ECG Indices Poorly Predict Left Ventricular Hypertrophy and Are Applicable Only in Individuals with Low Cardiovascular Risk
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Data Collection and Assays
2.3. Ethical Issues
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. Clinical and Biochemical Factors
4.2. Electrocardiographic Indicators
4.3. Health Related Quality of Life
4.4. Limitation
4.5. Clinical Applications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Levy, D.; Garrison, R.J.; Savage, D.D.; Kannel, W.B.; Castelli, W.P. Left Ventricular Mass and Incidence of Coronary Heart Disease in an Elderly Cohort. Ann. Intern. Med. 1989, 110, 101. [Google Scholar] [CrossRef]
- Koren, M.J.; Devereux, R.B.; Casale, P.N.; Savage, D.D.; Laragh, J.H. Relation of Left Ventricular Mass and Geometry to Morbidity and Mortality in Uncomplicated Essential Hypertension. Ann. Intern. Med. 1991, 114, 345. [Google Scholar] [CrossRef]
- Aronow, W.S.; Fleg, J.L.; Pepine, C.J.; Artinian, N.T.; Bakris, G.; Brown, A.S.; Ferdinand, K.C.; Forciea, M.A.; Frishman, W.H.; Jaigobin, C.; et al. ACCF/AHA 2011 Expert Consensus Document on Hypertension in the Elderly. Circulation 2011, 123, 2434–2506. [Google Scholar] [CrossRef]
- Aronow, W.S.; Ahn, C.; Kronzon, I.; Koenigsberg, M. Congestive heart failure, coronary events and atherothrombotic brain infarction in elderly blacks and whites with systemic hypertension and with and without echocardiographic and electrocardiographic evidence of left ventricular hypertrophy. Am. J. Cardiol. 1991, 67, 295–299. [Google Scholar] [CrossRef]
- Kannel, W.B.; Dannenberg, A.L.; Levy, D. Population implications of electrocardiographic left ventricular hypertrophy. Am. J. Cardiol. 1987, 60, 85–93. [Google Scholar] [CrossRef]
- Levy, D.; Garrison, R.J.; Savage, D.D.; Kannel, W.B.; Castelli, W.P. Prognostic Implications of Echocardiographically Determined Left Ventricular Mass in the Framingham Heart Study. N. Engl. J. Med. 1990, 322, 1561–1566. [Google Scholar] [CrossRef]
- Bluemke, D.A.; Kronmal, R.A.; Lima, J.A.; Liu, K.; Olson, J.; Burke, G.L.; Folsom, A.R. The Relationship of Left Ventricular Mass and Geometry to Incident Cardiovascular Events. J. Am. Coll. Cardiol. 2008, 52, 2148–2155. [Google Scholar] [CrossRef] [PubMed]
- Kannel, W.B. Prevalence and natural history of electrocardiographic left ventricular hypertrophy. Am. J. Med. 1983, 75, 4–11. [Google Scholar] [CrossRef]
- Moser, M. Initial workup of the hypertensive patients. In Hypertensive Primer: The Essential of High Blood Pressure; Williams and Wilkins: Philadelphia, PA, USA, 1998. [Google Scholar]
- Rawshani, A.; Rawshani, A.; Franzen, S.; Eliasson, B.; Svensson, A.-M.; Miftaraj, M.; McGuire, D.K.; Sattar, N.; Rosengren, A.; Gudbjörnsdottir, S. Mortality and Cardiovascular Disease in Type 1 and Type 2 Diabetes. N. Engl. J. Med. 2017, 376, 1407–1418. [Google Scholar] [CrossRef]
- Ohira, T.; Iso, H. Cardiovascular Disease Epidemiology in Asia. Circ. J. 2013, 77, 1646–1652. [Google Scholar] [CrossRef]
- WHO. Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation; WHO: Geneva, Switzerland, 2008; pp. 8–11. [Google Scholar]
- Sokolow, M.; Lyon, T.P. The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am. Hear. J. 1949, 37, 161–186. [Google Scholar] [CrossRef]
- Casale, P.N.; Devereux, R.B.; Alonso, D.R.; Campo, E.; Kligfield, P. Improved sex-specific criteria of left ventricular hypertrophy for clinical and computer interpretation of electrocardiograms: Validation with autopsy findings. Circulation 1987, 75, 565–572. [Google Scholar] [CrossRef] [PubMed]
- Feldstein, C.A.; Akopian, M.; Olivieri, A.O.; Kramer, A.P.; Nasi, M.; Garrido, D. A comparison of body mass index and waist-to-hip ratio as indicators of hypertension risk in an urban Argentine population: A hospital-based study. Nutr. Metab. Cardiovasc. Dis. 2005, 15, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Mattar, J.A. A Simple Calculation to Estimate Body Surface Area in Adults and Its Correlation with the Du Bois Formula. Crit. Care Med. 1989, 17, 846. [Google Scholar] [CrossRef] [PubMed]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; Gonzalez-Juanatey, J.R.; Harjola, V.-P.; A Jankowska, E.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Hear. J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F.; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Hear. J. Cardiovasc. Imaging 2016, 17, 1321–1360. [Google Scholar] [CrossRef]
- Touboul, P.-J.; Hennerici, M.; Meairs, S.; Adams, H.; Amarenco, P.; Bornstein, N.; Csiba, L.; Desvarieux, M.; Ebrahim, S.; Fatar, M.; et al. Mannheim Carotid Intima-Media Thickness Consensus (2004–2006). Cerebrovasc. Dis. 2006, 23, 75–80. [Google Scholar] [CrossRef]
- Barnett, H.J.M.; Taylor, D.W.; Haynes, R.B.; Sackett, D.L.; Peerless, S.J.; Ferguson, G.G.; Fox, A.J.; Rankin, R.N.; Hachinski, V.C.; Wiebers, D.O.; et al. Beneficial Effect of Carotid Endarterectomy in Symptomatic Patients with High-Grade Carotid Stenosis. N. Engl. J. Med. 1991, 325, 445–453. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; A Ference, B.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Hear. J. 2019, 41, 111–188. [Google Scholar] [CrossRef]
- Zdrojewski, T.R.; Jankowski, P.; Bandosz, P.; Bartuś, S.; Chwojnicki, K.; Drygas, W.; Gaciong, Z.; Hoffman, P.; Kalarus, Z.; Kaźmierczak, J.; et al. A new version of cardiovascular risk assessment system and risk charts calibrated for Polish population. Kardiol. Pol. 2015, 73, 958–961. [Google Scholar] [CrossRef]
- Conroy, R.; Pyörälä, K.; Fitzgerald, A.; Sans, S.; Menotti, A.; De Backer, G.; De Bacquer, D.; Ducimetière, P.; Jousilahti, P.; Keil, U.; et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur. Hear. J. 2003, 24, 987–1003. [Google Scholar] [CrossRef]
- Janssen, B.M.; Birnie, E.; Bonsel, G.J. Quantification of the level descriptors for the standard EQ-5D three-level system and a five-level version according to two methods. Qual. Life Res. 2008, 17, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Schisterman, E.F.; Perkins, N.; Liu, A.; Bondell, H.D. Optimal Cut-point and Its Corresponding Youden Index to Discriminate Individuals Using Pooled Blood Samples. Epidemiology 2005, 16, 73–81. [Google Scholar] [CrossRef]
- Okin, P.M.; Wachtell, K.; Devereux, R.B.; Harris, K.E.; Jern, S.; Kjeldsen, S.E.; Julius, S.; Lindholm, L.H.; Nieminen, M.S.; Edelman, J.M.; et al. Regression of Electrocardiographic Left Ventricular Hypertrophy and Decreased Incidence of New-Onset Atrial Fibrillation in Patients With Hypertension. JAMA 2006, 296, 1242. [Google Scholar] [CrossRef]
- Rials, S.J.; Wu, Y.; Xu, X.; Filart, R.A.; Marinchak, R.A.; Kowey, P.R. Regression of left ventricular hypertrophy with captopril restores normal ventricular action potential duration, dispersion of refractoriness, and vulnerability to inducible ventricular fibrillation. Circulation 1997, 96, 1330–1336. [Google Scholar] [CrossRef]
- Wachtell, K.; Palmieri, V.; Olsen, M.H.; Gerdts, E.; Papademetriou, V.; Nieminen, M.S.; Smith, G.; Dahlöf, B.; Aurigemma, G.P.; Devereux, R.B. Change in systolic left ventricular performance after 3 years of antihypertensive treatment: The Losartan Intervention for Endpoint (LIFE) Study. Circulation 2002, 106, 227–232. [Google Scholar] [CrossRef]
- Verdecchia, P.; Angeli, F.; Borgioni, C.; Gattobigio, R.; De Simone, G.; Devereux, R.B.; Porcellati, C. Changes in cardiovascular risk by reduction of left ventricular mass in hypertension: A meta-analysis. Am. J. Hypertens. 2003, 16, 895–899. [Google Scholar] [CrossRef]
- Schirmer, H.; Lunde, P.; Rasmussen, K. Prevalence of left ventricular hypertrophy in a general population; The Tromsø Study. Eur. Heart J. 1999, 20, 429–438. [Google Scholar] [CrossRef]
- Elffers, T.; Trompet, S.; De Mutsert, R.; Maan, A.C.; Lamb, H.J.; Macfarlane, P.W.; Rosendaal, F.R.; Jukema, J.W. Electrocardiographic Detection of Left Ventricular Hypertrophy; Adding Body Mass Index and Spatial QRS-T Angle: A Cross-Sectional Study. Cardiol. Ther. 2019, 8, 345–356. [Google Scholar] [CrossRef]
- Tanaka, K.; Tanaka, F.; Onoda, T.; Tanno, K.; Ohsawa, M.; Sakata, K.; Omama, S.; Ogasawara, K.; Ishibashi, Y.; Itai, K.; et al. Prognostic Value of Electrocardiographic Left Ventricular Hypertrophy on Cardiovascular Risk in a Non-Hypertensive Community-Based Population. Am. J. Hypertens. 2018, 31, 895–901. [Google Scholar] [CrossRef]
- Schillaci, G.; De Simone, G.; Reboldi, G.; Porcellati, C.; Devereux, R.B.; Verdecchia, P. Change in cardiovascular risk profile by echocardiography in low- or medium-risk hypertension. J. Hypertens. 2002, 20, 1519–1525. [Google Scholar] [CrossRef] [PubMed]
- Mancusi, C.; Angeli, F.; Verdecchia, P.; Poltronieri, C.; De Simone, G.; Reboldi, G. Echocardiography in Low-Risk Hypertensive Patients. J. Am. Heart Assoc. 2019, 8, e013497. [Google Scholar] [CrossRef] [PubMed]
- Karakan, S.; Inan, B. The relationship between left ventricular mass index and body composition in new-diagnosed hypertensive patients. Clin. Hypertens. 2015, 21, 23. [Google Scholar] [CrossRef] [PubMed]
- Sagie, A.; Benjamin, E.J.; Galderisi, M.; Larson, M.G.; Evans, J.C.; Fuller, D.L.; Lehman, B.; Levy, D. Echocardiographic assessment of left ventricular structure and diastolic filling in elderly subjects with borderline isolated systolic hypertension (the Framingham Heart Study). Am. J. Cardiol. 1993, 72, 662–665. [Google Scholar] [CrossRef]
- Post, W.S.; Larson, M.G.; Levy, D. Impact of left ventricular structure on the incidence of hypertension. The Framingham Heart Study. Circulation 1994, 90, 179–185. [Google Scholar] [CrossRef]
- Johnson, D.B.; Dell’Italia, L.J. Cardiac hypertrophy and failure in hypertension. Curr. Opin. Nephrol. Hypertens. 1996, 5, 186–191. [Google Scholar] [CrossRef]
- Post, W.S.; Larson, M.G.; Myers, R.; Galderisi, M.; Levy, D. Heritability of Left Ventricular Mass. Hypertension 1997, 30, 1025–1028. [Google Scholar] [CrossRef]
- Brady, T.M. The Role of Obesity in the Development of Left Ventricular Hypertrophy Among Children and Adolescents. Curr. Hypertens. Rep. 2016, 18, 3. [Google Scholar] [CrossRef]
- Manolio, T.A.; Levy, D.; Garrison, R.J.; Castelli, W.P.; Kannel, W.B. Relation of alcohol intake to left ventricular mass: The Framingham study. J. Am. Coll. Cardiol. 1991, 17, 717–721. [Google Scholar] [CrossRef]
- Shuster, A.; Patlas, M.; Pinthus, J.H.; Mourtzakis, M. The clinical importance of visceral adiposity: A critical review of methods for visceral adipose tissue analysis. Br. J. Radiol. 2012, 85, 1–10. [Google Scholar] [CrossRef]
- Sekikawa, A.; Eguchi, H.; Igarashi, K.; Tominaga, M.; Abe, T.; Fukuyama, H.; Kato, T. Waist to Hip Ratio, Body Mass Index, and Glucose Intolerance from Funagata Population-Based Diabetes Survey in Japan. Tohoku J. Exp. Med. 1999, 189, 11–20. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Krotkiewski, M.; Björntorp, P.; Sjöström, L.; Smith, U. Impact of obesity on metabolism in men and women. Importance of regional adipose tissue distribution. J. Clin. Investig. 1983, 72, 1150–1162. [Google Scholar] [CrossRef] [PubMed]
- Weyer, C.; Foley, J.E.; Bogardus, C.; Tataranni, P.A.; Pratley, R.E. Enlarged subcutaneous abdominal adipocyte size, but not obesity itself, predicts Type II diabetes independent of insulin resistance. Diabetologia 2000, 43, 1498–1506. [Google Scholar] [CrossRef] [PubMed]
- Mulè, G.; Nardi, E.; Cottone, S.; Cusimano, P.; Palermo, A.; Incalcaterra, F.; Giandalia, M.E.; Cerasola, G. Impact of the metabolic syndrome on total arterial compliance in essential hypertension patients. J. Cardiometab. Syndr. 2007, 2, 84–90. [Google Scholar] [CrossRef]
- Inoue, T.; Arima, H.; Katsuimata, Y.; Iseki, C.; Kinjo, K.; Iseki, K. Development of Electrocardiographic Left Ventricular Hypertrophy and Resting Heart Rate Over Time: Findings From the OGHMA Study. Angiology 2019, 71, 70–76. [Google Scholar] [CrossRef]
- Carlsson, M.B.; Trägårdh, E.; Engblom, H.; Hedström, E.; Wagner, G.; Pahlm, O.; Arheden, H. Left ventricular mass by 12-lead electrocardiogram in healthy subjects: Comparison to cardiac magnetic resonance imaging. J. Electrocardiol. 2006, 39, 67–72. [Google Scholar] [CrossRef]
- Sinning, C.; Keller, T.; Zeller, T.; Ojeda, F.; Schluter, M.; Schnabel, R.; Lubos, E.; Bickel, C.; Lackner, K.J.; Diemert, P.; et al. Association of high-sensitivity assayed troponin I with cardiovascular phenotypes in the general population: The population-based Gutenberg health study. Clin. Res. Cardiol. 2013, 103, 211–222. [Google Scholar] [CrossRef]
- De Lemos, J.A.; Drazner, M.H.; Omland, T.; Ayers, C.R.; Khera, A.; Rohatgi, A.; Hashim, I.; Berry, J.D.; Das, S.R.; Morrow, D.A.; et al. Association of troponin T detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. JAMA 2010, 304, 2503–2512. [Google Scholar] [CrossRef]
- Fatima, N.; Zaman, M.U.; Ishaq, M.; Baloch, D.J.; Bano, M.; Bano, S.; Bano, N.; Bano, N. Impact of glycosylated hemoglobin (HBA1C) on the extent of perfusion abnormalities and left ventricular dysfunction using gated myocardial perfusion imaging and clinical outcomes in diabetic patients. Nucl. Med. Commun. 2013, 34, 489–494. [Google Scholar] [CrossRef]
- Markuszewski, L.; Grycewicz, T.; Pietruszyński, R.; Michałkiewicz, D.; Roszczyk, N. Glycosylated hemoglobin and left ventricular diastolic dysfunction in patients with type 2 diabetes mellitus. Pol. Merkur. Lekarski. 2006, 21, 8–11. [Google Scholar]
- Cuspidi, C.; Negri, F.; Sala, C.; Valerio, C.; Mancia, G. Association of left atrial enlargement with left ventricular hypertrophy and diastolic dysfunction: A tissue Doppler study in echocardiographic practice. Blood Press. 2011, 21, 24–30. [Google Scholar] [CrossRef]
- Vasan, R.S.; Benjamin, E.J.; Larson, M.G.; Leip, E.P.; Wang, T.J.; Wilson, P.W.F.; Levy, D. Plasma Natriuretic Peptides for Community Screening for Left Ventricular Hypertrophy and Systolic Dysfunction. JAMA 2002, 288, 1252–1259. [Google Scholar] [CrossRef]
- Costello-Boerrigter, L.C.; Boerrigter, G.; Redfield, M.M.; Rodeheffer, R.J.; Urban, L.H.; Mahoney, U.W.; Jacobsen, S.; Heublein, D.M.; Burnett, J.C. Amino-Terminal Pro-B-Type Natriuretic Peptide and B-Type Natriuretic Peptide in the General Community. J. Am. Coll. Cardiol. 2006, 47, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Chlabicz, M.; Jamiołkowski, J.; Paniczko, M.; Sowa, P.; Łapińska, M.; Szpakowicz, M.; Jurczuk, N.; Kondraciuk, M.; Raczkowski, A.; Sawicka, E.; et al. Independent Impact of Gynoid Fat Distribution and Free Testosterone on Circulating Levels of N-Terminal Pro-Brain Natriuretic Peptide (NT-proBNP) in Humans. J. Clin. Med. 2019, 9, 74. [Google Scholar] [CrossRef] [PubMed]
- Devereux, R.B.; Wachtell, K.; Gerdts, E.; Boman, K.; Nieminen, M.S.; Papademetriou, V.; Rokkedal, J.; Harris, K.; Aurup, P.; Dahlöf, B. Prognostic Significance of Left Ventricular Mass Change During Treatment of Hypertension. JAMA 2004, 292, 2350. [Google Scholar] [CrossRef] [PubMed]
- Investigators, S.; Yusuf, S.; Pitt, B.; Davis, C.E.; Hood, W.B., Jr.; Cohn, J.N. Effect of Enalapril on Mortality and the Development of Heart Failure in Asymptomatic Patients with Reduced Left Ventricular Ejection Fractions. N. Engl. J. Med. 1992, 327, 685–691. [Google Scholar] [CrossRef]
- Levy, D.; Labib, S.B.; Anderson, K.M.; Christiansen, J.C.; Kannel, W.B.; Castelli, W.P. Determinants of sensitivity and specificity of electrocardiographic criteria for left ventricular hypertrophy. Circulation 1990, 81, 815–820. [Google Scholar] [CrossRef]
- Abergel, E.; Tase, M.; Menard, J.; Chatellier, G. Influence of obesity on the diagnostic value of electrocardiographic criteria for detecting left ventricular hypertrophy. Am. J. Cardiol. 1996, 77, 739–744. [Google Scholar] [CrossRef]
- Pewsner, D.; Jüni, P.; Egger, M.; Battaglia, M.; Sundström, J.; Bachmann, L.M. Accuracy of electrocardiography in diagnosis of left ventricular hypertrophy in arterial hypertension: Systematic review. BMJ 2007, 335, 711. [Google Scholar] [CrossRef]
- Ricciardi, D.; Vetta, G.; Nenna, A.; Picarelli, F.; Creta, A.; Segreti, A.; Cavallaro, C.; Carpenito, M.; Gioia, F.; Di Belardino, N.; et al. Current diagnostic ECG criteria for left ventricular hypertrophy. J. Cardiovasc. Med. 2020, 21, 128–133. [Google Scholar] [CrossRef]
- Courand, P.; Lantelme, P.; Gosse, P. Electrocardiographic detection of left ventricular hypertrophy: Time to forget the Sokolow-Lyon index? Arch. Cardiovasc. Dis. 2015, 108, 277–280. [Google Scholar] [CrossRef] [PubMed]
- Okin, P.M.; Jern, S.; Devereux, R.B.; Kjeldsen, S.E.; Dahlöf, B.; Life, S.G. Effect of Obesity on Electrocardiographic Left Ventricular Hypertrophy in Hypertensive Patients. Hypertension 2000, 35, 13–18. [Google Scholar] [CrossRef][Green Version]
- Shirani, J.; Berezowski, K.; Roberts, W.C. Quantitative measurement of normal and excessive (cor adiposum) subepicardial adipose tissue, its clinical significance, and its effect on electrocardiographic QRS voltage. Am. J. Cardiol. 1995, 76, 414–418. [Google Scholar] [CrossRef]
- Devlin, N.; Brooks, R. EQ-5D and the EuroQol Group: Past, Present and Future. Appl. Health Econ. Health Policy 2017, 15, 127–137. [Google Scholar] [CrossRef] [PubMed]
| Variable Value (n = 676) | |
|---|---|
| Age, years | 48.65 ± 15.26 |
| Male sex | 277 (41.0) |
| SCORE Risk, % | 4.31 |
| BMI, kg/m2 | 26.70 ± 4.85 |
| BMI < 25 kg/m2 | 271 (40.1) |
| BMI 25–29.99 kg/m2 | 244 (36.1) |
| BMI ≥ 30 kg/m2 | 161 (23.8) |
| NT-proBNP, pg/mL | 90.02 ± 183.06 |
| hs-TnT, pg/mL | 6.40 ± 4.95 |
| LVEF biplane, % | 58.13 ± 5.68 |
| Diastolic dysfunction of left ventricle | 84 (12.4) |
| LVMIBMI *, g/m2 | 78.64 ± 21.04 |
| LVMIBMI *, ≥95 g/m2 women, ≥115 g/m2 men | 69 (10.2) |
| LAVI, mL/m2 | 22.60 ± 7.02 |
| LAVI, >34 mL/m2 | 40 (5.9) |
| Sokolow–Lyon index, mm | 22.04 ± 7.09 |
| Sokolow–Lyon index, >35 mm | 32 (4.7) |
| Cornell index, mm | 11.71 ± 5.36 |
| Cornell index, >28 mm men, >20 mm women | 17 (2.5) |
| Lewis index, mm | 2.14 ± 8.40 |
| Lewis index, >17 mm | 23 (3.4) |
| Creatinine, μmoL/L | 70.83 ± 15.34 |
| GFR, mL/min/1.73 m2 | 113.84 ± 35.74 |
| BPs, mmHg | 123.53 ± 18.07 |
| BPd, mmHg | 81.75 ± 10.39 |
| BP ≥ 140 and/or ≥90 mmHg | 167 (24.7) |
| HR, bpm | 72.37 ± 11.09 |
| Carotid plaque | 287 (42.5) |
| History of hypertension | 192(28.4) |
| History of diabetes | 47 (7.0) |
| History of atrial fibrillation | 22 (3.3) |
| History of myocardial infarction | 14 (2.1) |
| History of coronary heart disease | 16 (2.4) |
| History of heart failure | 8 (1.2) |
| History of heart defect | 10 (1.5) |
| History of peripheral artery disease | 6 (0.9) |
| History of stroke | 6 (0.9) |
| Currently smoking | 141 (20.9) |
| Variable | Cardiovascular Risk | |||
|---|---|---|---|---|
| Low Risk n = 345 | Moderate Risk n = 147 | High Risk n = 108 | Very High Risk n = 67 | |
| Male sex | 130 (37.7) | 58 (39.5) | 45 (41.7) | 38 (56.7) |
| Age, years | 39.33 ± 13.14 | 55.17 ± 7.96 | 61.75 ± 9.32 | 65.79 ± 7.65 |
| LVMI *, g/m2 | 73.25 ± 19.18 | 80.70 ± 18.34 | 85.37 ± 21.01 | 89.46 ± 24.37 |
| LVMI *, ≥95 g/m2 women, ≥115 g/m2 men | 17 (5.1) | 15 (10.6) | 20 (19.8) | 11 (17.7) |
| Use of beta-blockers | 21 (6.1) | 38 (25.9) | 30 (27.8) | 37 (55.2) |
| Sokolow–Lyon index, mm | 22.67 ± 7.20 | 21.02 ± 6.63 | 20.82 ± 6.73 | 20.62 ± 6.43 |
| Sokolow–Lyon index, >35 mm | 22 (6.4) | 3 (2.0) | 3 (2.8) | 1 (1.5) |
| Cornell index, mm | 10.78 ± 5.49 | 11.74 ± 4.26 | 12.71 ± 5.09 | 14.43 ± 5.58 |
| Cornell index, >28 mm men, >20 mm women | 9 (2.6) | 2 (1.4) | 1 (0.9) | 3 (4.5) |
| Lewis index, mm | −0.24 ± 8.47 | 4.54 ± 7.01 | 5.75 ± 7.59 | 5.50 ± 7.05 |
| Lewis index, >17 mm | 7 (2.0) | 7 (4.8) | 6 (5.6) | 4 (6.0) |
| Variable | Study Population (n = 676) | ||
|---|---|---|---|
| Subjects without LVHBSA * | Subjects with LVHBSA * | p-Values | |
| Sample size | 607 (89.8) | 69 (10.2) | |
| Male sex | 249 (41.0) | 28 (40.6) | 0.944 |
| Age, years | 47.37 ± 15.08 | 59.93 ± 11.91 | <0.001 |
| BMI, kg/m2 | 26.34 ± 4.74 | 29.87 ± 4.71 | <0.001 |
| BMI < 25 kg/m2 | 261 (43.3) | 10 (14.5) | <0.001 |
| BMI 25–29.99 kg/m2 | 218 (35.9) | 26 (37.7) | <0.001 |
| BMI ≥ 30 kg/m2 | 128 (21.1) | 33 (47.0) | <0.001 |
| SCORE Risk, % | 3.35 | 4.47 | 0.001 |
| Carotid plaque | 238 (39.2) | 49 (71.0) | <0.001 |
| BPs, mmHg | 122.65 ± 17.94 | 131.46 ± 17.44 | <0.001 |
| BPd, mmHg | 81.57 ± 10.34 | 83.38 ± 10.72 | 0.149 |
| HR, bpm | 72.65 ± 11.11 | 69.80 ± 10.65 | 0.044 |
| LVEF BP, % | 58.22 ± 5.57 | 57.28 ± 6.56 | 0.422 |
| LVMIBSA, g/m2 | 74.26 ± 16.20 | 117.20 ± 19.34 | <0.001 |
| LAVI, ml/m2 | 22.16 ± 6.44 | 26.49 ± 10.12 | <0.001 |
| Diastolic dysfunction of left ventricle | 68 (11.2) | 16 (23.2) | 0.004 |
| P wave time, ms | 105.82 ± 10.17 | 112.09 ± 14.48 | <0.001 |
| QRS time, ms | 90.59 ± 9.42 | 93.07 ± 8.48 | 0.019 |
| Sokolow–Lyon index, mm | 22.00 ± 7.04 | 22.38 ± 7.52 | 0.818 |
| Sokolow–Lyon index, > 35 mm | 29 (4.8) | 3(4.3) | 0.873 |
| Cornell index, mm | 11.40 ± 5.24 | 14.49 ± 5.69 | <0.001 |
| Cornell index, >28 mm men, >20 mm women | 14 (2.3) | 3 (4.3) | 0.305 |
| Lewis index, mm | 1.57 ± 8.30 | 7.08 ± 7.65 | <0.001 |
| Lewis index, >17 mm | 16 (2.6) | 7 (10.1) | 0.001 |
| NT-proBNP, pg/mL | 72.79 ± 79.91 | 212.81 ± 460.96 | <0.001 |
| hs-TnT, pg/mL | 5.94 ± 3.81 | 9.73 ± 9.17 | <0.001 |
| Fasting glucose, mg/dL | 99.63 ± 14.73 | 111.22 ± 34.21 | 0.002 |
| 120 min glucose, mg/dL | 121.46 ± 38.06 | 147.96 ± 42.18 | <0.001 |
| Fasting insulin, µUL/mL | 11.32 ± 6.69 | 13.40 ± 8.90 | 0.076 |
| 120 min Insulin, µUL/mL | 58.12 ± 51.52 | 89.27 ± 118.74 | 0.004 |
| HbA1c, % | 5.43 ± 0.48 | 5.90 ± 0.94 | <0.001 |
| HOMA-IR | 2.84 ± 2.04 | 3.71 ± 2.87 | 0.013 |
| GFR, mL/min/1.73 m2 | 114.76 ± 35.98 | 105.77 ± 32.75 | 0.045 |
| hsCRP, mg/L | 1.64 ± 3.36 | 2.67 ± 4.76 | 0.001 |
| Waist, cm | 85.68 ± 13.17 | 93.91 ± 11.17 | <0.001 |
| Hips, cm | 98.73 ± 9.22 | 104.44 ± 9.44 | <0.001 |
| WHR | 0.87 ± 0.10 | 0.90 ± 0.09 | 0.008 |
| FMI, kg/m2 | 8.94 ± 3.50 | 11.16 ± 3.54 | <0.001 |
| % fat | 33.18 ± 7.50 | 35.55 ± 7.06 | 0.017 |
| Total fat mass, kg | 25.38 ± 9.02 | 31.58 ± 8.74 | <0.001 |
| Total lean mass, kg | 48.39 ± 10.70 | 50.08 ± 9.83 | 0.105 |
| Android fat mass, kg | 2.30 ± 1.20 | 3.02 ± 1.10 | <0.001 |
| Android lean mass, kg | 3.30 ± 0.71 | 3.53 ± 0.68 | 0.009 |
| Gynoid fat mass, kg | 3.98 ± 1.37 | 4.59 ± 1.50 | 0.001 |
| Legs fat mass, kg | 7.58 ± 2.72 | 8.52 ± 3.11 | 0.021 |
| Visceral mass, kg | 1.12 ± 0.92 | 1.78 ± 0.98 | <0.001 |
| A/G fat mass ratio | 0.57 ± 0.22 | 0.68 ± 0.22 | <0.001 |
| G/T fat mass ratio | 0.16 ± 0.03 | 0.15 ± 0.02 | 0.005 |
| A/T fat mass ratio | 0.09 ± 0.02 | 0.10 ± 0.02 | <0.001 |
| Legs/T fat mass ratio | 0.31 ± 0.07 | 0.28 ± 0.06 | 0.001 |
| History of hypertension | 159 (26.2) | 33 (47.8) | <0.001 |
| History of diabetes | 34 (5.6) | 13 (18.8) | <0.001 |
| History of atrial fibrillation | 15 (2.5) | 7 (10.1) | 0.001 |
| History of myocardial infarction | 10 (1.6) | 4 (5.8) | 0.022 |
| History of coronary heart disease | 12 (2.0) | 4 (5.8) | 0.049 |
| History of heart failure | 9 (1.5) | 1 (1.4) | 0.979 |
| History of valvular heart defect | 8 (1.3) | 0 (0.0) | 0.336 |
| History of peripheral artery disease | 4 (0.7) | 2 (2.9) | 0.061 |
| History of stroke | 3 (0.5) | 3 (4.3) | 0.001 |
| Use of beta-blockers | 97 (16.0) | 26 (37.7) | <0.001 |
| Currently smoking | 125 (20.6) | 16 (23.2) | 0.630 |
| Variable | Model 1 | Model 2 | ||||||
|---|---|---|---|---|---|---|---|---|
| OR Unstandardized | 95% C.I. | OR Standardized ** | p | OR Unstandardized | 95% C.I. | OR Standardized ** | p | |
| BPs, mmHg | 1.010 | 0.994–1.026 | 1.194 | 0.216 | - | - | - | |
| BPd, mmHg | 1.004 | 0.977–1.032 | 1.043 | 0.773 | - | - | - | |
| HR, bpm | 0.986 | 0.963–1.011 | 0.859 | 0.271 | 0.983 | 0.959–1.009 | 0.829 | 0.192 |
| LVEF BP, % | 1.004 | 0.958–1.053 | 1.024 | 0.862 | 1.014 | 0.964–1.067 | 1.083 | 0.589 |
| LAVI, ml/m2 | 1.044 | 1.008–1.082 | 1.356 | 0.016 | 1.045 | 1.007–1.086 | 1.366 | 0.021 |
| P wave time, ms | 1.021 | 0.994–1.049 | 1.253 | 0.129 | 1.017 | 0.989–1.045 | 1.199 | 0.236 |
| QRS time, ms | 1.046 | 1.010–1.083 | 1.519 | 0.012 | 1.044 | 1.007–1.082 | 1.496 | 0.019 |
| Sokolow–Lyon index, mm | 1.041 | 0.999–1.085 | 1.332 | 0.054 | 1.044 | 1.001–1.089 | 1.357 | 0.047 |
| Cornell index, mm | 1.080 | 1.026–1.137 | 1.510 | 0.003 | 1.071 | 1.015–1.129 | 1.442 | 0.012 |
| Lewis index, mm | 1.042 | 1.005–1.081 | 1.417 | 0.025 | 1.044 | 1.006–1.083 | 1.433 | 0.024 |
| NT-proBNP, pg/mL | 1.002 | 1.000–1.004 | 1.413 | 0.088 | 1.002 | 1.000–1.004 | 1.350 | 0.118 |
| hs-TnT, pg/mL | 1.069 | 1.005–1.137 | 1.392 | 0.034 | 1.077 | 1.006–1.152 | 1.441 | 0.032 |
| Fasting glucose, mg/dL | 1.007 | 0.996–1.019 | 1.142 | 0.218 | 1.008 | 0.994–1.022 | 1.152 | 0.284 |
| 120 min glucose, mg/dL | 1.004 | 0.997–1.012 | 1.176 | 0.274 | 1.006 | 0.998–1.013 | 1.246 | 0.154 |
| Fasting insulin, µUL/mL | 0.983 | 0.942–1.026 | 0.888 | 0.434 | 0.998 | 0.955–1.043 | 0.989 | 0.943 |
| 120 Insulin, µUL/mL | 1.001 | 0.997–1.005 | 1.062 | 0.623 | 1.002 | 0.998–1.006 | 1.156 | 0.252 |
| HbA1c, % | 1.755 | 1.149–2.680 | 1.372 | 0.009 | 1.940 | 1.101–3.418 | 1.451 | 0.022 |
| HOMA-IR | 0.966 | 0.849–1.100 | 0.928 | 0.604 | 1.000 | 0.872–1.147 | 1.000 | 0.998 |
| hsCRP, mg/L | 1.019 | 0.965–1.076 | 1.070 | 0.496 | 1.021 | 0.966–1.079 | 1.076 | 0.460 |
| WHR | 0.126 | 0.002–9.095 | 0.819 | 0.342 | 0.166 | 0.002–13.570 | 0.841 | 0.424 |
| % fat | 0.001 | 0.000–4.083 | 0.613 | 0.107 | 0.003 | 0.000–10.576 | 0.650 | 0.165 |
| Total fat mass, kg | 0.951 | 0.880–1.028 | 0.635 | 0.210 | 0.955 | 0.880–1.036 | 0.655 | 0.267 |
| Total lean mass, kg | 1.038 | 0.980–1.100 | 1.490 | 0.203 | 1.037 | 0.977–1.101 | 1.471 | 0.230 |
| Android fat mass, kg | 0.722 | 0.434–1.199 | 0.673 | 0.208 | 0.764 | 0.444–1.314 | 0.721 | 0.330 |
| Gynoid fat mass, kg | 1.005 | 0.690–1.465 | 1.008 | 0.977 | 1.037 | 0.700–1.535 | 1.051 | 0.858 |
| Legs fat mass, kg | 0.980 | 0.832–1.154 | 0.945 | 0.807 | 0.987 | 0.831–1.174 | 0.965 | 0.885 |
| Visceral mass, kg | 1.039 | 0.631–1.708 | 1.036 | 0.881 | 1.056 | 0.621–1.798 | 1.053 | 0.840 |
| A/G fat mass ratio, % | 0.999 | 0.980–1.018 | 0.970 | 0.890 | 1.001 | 0.981–1.021 | 1.015 | 0.949 |
| G/T fat mass ratio, % | 1.063 | 0.907–1.245 | 1.180 | 0.453 | 1.068 | 0.905–1.262 | 1.197 | 0.436 |
| A/T fat mass ratio, % | 1.034 | 0.829–1.290 | 1.075 | 0.766 | 1.079 | 0.856–1.361 | 1.180 | 0.518 |
| Legs/T fat mass ratio, % | 0.993 | 0.934–1.055 | 0.949 | 0.811 | 0.991 | 0.929–1.057 | 0.938 | 0.780 |
| Risk SCORE, % | 0.995 | 0.914–1.084 | 1.000 | 0.912 | 0.977 | 0.888–1.074 | 0.999 | 0.626 |
| Variable | Model 3 | Model 4 | ||||||
|---|---|---|---|---|---|---|---|---|
| OR Unstandardized | 95% C.I. | OR Standardized ** | p | OR Unstandardized | 95% C.I. | OR Standardized ** | p | |
| BPs, mmHg | 1.012 | 0.997–1.027 | 1.242 | 0.120 | - | - | - | - |
| BPd, mmHg | 1.010 | 0.983–1.038 | 1.112 | 0.461 | - | - | - | - |
| HR, bpm | 0.988 | 0.964–1.012 | 0.871 | 0.316 | 0.984 | 0.960–1.010 | 0.840 | 0.224 |
| LVEF BP, % | 1.001 | 0.955–1.050 | 1.008 | 0.956 | 1.011 | 0.961–1.063 | 1.063 | 0.675 |
| LAVI, ml/m2 | 1.047 | 1.011–1.084 | 1.381 | 0.009 | 1.048 | 1.010–1.088 | 1.389 | 0.014 |
| P wave time, ms | 1.027 | 1.001–1.055 | 1.341 | 0.042 | 1.022 | 0.995–1.050 | 1.261 | 0.118 |
| QRS time, ms | 1.048 | 1.014–1.084 | 1.553 | 0.006 | 1.046 | 1.010–1.082 | 1.517 | 0.012 |
| Sokolow–Lyon index, mm | 1.027 | 0.988–1.068 | 1.211 | 0.176 | 1.034 | 0.992–1.077 | 1.264 | 0.112 |
| Cornell index, mm | 1.082 | 1.029–1.137 | 1.525 | 0.002 | 1.071 | 1.017–1.128 | 1.443 | 0.010 |
| Lewis index, mm | 1.053 | 1.017–1.090 | 1.540 | 0.004 | 1.053 | 1.016–1.091 | 1.539 | 0.005 |
| NT-proBNP, pg/mL | 1.002 | 1.000–1.005 | 1.537 | 0.058 | 1.002 | 1.000–1.004 | 1.468 | 0.077 |
| hs-TnT, pg/mL | 1.078 | 1.014–1.147 | 1.453 | 0.016 | 1.081 | 1.012–1.156 | 1.472 | 0.021 |
| Fasting glucose, mg/dL | 1.011 | 1.000–1.023 | 1.224 | 0.056 | 1.011 | 0.997–1.025 | 1.218 | 0.132 |
| 120 min glucose, mg/dL | 1.007 | 1.000–1.014 | 1.300 | 0.063 | 1.008 | 1.000–1.015 | 1.344 | 0.046 |
| Fasting insulin, µUL/mL | 1.011 | 0.975–1.048 | 1.079 | 0.555 | 1.019 | 0.981–1.060 | 1.145 | 0.329 |
| 120 Insulin, µUL/mL | 1.002 | 0.999–1.006 | 1.154 | 0.231 | 1.003 | 0.999–1.008 | 1.236 | 0.103 |
| HbA1c, % | 1.961 | 1.299–2.961 | 1.460 | 0.001 | 2.127 | 1.212–3.731 | 1.528 | 0.009 |
| HOMA -IR | 1.045 | 0.936–1.167 | 1.100 | 0.434 | 1.063 | 0.942–1.199 | 1.142 | 0.322 |
| hsCRP, mg/L | 1.029 | 0.975–1.085 | 1.106 | 0.296 | 1.028 | 0.975–1.084 | 1.103 | 0.306 |
| WHR | 3.194 | 0.074–137.489 | 1.118 | 0.545 | 2.485 | 0.048–127.726 | 1.092 | 0.651 |
| % fat | 21.797 | 0.052–9204.292 | 1.261 | 0.318 | 16.272 | 0.031–8603.827 | 1.234 | 0.383 |
| Total fat mass, kg | 1.050 | 1.011–1.090 | 1.558 | 0.011 | 1.046 | 1.006–1.088 | 1.510 | 0.024 |
| Total lean mass, kg | 1.076 | 1.025–1.130 | 2.184 | 0.003 | 1.071 | 1.019–1.125 | 2.067 | 0.007 |
| Android fat mass, kg | 1.390 | 1.058–1.826 | 1.491 | 0.018 | 1.380 | 1.027–1.853 | 1.478 | 0.032 |
| Gynoid fat mass, kg | 1.406 | 1.104–1.793 | 1.609 | 0.006 | 1.384 | 1.082–1.771 | 1.573 | 0.010 |
| Legs fat mass, kg | 1.147 | 1.018–1.293 | 1.462 | 0.025 | 1.143 | 1.012–1.292 | 1.450 | 0.032 |
| Visceral mass, kg | 1.608 | 1.124–2.300 | 1.567 | 0.009 | 1.581 | 1.064–2.347 | 1.542 | 0.023 |
| A/G fat mass ratio, % | 1.013 | 0.997–1.030 | 1.350 | 0.112 | 1.013 | 0.995–1.031 | 1.340 | 0.151 |
| G/T fat mass ratio, % | 0.978 | 0.844–1.133 | 0.941 | 0.765 | 1.001 | 0.857–1.171 | 1.004 | 0.985 |
| A/T fat mass ratio, % | 1.232 | 1.028–1.476 | 1.572 | 0.024 | 1.246 | 1.026–1.512 | 1.610 | 0.026 |
| Legs/T fat mass ratio, % | 0.959 | 0.907–1.014 | 0.746 | 0.137 | 0.964 | 0.909–1.023 | 0.776 | 0.226 |
| Risk SCORE, % | 0.988 | 0.909–1.075 | 0.999 | 0.788 | 0.969 | 0.883–1.063 | 0.998 | 0.504 |
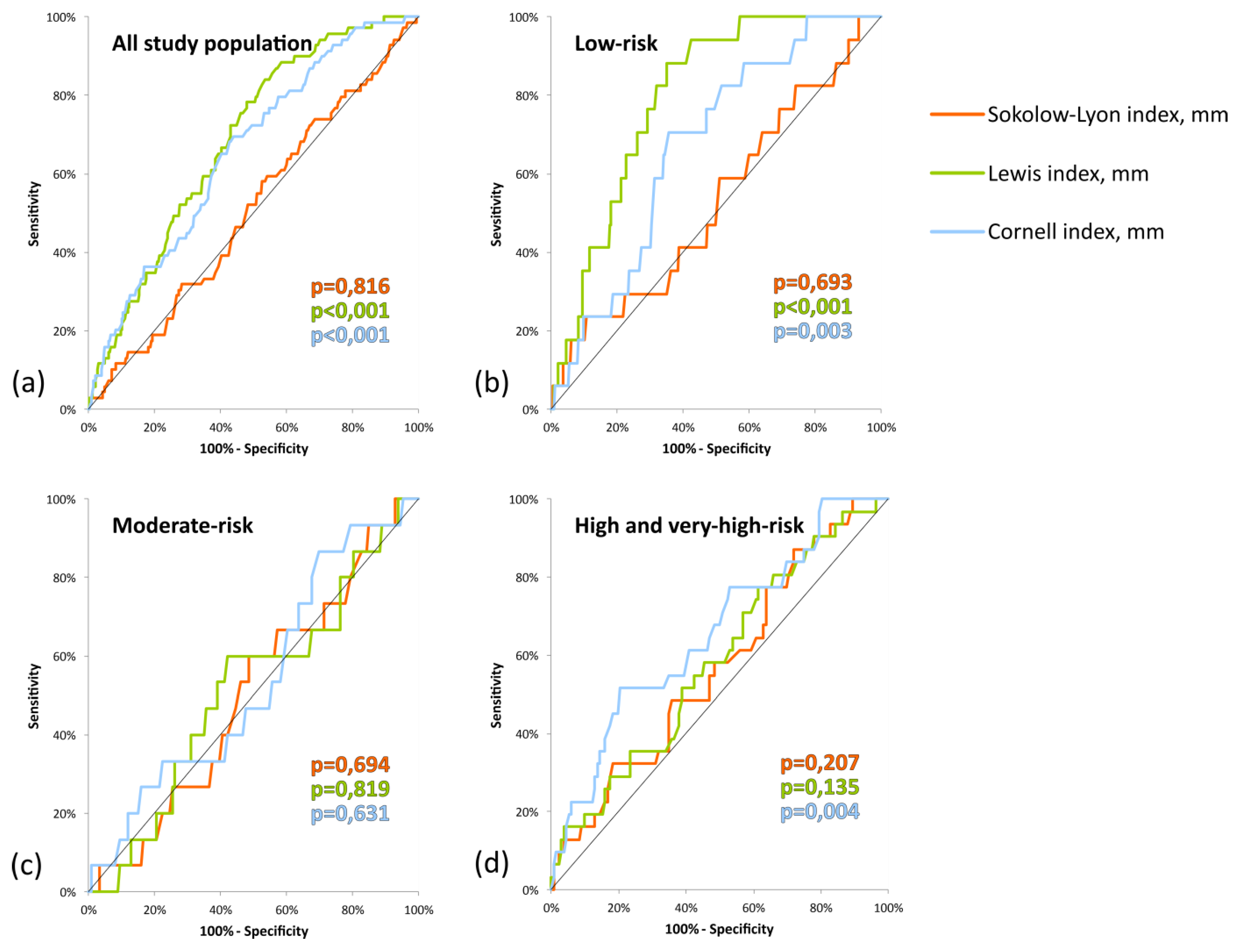
| Study Population | Variable | |||||||
|---|---|---|---|---|---|---|---|---|
| Cut-Off Point, mm | Sensitivity, % | Specificity, % | NPV, % | PPV, % | AUC | 95% C.I. (AUC) | p | |
| All Study Population | ||||||||
| Sokolow–Lyon index, mm | >20.75 | 57.97 | 47.45 | 90.85 | 11.14 | 0.5085 | 0.437–0.580 | 0.8162 |
| Cornell index, mm | >11.55 | 69.57 | 56.01 | 94.18 | 15.24 | 0.6575 ** | 0.593–0.722 | <0.001 |
| Lewis index, mm | >0.15 | 84.06 | 46.62 | 96.26 | 15.18 | 0.6869 ** | 0.628–0.745 | <0.001 |
| Low-Risk | ||||||||
| Sokolow–Lyon index, mm | <15.05 | 23.53 | 89.34 | 95.64 | 10.53 | 0.5300 | 0.381–0.679 | 0.6932 |
| Cornell index, mm | >11.55 | 70.59 | 64.26 | 97.62 | 9.52 | 0.6708 | 0.559–0.783 | 0.0027 |
| Lewis index, mm | >0.75 | 88.24 | 64.89 | 99.04 | 11.81 | 0.7966 ** | 0.718–0.875 | <0.001 |
| Moderate-Risk | ||||||||
| Sokolow–Lyon index, mm | >21.05 | 60.00 | 51.59 | 91.55 | 12.86 | 0.5034 | 0.355–0.652 | 0.9638 |
| Cornell index, mm | <13.75 | 86.67 | 30.16 | 95.00 | 12.87 | 0.5376 | 0.384–0.691 | 0.6309 |
| Lewis index, mm | <3.35 | 60.00 | 57.94 | 92.41 | 14.52 | 0.5183 | 0.362–0.674 | 0.8187 |
| High and Very-High Risk | ||||||||
| Sokolow–Lyon index, mm | >16.20 | 87.10 | 28.03 | 90.24 | 22.13 | 0.5714 | 0.461–0.682 | 0.2066 |
| Cornell index, mm | >16.30 | 51.61 | 79.55 | 87.50 | 37.21 | 0.6581 | 0.550–0.766 | 0.0042 |
| Lewis index, mm | >2.50 | 77.42 | 38.64 | 87.93 | 22.86 | 0.5844 | 0.474–0.695 | 0.1351 |
| Study Population | Variable | |||||||
| Cut-Off Point, mm | Sensitivity, % * | Cut-Off Point, mm | Sensitivity, % ** | Cut-Off Point, mm | Specificity, % *** | Cut-Off Point, mm | Specificity, % **** | |
| All Study Population | ||||||||
| Sokolow–Lyon index, mm | >30.85 | 11.59 | >27.85 | 18.84 | >13.45 | 9.23 | >16.35 | 22.41 |
| Cornell index, mm | >18.36 | 21.74 | >15.65 | 36.23 | >8.05 | 28.83 | >9.45 | 40.53 |
| Lewis index, mm | >12.55 | 20.29 | >8.90 | 34.78 | >−2.70 | 32.95 | >0.65 | 48.93 |
| Low-Risk | ||||||||
| Sokolow–Lyon index, mm | <14.95 | 17.65 | <16.55 | 23.53 | <33.15 | 10.03 | <26.85 | 26.02 |
| Cornell index, mm | >18.15 | 23.53 | >14.50 | 29.41 | >6.85 | 27.90 | >9.35 | 48.28 |
| Lewis index, mm | >11.50 | 29.41 | >6.95 | 52.94 | >-0.30 | 59.25 | >1.35 | 68.03 |
| Moderate-Risk | ||||||||
| Sokolow–Lyon index, mm | >29.90 | 6.67 | >27.20 | 13.33 | >13.50 | 15.08 | >14.10 | 20.63 |
| Cornell index, mm | <7.15 | 13.33 | <8.35 | 26.67 | <15.30 | 20.63 | <13.50 | 32.54 |
| Lewis index, mm | <−4.00 | 6.67 | <−1.90 | 13.33 | <12.35 | 11.11 | <9.50 | 20.63 |
| High and Very-High Risk | ||||||||
| Sokolow–Lyon index, mm | >29.60 | 16.13 | >25.25 | 32.26 | >15.45 | 21.97 | >17.05 | 29.55 |
| Cornell index, mm | >18.90 | 22.58 | >16.45 | 45.16 | >8.90 | 20.45 | >10.35 | 30.30 |
| Lewis index, mm | >15.10 | 19.35 | >11.25 | 29.03 | >−1.00 | 21.97 | >1.70 | 34.09 |
| CV Risk | Frequency of Exertion Dyspnea * | ||
|---|---|---|---|
| No LVH ** | LVH ** | p | |
| Using ECHO | |||
| Low risk | 44 (14.9) | 6 (37.5) | 0.028 |
| Moderate risk | 30 (28.6) | 4 (33.3) | 0.743 |
| High risk | 14 (19.4) | 2 (11.8) | 0.727 |
| Using Sokolow–Lyon Index | |||
| Low risk | 49 (16.3) | 1 (4.8) | 0.219 |
| Moderate risk | 34 (28.3) | 1 (50) | 0.493 |
| High risk | 16 (17.4) | 1 (33.3) | 0.450 |
| Using Cornel Index | |||
| Low risk | 48 (15.3) | 2 (25.0) | 0.361 |
| Moderate risk | 35 (29.2) | 0 (0.0) | 1.000 |
| High risk | 17 (18.1) | 0 (0.0) | 1.000 |
| Using Lewis Index | |||
| Low risk | 48 (15.2) | 2 (40.0) | 0.174 |
| Moderate risk | 34 (29.6) | 1 (14.3) | 0.672 |
| High risk | 17 (19.1) | 0 (0.0) | 0.587 |
| No LVH * | LVH * | p | ||
|---|---|---|---|---|
| Low CV Risk | ||||
| Last visit to a doctor or for a diagnostic procedure | during the last month | 113 (35.6) | 12 (70.6) | 0.014 |
| during the last year | 164 (51.7) | 5 (29.4) | ||
| over a year ago or at all | 40 (12.6) | 0 (0.0) | ||
| Moderate CV Risk | ||||
| Last visit to a doctor or for a diagnostic procedure | during the last month | 55 (44.4) | 3 (20.0) | 0.001 |
| during the last year | 59 (47.6) | 5 (33.3) | ||
| over a year ago or at all | 10 (8.1) | 7 (46.7) | ||
| High CV Risk | ||||
| Last visit to a doctor or for a diagnostic procedure | during the last month | 39 (48.8) | 9 (45.0) | 0.936 |
| during the last year | 34 (42.5) | 9 (45.0) | ||
| over a year ago or at all | 7 (8.8) | 2 (10.0) | ||
| Very High CV Risk | ||||
| Last visit to a doctor or for a diagnostic procedure | during the last month | 25 (49.0) | 7 (63.6) | 0.603 |
| during the last year | 22 (43.1) | 3 (27.3) | ||
| over a year ago or at all | 4 (7.8) | 1 (9.1) | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chlabicz, M.; Jamiołkowski, J.; Paniczko, M.; Sowa, P.; Szpakowicz, M.; Łapińska, M.; Jurczuk, N.; Kondraciuk, M.; Ptaszyńska-Kopczyńska, K.; Raczkowski, A.; et al. ECG Indices Poorly Predict Left Ventricular Hypertrophy and Are Applicable Only in Individuals with Low Cardiovascular Risk. J. Clin. Med. 2020, 9, 1364. https://doi.org/10.3390/jcm9051364
Chlabicz M, Jamiołkowski J, Paniczko M, Sowa P, Szpakowicz M, Łapińska M, Jurczuk N, Kondraciuk M, Ptaszyńska-Kopczyńska K, Raczkowski A, et al. ECG Indices Poorly Predict Left Ventricular Hypertrophy and Are Applicable Only in Individuals with Low Cardiovascular Risk. Journal of Clinical Medicine. 2020; 9(5):1364. https://doi.org/10.3390/jcm9051364
Chicago/Turabian StyleChlabicz, Małgorzata, Jacek Jamiołkowski, Marlena Paniczko, Paweł Sowa, Małgorzata Szpakowicz, Magda Łapińska, Natalia Jurczuk, Marcin Kondraciuk, Katarzyna Ptaszyńska-Kopczyńska, Andrzej Raczkowski, and et al. 2020. "ECG Indices Poorly Predict Left Ventricular Hypertrophy and Are Applicable Only in Individuals with Low Cardiovascular Risk" Journal of Clinical Medicine 9, no. 5: 1364. https://doi.org/10.3390/jcm9051364
APA StyleChlabicz, M., Jamiołkowski, J., Paniczko, M., Sowa, P., Szpakowicz, M., Łapińska, M., Jurczuk, N., Kondraciuk, M., Ptaszyńska-Kopczyńska, K., Raczkowski, A., Szpakowicz, A., & Kamiński, K. A. (2020). ECG Indices Poorly Predict Left Ventricular Hypertrophy and Are Applicable Only in Individuals with Low Cardiovascular Risk. Journal of Clinical Medicine, 9(5), 1364. https://doi.org/10.3390/jcm9051364






