1. Introduction
While accounting for a minority of adult strokes, hemorrhagic strokes account for half of all strokes seen in children, and occur in approximately 1–2 per 100,000 children per year [
1,
2]. The etiologies of hemorrhagic stroke differ in children as well; hypertensive hemorrhage rarely occurs in children, and cerebral amyloid angiopathy is almost exclusively an adult disease [
3]. Trauma is the most common cause of intracerebral hemorrhage (ICH) in children, and the distinction between traumatic versus spontaneous hemorrhage can be challenging. Spontaneous ICH in children is most often caused by an underlying structural lesion, most often a congenital vascular malformation. Patterns of hemorrhage can provide a clue to etiology—a child with an ICH extending into the ventricles or subarachnoid space most likely has a brain arteriovenous malformation (AVM), a child with a pure ICH (involving the parenchyma only) has about an equal chance of an AVM or cavernous malformation [
4]. Cerebral aneurysms rarely cause intraparenchymal hemorrhage, but are the most common cause of pure subarachnoid hemorrhage, even in children. Arteriovenous fistulas (AVF) in children, compared to adults, are more likely pial (as opposed to dural) and congenital (as opposed to acquired) [
5]. While most AVMs lesions in children are spontaneous, features suggesting an underlying genetic syndrome include multiple AVMs, AVMs in unusual locations (e.g., spinal), and vascular birthmarks, in addition to a positive family history (autosomal dominant inheritance pattern) [
6]. Multiple cavernous malformations similarly suggest a genetic syndrome, and vascular birthmarks can again serve as a clue [
7]
In this review, we therefore give an overview about the clinical presentation of pediatric patients with intracerebral hemorrhage and with differential diagnoses in the emergency department. We also describe how neuroimaging of children with intracerebral hemorrhage should be tailored to specific situations and clinical contexts and recommend specific imaging protocols for acute and repeat imaging.
2. Diagnosis of Intracerebral Hemorrhage in the Emergency Department
Presenting symptoms of ICH in children can be nonspecific, particularly without preceding head trauma to raise initial suspicion. Headache is the most common feature of ICH in non-neonates, occurring in up to 80% of children [
8,
9,
10]. While acute ‘thunderclap headache’ is often associated with aneurysmal subarachnoid hemorrhage in adults, the quality and severity of the headache in children may be more subtle, and difficult to distinguish from migraine [
9]. Generalized or focal seizures occur in 20%–40% [
11,
12,
13], focal neurologic deficits in 13%–50% [
9,
10,
14], and signs of increased intracranial pressure (nausea, vomiting, depressed level of consciousness) in 50%–60% of children [
10,
11,
15]. Older children (≥6 years) are more likely to present with focal neurologic deficits and are also more likely to be able to articulate the quality and severity of headache, prompting emergent work-up. Younger children, on the other hand, more often present with non-localizing symptoms such as irritability, difficulty feeding, and lethargy, making it difficult to decide whom to image emergently [
9,
14]. Mackay, et al. investigated features distinguishing true stroke from stroke mimics in the emergency department, and found that acute onset of symptoms, vomiting, altered mental status, inability to walk, abnormal Glasgow coma scale score (GCS) and coma were associated with hemorrhagic stroke on univariate analysis; importantly, seizure at stroke onset did not predict a stroke mimic, highlighting a key difference between stroke presentation in children versus adults [
16]. Initial assessment in the emergency department should be rapid, and focus on signs of increased ICP, such as pupillary size and response (fixed, dilated or sluggish pupils or anisocoria); eye movements (cranial nerve VI palsies or forced downgaze), and optic discs when possible (papilledema). Level of consciousness may be evaluated with the Glasgow Coma Scale and focal neurologic deficits with a NIH stroke scale when possible [
17]. Neurocutaneous or other genetic stigmata may also raise suspicion for ICH in a child with otherwise nonspecific symptoms. For any child acutely deteriorating, stabilizing airway, breathing and circulation is critical prior to emergent neuroimaging.
3. Acute Imaging Work-up
The choice of neuroimaging modality should always be adjusted to clinical presentation and suspected cause. In children with acute focal neurological deficits, most pediatric stroke guidelines recommend brain magnetic resonance imaging (MRI) as first imaging modality especially in suspected ischemic stroke, where computed tomography (CT) may be less sensitive for detection of early ischemic changes [
17,
18]. Yet, in children with suspected intracranial hemorrhage, CT has several advantages, including greater accessibility and faster acquisition time [
3] limiting the risk of requiring sedation for imaging acquisition, hence often counterbalancing the disadvantages of radiation and iodine contrast exposure [
17], in the context of a life-threatening condition. Altogether, MRI should be preferred in stable and calm children, and CT favored in children with vigilance alteration, agitation or acutely worsening neurological symptoms.
After the positive diagnosis, careful evaluation of risk factors for secondary neurological deterioration is mandated. Pediatric counterparts to the adult ICH scoring system [
19] have been developed in order to predict severity and outcome of pediatric ICH. These scores consider a number of factors, including ICH/brain volume ratio; infratentorial location; intraventricular hemorrhage; hydrocephalus; mass effect/brain herniation; and altered mental status [
10,
20]. Higher ICH score has been associated with worse outcomes, and presence of markers of severity should prompt consideration for immediate transfer to a pediatric neuro-intensive care environment.
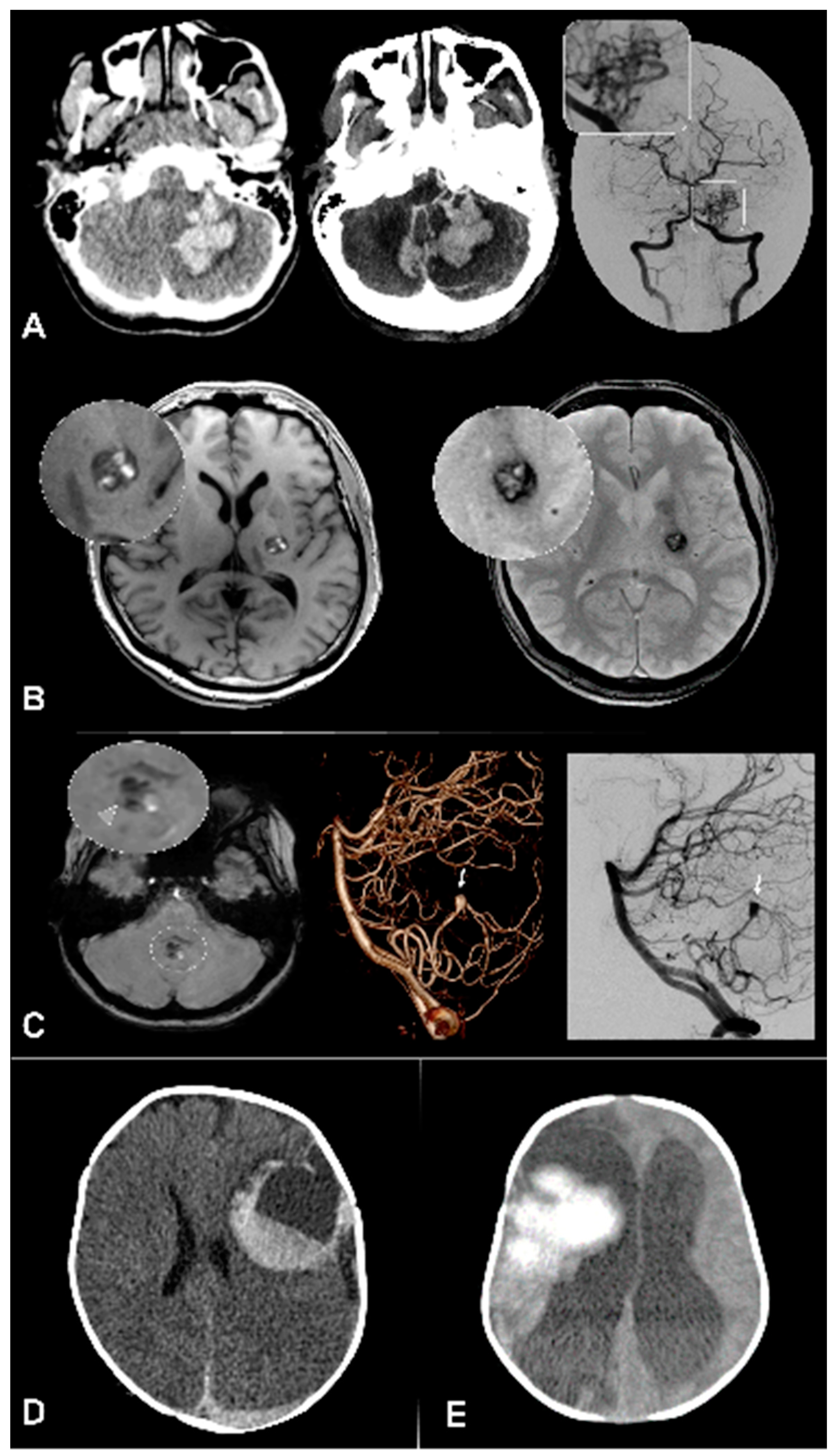
Intracranial vascular imaging (CT or MR angiography) should then systematically be acquired as part of the initial diagnostic examination. Indeed, there is a high prevalence of readily identifiable vascular lesions such as arteriovenous malformations (AVM), arteriovenous fistulas (AVF), or aneurysms in children with ICH. (
Figure 1) If identified, high recurrence risk sectors (ectasia or arterial aneurysm) should be searched for so as to guide therapeutic management, and prevent early recurrent bleeding [
17].
Digital subtraction angiography (DSA) has a central role for further characterization of vascular anomalies, and to investigate ICHs with undetermined etiology, due to its higher spatial and temporal resolutions and consequent higher sensitivity for intracranial shunts detection. (
Figure 1 and
Figure 2) The optimal timing for DSA realization is unknown, but should theoretically be performed as soon as possible in children with ICH of unknown origin to identify and treat occult vascular malformations. Of note, DSA is a low risk and often high yield examination in children: a recent analysis of pediatric patients revealed a 0% complication rate during the procedure and a 0.4% postprocedural complication rate [
21,
22].
In the absence of intracranial arteriovenous shunt, the second most prevalent etiology are cavernomas, more conspicuously detected using MRI. Similarly, hemorrhagic brain tumors should be searched for using contrast enhanced MRI [
3].
To summarize, the optimal acute imaging sequence for a child with ICH would be CT or MR with vascular imaging (CTA-MRA), followed with gadolinium enhanced MRI if the initial modality was CT, finally completed DSA in the absence of identifiable cause.
4. Advanced Imaging and MR Protocol
The specificity of ICH etiological spectrum in children makes advanced MR imaging techniques particularly useful for the routine evaluation of pediatric ICH etiology.
As arteriovenous shunts are the most prominent cause for hemorrhage in children, perfusion imaging such as arterial spin labelling, and dynamic vascular imaging such as time-resolved multiphase MR-angiography can give immediate insight on the underlying etiology and help tailor therapeutic management (See
Figure 3—Advanced imaging)
Arterial spin labelling is a MR based non-contrast perfusion technique that has been shown to identify areas of high cerebral blood flow in pediatric AVMs with good sensitivity [
23]. Quantifying its added value in the routine acute evaluation of pediatric ICH is an unmet need, but it is a useful and easy-to-use adjunct in clinical practice.
Similarly, dynamic MR-angiography can provide key information with regards to the presence of an arteriovenous shunt, as well as an accurate preliminary delineation of arterial feeders, nidus sectors, venous outflow and their respective angiodynamics.
Altogether, when acquiring MRI for the etiological work-up of a child with pediatric ICH, the following sequence protocol is advisable:
T2* Gradient Echo, or its 3D susceptibility weighted imaging derivatives; for the positive the diagnosis of blood breakdown products and the identification of other lesions (e.g., distinct cavernomas in cavernomatosis), to detect intraventricular blood.
Diffusion weighted imaging, to identify areas of restricted diffusion that can point towards a hemorrhagic transformation of an acute ischemic stroke or towards a venous infarction in the context of cerebral venous thrombosis.
FLAIR or T2 (in children younger than 2 years old), to identify pre-existing brain lesions, including brain tumors, and quantify edema, to evaluate ventricles volume and hydrocephalus.
Pre contrast T1.
Whole brain time-of-flight angiography, to identify macro-vascular lesions.
Arterial spin labeling (ASL) perfusion, to identify arteriovenous shunts.
Dynamic MR-angiography, to identify and characterize high flow arteriovenous shunts.
Post-contrast T1, to identify enhancing tumors, delineate an arteriovenous malformation or other vascular malformations.
5. Specific Considerations According to Suspected Cause
5.1. Arteriovenous Malformation
In most vascular pathologies (AVMs, AVFs, and aneurysms) except cavernous malformation (CM), DSA will be key for further lesion characterization but a CM may also be accompanied by a second vascular lesion, such as an AVM, in which case a DSA may be useful. The major differential after diagnosis of ICH in children is the presence of an AVM as it is the most common vascular lesion in this age group, with a hemorrhage risk of up to 6% per year and a mortality rate of up to 25% per hemorrhage [
24,
25,
26]. Treatment decisions for AVM greatly rely on DSA because it offers the greatest resolution of the nidus region and feeding arteries. Around 15% of cerebral AVMs receive some blood supply from meningeal arteries that are usually not visible on MRA [
27,
28]. Moreover, DSA and especially 3D-DSA is superior to CTA/MRA for assessment of outflow stenosis and deep venous drainage [
29]. Newer technologies (4D-DSA) combine the aforementioned exceptional spatial resolution of DSA with a sufficient temporal resolution further enhancing treatment decisions [
30,
31]. At baseline, parts of the AVM architecture may be obscured by fresh clots causing the need for reimaging after clot resorption [
32,
33], and prompting caution with regards to draining vein obstruction.
5.2. Cavernous Malformation
Cavernous malformations (CM) is amongst most frequent causes for non-traumatic pediatric ICH. It typically appears on T2 * Gradient Echo weighted sequences as a multilobulated well-defined lesion with blooming hypointensity [
34,
35]. The presence of distinct signal intensities on T1 within the lesions lobules is highly suggestive of the diagnosis. A genetic or post radiation pathogenesis may be present in case of multiple CMs [
36]. Identifying a developmental venous anomaly (DVA) in the immediate vicinity of the lesion adds to the imaging suspicion, and can guide surgical approach.
5.3. Aneurysms and Pseudo-Aneurysms
CTA/MRA are often used as first screening for aneurysms [
37,
38]; however, DSA is still the gold standard with highest detection rates (97% of patients versus 80% of the time without DSA), especially for the detection of small aneurysms under 4 mm [
11,
39,
40,
41]. An important advantage of DSA is the possibility to perform rotational angiographies and thereby create 3D reconstructions of every aspect of the aneurysm. This allows for a highly detailed depiction of the aneurysm anatomy, enabling for best possible planning of therapeutic strategies [
42]. Moreover, for example in anterior communicating aneurysms the contralateral ICA and A1 can be depicted and merged with the ipsilateral side to plan endovascular therapy [
43].
6. Follow up and Repeat Imaging
When the initial imaging work-up is inconclusive, and in the absence of systemic concurrent causes, repeated brain imaging should be considered as all structural underlying etiologies may be masked by the acute mass effect caused by the hemorrhage. Vascular lesions can be masked or partially destroyed by the initial hemorrhage and the risk of rebleeding is hypothesized to be higher when the clot retracts [
12].
Some indirect arguments may point to the presence of an underlying parenchymal lesion. This most notably includes the early detection of peri-hematoma brain edema. Indeed, edema typically develops after 48–72 h, hence important edema at baseline suggest the presence of a pre-existing tumoral lesion, which should prompt early re-imaging so as not to delay etiological care.
The timing of repeat imaging should be tailored to specific clinical context and should include repeat DSA. Common temporal landmarks include after mass effect contraction (within three weeks), and after complete hemorrhage resorption (within three to six months) if intermediate control remained inconclusive.
7. Conclusions
Neuroimaging of children with intracerebral hemorrhage should be tailored to specific situations and clinical contexts. Yet, one must keep in mind the high prevalence of underlying vascular lesions and adapt imaging protocol accordingly. Vascular imaging plays a key role regardless of modality. MRI, including advanced sequences, should be favored whenever possible at the acute phase.
Author Contributions
Conceptualization, P.B.S., M.-N.P., H.J.F., S.L., O.N., G.B.; methodology, P.B.S., M.-N.P., H.J.F., S.L., O.N., G.B.; investigation, P.B.S., M.-N.P., H.J.F., S.L., O.N., G.B.; writing—original draft preparation, P.B.S., M.-N.P., H.J.F., S.L., O.N., G.B.; writing—review and editing, P.B.S., M.-N.P., H.J.F., S.L., O.N., G.B.; visualization, P.B.S., G.B.; supervision, P.B.S., G.B.; project administration, P.B.S., G.B. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Broderick, J.; Brott, T.; Prenger, E.; Leach, A. Stroke in Children Within a Major Metropolitan Area: The Surprising Importance of Intracerebral Hemorrhage. J. Child Neurol. 1993. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, N.; Johnston, S.C.; Wu, Y.W.; Sidney, S.; Fullerton, H.J. Imaging data reveal a higher pediatric stroke incidence than prior US estimates. Stroke 2009, 40, 3415–3421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boulouis, G.; Blauwblomme, T.; Hak, J.F.; Benichi, S.; Kirton, A.; Meyer, P.; Chevignard, M.; Tournier-Lasserve, E.; MacKay, M.T.; Chabrier, S.; et al. Nontraumatic Pediatric Intracerebral Hemorrhage. Stroke 2020. [Google Scholar] [CrossRef] [PubMed]
- Jordan, L.C.; Johnston, S.C.; Wu, Y.W.; Sidney, S.; Fullerton, H.J. The importance of cerebral aneurysms in childhood hemorrhagic stroke a population-based study. Stroke 2009. [Google Scholar] [CrossRef] [Green Version]
- Terada, A.; Komiyama, M.; Ishiguro, T.; Niimi, Y.; Oishi, H. Nationwide survey of pediatric intracranial arteriovenous shunts in Japan: Japanese Pediatric Arteriovenous Shunts Study (JPAS). J. Neurosurg.: Pediatrics 2018, 22, 550–558. [Google Scholar] [CrossRef] [Green Version]
- Cai, R.; Liu, F.; Hua, C.; Yu, Z.; Ramien, M.; Malic, C.; Yu, W.; Zhang, X.; Liu, Y.; Jin, Y.; et al. A novel RASA1 mutation causing capillary malformation-arteriovenous malformation (CM-AVM): the first genetic clinical report in East Asia. Hereditas 2018. [Google Scholar] [CrossRef]
- Sirvente, J.; Enjolras, O.; Wassef, M.; Tournier-Lasserve, E.; Labauge, P. Frequency and phenotypes of cutaneous vascular malformations in a consecutive series of 417 patients with familial cerebral cavernous malformations. J. Eur. Acad. Dermatology Venereol. 2009. [Google Scholar] [CrossRef]
- Liu, J.; Wang, D.; Lei, C.; Xiong, Y.; Yuan, R.; Hao, Z.; Tao, W.; Liu, M. Etiology, clinical characteristics and prognosis of spontaneous intracerebral hemorrhage in children: A prospective cohort study in China. J. Neurol. Sci. 2015. [Google Scholar] [CrossRef]
- Meyer-Heim, A.D.; Boltshauser, E. Spontaneous intracranial haemorrhage in children: Aetiology, presentation and outcome. Brain Dev. 2003. [Google Scholar] [CrossRef]
- Beslow, L.A.; Licht, D.J.; Smith, S.E.; Storm, P.B.; Heuer, G.G.; Zimmerman, R.A.; Feiler, A.M.; Kasner, S.E.; Ichord, R.N.; Jordan, L.C. Predictors of outcome in childhood intracerebral hemorrhage: A prospective consecutive cohort study. Stroke 2010. [Google Scholar] [CrossRef] [Green Version]
- Al-Jarallah, A.; Al-Rifai, M.T.; Riela, A.R.; Roach, E.S. Nontraumatic brain hemorrhage in children: Etiology and presentation. J. Child Neurol. 2000. [Google Scholar] [CrossRef] [PubMed]
- Beslow, L.A.; Ichord, R.N.; Gindville, M.C.; Kleinman, J.T.; Bastian, R.A.; Smith, S.E.; Licht, D.J.; Hillis, A.E.; Jordan, L.C. Frequency of Hematoma expansion after spontaneous intracerebral hemorrhage in children. JAMA Neurol. 2014. [Google Scholar] [CrossRef] [Green Version]
- Beslow, L.A.; Abend, N.S.; Gindville, M.C.; Bastian, R.A.; Licht, D.J.; Smith, S.E.; Hillis, A.E.; Ichord, R.N.; Jordan, L.C. Pediatric intracerebral hemorrhage: Acute symptomatic seizures and epilepsy. JAMA Neurol. 2013. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lo, W.D.; Lee, J.E.; Rusin, J.; Perkins, E.; Roach, E.S. Intracranial hemorrhage in children: An evolving spectrum. Arch. Neurol. 2008. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jordan, L.C.; Kleinman, J.T.; Hillis, A.E. Intracerebral hemorrhage volume predicts poor neurologic outcome in children. Stroke 2009. [Google Scholar] [CrossRef]
- Mackay, M.T.; Yock-Corrales, A.; Churilov, L.; Monagle, P.; Donnan, G.A.; Babl, F.E. Differentiating Childhood Stroke from Mimics in the Emergency Department. Stroke 2016. [Google Scholar] [CrossRef]
- Ferriero, D.M.; Fullerton, H.J.; Bernard, T.J.; Billinghurst, L.; Daniels, S.R.; Debaun, M.R.; Deveber, G.; Ichord, R.N.; Jordan, L.C.; Massicotte, P.; et al. Management of stroke in neonates and children: A scientific statement from the American Heart Association/American stroke association. Stroke 2019. [Google Scholar] [CrossRef] [Green Version]
- Medley, T.L.; Miteff, C.; Andrews, I.; Ware, T.; Cheung, M.; Monagle, P.; Mandelstam, S.; Wray, A.; Pridmore, C.; Troedson, C.; et al. Australian Clinical Consensus Guideline: The diagnosis and acute management of childhood stroke. Int. J. Stroke 2019. [Google Scholar] [CrossRef] [Green Version]
- Hemphill, J.C.; Bonovich, D.C.; Besmertis, L.; Manley, G.T.; Johnston, S.C. The ICH score: A simple, reliable grading scale for intracerebral hemorrhage. Stroke 2001. [Google Scholar] [CrossRef] [Green Version]
- Guédon, A.; Blauwblomme, T.; Boulouis, G.; Jousset, C.; Meyer, P.; Kossorotoff, M.; Bourgeois, M.; Puget, S.; Zerah, M.; Oppenheim, C.; et al. Predictors of outcome in patients with pediatric intracerebral hemorrhage: Development and validation of a modified score. Radiology 2018. [Google Scholar] [CrossRef]
- Ellis, M.J.; Amlie-Lefond, C.; Orbach, D.B. Endovascular therapy in children with acute ischemic stroke: review and recommendations. Neurology 2012, 79, S158–S164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orbach, D.B.; Stamoulis, C.; Strauss, K.J.; Manchester, J.; Smith, E.R.; Scott, R.M.; Lin, N. Neurointerventions in children: Radiation exposure and its import. Am. J. Neuroradiol. 2014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blauwblomme, T.; Naggara, O.; Brunelle, F.; Grévent, D.; Puget, S.; Di Rocco, F.; Beccaria, K.; Paternoster, G.; Ourgeois, M.; Kossorotoff, M.; et al. Arterial spin labeling magnetic resonance imaging: Toward noninvasive diagnosis and follow-up of pediatric brain arteriovenous malformations. J. Neurosurg. Pediatr. 2015. [Google Scholar] [CrossRef] [PubMed]
- Fullerton, H.J.; Achrol, A.S.; Johnston, S.C.; McCulloch, C.E.; Higashida, R.T.; Lawton, M.T.; Sidney, S.; Young, W.L. Long-term hemorrhage risk in children versus adults with brain arteriovenous malformations. Stroke 2005. [Google Scholar] [CrossRef]
- Lawton, M.T.; Rutledge, W.C.; Kim, H.; Stapf, C.; Whitehead, K.J.; Li, D.Y.; Krings, T.; TerBrugge, K.; Kondziolka, D.; Morgan, M.K.; et al. Brain arteriovenous malformations. Nat. Rev. Dis. Prim. 2015. [Google Scholar] [CrossRef]
- Ding, D.; Starke, R.M.; Kano, H.; Mathieu, D.; Huang, P.P.; Feliciano, C.; Rodriguez-Mercado, R.; Almodovar, L.; Grills, I.S.; Silva, D.; et al. International multicenter cohort study of pediatric brain arteriovenous malformations. Part 1: Predictors of hemorrhagic presentation. J. Neurosurg. Pediatr. 2017. [Google Scholar] [CrossRef] [Green Version]
- Yeung, R.; Ahmad, T.; Aviv, R.I.; De Tilly, L.; Fox, A.J.; Symons, S.P. Comparison of CTA to DSA in determining the etiology of spontaneous ICH. Can. J. Neurol. Sci. 2009. [Google Scholar] [CrossRef] [Green Version]
- Newton, T.H.; Cronqvist, S. Involvement of dural arteries in intracranial arteriovenous malformations. Radiology 1969. [Google Scholar] [CrossRef]
- Ellis, M.J.; Armstrong, D.; Vachhrajani, S.; Kulkarni, A.V.; Dirks, P.B.; Drake, J.M.; Smith, E.R.; Scott, R.M.; Orbach, D.B. Angioarchitectural features associated with hemorrhagic presentation in pediatric cerebral arteriovenous malformations. J. Neurointerv. Surg. 2013. [Google Scholar] [CrossRef] [Green Version]
- Lang, S.; Gölitz, P.; Struffert, T.; Rösch, J.; Rössler, K.; Kowarschik, M.; Strother, C.; Doerfler, A. 4D DSA for dynamic visualization of cerebral vasculature: A single-center experience in 26 cases. Am. J. Neuroradiol. 2017. [Google Scholar] [CrossRef] [Green Version]
- Ognard, J.; Magro, E.; Caroff, J.; Ben Salem, D.; Andouard, S.; Nonent, M.; Gentric, J.C. A new time-resolved 3D angiographic technique (4D DSA): Description, and assessment of its reliability in Spetzler–Martin grading of cerebral arteriovenous malformations. J. Neuroradiol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Cánovas, D.; Gil, A.; Jato, M.; de Miquel, M.; Rubio, F. Clinical outcome of spontaneous non-aneurysmal subarachnoid hemorrhage in 108 patients. Eur. J. Neurol. 2012. [Google Scholar] [CrossRef] [PubMed]
- Elhadi, A.M.; Zabramski, J.M.; Almefty, K.K.; Mendes, G.A.C.; Nakaji, P.; McDougall, C.G.; Albuquerque, F.C.; Preul, M.C.; Spetzler, R.F. Spontaneous subarachnoid hemorrhage of unknown origin: Hospital course and long-term clinical and angiographic follow-up. J. Neurosurg. 2015. [Google Scholar] [CrossRef] [PubMed]
- Rigamonti, D.; Drayer, B.P.; Johnson, P.C.; Hadley, M.N.; Zabramski, J.; Spetzler, R.F. The MRI appearance of cavernous malformations (angiomas). J. Neurosurg. 1987. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sage, M.R.; Blumbergs, P.C. Cavernous haemangiomas (angiomas) of the brain. Australas. Radiol. 2001. [Google Scholar] [CrossRef]
- Baumgartner, J.E.; Ater, J.L.; Ha, C.S.; Kuttesch, J.F.; Leeds, N.E.; Fuller, G.N.; Wilson, R.J. Pathologically proven cavernous angiomas of the brain following radiation therapy for pediatric brain tumors. Pediatr. Neurosurg. 2003. [Google Scholar] [CrossRef]
- Roach, E.S.; Golomb, M.R.; Adams, R.; Biller, J.; Daniels, S.; Deveber, G.; Ferriero, D.; Jones, B.V.; Kirkham, F.J.; Scott, R.M.; et al. Management of stroke in infants and children: A scientific statement from a special writing group of the american heart association stroke council and the council on cardiovascular disease in the young. Stroke 2008. [Google Scholar] [CrossRef] [Green Version]
- Kumra, S.; Ashtari, M.; Anderson, B.; Cervellione, K.L.; Kan, L. Ethical and practical considerations in the management of incidental findings in pediatric MRI studies. J. Am. Acad. Child Adolesc. Psychiatry 2006. [Google Scholar] [CrossRef]
- Korogi, Y.; Takahashi, M.; Katada, K.; Ogura, Y.; Hasuo, K.; Ochi, M.; Utsunomiya, H.; Abe, T.; Imakita, S. Intracranial aneurysms: Detection with three-dimensional CT angiography with volume rendering - Comparison with conventional angiographic and surgical findings. Radiology 1999. [Google Scholar] [CrossRef]
- Vieco, P.T.; Shuman, W.P.; Alsofrom, G.E.; Gross, C.E. Detection of circle of Willis aneurysms in patients with acute subarachnoid hemorrhage: A comparison of CT angiography and digital subtraction angiography. Am. J. Roentgenol. 1995. [Google Scholar] [CrossRef] [Green Version]
- Alberico, R.A.; Patel, M.; Casey, S.; Jacobs, B.; Maguire, W.; Decker, R.; Heinz, E.R. Evaluation of the circle of Willis with three-dimensional CT angiography in patients with suspected intracranial aneurysms. Am. J. Neuroradiol. 1995. [Google Scholar]
- Cancelliere, N.M.; Najafi, M.; Brina, O.; Bouillot, P.; Vargas, M.I.; Lovblad, K.O.; Krings, T.; Pereira, V.M.; Steinman, D.A. 4D-CT angiography versus 3D-rotational angiography as the imaging modality for computational fluid dynamics of cerebral aneurysms. J. Neurointerv. Surg. 2019. [Google Scholar] [CrossRef] [PubMed]
- Rösch, J.; Lang, S.; Gölitz, P.; Kallmünzer, B.; Rössler, K.; Doerfler, A.; Struffert, T. Value of Flat-detector Computed Tomography Angiography with Intravenous Contrast Media Injection in the Evaluation and Treatment of Acutely Ruptured Aneurysms of the AcomA complex: A Single Center Experience in 15 Cases. Clin. Neuroradiol. 2018. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).