Relationship between HIF-1 and Circadian Clock Proteins in Obstructive Sleep Apnea Patients—Preliminary Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Material Collection and Protein Level Assessment
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Heinzer, R.; Vat, S.; Marques-Vidal, P.; Marti-Soler, H.; Andries, D.; Tobback, N.; Mooser, V.; Preisig, M.; Malhotra, A.; Waeber, G.; et al. Prevalence of sleep-disordered breathing in the general population: The HypnoLaus study. Lancet Respir. Med. 2015, 3, 310–318. [Google Scholar] [CrossRef]
- Semenza, G.L. Hypoxia-inducible factors in physiology and medicine. Cell 2012, 148, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Gabryelska, A.; Szmyd, B.; Panek, M.; Szemraj, J.; Kuna, P.; Białasiewicz, P. Serum hypoxia-inducible factor-1α protein level as a diagnostic marker of obstructive sleep apnea. Pol. Arch. Intern. Med. 2020, 130, 158–160. [Google Scholar] [CrossRef] [PubMed]
- Gabryelska, A.; Stawski, R.; Sochal, M.; Szmyd, B.; Białasiewicz, P. Influence of one-night CPAP therapy on the changes of HIF-1α protein in OSA patients—A pilot study. J. Sleep Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, J.S. Transcriptional architecture of the mammalian circadian clock. Nat. Rev. Genet. 2017, 18, 164–179. [Google Scholar] [CrossRef] [PubMed]
- Burioka, N.; Koyanagi, S.; Endo, M.; Takata, M.; Fukuoka, Y.; Miyata, M.; Takeda, K.; Chikumi, H.; Ohdo, S.; Shimizu, E. Clock gene dysfunction in patients with obstructive sleep apnoea syndrome. Eur. Respir. J. 2008, 32, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Moreira, S.; Rodrigues, R.; Barros, A.B.; Pejanovic, N.; Neves-Costa, A.; Pedroso, D.; Pereira, C.; Fernandes, D.; Rodrigues, J.V.; Barbara, C.; et al. Changes in Expression of the CLOCK Gene in Obstructive Sleep Apnea Syndrome Patients Are Not Reverted by Continuous Positive Airway Pressure Treatment. Front. Med. (Lausanne) 2017, 4, 187. [Google Scholar] [CrossRef] [PubMed]
- Kapur, V.K.; Auckley, D.H.; Chowdhuri, S.; Kuhlmann, D.C.; Mehra, R.; Ramar, K.; Harrod, C.G. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. JCSM 2017, 13, 479–504. [Google Scholar] [CrossRef] [PubMed]
- Gabryelska, A.; Łukasik, Z.M.; Makowska, J.S.; Białasiewicz, P. Obstructive Sleep Apnea: From Intermittent Hypoxia to Cardiovascular Complications via Blood Platelets. Front. Neurol. 2018, 9, 635. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.-Y.; Lin, P.-W.; Lin, H.-C.; Lin, P.-M.; Chen, I.-Y.; Friedman, M.; Hung, C.-F.; Salapatas, A.M.; Lin, M.-C.; Lin, S.-F. Alternations of Circadian Clock Genes Expression and Oscillation in Obstructive Sleep Apnea. J. Clin. Med. 2019, 8, 1634. [Google Scholar] [CrossRef] [PubMed]
- Canales, M.T.; Holzworth, M.; Bozorgmehri, S.; Ishani, A.; Weiner, I.D.; Berry, R.B.; Beyth, R.J.; Gumz, M. Clock gene expression is altered in veterans with sleep apnea. Physiol. Genom. 2019, 51, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Firsov, D.; Bonny, O. Circadian rhythms and the kidney. Nat. Rev. Nephrol. 2018, 14, 626–635. [Google Scholar] [CrossRef] [PubMed]
- Adamovich, Y.; Ladeuix, B.; Golik, M.; Koeners, M.P.; Asher, G. Rhythmic Oxygen Levels Reset Circadian Clocks through HIF1α. Cell Metab. 2017, 25, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Manella, G.; Aviram, R.; Bolshette, N.; Muvkadi, S.; Golik, M.; Smith, D.F.; Asher, G. Hypoxia induces a time- and tissue-specific response that elicits intertissue circadian clock misalignment. Proc. Natl. Acad. Sci. USA 2020, 117, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Chilov, D.; Hofer, T.; Bauer, C.; Wenger, R.H.; Gassmann, M. Hypoxia affects expression of circadian genes PER1 and CLOCK in mouse brain. FASEB J. 2001, 15, 2613–2622. [Google Scholar] [CrossRef] [PubMed]

| OSA Group (n = 10) | Control Group (n = 10) | p Value | |
|---|---|---|---|
| Age (years) | 50.30 ± 9.75 | 49.00 ± 10.19 | 0.774 |
| BMI (kg/m2) | 34.48 ± 2.95 | 28.1 ± 4.1 | 0.001 |
| Sex | 90%M | 70%M | 0.264 |
| HIF-1α evening (pg/mL) | 1287.64 (452.31–2069.13) | 606.45 (327.97–1073.51) | 0.020 |
| HIF-1α morning (pg/mL) | 1236.97 ± 871.44 | 742.06 ± 450.65 | 0.043 |
| HIF-1β evening (ng/mL) | 72.59 ± 0.94 | 71.50 ± 1.32 | 0.047 |
| HIF-1β morning (ng/mL) | 72.38 ± 1.08 | 71.26 ± 1.65 | 0.091 |
| CLOCK evening (ng/mL) | 3.73 ± 0.35 | 3.38 ± 0.33 | 0.037 |
| CLOCK morning (ng/mL) | 3.52 ± 0.15 | 3.31 ± 0.20 | 0.019 |
| BMAL1 evening (ng/mL) | 9.32 ± 0.51 | 9.00 ± 0.40 | 0.132 |
| BMAL1 morning (ng/mL) | 9.52 ± 0.47 | 8.87 ± 0.61 | 0.016 |
| PER1 evening (ng/mL) | 266.75 (209.54–419.87) | 169.32 (134.50–204.97) | 0.004 |
| PER1 morning (ng/mL) | 38.01 (30.05–68.96) | 23.84 (18.22–38.39) | 0.029 |
| CRY1 evening (ng/mL) | 280.26 (197.31–422.36) | 185.21 (171.59–209.50) | 0.035 |
| CRY1 morning (ng/mL) | 39.38 (30.55–43.43) | 27.95 (15.97–40.84) | 0.105 |
| TST (h) | 6.43 ± 0.83 | 6.08 ± 0.68 | 0.321 |
| Percentage of time of TST spent in REM stage (%) | 19.03 ± 7.01 | 20.85 ± 8.09 | 0.597 |
| Arousal Index | 24.80 (20.15–34.18) | 15.20 (6.73–19.75) | 0.005 |
| AHI | 56.40 (44.98–65.33) | 1.30 (0.38–3.00) | <0.001 |
| AHI REM | 29.81 (17.11–56.67) | 0.00 (0.00–4.88) | <0.001 |
| AHI nREM | 46.99 (33.54–64.91) | 1.07 (0.20–1.42) | <0.001 |
| ODI | 57.85 (45.00–84.83) | 2.00 (0.98–3.00) | <0.001 |
| Awake SpO2 | 89.85 (83.65–93.60) | 93.85 (92.45–94.85) | 0.005 |
| Mean SpO2 of desaturation | 84.60 (74.50–89.73) | 91.75 (90.35–92.90) | <0.001 |
| Minimal SpO2 | 63.45 (40.85–75.18) | 88.90 (84.73–91.90) | <0.001 |
| Time spent with SpO2 below 90% (min) | 107.95 (73.05–278.58) | 0.55 (0.00–5.50) | <0.001 |
| Percentage of time with SpO2 90% (%) | 27.96 (20.44–64.69) | 0.15 (0.00–1.48) | <0.001 |
| Corrected Model | HIF-1α Protein Level-Evening | AHI | ODI | BMI | |||
|---|---|---|---|---|---|---|---|
| p Value | R Squared | p Value | |||||
| Protein Level | Multivariate General Linear Model | - | 0.025 | 0.123 | 0.131 | 1.505 | |
| CLOCK evening | 0.046 | 0.455 | 0.056 | 0.064 | 0.074 | 0.699 | |
| CLOCK morning | 0.059 | 0.435 | 0.654 | 0.086 | 0.356 | 0.115 | |
| BMAL1 evening | 0.707 | 0.126 | 0.687 | 0.387 | 0.596 | 0.415 | |
| BMAL1 morning | 0.057 | 0.438 | 0.143 | 0.795 | 0.674 | 0.321 | |
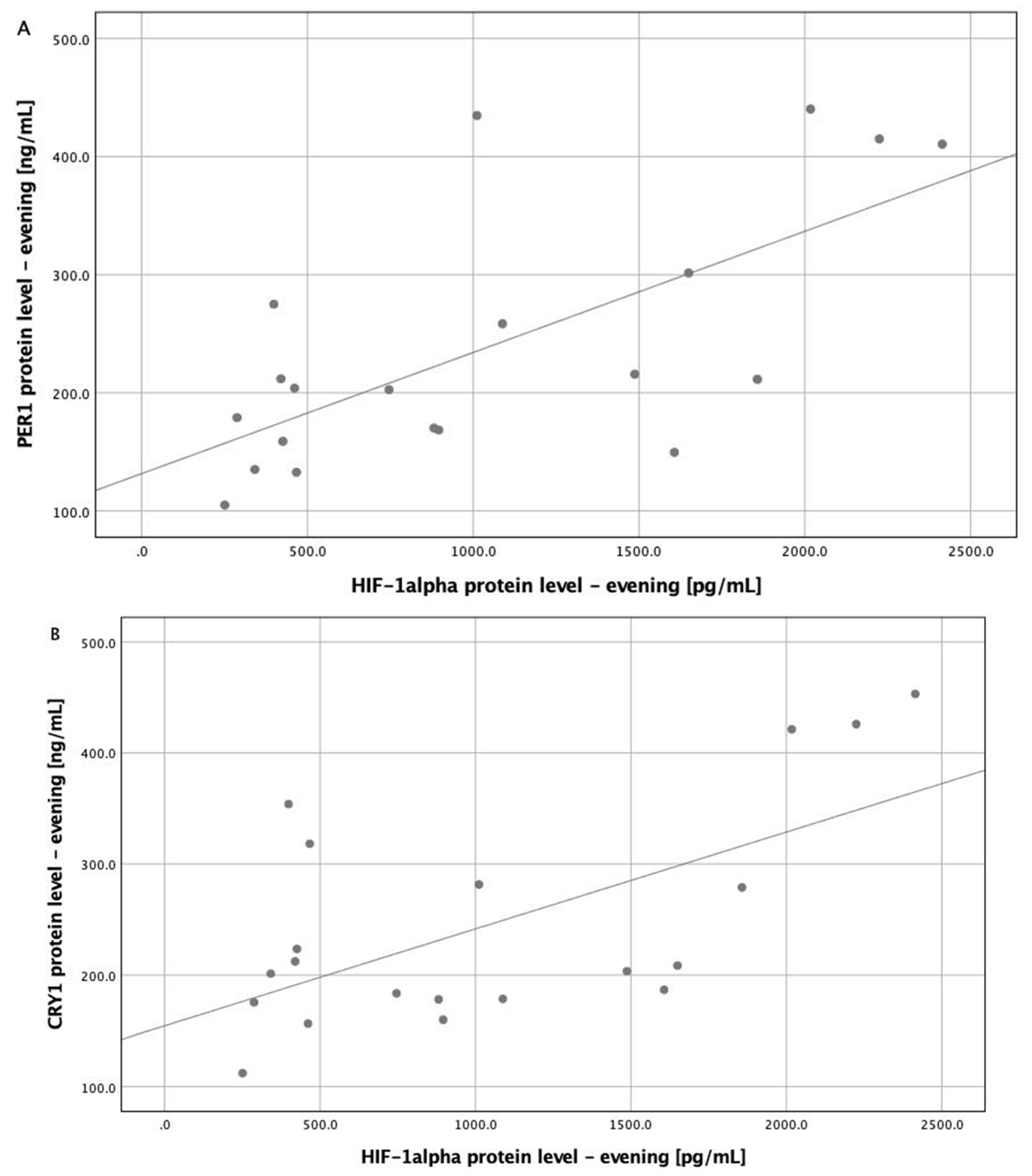
| PER1 evening | 0.008 | 0.583 | 0.020 | 0.379 | 0.627 | 0.784 | |
| PER1 morning | 0.006 | 0.593 | 0.972 | 0.012 | 0.003 | 0.662 | |
| CRY1 evening | 0.043 | 0.461 | 0.052 | 0.903 | 0.706 | 0.707 | |
| CRY1 morning | 0.487 | 0.194 | 0.629 | 0.604 | 0.746 | 0.400 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gabryelska, A.; Sochal, M.; Turkiewicz, S.; Białasiewicz, P. Relationship between HIF-1 and Circadian Clock Proteins in Obstructive Sleep Apnea Patients—Preliminary Study. J. Clin. Med. 2020, 9, 1599. https://doi.org/10.3390/jcm9051599
Gabryelska A, Sochal M, Turkiewicz S, Białasiewicz P. Relationship between HIF-1 and Circadian Clock Proteins in Obstructive Sleep Apnea Patients—Preliminary Study. Journal of Clinical Medicine. 2020; 9(5):1599. https://doi.org/10.3390/jcm9051599
Chicago/Turabian StyleGabryelska, Agata, Marcin Sochal, Szymon Turkiewicz, and Piotr Białasiewicz. 2020. "Relationship between HIF-1 and Circadian Clock Proteins in Obstructive Sleep Apnea Patients—Preliminary Study" Journal of Clinical Medicine 9, no. 5: 1599. https://doi.org/10.3390/jcm9051599
APA StyleGabryelska, A., Sochal, M., Turkiewicz, S., & Białasiewicz, P. (2020). Relationship between HIF-1 and Circadian Clock Proteins in Obstructive Sleep Apnea Patients—Preliminary Study. Journal of Clinical Medicine, 9(5), 1599. https://doi.org/10.3390/jcm9051599





