Effects of Anesthesia Techniques on Outcomes after Hip Fracture Surgery in Elderly Patients: A Prospective, Randomized, Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Anesthesia Procedure
2.2. Outcome Assessment
2.3. Statistical Analysis
3. Results
3.1. Study Population, Demographic Data, and Perioperative Characteristics
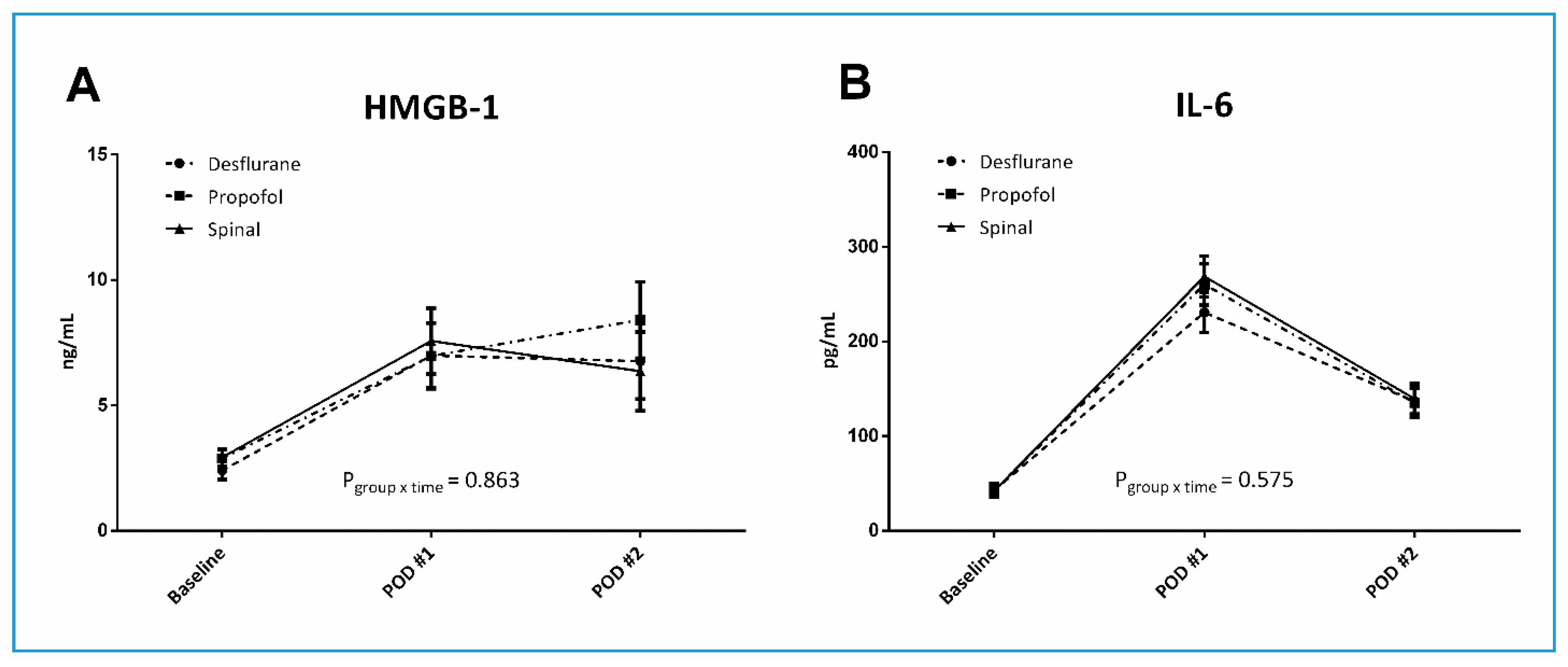
3.2. Proinflammatory Cytokines and Routine Laboratory Tests
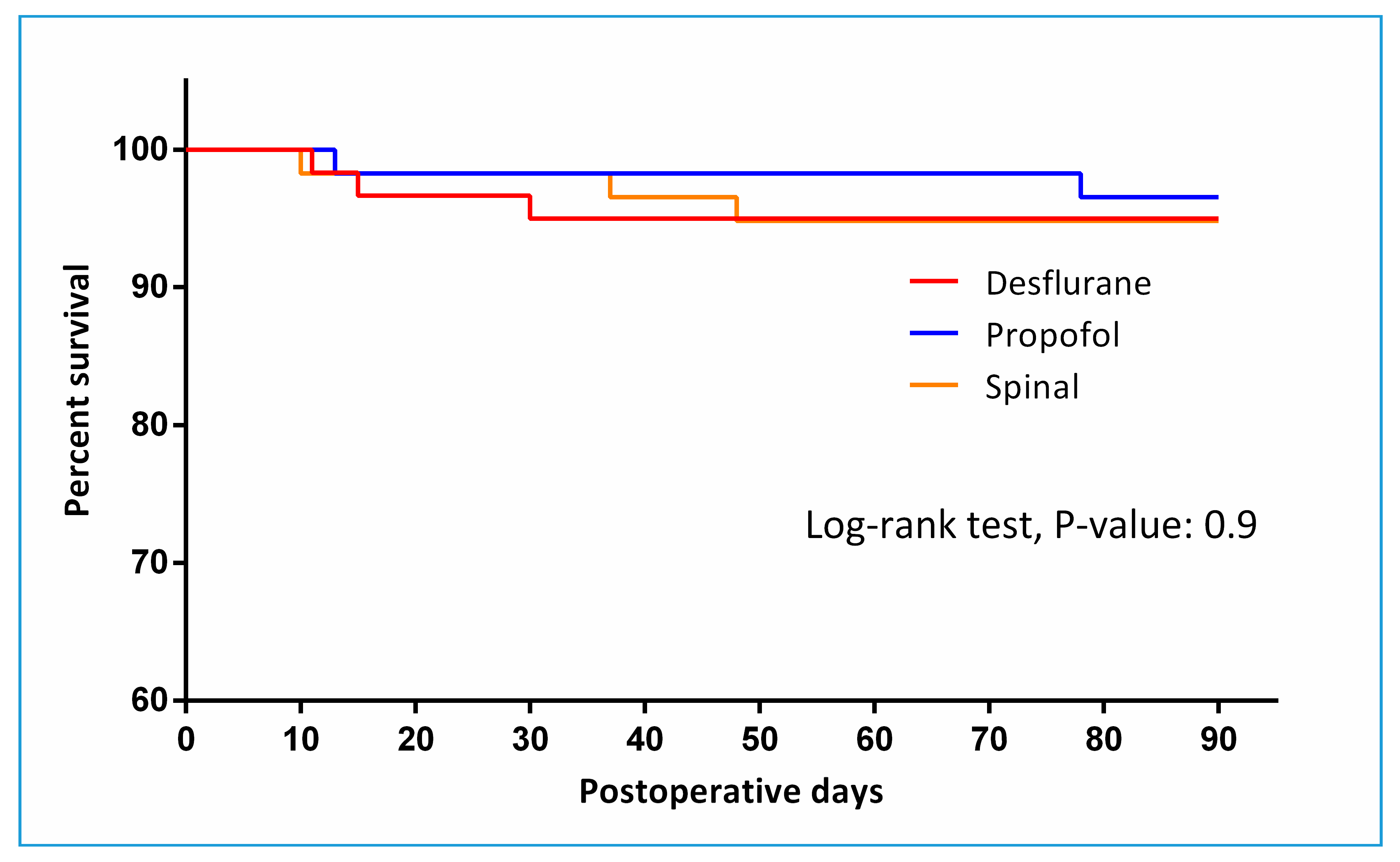
3.3. Postoperative Morbidity and Mortality
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Murthy, S.; Hepner, D.L.; Cooper, Z.; Bader, A.M.; Neuman, M.D. Controversies in anaesthesia for noncardiac surgery in older adults. Br. J. Anaesth. 2015, 115, ii15–ii25. [Google Scholar] [CrossRef] [PubMed]
- Kowark, A.; Adam, C.; Ahrens, J.; Bajbouj, M.; Bollheimer, C.; Borowski, M.; Dodel, R.; Dolch, M.; Hachenberg, T.; Henzler, D.; et al. Improve hip fracture outcome in the elderly patient (ihope): A study protocol for a pragmatic, multicentre randomised controlled trial to test the efficacy of spinal versus general anaesthesia. BMJ Open 2018, 8, e023609. [Google Scholar] [CrossRef] [PubMed]
- Laulund, A.S.; Lauritzen, J.B.; Duus, B.R.; Mosfeldt, M.; Jorgensen, H.L. Routine blood tests as predictors of mortality in hip fracture patients. Injury 2012, 43, 1014–1020. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.; Wang, X.; Liu, Z.; Chen, X.; Zhang, J. Plasma concentrations of pro- and anti-inflammatory cytokines and outcome prediction in elderly hip fracture patients. Injury 2011, 42, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Kang, R.; Chen, R.; Zhang, Q.; Hou, W.; Wu, S.; Cao, L.; Huang, J.; Yu, Y.; Fan, X.G.; Yan, Z.; et al. Hmgb1 in health and disease. Mol. Asp. Med. 2014, 40, 1–116. [Google Scholar] [CrossRef] [PubMed]
- Guay, J.; Parker, M.J.; Gajendragadkar, P.R.; Kopp, S. Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst. Rev. 2016, 2, CD000521. [Google Scholar] [CrossRef]
- Coetzee, J.F.; Glen, J.B.; Wium, C.A.; Boshoff, L. Pharmacokinetic model selection for target controlled infusions of propofol. Assessment of three parameter sets. Anesthesiology 1995, 82, 1328–1345. [Google Scholar] [CrossRef]
- Minto, C.F.; Schnider, T.W.; Shafer, S.L. Pharmacokinetics and pharmacodynamics of remifentanil. Ii. Model application. Anesthesiology 1997, 86, 24–33. [Google Scholar] [CrossRef]
- Giannoudis, P.V.; Mallina, R.; Harwood, P.; Perry, S.; Sante, E.D.; Pape, H.C. Pattern of release and relationship between hmgb-1 and il-6 following blunt trauma. Injury 2010, 41, 1323–1327. [Google Scholar] [CrossRef]
- Hung, W.W.; Morrison, R.S. Hip fracture: A complex illness among complex patients. Ann. Intern. Med. 2011, 155, 267–268. [Google Scholar] [CrossRef]
- Van Waesberghe, J.; Stevanovic, A.; Rossaint, R.; Coburn, M. General vs. Neuraxial anaesthesia in hip fracture patients: A systematic review and meta-analysis. BMC Anesth. 2017, 17, 87. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, C.M.; McLoughlin, L.; Patterson, C.C.; Clarke, M.; McCourt, K.C.; McBrien, M.E.; McAuley, D.F.; Shields, M.O. Perioperative outcomes in the context of mode of anaesthesia for patients undergoing hip fracture surgery: Systematic review and meta-analysis. Br. J. Anaesth. 2018, 120, 37–50. [Google Scholar] [CrossRef] [PubMed]
- Neuman, M.D.; Ellenberg, S.S.; Sieber, F.E.; Magaziner, J.S.; Feng, R.; Carson, J.L.; Investigators, R. Regional versus general anesthesia for promoting independence after hip fracture (regain): Protocol for a pragmatic, international multicentre trial. BMJ Open 2016, 6, e013473. [Google Scholar] [CrossRef] [PubMed]
- Valentin, N.; Lomholt, B.; Jensen, J.S.; Hejgaard, N.; Kreiner, S. Spinal or general anaesthesia for surgery of the fractured hip? A prospective study of mortality in 578 patients. Br. J. Anaesth. 1986, 58, 284–291. [Google Scholar] [CrossRef] [PubMed]
- Davis, F.M.; Woolner, D.F.; Frampton, C.; Wilkinson, A.; Grant, A.; Harrison, R.T.; Roberts, M.T.; Thadaka, R. Prospective, multi-centre trial of mortality following general or spinal anaesthesia for hip fracture surgery in the elderly. Br. J. Anaesth. 1987, 59, 1080–1088. [Google Scholar] [CrossRef] [PubMed]
- Heidari, S.M.; Soltani, H.; Hashemi, S.J.; Talakoub, R.; Soleimani, B. Comparative study of two anesthesia methods according to postoperative complications and one month mortality rate in the candidates of hip surgery. J. Res. Med Sci. 2011, 16, 323–330. [Google Scholar] [PubMed]
- Parker, M.J.; Griffiths, R. General versus regional anaesthesia for hip fractures. A pilot randomised controlled trial of 322 patients. Injury 2015, 46, 1562–1566. [Google Scholar] [CrossRef]
- Neuman, M.D.; Silber, J.H.; Elkassabany, N.M.; Ludwig, J.M.; Fleisher, L.A. Comparative effectiveness of regional versus general anesthesia for hip fracture surgery in adults. Anesthesiology 2012, 117, 72–92. [Google Scholar] [CrossRef]
- White, S.M.; Moppett, I.K.; Griffiths, R. Outcome by mode of anaesthesia for hip fracture surgery. An observational audit of 65 535 patients in a national dataset. Anaesthesia 2014, 69, 224–230. [Google Scholar] [CrossRef]
- Saribal, D.; Hocaoglu-Emre, F.S.; Erdogan, S.; Bahtiyar, N.; Caglar Okur, S.; Mert, M. Inflammatory cytokines il-6 and tnf-alpha in patients with hip fracture. Osteoporos. Int. 2019, 30, 1025–1031. [Google Scholar] [CrossRef]
- Venereau, E.; De Leo, F.; Mezzapelle, R.; Careccia, G.; Musco, G.; Bianchi, M.E. Hmgb1 as biomarker and drug target. Pharm. Res. 2016, 111, 534–544. [Google Scholar] [CrossRef]
- Wang, X.W.; Karki, A.; Zhao, X.J.; Xiang, X.Y.; Lu, Z.Q. High plasma levels of high mobility group box 1 is associated with the risk of sepsis in severe blunt chest trauma patients: A prospective cohort study. J. Cardiothorac. Surg. 2014, 9, 133. [Google Scholar] [CrossRef] [PubMed]
- Dang, W.; Zhang, X.; Yao, Y.M.; Su, Q.; Guo, Y.F.; Sun, R.J.; Qin, Y.H.; Ma, J.X.; Zhao, X.D. [Effect of early intensive insulin therapy on high mobility group box 1 protein levels and prognosis of patients with severe trauma]. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2011, 23, 173–175. [Google Scholar] [PubMed]
- Fei, J.; Yu, H.J.; Zhou, J.; Huang, X.K.; Liang, H.P.; Jiang, Y.G. [Study on high mobility group-1 protein in patients with multiple trauma]. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2005, 17, 273–275. [Google Scholar] [PubMed]
- Manganelli, V.; Signore, M.; Pacini, I.; Misasi, R.; Tellan, G.; Garofalo, T.; Lococo, E.; Chirletti, P.; Sorice, M.; Delogu, G. Increased hmgb1 expression and release by mononuclear cells following surgical/anesthesia trauma. Crit Care 2010, 14, R197. [Google Scholar] [CrossRef] [PubMed]
- Jia, J.; Sun, Y.; Hu, Z.; Li, Y.; Ruan, X. Propofol inhibits the release of interleukin-6, 8 and tumor necrosis factor-alpha correlating with high-mobility group box 1 expression in lipopolysaccharides-stimulated raw 264.7 cells. BMC Anesth. 2017, 17, 148. [Google Scholar] [CrossRef]
- Wang, H.L.; Liu, Y.Y.; Yan, H.D.; Wang, X.S.; Huang, R.; Lei, W.F. Intraoperative systemic lidocaine inhibits the expression of hmgb1 in patients undergoing radical hysterectomy. Int. J. Clin. Exp. Med. 2014, 7, 3398–3403. [Google Scholar]
- Wang, H.L.; Zhang, W.H.; Lei, W.F.; Zhou, C.Q.; Ye, T. The inhibitory effect of lidocaine on the release of high mobility group box 1 in lipopolysaccharide-stimulated macrophages. Anesth. Analg. 2011, 112, 839–844. [Google Scholar] [CrossRef]
- Seo, K.H.; Choi, J.W.; Jung, H.S.; Yoo, H.; Joo, J.D. The effects of remifentanil on expression of high mobility group box 1 in septic rats. J. Korean Med. Sci. 2017, 32, 542–551. [Google Scholar] [CrossRef]
- Mosfeldt, M.; Pedersen, O.B.; Riis, T.; Worm, H.O.; Mark, S.; Jorgensen, H.L.; Duus, B.R.; Lauritzen, J.B. Value of routine blood tests for prediction of mortality risk in hip fracture patients. Acta Orthop. 2012, 83, 31–35. [Google Scholar] [CrossRef]
- Hietala, P.; Strandberg, M.; Kiviniemi, T.; Strandberg, N.; Airaksinen, K.E. Usefulness of troponin t to predict short-term and long-term mortality in patients after hip fracture. Am. J. Cardiol. 2014, 114, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.G.; Lee, Y.K.; Park, H.P.; Sohn, H.M.; Oh, A.Y.; Jeon, Y.T.; Koo, K.H. C-reactive protein is an independent predictor for 1-year mortality in elderly patients undergoing hip fracture surgery: A retrospective analysis. Med. Baltim. 2016, 95, e5152. [Google Scholar] [CrossRef]
- Schraag, S.; Pradelli, L.; Alsaleh, A.J.O.; Bellone, M.; Ghetti, G.; Chung, T.L.; Westphal, M.; Rehberg, S. Propofol vs. Inhalational agents to maintain general anaesthesia in ambulatory and in-patient surgery: A systematic review and meta-analysis. BMC Anesth. 2018, 18, 162. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.; Lewis, S.R.; Pritchard, M.W.; Schofield-Robinson, O.J.; Shelton, C.L.; Alderson, P.; Smith, A.F. Intravenous versus inhalational maintenance of anaesthesia for postoperative cognitive outcomes in elderly people undergoing non-cardiac surgery. Cochrane Database Syst. Rev. 2018, 8, CD012317. [Google Scholar] [CrossRef] [PubMed]
- Irwin, M.G.; Chung, C.K.E.; Ip, K.Y.; Wiles, M.D. Influence of propofol-based total intravenous anaesthesia on peri-operative outcome measures: A narrative review. Anaesthesia 2020, 75, e90–e100. [Google Scholar] [CrossRef] [PubMed]
- Vasileiou, I.; Xanthos, T.; Koudouna, E.; Perrea, D.; Klonaris, C.; Katsargyris, A.; Papadimitriou, L. Propofol: A review of its non-anaesthetic effects. Eur. J. Pharm. 2009, 605, 1–8. [Google Scholar] [CrossRef]
- Takaono, M.; Yogosawa, T.; Okawa-Takatsuji, M.; Aotsuka, S. Effects of intravenous anesthetics on interleukin (il)-6 and il-10 production by lipopolysaccharide-stimulated mononuclear cells from healthy volunteers. Acta Anaesthesiol. Scand. 2002, 46, 176–179. [Google Scholar] [CrossRef]
- Sekandarzad, M.W.; van Zundert, A.A.J.; Lirk, P.B.; Doornebal, C.W.; Hollmann, M.W. Perioperative anesthesia care and tumor progression. Anesth. Analg. 2017, 124, 1697–1708. [Google Scholar] [CrossRef]
- Cassinello, F.; Prieto, I.; del Olmo, M.; Rivas, S.; Strichartz, G.R. Cancer surgery: How may anesthesia influence outcome? J. Clin. Anesth. 2015, 27, 262–272. [Google Scholar] [CrossRef]
- Wigmore, T.J.; Mohammed, K.; Jhanji, S. Long-term survival for patients undergoing volatile versus iv anesthesia for cancer surgery: A retrospective analysis. Anesthesiology 2016, 124, 69–79. [Google Scholar] [CrossRef]
- Biboulet, P.; Jourdan, A.; Van Haevre, V.; Morau, D.; Bernard, N.; Bringuier, S.; Capdevila, X. Hemodynamic profile of target-controlled spinal anesthesia compared with 2 target-controlled general anesthesia techniques in elderly patients with cardiac comorbidities. Reg. Anesth. Pain Med. 2012, 37, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Messina, A.; Frassanito, L.; Colombo, D.; Vergari, A.; Draisci, G.; Della Corte, F.; Antonelli, M. Hemodynamic changes associated with spinal and general anesthesia for hip fracture surgery in severe asa iii elderly population: A pilot trial. Minerva. Anestesiol. 2013, 79, 1021–1029. [Google Scholar] [PubMed]
- Monk, T.G.; Bronsert, M.R.; Henderson, W.G.; Mangione, M.P.; Sum-Ping, S.T.; Bentt, D.R.; Nguyen, J.D.; Richman, J.S.; Meguid, R.A.; Hammermeister, K.E. Association between intraoperative hypotension and hypertension and 30-day postoperative mortality in noncardiac surgery. Anesthesiology 2015, 123, 307–319. [Google Scholar] [CrossRef]
- Wesselink, E.M.; Kappen, T.H.; Torn, H.M.; Slooter, A.J.C.; van Klei, W.A. Intraoperative hypotension and the risk of postoperative adverse outcomes: A systematic review. Br. J. Anaesth. 2018, 121, 706–721. [Google Scholar] [CrossRef] [PubMed]
- Meng, L.; Yu, W.; Wang, T.; Zhang, L.; Heerdt, P.M.; Gelb, A.W. Blood pressure targets in perioperative care. Hypertension 2018, 72, 806–817. [Google Scholar] [CrossRef]
- Panula, J.; Pihlajamaki, H.; Mattila, V.M.; Jaatinen, P.; Vahlberg, T.; Aarnio, P.; Kivela, S.L. Mortality and cause of death in hip fracture patients aged 65 or older: A population-based study. BMC Musculoskelet. Disord. 2011, 12, 105. [Google Scholar] [CrossRef]
- Neuman, M.D.; Rosenbaum, P.R.; Ludwig, J.M.; Zubizarreta, J.R.; Silber, J.H. Anesthesia technique, mortality, and length of stay after hip fracture surgery. JAMA 2014, 311, 2508–2517. [Google Scholar] [CrossRef]


| Desflurane (n = 60) | Propofol (n = 58) | Spinal (n = 58) | p-Value | |
|---|---|---|---|---|
| Age (years) | 79.4 ± 7.7 | 80.5 ± 6.7 | 81.6 ± 6.7 | 0.234 |
| Male | 13 (21.7%) | 16 (27.6%) | 17 (29.3%) | 0.611 |
| Body mass index (kg/m2) | 22.5 (20.0, 24.8) | 22.3 (19.6, 24.8) | 22.8 (20.4, 25.1) | 0.787 |
| Comorbidities | ||||
| Dementia | 12 (20.0%) | 7 (12.1%) | 10 (17.2%) | 0.500 |
| Previous CVA | 17 (28.3%) | 14 (24.1%) | 11 (19.0%) | 0.490 |
| CAD | 15 (25.0%) | 14 (24.1%) | 12 (20.7%) | 0.843 |
| COPD | 2 (3.3%) | 1 (1.7%) | 5 (8.6%) | 0.175 |
| DM | 24 (40.0%) | 25 (43.1%) | 18 (31.0%) | 0.380 |
| Hypertension | 44 (73.3%) | 43 (74.1%) | 45 (77.6%) | 0.853 |
| Renal dysfunction | 8 (13.3%) | 12 (20.7%) | 13 (22.4%) | 0.405 |
| Baseline NT-proBNP | 267 (147, 747) | 404 (140, 1022) | 250 (168, 631) | 0.642 |
| Type of fracture | 0.170 | |||
| Femoral neck | 26 (43.3%) | 26 (44.8%) | 36 (62.1%) | |
| Intertrochanteric | 27 (45.0%) | 29 (50.0%) | 21 (36.2%) | |
| Subtrochanteric | 3 (5.0%) | 1 (1.7%) | 0 | |
| Other | 4 (6.7%) | 2 (3.4%) | 1 (1.7%) | |
| Time from injury to surgery (h) | 78.5 (46.8, 150.5) | 58.0 (39.3, 138.8) | 76.0 (52.0, 140.8) | 0.278 |
| Time from admission to surgery (h) | 46.5 (24.0, 71.0) | 42.0 (22.8, 70.0) | 47.5 (24.0, 72.0) | 0.951 |
| Desflurane (n = 60) | Propofol (n = 58) | Spinal (n = 58) | Overall p-Value | |
|---|---|---|---|---|
| Type of surgery | 0.235 | |||
| Bipolar hemiarthroplasty | 29 (48.3%) | 25 (43.1%) | 34 (58.6%) | |
| Internal fixation | 31 (51.7%) | 33 (56.9%) | 24 (41.4%) | |
| Anesthesia time (minutes) | 110 (100, 145) | 115 (100, 144) | 108 (96, 134) | 0.405 |
| Fluid balance | ||||
| Crystalloid (mL) | 600 (438, 850) | 600 (450, 850) | 500 (400, 688) *,† | 0.006 |
| Colloid (mL) | 0 (0, 0) | 0 (0, 0) | 0 (0, 100) | 0.227 |
| Urine output (mL) | 100 (50, 200) | 100 (51, 150) | 100 (30, 150) | 0.412 |
| Blood loss (mL) | 100 (50, 200) | 100 (50, 200) | 85 (50, 138) | 0.344 |
| Transfusion | ||||
| Amount of pRBC (U) | 0 (0, 0) | 0 (0, 1) | 0 (0, 0) | 0.047 |
| Vasopressor use | 37 (61.7%) | 34 (58.6%) | 16 (27.6%) *,† | 0.000 |
| Desflurane (n = 60) | Propofol (n = 58) | Spinal (n = 58) | p Value | |
|---|---|---|---|---|
| Hospital days | 6.5 (4.8, 9.0) | 7.0 (5.0, 9.0) | 7.0 (5.0, 11.0) | 0.416 |
| ICU days | 0.0 (0.0, 0.0) | 0.0 (0.0, 2.0) | 0.0 (0.0, 0.0) | 0.049 |
| Ventilator days | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.792 |
| Postoperative days | 3.0 (3.0, 5.0) | 3.0 (3.0, 6.0) | 4.0 (3.0, 6.0) | 0.573 |
| In-hospital complications | ||||
| Pulmonary complications | 4 (6.7%) | 5 (8.6%) | 4 (6.9%) | 0.907 |
| Cardiac complications | 3 (5.0%) | 2 (3.4%) | 2 (3.4%) | 0.883 |
| Delirium | 9 (15.0%) | 8 (13.8%) | 8 (13.8%) | 0.977 |
| Postoperative mortality | ||||
| In-hospital mortality | 1 (1.7%) | 0 | 2 (3.4%) | 0.357 |
| 30-day mortality | 2 (3.3%) | 1 (1.7%) | 1 (1.7%) | 0.794 |
| 90-day mortality | 3 (5.0%) | 2 (3.4%) | 3 (5.2%) | 0.886 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, S.; Kim, S.H.; Park, K.K.; Kim, S.J.; Bae, J.C.; Choi, Y.S. Effects of Anesthesia Techniques on Outcomes after Hip Fracture Surgery in Elderly Patients: A Prospective, Randomized, Controlled Trial. J. Clin. Med. 2020, 9, 1605. https://doi.org/10.3390/jcm9061605
Shin S, Kim SH, Park KK, Kim SJ, Bae JC, Choi YS. Effects of Anesthesia Techniques on Outcomes after Hip Fracture Surgery in Elderly Patients: A Prospective, Randomized, Controlled Trial. Journal of Clinical Medicine. 2020; 9(6):1605. https://doi.org/10.3390/jcm9061605
Chicago/Turabian StyleShin, Seokyung, Seung Hyun Kim, Kwan Kyu Park, Seon Ju Kim, Jae Chan Bae, and Yong Seon Choi. 2020. "Effects of Anesthesia Techniques on Outcomes after Hip Fracture Surgery in Elderly Patients: A Prospective, Randomized, Controlled Trial" Journal of Clinical Medicine 9, no. 6: 1605. https://doi.org/10.3390/jcm9061605
APA StyleShin, S., Kim, S. H., Park, K. K., Kim, S. J., Bae, J. C., & Choi, Y. S. (2020). Effects of Anesthesia Techniques on Outcomes after Hip Fracture Surgery in Elderly Patients: A Prospective, Randomized, Controlled Trial. Journal of Clinical Medicine, 9(6), 1605. https://doi.org/10.3390/jcm9061605





