Contemporary Management of Acute Lower Limb Ischemia: Determinants of Treatment Choice
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Surgery
2.3. Endovascular Treatment
2.4. Statistics
3. Results
4. Discussion
5. Conclusions
Funding
Conflicts of Interest
References
- Walker, T.G. Acute Limb Ischemia. Tech. Vasc. Interv. Radiol. 2009, 12, 117–129. [Google Scholar] [CrossRef] [PubMed]
- Lichtenberg, M.; Käunicke, M.; Hailer, B. Percutaneous mechanical thrombectomy for treatment of acute femoropopliteal bypass occlusion. Vasc. Health Risk Manag. 2012, 8, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Lukasiewicz, A. Treatment of acute lower limb ischaemia. Vasa 2016, 45, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Hennebry, T.A. Percutaneous isolated pharmaco-mechanical thrombolysis-thrombectomy system for the management of acute arterial limb ischemia: 30-day results from a single-center experience. Catheter. Cardiovasc. Interv. 2012, 80, 636–643. [Google Scholar] [CrossRef]
- Björck, M.; Earnshaw, J.J.; Acosta, S.; Gonçalves, F.B.; Cochennec, F.; Debus, E.S.; Hinchliffe, R.; Jongkind, V.; Koelemay, M.J.; Menyhei, G.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2020 Clinical Practice Guidelines on the Management of Acute Limb Ischaemia. Eur. J. Vasc. Endovasc. Surg. 2019, 59, 173–218. [Google Scholar] [CrossRef]
- Investigators, S. Results of a prospective randomized trial evaluating surgery versus thrombolysis for ischemia of the lower extremity. Ann. Surg. 1994, 220, 251–266. [Google Scholar]
- Ouriel, K.; Veith, F.J.; Sasahara, A.A. A Comparison of Recombinant Urokinase with Vascular Surgery as Initial Treatment for Acute Arterial Occlusion of the Legs. N. Engl. J. Med. 1998, 338, 1105–1111. [Google Scholar] [CrossRef]
- Veenstra, E.B.; Van Der Laan, M.J.; Zeebregts, C.J.; De Heide, E.-J.; Kater, M.; Bokkers, R.P. A systematic review and meta-analysis of endovascular and surgical revascularization techniques in acute limb ischemia. J. Vasc. Surg. 2019, 71, 654–668. [Google Scholar] [CrossRef]
- Taha, A.G.; Byrne, R.M.; Avgerinos, E.D.; Marone, L.K.; Makaroun, M.S.; Chaer, R.A. Comparative effectiveness of endovascular versus surgical revascularization for acute lower extremity ischemia. J. Vasc. Surg. 2015, 61, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Rutherford, R.B.; Baker, J.; Ernst, C.; Johnston, K.; Porter, J.M.; Ahn, S.; Jones, D.N. Recommended standards for reports dealing with lower extremity ischemia: Revised version. J. Vasc. Surg. 1997, 26, 517–538. [Google Scholar] [CrossRef]
- Lukasiewicz, A.; Lichota, W.; Thews, M. Outcomes of accelerated catheter-directed thrombolysis in patients with acute arterial thrombosis. Vasc. Med. 2016, 21, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.B.; Choi, H.C.; Lee, S.M.; Na, J.B.; Park, M.J.; Shin, H.S.; Won, J.H.; Lee, C.E.; Park, S.E. Combined treatment (image-guided thrombectomy and endovascular therapy with open femoral access) for acute lower limb ischemia: Clinical efficacy and outcomes. PLoS ONE 2019, 14, e0225136. [Google Scholar] [CrossRef] [PubMed]
- Weeda, E.R.; Bohm, N. Association between comorbid cancer and outcomes among admissions for acute ischemic stroke receiving systemic thrombolysis. Int. J. Stroke 2018, 14, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Tehan, P.E.; Sebastian, M.; Barwick, A.; Chuter, V.H. How sensitive and specific is continuous-wave Doppler for detecting peripheral arterial disease in people with and without diabetes? A cross-sectional study. Diabetes Vasc. Dis. Res. 2018, 15, 396–401. [Google Scholar] [CrossRef] [PubMed]
- Cao, P.; Eckstein, H.H.; De Rango, P.; Setacci, C.; Ricco, J.B.; de Donato, G.; Becker, F.; Robert-Ebadi, H.; Diehm, N.; Schmidli, J. Chapter II: Diagnostic methods. Eur. J. Vasc. Endovasc. Surg. 2011, 42, 13–32. [Google Scholar] [CrossRef]
- Olinic, D.M.; Stanek, A.; Tataru, A.-D.; Homorodean, C.; Olinic, M. Acute Limb Ischemia: An Update on Diagnosis and Management. J. Clin. Med. 2019, 8, 1215. [Google Scholar] [CrossRef]
- Hofmann, W.J.; Forstner, R.; Kofler, B.; Binder, K.; Ugurluoglu, A.; Magometschnigg, H. Pedal artery imaging—A comparison of selective digital subtraction angiography, contrast enhanced magnetic resonance angiography and duplex ultrasound. Eur. J. Vasc. Endovasc. Surg. 2002, 24, 287–292. [Google Scholar] [CrossRef][Green Version]
- Clinical classification of acute limb ischemia. J. Vasc. Surg. 2000, 31, 142–145.
- Lipsitz, E.C.; Veith, F.J. Fluoroscopically assisted thromboembolectomy: Should it be routine? Semin. Vasc. Surg. 2001, 14, 100–106. [Google Scholar] [CrossRef]
- Zaraca, F.; Stringari, C.; Ebner, J.A.; Ebner, H. Routine versus selectiveuse of intraoperative angiography during thromboembolectomy for acute lower limb ischemia: Analysis of outcomes. Ann. Vasc. Surg. 2010, 24, 621–627. [Google Scholar] [CrossRef]
- Byrne, R.M.; Taha, A.G.; Avgerinos, E.D.; Marone, L.K.; Makaroun, M.S.; Chaer, R.A. Contemporary outcomes of endovascular interventions for acute limb ischemia. J. Vasc. Surg. 2014, 59, 988–995. [Google Scholar] [CrossRef] [PubMed]
- Varki A Trousseau’s syndrome: Multiple definitions and multiple mechanisms. Blood 2007, 110, 1723–1729. [CrossRef] [PubMed]
| Thrombolysis Degree | Description |
|---|---|
| 0 | No effect of thrombolysis visible on angiography |
| 1 | Partial lysis without axial flow |
| 2 | Partial lysis with axial flow reconstitution |
| 3 | Complete thrombus lysis |
| Overall (%) | Surgery/ | Endovascular | p | |
|---|---|---|---|---|
| Hybrid (%) | ||||
| N (%) | 307 | 191 (62.2) | 94 (30.6) | |
| Age | 68 | 67.8 | 68.4 | NS |
| Sex (male) | 208 (67.8) | 120 (62.8) | 75 (79.8) | 0.004 # |
| BMI | 26.6 | 26.7 | 26.2 | NS |
| Duration | 1 * | 1 * | 4 * | <0.0001 ** |
| Rutherford 1 | 82 (26.7) | 39 (20.4) | 36 (38.3) | 0.0013 # |
| Rutherford 2A | 98 (31.9) | 46 (24.1) | 41 (43.6) | 0.001 # |
| Rutherford 2B | 38 (12.4) | 28 (14.7) | 10 (10.6) | NS |
| Rutherford 3 | 89 (29) | 78 (40.8) | 7 (7.4) | 0.00001 # |
| Etiology | 0.00001 ## | |||
| Embolus | 98 (31.9) | 85 (44.5) | 5 (5.3) | |
| Thrombosis | 209 (68.1) | 106 (55.5) | 89 (94.7) | |
| Location | ||||
| Aorta | 10 (3.3) | 7 (3.7) | 1 (1.1) | NS |
| Iliac | 79 (25.7) | 57 (29.8) | 17 (18.9) | 0.054 |
| Femoral | 194 (63.2) | 125 (65.4) | 59 (61.1) | NS |
| Popliteal | 99 (32.2) | 50 (26.2) | 42 (45.6) | 0.002 # |
| Tibial | 72 (23.5) | 34 (17.8) | 31 (34.4) | 0.004 # |
| Multilevel | 105 (34.2) | 50 (30.4) | 41 (43.6) | 0.003# |
| Smoker | 196 (66.7) | 113 (62.1) | 74 (80.4) | 0.001 # |
| HA | 170 (55.4) | 105 (55) | 54 (57.4) | NS |
| CAD | 102 (33.2) | 70 (36.6) | 22 (23.4) | 0.02 # |
| DM | 75 (24.4) | 49 (25.7) | 22 (23.4) | NS |
| CHF | 41 (13.4) | 34 (17.8) | 4 (4.3) | 0.002 # |
| STROKE | 31 (10.1) | 24 (12.6) | 6 (6.5) | NS |
| CRI | 20 (6.5) | 14 (7.3) | 4 (4.3) | NS |
| MI | 12 (3.9) | 11 (5.8) | 0 (0) | 0.02 ## |
| FA | 71 (23.1) | 59 (30.9) | 5 (5.3) | 0.00001 ## |
| ACTIVE CANCER | 43 (13.2) | 35 (18.3) | 4 (4.3) | 0.0008 ## |
| COLD | 21 (6.8) | 12 (6.3) | 6 (6.4) | NS |
| Overall | Surgery/ | Endovascular | p | |
|---|---|---|---|---|
| (307 patients) | Hybrid | (94 patients) | ||
| (191 patients) | ||||
| Procedures | ||||
| Conservative | 22 (7.2) | |||
| Surgical (overall) | 161 (52.4) | |||
| Embolectomy | 85 (27.7) | |||
| Thrombectomy | 83 (27) | |||
| Endarterectomy | 70 (22.8) | |||
| By-pass | 68 (22.2) | |||
| Angiography | 142 (46.3) | |||
| Endovascular (overall) | 94 (30.6) | |||
| Thrombolysis | 89 (29) | |||
| Mechanical thrombectomy | 4 (1.3) | |||
| Angioplasty/stent | 95 (30.9) | |||
| Stentgraft | 6 (2) | |||
| Hybrid | 30 (9.8) | |||
| Postoperative hospitalization | 4! | 5! | 2! | |
| Primary procedure success | 238 (77.5) | 156 (81.7) | 71 (75.5) | NS # |
| Final treatment success | 248 (80.8) | 156 (81.7) | 82 (86.2) | NS # |
| Reintervention | 36 (11.7) | 17 (8.9) | 19 (20.2) | 0.007 # |
| Major amputation (in hospital) | 23 (7.5) | 17 (8.9) | 4 (4.3) | NS * |
| Major amputation (6 months) | 14 (6.1) | 7 (5) | 7 (8.8) | NS * |
| Hospital mortality | 26 (8.5) | 18 (9.4) | 3 (3.2) | 0.09 * |
| Mortality (6 months) | 32 (10.4) | 24 (12.6) | 3 (3.2) | 0.001 * |
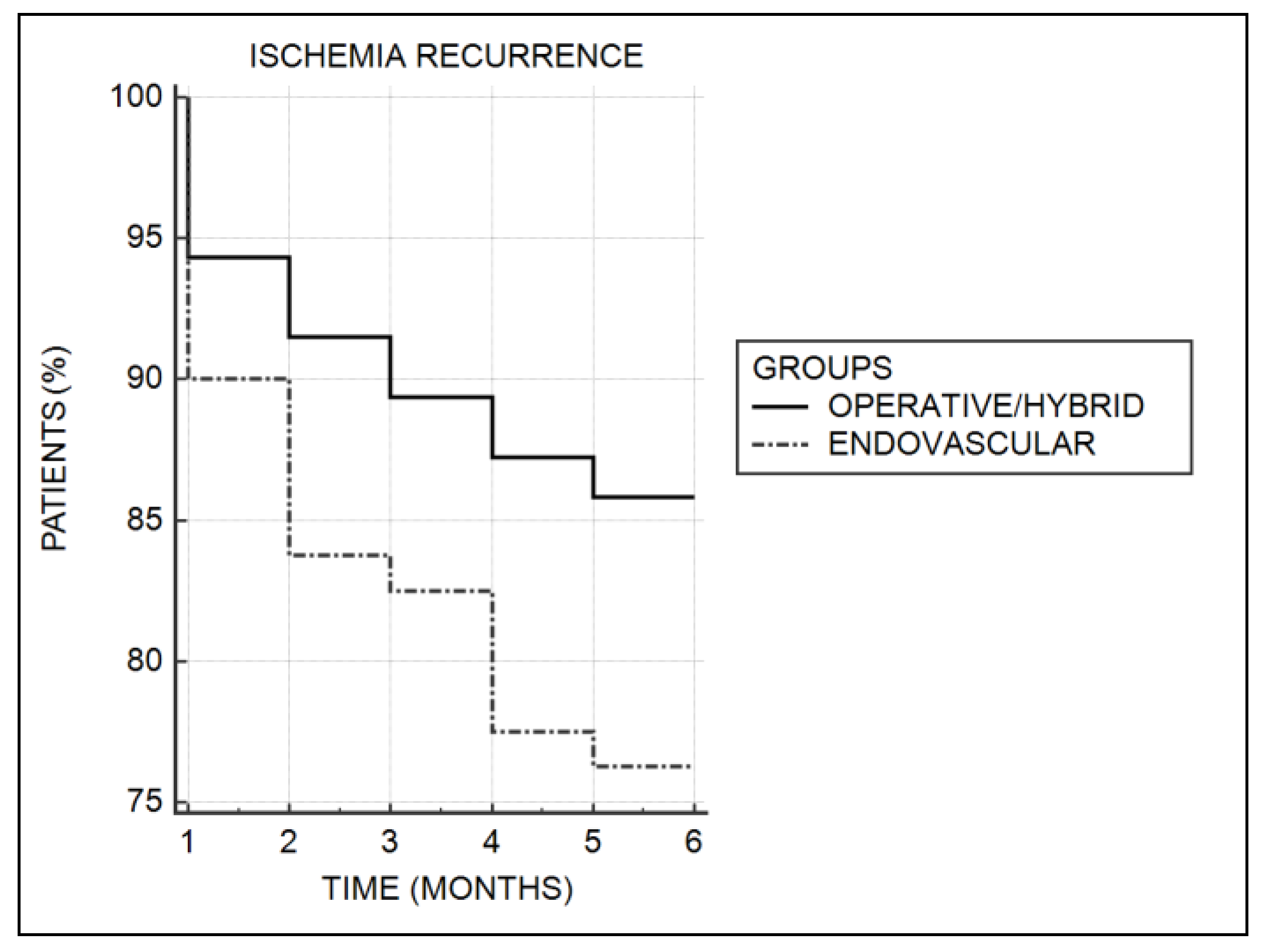
| Recurrent ischemia | 41 (17.7) | 20 (14.3) | 19 (23.8) | 0.07 # |
| Number of Patients (%) | |
|---|---|
| Endoluminal Treatment | 16 (17) |
| Hematoma | 6 (6.4) |
| Bleeding | 4 (4.3) |
| Intracranial bleeding | 1 (1.1) |
| Spinal cord hematoma | 1 (1.1) |
| Vascular bypass thrombosis | 1 (1.1) |
| Myocardial infarction | 1 (1.1) |
| Acute heart failure | 1 (1.1) |
| Symptomatic bradycardia | 1 (1.1) |
| Surgical treatment | 60 (34.1) |
| Recurrent thrombosis | 9 (5.1) |
| Multiorgan failure | 8 (4.5) |
| Surgical site infection | 6 (3.4) |
| Hematoma | 6 (3.4) |
| Lymphorrhea | 5 (2.8) |
| Bypass thrombosis | 5 (2.8) |
| Pulmonary edema | 1 (0.6) |
| Cardiac arrest | 3 (1.7) |
| Superior mesenteric artery embolus | 2 (1.1) |
| Surgical site bleeding | 2 (1.1) |
| Bypass infection | 2 (1.1) |
| Acute renal failure | 2 (1.1) |
| Myocardial infarction | 2 (1.1) |
| Gastrointestinal bleeding | 2 (1.1) |
| Hematuria | 2 (1.1) |
| Fever | 1 (0.6) |
| Pneumonia | 1 (0.6) |
| Stroke | 1 (0.6) |
| Hybrid Treatment | 10 (33.3) |
| Hematoma | 2 (6.7) |
| Urinary tract infection | 1 (3.3) |
| Bypass thrombosis | 1 (3.3) |
| Bleeding | 1 (3.3) |
| Acute cardiac failure | 2 (6.7) |
| Acute renal failure | 1 (3.3) |
| Surgical site infection | 1 (3.3) |
| Lymphorrhea | 1 (3.3) |
| Factor | Treatment | Complications | Amputation (p) | Death (p) | Recurrence |
|---|---|---|---|---|---|
| Success (p) | (p) | (p) | |||
| Rutherford class | <0.0001 ## | 0.009 ## | 0.004 ## | 0.0002 ## | 0.04 ## |
| Lesion type | |||||
| Embolus | NS # | NS # | NS # | 0.04 # | 0.053 # |
| Native thrombosis | NS # | 0.03 # | NS # | NS # | 0.03 # |
| Bypass thrombosis | NS # | NS # | NS # | NS # | 0.0001 # |
| Lesion location: | |||||
| Popliteal | NS # | NS # | 0.01 # | NS # | NS # |
| Tibial | 0.01 # | NS # | 0.0001 # | NS # | NS # |
| Multilevel | NS # | NS # | NS # | NS # | 0.01 # |
| Comorbidities | |||||
| ARI | 0.02 * | 0.0001 # | NS # | 0.002 # | NS # |
| CHF | 0.009 # | 0.05 # | 0.01 # | 0.0001 # | NS # |
| CRI | 0.06 # | NS # | NS # | 0.056 # | NS # |
| FA | 0.02 # | 0.02 # | NS # | 0.02 # | NS # |
| MI | NS # | NS # | NS # | <0.0001 # | NS # |
| NEO | NS # | 0.02 # | NS # | NS # | NS # |
| Treatment | |||||
| Conservative | NS # | NS # | NS # | 0.01 # | NS # |
| Complications | 0.0001 # | - | 0.0001 # | <0.0001 # | NS # |
| Reintervention | NS # | NS # | NS # | NS # | 0.04 # |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lukasiewicz, A. Contemporary Management of Acute Lower Limb Ischemia: Determinants of Treatment Choice. J. Clin. Med. 2020, 9, 1501. https://doi.org/10.3390/jcm9051501
Lukasiewicz A. Contemporary Management of Acute Lower Limb Ischemia: Determinants of Treatment Choice. Journal of Clinical Medicine. 2020; 9(5):1501. https://doi.org/10.3390/jcm9051501
Chicago/Turabian StyleLukasiewicz, Aleksander. 2020. "Contemporary Management of Acute Lower Limb Ischemia: Determinants of Treatment Choice" Journal of Clinical Medicine 9, no. 5: 1501. https://doi.org/10.3390/jcm9051501
APA StyleLukasiewicz, A. (2020). Contemporary Management of Acute Lower Limb Ischemia: Determinants of Treatment Choice. Journal of Clinical Medicine, 9(5), 1501. https://doi.org/10.3390/jcm9051501





