Treatment Motivations and Expectations in Patients with Actinic Keratosis: A German-Wide Multicenter, Cross-Sectional Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics Approval
2.2. Setting and Participants
2.3. Survey
2.4. Data Analysis
3. Results
3.1. Characteristics of the Study Population
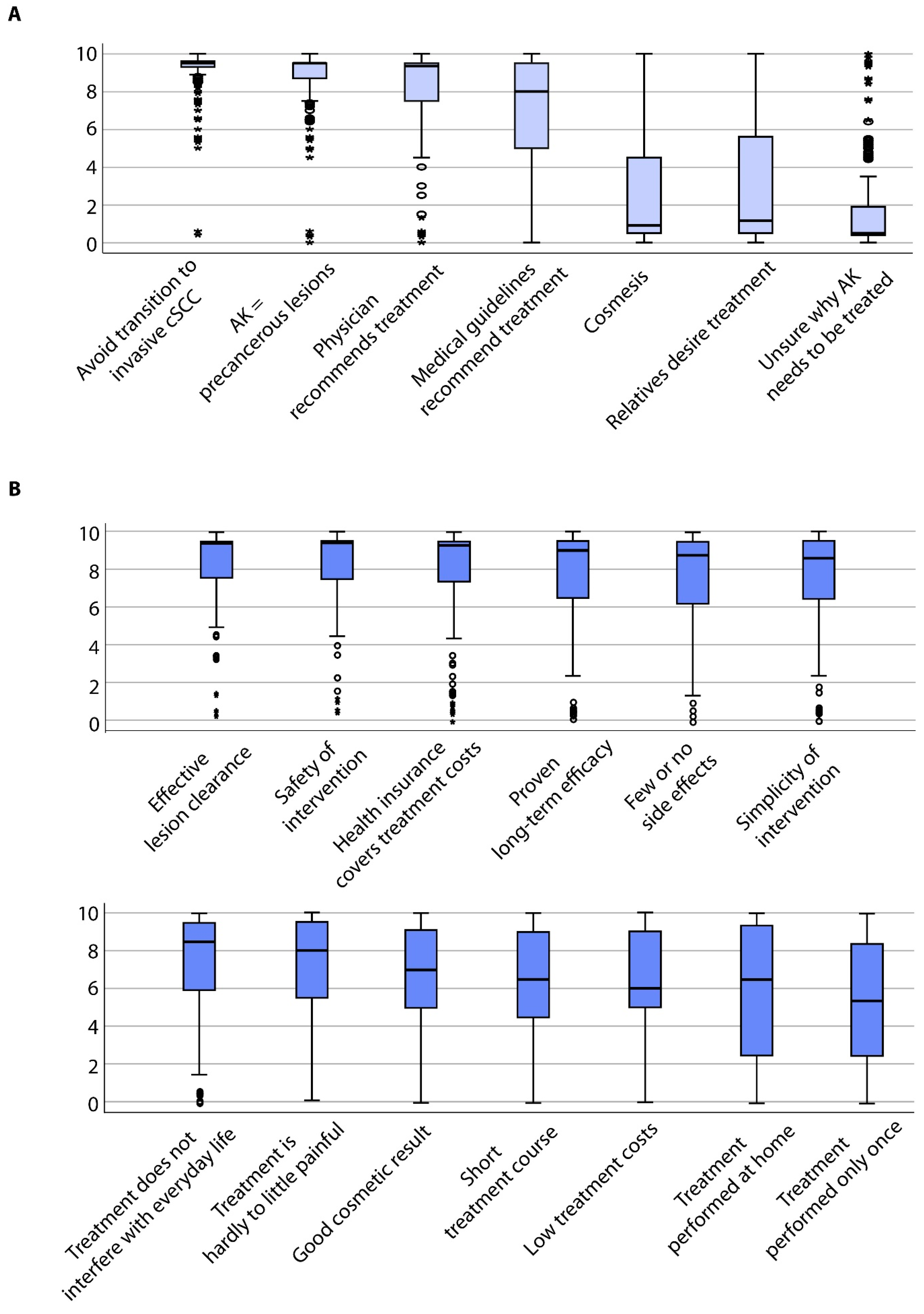
3.2. Items of Treatment Motivation
3.3. Items of Treatment Expectation
3.4. Correlation Analysis of Motivation and Expectation Items
3.5. Clustering Treatment Motivation and Expectation Items to Define Distinct Patient Populations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
Appendix A.1. Subgroup Analysis of Treatment Motivation Items
Appendix A.2. Subgroup Analysis of Treatment Expectation Items
References
- Salasche, S.J. Epidemiology of actinic keratoses and squamous cell carcinoma. J. Am. Acad. Dermatol. 2000, 42, S4–S7. [Google Scholar] [CrossRef]
- Moy, R.L. Clinical presentation of actinic keratoses and squamous cell carcinoma. J. Am. Acad. Dermatol. 2000, 42, S8–S10. [Google Scholar] [CrossRef]
- Röwert-Huber, J.; Patel, M.J.; Forschner, T.; Ulrich, C.; Eberle, J.; Kerl, H.; Sterry, W.; Stockfleth, E. Actinic keratosis is an early in situ squamous cell carcinoma: A proposal for reclassification. Br. J. Dermatol. 2007, 156, 8–12. [Google Scholar] [CrossRef]
- Criscione, V.D.; Weinstock, M.A.; Naylor, M.F.; Luque, C.; Eide, M.J.; Bingham, S.F.; for the Department of Veteran Affairs Topical Tretinoin Chemoprevention Trial Group. Actinic keratoses: Natural history and risk of malignant transformation in the Veterans Affairs Topical Tretinoin Chemoprevention Trial. Cancer 2009, 115, 2523–2530. [Google Scholar] [CrossRef] [PubMed]
- Werner, R.N.; Sammain, A.; Erdmann, R.; Hartmann, V.; Stockfleth, E.; Nast, A. The natural history of actinic keratosis: A systematic review. Br. J. Dermatol. 2013, 169, 502–518. [Google Scholar] [CrossRef] [PubMed]
- Cerio, R.; Dirschka, T.; Dréno, B.; Nart, I.; Lear, J.; Pellacani, G.; Peris, K.; Casas, A. Actinic Keratosis, a Chronic, Progressive Disease: Understanding Clinical Gaps to Optimise Patient Management. Acta Derm. Venereol. 2017, 97, 997–998. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, L.; Gambichler, T.; Kost, C.; Gupta, G.; Stucker, M.; Stockfleth, E.; Dirschka, T. Cutaneous squamous cell carcinomas are associated with basal proliferating actinic keratoses. Br. J. Dermatol. 2018, 180, 916–921. [Google Scholar] [CrossRef] [PubMed]
- Leiter, U.; Heppt, M.V.; Steeb, T.; Amaral, T.; Bauer, A.; Becker, J.C.; Breitbart, E.; Breuninger, H.; Diepgen, T.; Dirschka, T.; et al. S3 guideline for actinic keratosis and cutaneous squamous cell carcinoma (cSCC)—Short version, part 2: Epidemiology, surgical and systemic treatment of cSCC, follow-up, prevention and occupational disease. J. Dtsch. Dermatol. Ges. 2020, 18, 400–413. [Google Scholar] [CrossRef] [PubMed]
- Heppt, M.V.; Leiter, U.; Steeb, T.; Amaral, T.; Bauer, A.; Becker, J.C.; Breitbart, E.; Breuninger, H.; Diepgen, T.; Dirschka, T.; et al. S3 guideline for actinic keratosis and cutaneous squamous cell carcinoma—Short version, part 1: Diagnosis, interventions for actinic keratoses, care structures and quality-of-care indicators. J. Dtsch. Dermatol. Ges. 2020, 18, 275–294. [Google Scholar] [CrossRef]
- Dirschka, T.; Gupta, G.; Micali, G.; Stockfleth, E.; Basset-Séguin, N.; Del Marmol, V.; Dummer, R.; Jemec, G.; Malvehy, J.; Peris, K.; et al. Real-world approach to actinic keratosis management: Practical treatment algorithm for office-based dermatology. J. Dermatol. Treat. 2016, 28, 1–12. [Google Scholar] [CrossRef]
- Bridges, J.F.P.; Hauber, B.; Marshall, D.A.; Lloyd, A.; Prosser, L.A.; Regier, D.A.; Johnson, F.R.; Mauskopf, J. Conjoint Analysis Applications in Health—A Checklist: A Report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Heath 2011, 14, 403–413. [Google Scholar] [CrossRef] [PubMed]
- Kopasker, D.; Kwiatkowski, A.; Matin, R.; Harwood, C.; Ismail, F.; Lear, J.; Thomson, J.; Hasan, Z.-U.; Wali, G.; Milligan, A.; et al. Patient preferences for topical treatment of actinic keratoses: A discrete-choice experiment. Br. J. Dermatol. 2018, 180, 902–909. [Google Scholar] [CrossRef] [PubMed]
- Cerio, R. The importance of patient-centred care to overcome barriers in the management of actinic keratosis. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Berker, D. A discrete-choice experiment and actinic keratosis: What is the answer? Br. J. Dermatol. 2019, 180, 691–692. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, K.A.; Schlessinger, D.I.; Vasic, J.; Iyengar, S.; Qaseem, Y.; Behshad, R.; DeHoratius, D.M.; Denes, P.; Drucker, A.M.; Dzubow, L.M.; et al. Core Outcome Set for Actinic Keratosis Clinical Trials. JAMA Dermatol. 2020, 156, 326. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, U.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P.; Von Elm, E.; Altman, U.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef]
- Tabachniek, B.G.; Fidell, L.S. Book Review: Reply to Widaman’s Review of Using Multivariate Statistics. Appl. Psychol. Meas. 1984, 8, 471. [Google Scholar] [CrossRef]
- Philipp-Dormston, W.G.; Battistella, M.; Boussemart, L.; Di Stefani, A.; Broganelli, P.; Thoms, K.-M. Patient-centered management of actinic keratosis. Results of a multi-center clinical consensus analyzing non-melanoma skin cancer patient profiles and field-treatment strategies. J. Dermatol. Treat. 2019, 1–7. [Google Scholar] [CrossRef]
- Maisel, A.; Waldman, A.; Furlan, K.; Weil, A.; Sacotte, K.; Lazaroff, J.M.; Lin, K.; Aranzazu, D.; Avram, M.M.; Bell, A.; et al. Self-reported Patient Motivations for Seeking Cosmetic Procedures. JAMA Dermatol. 2018, 154, 1167. [Google Scholar] [CrossRef]
- Waldman, A.; Maisel, A.; Weil, A.; Iyengar, S.; Sacotte, K.; Lazaroff, J.M.; Kurumety, S.; Shaunfield, S.L.; Reynolds, K.A.; Poon, E.; et al. Patients believe that cosmetic procedures affect their quality of life: An interview study of patient-reported motivations. J. Am. Acad. Dermatol. 2019, 80, 1671–1681. [Google Scholar] [CrossRef] [PubMed]
- Storer, M.; Zhu, Z.; Sokil, M.; Ford, M.; Neugebauer, R.; Asgari, M.M. Community-Based Practice Variations in Topical Treatment of Actinic Keratoses. JAMA Dermatol. 2017, 153, 468–470. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Roman, J.; Elpern, D.J. Helping Patients Decide on Treatment Options for Actinic Keratosis-Living in Cryo Nation. JAMA Dermatol. 2017, 153, 251–253. [Google Scholar] [CrossRef] [PubMed]
- Noels, E.; Lugtenberg, M.; Egmond, S.; Droger, S.; Buis, P.; Nijsten, T.; Wakkee, M. Insight into the management of actinic keratosis: A qualitative interview study among general practitioners and dermatologists. Br. J. Dermatol. 2019, 181, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Berry, K.; Butt, M.; Kirby, J.S. Influence of Information Framing on Patient Decisions to Treat Actinic Keratosis. JAMA Dermatol. 2017, 153, 421–426. [Google Scholar] [CrossRef]


| Sample | % (n) |
|---|---|
| Sex (n = 399) | |
| Female | 26.3 (105) |
| Male | 73.7 (294) |
| Age (n = 395) | |
| years (median, range) | 77 (43–94) |
| years (mean ± standard deviation) | 75.10 ± 9.45 |
| Family status (n = 396) | |
| Single/unmarried | 5.3 (21) |
| Married | 73.5 (291) |
| Divorced | 5.6 (22) |
| Widowed | 15.7 (62) |
| Risk exposure for skin cancer (n = 333) | |
| Yes | 9.0 (30) |
| No | 91.0 (303) |
| Health insurance (n = 396) | |
| Statutory health insurance | 76.8 (304) |
| Private health insurance | 23.2 (92) |
| Immunosuppression (n = 382) | |
| No | 92.1 (352) |
| Yes | 7.9 (30) |
| Organ transplant recipient | 56.7 (17) |
| Autoimmune disease | 16.7 (5) |
| Other | 26.7 (8) |
| Previous treatment of AK (n = 396) | |
| Yes | 83.6 (331) |
| No | 15.4 (61) |
| Unsure | 1.0 (4) |
| Last treatment of AK (n = 292) | |
| months (median, range) | 6 (0–300) |
| months (mean ± standard deviation) | 18.62 ± 32.35 |
| Number of AK to be treated at the visit (n = 351) | |
| 1–3 | 47.6 (167) |
| 4–6 | 22.5 (79) |
| ≥7 | 29.9 (105) |
| Outdoor profession (n = 333) | |
| Yes | 9.0 (30) |
| No | 91.0 (303) |
| Localization of AK (n = 398) | |
| Scalp | 57.3 (228) |
| Face | 61.6 (245) |
| Trunk | 8.0 (32) |
| Extremities | 31.4 (125) |
| Only face/scalp | 65.5 (261) |
| Only trunk/extremities | 10.6 (42) |
| All sites | 23.9 (95) |
| Treatment Motivation | Treatment Expectation | |||||
|---|---|---|---|---|---|---|
| Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 | |||
| Leading item |  Physician recommendation |  Unclear why AK need treatment |  Simplicity |  No impairment in daily life |  Safety | |
| Associated items | (+) AK = precancerous condition Avoid transition to cSCC | (−) Physician recommendation AK = precancerous condition Avoid transition to cSCC | (+) Desire of relatives | (+) Safety Few adverse events Little painfulness | (+) Few adverse events Little painfulness | (+) Long-term efficacy Effective lesion clearance Few adverse events Little painfulness |
| Patient characteristic | Well informed about condition Fear of AK progress | Indifferent to condition May be approached by relatives Intrinsic and extrinsic motivation deficits | The convenient patient Motivated for treatment if it does not interfere with daily life | Discerning and rational-thinking patient Highly motivated but with high expectations of treatment | ||
| Degree of motivation | High | Low | Moderate | High | ||
| Degree of expectation | Moderate | Low | High | High | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Steeb, T.; Wessely, A.; von Bubnoff, D.; Dirschka, T.; Drexler, K.; Falkenberg, C.; Hassel, J.C.; Hayani, K.; Hüning, S.; Kähler, K.C.; et al. Treatment Motivations and Expectations in Patients with Actinic Keratosis: A German-Wide Multicenter, Cross-Sectional Trial. J. Clin. Med. 2020, 9, 1438. https://doi.org/10.3390/jcm9051438
Steeb T, Wessely A, von Bubnoff D, Dirschka T, Drexler K, Falkenberg C, Hassel JC, Hayani K, Hüning S, Kähler KC, et al. Treatment Motivations and Expectations in Patients with Actinic Keratosis: A German-Wide Multicenter, Cross-Sectional Trial. Journal of Clinical Medicine. 2020; 9(5):1438. https://doi.org/10.3390/jcm9051438
Chicago/Turabian StyleSteeb, Theresa, Anja Wessely, Dagmar von Bubnoff, Thomas Dirschka, Konstantin Drexler, Conrad Falkenberg, Jessica C. Hassel, Kinan Hayani, Svea Hüning, Katharina C. Kähler, and et al. 2020. "Treatment Motivations and Expectations in Patients with Actinic Keratosis: A German-Wide Multicenter, Cross-Sectional Trial" Journal of Clinical Medicine 9, no. 5: 1438. https://doi.org/10.3390/jcm9051438
APA StyleSteeb, T., Wessely, A., von Bubnoff, D., Dirschka, T., Drexler, K., Falkenberg, C., Hassel, J. C., Hayani, K., Hüning, S., Kähler, K. C., Karrer, S., Krammer, C., Leiter, U., Lill, D., Marsela, E., Meiwes, A., Nashan, D., Nasifoglu, S., Schmitz, L., ... Heppt, M. V. (2020). Treatment Motivations and Expectations in Patients with Actinic Keratosis: A German-Wide Multicenter, Cross-Sectional Trial. Journal of Clinical Medicine, 9(5), 1438. https://doi.org/10.3390/jcm9051438








