5 ± 6.8 | 34.4 ± 10.5 | 17 |
| ______ | ___ | ___ | ||||||||
| Conventional UKA 17 | 59.5 ± 9.9 | 39.3 ± 15.5 | ||||||||
| Harbourne et al. 2018 | 3 | 995 | 44 | 54 | UKA 420 | n/a | n/a | 67 ± 10 | 12 | 16 |
| __ | __ | _____ | ___ | |||||||
| 6 | 9 | TKA 575 | 70 ± 9 | |||||||
| Lygre et al. 2010 | 3 | 1344 | 152 | 220 690 | UKA: 372 | Genesis Uni (Smith & Nephew), Miller-Galante all poly Uni (Zimmer), Oxford III (Biomet). | Fixed/mobile and cemented. | 68.8 ± 8.8 | 58.8 ± 27.6 | 15 |
| _ | ____ | ____ | ___ | ___ | ___ | |||||
| 282 | TKA: 972 | AGC (Biomet), Genesis I (Smith & Nephew), LCS (DePuy) and NexGen (Zimmer). | Fixed bearing and cemented. | 76 ± 7.7 | 84 ± 28.8 | |||||
| Matthews et al. 2013 | 2 | 68 | 10 | 24 | UKA 34 | n/a | n/a | UKA 67.3 ± 9.1 | 12 | 15 |
| _ | _ | ____ | ___ | |||||||
| 14 | 20 | TKA 34 | TKA 69.2 ± 7.7 | |||||||
| Naal et al. 2007 | 4 | 83 (83) | 45 | 38 | UKA | Preservation prosthesis (DePuy). | Fixed bearing and cemented. | 65.5 ± 9.1 years (47–83) | 12 | 10 |
| Pandit et al. 2011 | 4 | 818 (1000) | - | - | UKA | Phase 3 Oxford medial UKA (Biomet). | Mobile bearing and cemented. | 66 (32–88) | 67.2 | 11 |
| Pandit et al. 2015 | 4 | 579 (520) | 299 | 221 | UKA | Phase 3 Oxford medial UKA (Biomet). | Mobile bearing and cementless | 65.1 ± 10.3 (35–94) | 40.8 ± 20.4 | 12 |
| Pietschmann et al. 2012 | 3 | 131 | 57 | 74 | UKA | Phase 3 Oxford medial UKA (Biomet). | Mobile bearing and cemented. | 65.3 (44–90) | 50.4 (12–120) | 7 |
| Walton et al. 2010 | 3 | 150 (183) | 76 | 74 | UKA | Phase 3 Oxford medial UKA (Biomet). | Mobile bearing and cemented. | 71.5 ± 9.85 | 12 | 12 |
| _ | _ | _ | _ | _ | _ | _ | ||||
| 120 (142) | 61 | 59 | TKA | n/a | n/a | 71.53 ± 9.87 | ||||
| Wylde et al. 2008 | 3 | 966 | 48 511 | 52 355 | UKA: 100 TKA: 866 | n/a | n/a | 66 (45–88) 69.6 (26–93) | 24 | 16 |
| Author and Year | N.er of Patients | Preoperative | Postoperative | Outcome | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Canetti R. 2018 | 28 | 66.3 | 8.9 | 97.2 | 5.9 | KSS-Objective |
| 84.6 | 11.3 | 96.4 | 9.2 | KSS-Functional | ||
| 6.4 | 1.6 | 6.6 | 1.4 | UCLA | ||
| n/a | n/a | 96.4 | 8.3 | Lysholm scale | ||
| Naal F. 2007 | 83 | 129.9 | 24.8 | 186.9 | 18.3 | KSS total |
| Pandit H. 2011 | 1000 | 24.7 | 8.7 | 38.6 | 8.4 | OKS |
| 2.3 | 1.1 | 2 | 8.4 | Tegner activity score | ||
| 68.7 | 18 | 81.1 | 11.3 | AKSS-F | ||
| 47.4 | 20 | 81.1 | 16 | AKSS-O | ||
| Pandit H. 2015 | 520 | 27 | 9 | 43 | 7 | OKS |
| 3 | n/a | 3 | n/a | Tegner activity score | ||
| 71 | 17 | 86 | 16 | AKSS-F | ||
| 52 | 20 | 92 | 12 | AKSS-O | ||
| Pietschmann M. 2012 | 131 | n/a | n/a | 95.3 | 9.5 | KSS-Objective |
| n/a | n/a | 86.7 | 13.8 | KSS-Functional | ||
| n/a | n/a | 6 | 1 | UCLA | ||
| n/a | n/a | 189 | 26.8 | KSS total | ||
| n/a | n/a | 38.6 | 7.3 | OKS | ||
| n/a | n/a | 90.6 | 9.7 | WOMAC ADL | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Papalia, R.; Zampogna, B.; Torre, G.; Diaz Balzani, L.A.; Vasta, S.; Papalia, G.; De Vincentis, A.; Denaro, V. Return to Sport Activity in the Elderly Patients after Unicompartmental Knee Arthroplasty: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 1756. https://doi.org/10.3390/jcm9061756
Papalia R, Zampogna B, Torre G, Diaz Balzani LA, Vasta S, Papalia G, De Vincentis A, Denaro V. Return to Sport Activity in the Elderly Patients after Unicompartmental Knee Arthroplasty: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2020; 9(6):1756. https://doi.org/10.3390/jcm9061756
Chicago/Turabian StylePapalia, Rocco, Biagio Zampogna, Guglielmo Torre, Lorenzo Alirio Diaz Balzani, Sebastiano Vasta, Giuseppe Papalia, Antonio De Vincentis, and Vincenzo Denaro. 2020. "Return to Sport Activity in the Elderly Patients after Unicompartmental Knee Arthroplasty: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 9, no. 6: 1756. https://doi.org/10.3390/jcm9061756
APA StylePapalia, R., Zampogna, B., Torre, G., Diaz Balzani, L. A., Vasta, S., Papalia, G., De Vincentis, A., & Denaro, V. (2020). Return to Sport Activity in the Elderly Patients after Unicompartmental Knee Arthroplasty: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 9(6), 1756. https://doi.org/10.3390/jcm9061756






