The Effect of Probiotics on Symptoms, Gut Microbiota and Inflammatory Markers in Infantile Colic: A Systematic Review, Meta-Analysis and Meta-Regression of Randomized Controlled Trials
Abstract
1. Introduction
2. Methods
2.1. Search Strategy and Inclusion Criteria
2.2. Data Abstraction and Outcomes
2.3. Data Synthesis and Statistical Analyses
3. Results
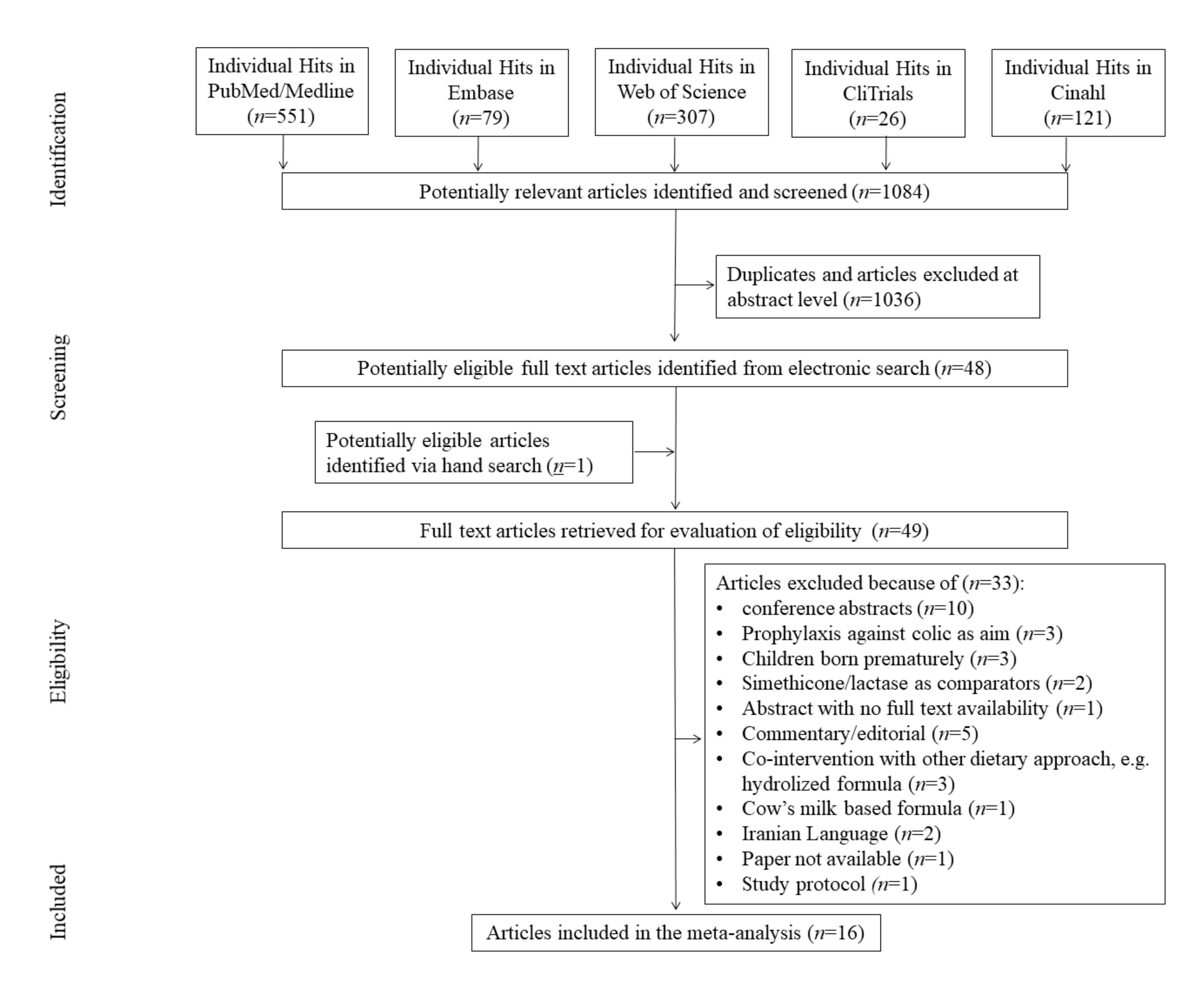
3.1. Search Results
3.2. Study, Patient, and Treatment Characteristics
3.3. Risk of Bias (ROB)
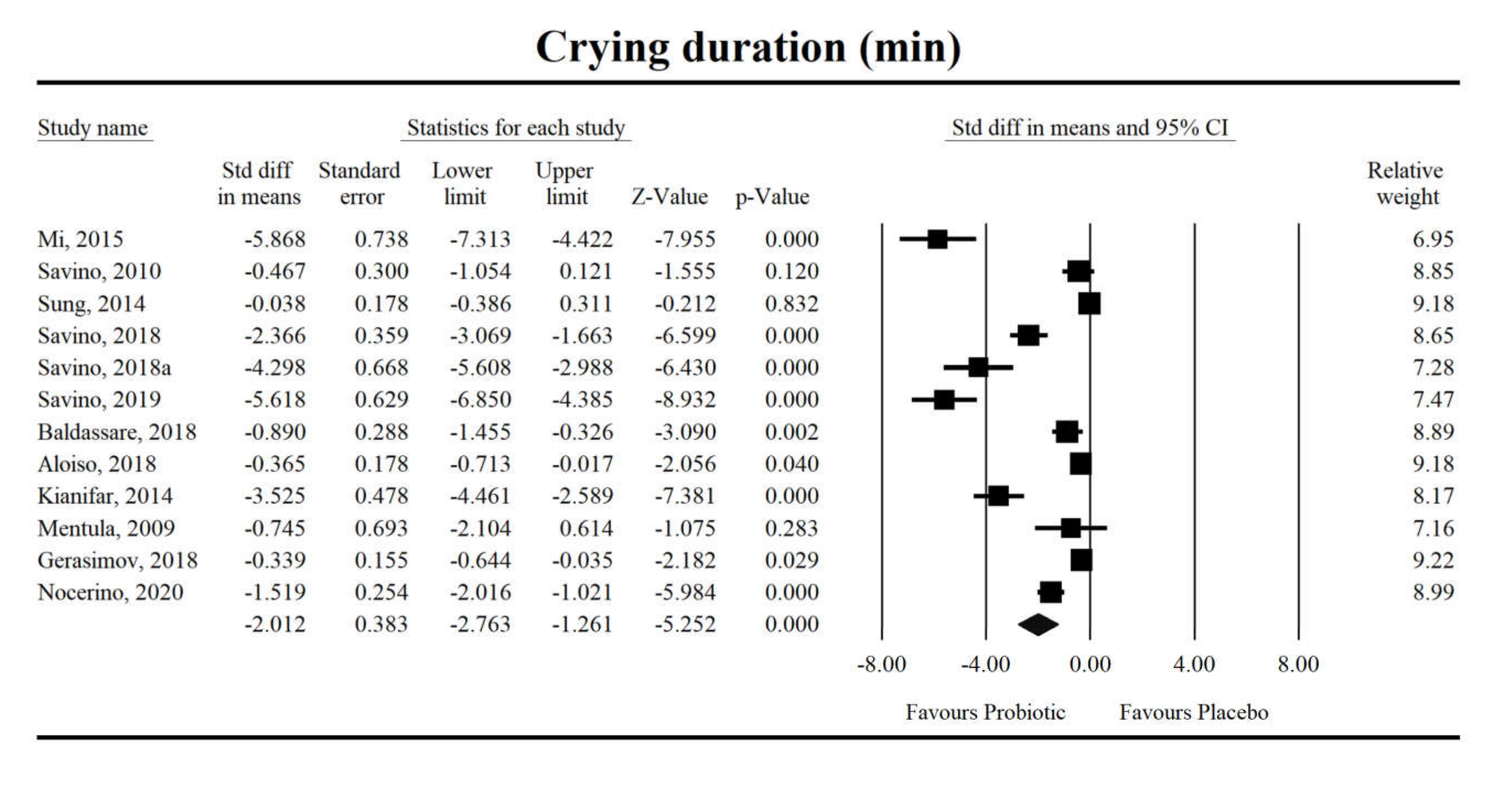
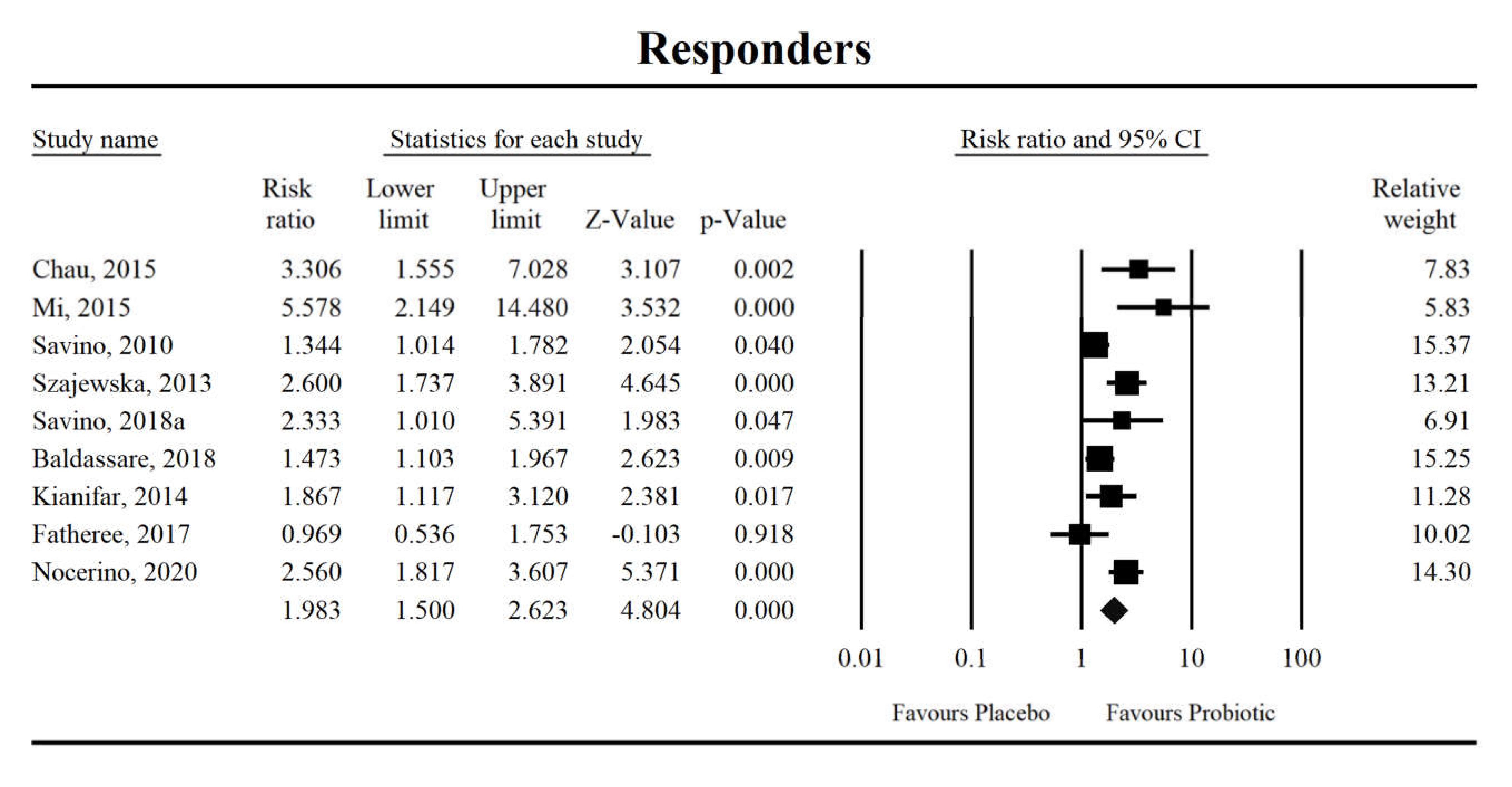
3.4. Effects on Crying Duration and Response to Probiotic Intervention
3.5. Microbiota and Immunological Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Wessel, M.A.; Cobb, J.C.; Jackson, E.B.; Harris, G.S.; Detwiler, A.C. Paroxysmal fussing in infancy, sometimes called colic. Pediatrics 1954, 14, 421–435. [Google Scholar] [PubMed]
- Drossman, D.A.; Hasler, W.L. Rome IV-Functional GI Disorders: Disorders of Gut-Brain Interaction. Gastroenterology 2016, 150, 1257–1261. [Google Scholar] [CrossRef] [PubMed]
- Benninga, M.A.; Faure, C.; Hyman, P.E.; St James Roberts, I.; Schechter, N.L.; Nurko, S. Childhood Functional Gastrointestinal Disorders: Neonate/Toddler. Gastroenterology 2016, 130, 1519–1526. [Google Scholar] [CrossRef]
- Vandenplas, Y.; Abkari, A.; Bellaiche, M.; Benninga, M.; Chouraqui, J.P.; Çokura, F.; Harb, T.; Hegar, B.; Lifschitz, C.; Ludwig, T.; et al. Prevalence and Health Outcomes of Functional Gastrointestinal Symptoms in Infants From Birth to 12 Months of Age. J. Pediatr. Gastroenterol. Nutr. 2015, 61, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Palsson, O.S.; Whitehead, W.E.; van Tilburg, M.A.L.; Chang, L.; Chey, W.; Crowell, M.D.; Keefer, L.; Lembo, A.J.; Parkman, H.P.; Rao, S.S.; et al. Rome IV Diagnostic Questionnaires and Tables for Investigators and Clinicians. Gastroenterology 2016, 150, 1481–1491. [Google Scholar] [CrossRef] [PubMed]
- Rautava, P.; Helenius, H.; Lehtonen, L. Psychosocial predisposing factors for infantile colic. BMJ 1993, 307, 600–604. [Google Scholar] [CrossRef][Green Version]
- St James-Roberts, I.; Halil, T. Infant crying patterns in the first year: Normal community and clinical findings. J. Child Psychol. Psychiatry 1991, 32, 951–968. [Google Scholar] [CrossRef]
- Zeevenhooven, J.; Koppen, I.J.N.; Benninga, M.A. The New Rome IV Criteria for Functional Gastrointestinal Disorders in Infants and Toddlers. Pediatr. Gastroenterol. Hepatol. Nutr. 2017, 20, 1–13. [Google Scholar] [CrossRef]
- Daelemans, S.; Peeters, L.; Hauser, B.; Vandenplas, Y. Recent advances in understanding and managing infantile colic. F1000Research 2018, 7. [Google Scholar] [CrossRef]
- Sarasu, J.M.; Narang, M.; Shah, D. Infantile Colic: An Update. Indian Pediatr. 2018, 55, 979–987. [Google Scholar] [CrossRef]
- Douglas, P.; Hill, P. Managing infants who cry excessively in the first few months of life. BMJ 2011, 343, d7772. [Google Scholar] [CrossRef] [PubMed]
- Talge, N.M.; Neal, C.; Glover, V. Early Stress, Translational Research and Prevention Science Network: Fetal and Neonatal Experience on Child and Adolescent Mental Health Antenatal maternal stress and long-term effects on child neurodevelopment: How and why? J. Child Psychol. Psychiatry 2007, 48, 245–261. [Google Scholar] [CrossRef]
- Van den Berg, M.P.; van der Ende, J.; Crijnen, A.A.M.; Jaddoe, V.W.V.; Moll, H.A.; Mackenbach, J.P.; Hofman, A.; Hengeveld, M.W.; Tiemeier, H.; Verhulst, F.C. Paternal depressive symptoms during pregnancy are related to excessive infant crying. Pediatrics 2009, 124, e96–e103. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.K. Is colic a gastrointestinal disorder? Curr. Opin. Pediatr. 2002, 14, 588–592. [Google Scholar] [CrossRef] [PubMed]
- De Weerth, C.; Fuentes, S.; Puylaert, P.; de Vos, W.M. Intestinal microbiota of infants with colic: Development and specific signatures. Pediatrics 2013, 131, e550–e558. [Google Scholar] [CrossRef] [PubMed]
- Rhoads, J.M.; Fatheree, N.Y.; Norori, J.; Liu, Y.; Lucke, J.F.; Tyson, J.E.; Ferris, M.J. Altered fecal microflora and increased fecal calprotectin in infants with colic. J. Pediatr. 2009, 155, 823–828. [Google Scholar] [CrossRef]
- Rhoads, J.M.; Collins, J.; Fatheree, N.Y.; Hashmi, S.S.; Taylor, C.M.; Luo, M.; Hoang, T.K.; Gleason, W.A.; Van Arsdall, M.R.; Navarro, F.; et al. Infant Colic Represents Gut Inflammation and Dysbiosis. J. Pediatr. 2018, 203, 55–61. [Google Scholar] [CrossRef]
- Savino, F.; Cordisco, L.; Tarasco, V.; Calabrese, R.; Palumeri, E.; Matteuzzi, D. Molecular identification of coliform bacteria from colicky breastfed infants. Acta Paediatr. 2009, 98, 1582–1588. [Google Scholar] [CrossRef]
- Savino, F.; Garro, M.; Montanari, P.; Galliano, I.; Bergallo, M. Crying Time and RORγ/FOXP3 Expression in Lactobacillus reuteri DSM17938-Treated Infants with Colic: A Randomized Trial. J. Pediatr. 2018, 192, 171–177. [Google Scholar] [CrossRef]
- Savino, F.; Cresi, F.; Pautasso, S.; Palumeri, E.; Tullio, V.; Roana, J.; Silvestro, L.; Oggero, R. Intestinal microflora in breastfed colicky and non-colicky infants. Acta Paediatr. 2004, 93, 825–829. [Google Scholar] [CrossRef]
- Eutamène, H.; Garcia-Rodenas, C.L.; Yvon, S.; d’Aldebert, E.; Foata, F.; Berger, B.; Sauser, J.; Theodorou, V.; Bergonzelli, G.; Mas, E. Luminal contents from the gut of colicky infants induce visceral hypersensitivity in mice. Neurogastroenterol. Motil. 2017, 29. [Google Scholar] [CrossRef] [PubMed]
- Salvatore, S.; Barberi, S.; Borrelli, O.; Castellazzi, A.; Di Mauro, D.; Di Mauro, G.; Doria, M.; Francavilla, R.; Landi, M.; Martelli, A.; et al. Pharmacological interventions on early functional gastrointestinal disorders. Ital. J. Pediatr. 2016, 42, 68. [Google Scholar] [CrossRef] [PubMed]
- Illingworth, R.S. Evening Colic in Infants: A Double-Blind Trial of Dicyclomine Hydrochloride. The Lancet 1959, 274, 1119–1120. [Google Scholar] [CrossRef]
- Blomquist, H.K.; Mjörndal, T.; Tiger, G. Dicycloverin chloride solution—A remedy for severe infantile colic. Lakartidningen 1983, 80, 116–118. [Google Scholar] [PubMed]
- Oggero, R.; Garbo, G.; Savino, F.; Mostert, M. Dietary modifications versus dicyclomine hydrochloride in the treatment of severe infantile colics. Acta Paediatr. 1994, 83, 222–225. [Google Scholar] [CrossRef]
- Goldman, M.H. Dicycloverine for persistent crying in babies: Dicycloverine is contraindicated in infants. BMJ 2004, 328, 956. [Google Scholar] [CrossRef]
- Shamir, R.; St James-Roberts, I.; Di Lorenzo, C.; Burns, A.J.; Thapar, N.; Indrio, F.; Riezzo, G.; Raimondi, F.; Di Mauro, A.; Francavilla, R.; et al. Infant crying, colic, and gastrointestinal discomfort in early childhood: A review of the evidence and most plausible mechanisms. J. Pediatr. Gastroenterol. Nutr. 2013, 57 (Suppl. 1), S1–S45. [Google Scholar] [CrossRef]
- Bruyas-Bertholon, V.; Lachaux, A.; Dubois, J.-P.; Fourneret, P.; Letrilliart, L. Which treatments for infantile colics? La Presse Médicale 2012, 41, e404–e410. [Google Scholar] [CrossRef]
- Danielsson, B.; Hwang, C.P. Treatment of infantile colic with surface active substance (simethicone). Acta Paediatr. Scand. 1985, 74, 446–450. [Google Scholar] [CrossRef]
- Metcalf, T.J.; Irons, T.G.; Sher, L.D.; Young, P.C. Simethicone in the treatment of infant colic: A randomized, placebo-controlled, multicenter trial. Pediatrics 1994, 94, 29–34. [Google Scholar]
- Savino, F.; Brondello, C.; Cresi, F.; Oggero, R.; Silvestro, L. Cimetropium bromide in the treatment of crisis in infantile colic. J. Pediatr. Gastroenterol. Nutr. 2002, 34, 417–419. [Google Scholar] [CrossRef] [PubMed]
- Gieruszczak-Białek, D.; Konarska, Z.; Skórka, A.; Vandenplas, Y.; Szajewska, H. No effect of proton pump inhibitors on crying and irritability in infants: Systematic review of randomized controlled trials. J. Pediatr. 2015, 166, 767–770. [Google Scholar] [CrossRef] [PubMed]
- Savino, F.; Galliano, I.; Savino, A.; Daprà, V.; Montanari, P.; Calvi, C.; Bergallo, M. Lactobacillus reuteri DSM 17938 Probiotics May Increase CC-Chemokine Receptor 7 Expression in Infants Treated with for Colic. Front. Pediatr. 2019, 7, 292. [Google Scholar] [CrossRef] [PubMed]
- Szajewska, H.; Gyrczuk, E.; Horvath, A. Lactobacillus reuteri DSM 17938 for the Management of Infantile Colic in Breastfed Infants: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Pediatr. 2013, 162, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Sung, V.; Hiscock, H.; Tang, M.L.K.; Mensah, F.K.; Nation, M.L.; Satzke, C.; Heine, R.G.; Stock, A.; Barr, R.G.; Wake, M. Treating infant colic with the probiotic Lactobacillus reuteri: Double blind, placebo controlled randomised trial. BMJ 2014, 348, g2107. [Google Scholar] [CrossRef] [PubMed]
- Indrio, F.; Mauro, A.D.; Riezzo, G.; Civardi, E.; Intini, C.; Corvaglia, L.; Ballardini, E.; Bisceglia, M.; Cinquetti, M.; Brazzoduro, E.; et al. Prophylactic Use of a Probiotic in the Prevention of Colic, Regurgitation, and Functional Constipation: A Randomized Clinical Trial. JAMA Pediatr. 2014, 168, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Sung, V.; D’Amico, F.; Cabana, M.D.; Chau, K.; Koren, G.; Savino, F.; Szajewska, H.; Deshpande, G.; Dupont, C.; Indrio, F.; et al. Lactobacillus reuteri to Treat Infant Colic: A Meta-analysis. Pediatrics 2018, 141, e20171811. [Google Scholar] [CrossRef]
- Ong, T.G.; Gordon, M.; Banks, S.S.; Thomas, M.R.; Akobeng, A.K. Probiotics to prevent infantile colic. Cochrane Database Syst. Rev. 2019. [Google Scholar] [CrossRef]
- Schreck Bird, A.; Gregory, P.J.; J alloh, M.A.; Risoldi Cochrane, Z.; Hein, D.J. Probiotics for the Treatment of Infantile Colic: A Systematic Review. J. Pharm. Pract. 2017, 30, 366–374. [Google Scholar] [CrossRef]
- Skonieczna-Żydecka, K.; Kaczmarczyk, M.; Łoniewski, I.; Lara, L.F.; Koulaouzidis, A.; Misera, A.; Maciejewska, D.; Marlicz, W. A Systematic Review, Meta-Analysis, and Meta-Regression Evaluating the Efficacy and Mechanisms of Action of Probiotics and Synbiotics in the Prevention of Surgical Site Infections and Surgery-Related Complications. J. Clin. Med. 2018, 7, E556. [Google Scholar] [CrossRef]
- Marlicz, W.; Skonieczna-Żydecka, K.; Yung, D.E.; Loniewski, I.; Koulaouzidis, A. Endoscopic findings and colonic perforation in microscopic colitis: A systematic review. Dig. Liver Dis. 2017, 49, 1073–1085. [Google Scholar] [CrossRef] [PubMed]
- Skonieczna-Żydecka, K.; Łoniewski, I.; Misera, A.; Stachowska, E.; Maciejewska, D.; Marlicz, W.; Galling, B. Second-generation antipsychotics and metabolism alterations: A systematic review of the role of the gut microbiome. Psychopharmacology 2018, 236, 1491–1512. [Google Scholar]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Aloisio, I.; Prodam, F.; Giglione, E.; Bozzi Cionci, N.; Solito, A.; Bellone, S.; Baffoni, L.; Mogna, L.; Pane, M.; Bona, G.; et al. Three-Month Feeding Integration with Bifidobacterium Strains Prevents Gastrointestinal Symptoms in Healthy Newborns. Front. Nutr. 2018, 5, 39. [Google Scholar] [CrossRef]
- Baldassarre, M.E.; Di Mauro, A.; Tafuri, S.; Rizzo, V.; Gallone, M.S.; Mastromarino, P.; Capobianco, D.; Laghi, L.; Zhu, C.; Capozza, M.; et al. Effectiveness and Safety of a Probiotic-Mixture for the Treatment of Infantile Colic: A Double-Blind, Randomized, Placebo-Controlled Clinical Trial with Fecal Real-Time PCR and NMR-Based Metabolomics Analysis. Nutrients 2018, 10, 195. [Google Scholar] [CrossRef]
- Chau, K.; Lau, E.; Greenberg, S.; Jacobson, S.; Yazdani-Brojeni, P.; Verma, N.; Koren, G. Probiotics for infantile colic: A randomized, double-blind, placebo-controlled trial investigating Lactobacillus reuteri DSM 17938. J. Pediatr. 2015, 166, 74–78. [Google Scholar] [CrossRef]
- Mentula, S.; Tuure, T.; Koskenala, R.; Korpela, R.; Könönen, E. Microbial composition and fecal fermentation end products from colicky infants—A probiotic supplementation pilot. Microb. Ecol. Health Dis. 2008, 20, 37–47. [Google Scholar]
- Savino, F.; Cordisco, L.; Tarasco, V.; Palumeri, E.; Calabrese, R.; Oggero, R.; Roos, S.; Matteuzzi, D. Lactobacillus reuteri DSM 17938 in Infantile Colic: A Randomized, Double-Blind, Placebo-Controlled Trial. Pediatrics 2010, 126, e526–e533. [Google Scholar] [CrossRef]
- Savino, F.; Galliano, I.; Garro, M.; Savino, A.; Daprà, V.; Montanari, P.; Bergallo, M. Regulatory T cells and Toll-like receptor 2 and 4 mRNA expression in infants with colic treated with Lactobacillus reuteri DSM17938. Benef. Microbes 2018, 9, 917–925. [Google Scholar] [CrossRef]
- Kianifar, H.; Ahanchian, H.; Grover, Z.; Jafari, S.; Noorbakhsh, Z.; Khakshour, A.; Sedaghat, M.; Kiani, M. Synbiotic in the management of infantile colic: A randomised controlled trial. J Paediatr. Child Health 2014, 50, 801–805. [Google Scholar] [CrossRef] [PubMed]
- Fatheree, N.Y.; Liu, Y.; Taylor, C.M.; Hoang, T.K.; Cai, C.; Rahbar, M.H.; Hessabi, M.; Ferris, M.; McMurtry, V.; Wong, C.; et al. Lactobacillus reuteri for Infants with Colic: A Double-Blind, Placebo-Controlled, Randomized Clinical Trial. J. Pediatr. 2017, 191, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Mi, G.-L.; Zhao, L.; Qiao, D.-D.; Kang, W.-Q.; Tang, M.-Q.; Xu, J.-K. Effectiveness of Lactobacillus reuteri in infantile colic and colicky induced maternal depression: A prospective single blind randomized trial. Antonie Van Leeuwenhoek 2015, 107, 1547–1553. [Google Scholar] [CrossRef] [PubMed]
- Nocerino, R.; De Filippis, F.; Cecere, G.; Marino, A.; Micillo, M.; Di Scala, C.; de Caro, C.; Calignano, A.; Bruno, C.; Paparo, L.; et al. The therapeutic efficacy of Bifidobacterium animalis subsp. lactis BB-12® in infant colic: A randomised, double blind, placebo-controlled trial. Aliment. Pharmacol. Ther. 2020, 51, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Gerasimov, S.; Gantzel, J.; Dementieva, N.; Schevchenko, O.; Tsitsura, O.; Guta, N.; Bobyk, V.; Kaprus, V. Role of Lactobacillus rhamnosus (FloraActiveTM) 19070-2 and Lactobacillus reuteri (FloraActiveTM) 12246 in Infant Colic: A Randomized Dietary Study. Nutrients 2018, 10, 1975. [Google Scholar] [CrossRef]
- Nation, M.L.; Dunne, E.M.; Joseph, S.J.; Mensah, F.K.; Sung, V.; Satzke, C.; Tang, M.L.K. Impact of Lactobacillus reuteri colonization on gut microbiota, inflammation, and crying time in infant colic. Sci. Rep. 2017, 7, 1–8. [Google Scholar] [CrossRef]
- Peura, S.; Fall, T.; Almqvist, C.; Andolf, E.; Hedman, A.; Pershagen, G.; Helmersson-Karlqvist, J.; Larsson, A. Normal values for calprotectin in stool samples of infants from the population-based longitudinal born into life study. Scand. J. Clin. Lab. Invest. 2018, 78, 120–124. [Google Scholar] [CrossRef]
- Albanna, E.A.; Ahmed, H.S.; Awad, H.A. Stool calprotectin in necrotizing enterocolitis. J. Clin. Neonatol. 2014, 3, 16. [Google Scholar]
- Ahmed, M.; Billoo, A.G.; Iqbal, K.; Memon, A. Clinical Efficacy of Lactase Enzyme Supplement In Infant Colic: A Randomised Controlled Trial. J. Pak. Med. Assoc. 2018, 68, 1744–1747. [Google Scholar]
- Biagioli, E.; Tarasco, V.; Lingua, C.; Moja, L.; Savino, F. Pain-relieving agents for infantile colic. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef]
- Kanabar, D.; Randhawa, M.; Clayton, P. Improvement of symptoms in infant colic following reduction of lactose load with lactase. J. Hum. Nutr. Diet. 2001, 14, 359–363. [Google Scholar] [CrossRef] [PubMed]
- Martinelli, M.; Ummarino, D.; Giugliano, F.P.; Sciorio, E.; Tortora, C.; Bruzzese, D.; De Giovanni, D.; Rutigliano, I.; Valenti, S.; Romano, C.; et al. Efficacy of a standardized extract of Matricariae chamomilla L., Melissa officinalis L. and tyndallized Lactobacillus acidophilus (HA122) in infantile colic: An open randomized controlled trial. Neurogastroenterol. Motil. 2017, 29, e13145. [Google Scholar] [CrossRef] [PubMed]
- Savino, F.; Pelle, E.; Palumeri, E.; Oggero, R.; Miniero, R. Lactobacillus reuteri (American Type Culture Collection Strain 55730) Versus Simethicone in the Treatment of Infantile Colic: A Prospective Randomized Study. Pediatrics 2007, 119, e124–e130. [Google Scholar] [CrossRef] [PubMed]
- Stahlberg, M.R. Infantile colic: Occurrence and risk factors. Eur. J. Pediatr. 1984, 143, 108–111. [Google Scholar] [CrossRef]
- Camilleri, M.; Park, S.-Y.; Scarpato, E.; Staiano, A. Exploring Hypotheses and Rationale for Causes of Infantile Colic. Neurogastroenterol. Motil. 2017, 29, e12943. [Google Scholar] [CrossRef]
- Kusaka, R.; Ohgi, S.; Shigemori, K.; Fujimoto, T. Crying and Behavioral Characteristics in Premature Infants. J. Jpn. Phys. Ther. Assoc. 2008, 11, 15–21. [Google Scholar] [CrossRef]
- Sung, V.; Collett, S.; de Gooyer, T.; Hiscock, H.; Tang, M.; Wake, M. Probiotics to prevent or treat excessive infant crying: Systematic review and meta-analysis. JAMA Pediatr. 2013, 167, 1150–1157. [Google Scholar] [CrossRef]
- Dryl, R.; Szajewska, H. Probiotics for management of infantile colic: A systematic review of randomized controlled trials. Arch. Med. Sci. 2018, 14, 1137–1143. [Google Scholar] [CrossRef]
- Pannaraj, P.S.; Li, F.; Cerini, C.; Bender, J.M.; Yang, S.; Rollie, A.; Adisetiyo, H.; Zabih, S.; Lincez, P.J.; Bittinger, K.; et al. Association Between Breast Milk Bacterial Communities and Establishment and Development of the Infant Gut Microbiome. JAMA Pediatr. 2017, 171, 647–654. [Google Scholar] [CrossRef]
- Moossavi, S.; Sepehri, S.; Robertson, B.; Bode, L.; Goruk, S.; Field, C.J.; Lix, L.M.; de Souza, R.J.; Becker, A.B.; Mandhane, P.J.; et al. Composition and Variation of the Human Milk Microbiota Are Influenced by Maternal and Early-Life Factors. Cell Host Microbe 2019, 25, 324–335. [Google Scholar] [CrossRef]
- Dominguez-Bello, M.G.; Godoy-Vitorino, F.; Knight, R.; Blaser, M.J. Role of the microbiome in human development. Gut 2019, 68, 1108–1114. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.W.; Greer, F.R. American Academy of Pediatrics Committee on Nutrition; American Academy of Pediatrics Section on Gastroenterology, Hepatology, and Nutrition Probiotics and prebiotics in pediatrics. Pediatrics 2010, 126, 1217–1231. [Google Scholar] [CrossRef] [PubMed]
- Savino, F.; Ceratto, S.; Opramolla, A.; Locatelli, E.; Tarasco, V.; Amaretti, A. Coliforms and infant colic: Fish analysis of fecal samples of breastfed and formula fed infants. J. Pediatr. Gastroenterol. Nutr. 2013, 56, 472. [Google Scholar]
- Hermansson, H.; Kumar, H.; Collado, M.C.; Salminen, S.; Isolauri, E.; Rautava, S. Breast Milk Microbiota Is Shaped by Mode of Delivery and Intrapartum Antibiotic Exposure. Front. Nutr. 2019, 6, 4. [Google Scholar] [CrossRef] [PubMed]
- Łoniewska, B.; Węgrzyn, D.; Adamek, K.; Kaczmarczyk, M.; Skonieczna-Żydecka, K.; Adler, G.; Jankowska, A.; Uzar, I.; Kordek, A.; Celewicz, M.; et al. The Influence of Maternal-Foetal Parameters on Concentrations of Zonulin and Calprotectin in the Blood and Stool of Healthy Newborns during the First Seven Days of Life. An Observational Prospective Cohort Study. J. Clin. Med. 2019, 8, 473. [Google Scholar] [CrossRef]
- McCreedy, A.; Bird, S.; Brown, L.J.; Shaw-Stewart, J.; Chen, Y.-F. Effects of maternal caffeine consumption on the breastfed child: A systematic review. Swiss Med. Wkly. 2018, 148, w14665. [Google Scholar] [CrossRef]
- Shenassa, E.D.; Brown, M.-J. Maternal smoking and infantile gastrointestinal dysregulation: The case of colic. Pediatrics 2004, 114, e497–e505. [Google Scholar] [CrossRef]
- Milidou, I.; Henriksen, T.B.; Jensen, M.S.; Olsen, J.; Søndergaard, C. Nicotine replacement therapy during pregnancy and infantile colic in the offspring. Pediatrics 2012, 129, e652–e658. [Google Scholar] [CrossRef]
- Sjarif, D.R. Nutritional Intervention in Infantile Colic: Mini Review. IPCB 2017, 3, 266–272. [Google Scholar] [CrossRef]
- Bäckhed, F.; Roswall, J.; Peng, Y.; Feng, Q.; Jia, H.; Kovatcheva-Datchary, P.; Li, Y.; Xia, Y.; Xie, H.; Zhong, H.; et al. Dynamics and Stabilization of the Human Gut Microbiome during the First Year of Life. Cell Host Microbe 2015, 17, 690–703. [Google Scholar] [CrossRef]
- Lee, Y.M.; Min, C.-Y.; Choi, Y.J.; Jeong, S.J. Delivery and feeding mode affects fecal calprotectin levels in infants <7 months old. Early Hum. Dev. 2017, 108, 45–48. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Ma, J.; Geng, S.; Wang, J.; Liu, J.; Zhang, J.; Sheng, X. Fecal Calprotectin Concentrations in Healthy Children Aged 1–18 Months. PLoS ONE 2015, 10, e0119574. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Sutton, A.J.; Ioannidis, J.P.A.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef] [PubMed]


| Study (Country) | Study Description | Sample Description | Intervention | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Design, Blinding | ROB^ | n Randomized/ Analyzed | Duration (Days) | Study Focus | Age (Mean ± SD, Days) | Male (%) | Breast-fed (%) | Probiotic Name | Probiotic Dose | |
| Aloiso et al., 2018 [45] (Italy) | DB | 4 | 158/155 | 90 | efficacy against functional gastrointestinal disorders | 10.5 ± 2.15 | 52.26 | 83.87 | B. breve BR03 (DSM 16604) and B. breve B632 (DSM 24706) | drops containing 108 CFU of each strain |
| Baldassare et al., 2018 [46] (Italy) | DB | 7 | 62/53 | 21 | efficacy in infantile colic | 38.75 ± 1.72 | 58.49 | 100 | L. paracasei DSM 24733, L. plantarum DSM 24730, L. acidophilus DSM 24735, and L. delbrueckii subsp. bulgaricus DSM 24734), three strains of bifidobacteria (B. longum DSM 24736, B. breve DSM 24732, and B. longum ssp. infantis DSM 24737), and one strain of Streptococcus thermophilus DSM 24731 | 5 × 109 CFU/10 drops |
| Chau et al., 2015 [47] (Canada) | DB | 7 | 55/52 | 21 | efficacy in infantile colic | 39.73 ± 0.32 | 48.08 | 100 | L. reuteri DSM 17938 | 108 CFU in 5 drops/day |
| Fatheree et al., 2017 [52] (USA) | DB | 7 | 20/16 | 42 | efficacy against crying, fussing, inflammatory, immune, and microbiome variables | Probio: 57 (39. 72); PBO: 40 (34. 51) †† | 75 | 100 | L. reuteri DSM 17938 | 108/day |
| Gerasimov et al., 2018 [55] (Ukraine) | DB | 5 | 172/168 | 28 | efficacy against crying, fussing | 44.5 ± 15 | 50 | 100 | L. rhamnosus 19070-2, L. reuteri 12246 | 250 × 106 CFU + 3.33 mg FOS+200IU vitamin D3 |
| Kianifar et al., 2014 [51] (Australia) | DB | 7 | 50/45 | 30 | reduction of newborns crying over time | 42.17 ± 17.38 | 48.89 | 100 | L. casei, L. rhamnosus, Streptococcus thermophilus, B. breve, L. acidophilus, B. longum ssp. infantis, L. bulgaricus and FOS | 109 CFU/sachet |
| Mentula et al., 2008 [48] (Finland) | DB | 0 | 18.wrz | 14 | reduction of newborns crying over time and effect on gut microbiota | 21 ± nd | 33.33 | 100 | L. rhamnosus GG, L. rhamnosus LC705, B. longum ssp. infantis Bbi99, and Propionibacterium freudenreichii ssp. shermanii JS | L. rhamnosus GG:5 × 109 CFU; L. rhamnosus LC705: 5 × 109 CFU; B. breve Bbi99: 2 × 108 CFU; P. freudenreichii ssp. shermanii JS: 2 × 109 CFU |
| Mi et al., 2015 [53] (China) | SB | 5 | 42/39 | 28 | efficacy in infantile colic | 29.16 ± 15.59 | 56.41 | 87.18 | L. reuteri DSM 17938 | 108 CFU |
| Nation et al. 2017 [56] (Australia) | DB | 5 | 167/167 | 28 | The relationship between L. reuteri colonisation and crying time, microbial and inflammatory parameters *** | 50.18 ± 19.06 | 50.89 | 59.28 | L. reuteri DSM 17938 | 0.2 × 108 CFU/day |
| Nocerino et al., 2020 [54] (Italy) | DB | 7 | 80/78 | 28 | efficacy in infantile colic | 32.95 ± 5.15 | 55.12 | 100 | Bifidobacterium animalis subsp. lactis BB-12®, DSM 15954 | 109 CFU/day |
| Savino et al. 2010 [49] (Italy) | DB | 6 | 50/46 | 21 | efficacy in infantile colic and its relationship to the gut microbiota | PBO: 28.5 (21) Probio: 32.5 (21) † | 63.04 | 100 | L. reuteri DSM 17 938 | 108 CFU |
| Savino et al., 2018 [19] (Italy) | DB | 5 | 87/60 | 30 | reduction of newborns crying and modifying the RORg/FOXP3 expression, gut microbiota and faecal calprotectin | 47.06 ± 23.4 | 43.33 | 83.33 | L. reuteri DSM 17938 | 108 CFU/ drop; 5 drops/day |
| Savino et al., 2018a [50] (Italy) | DB | 5 | 59/30 | 28 | influence on Treg and TLR expression (TLR 2 and TLR4) | 26.4 ± 12.36 | 40 | 100 | L. reuteri DSM 17938 | 0.2 × 108 CFU/drop; 5 drops |
| Savino et al., 2019 [33] (Italy) | nd | 1 | 50/50 | 28 | influence on CC-chemokine receptor 7 (CCR7) and interleukin 10 (IL-10) | <50; PBO: 28.5 (21) Probio: 32.5 (21) † | 58 | 100 | L. reuteri DSM 17938 | 108 CFU/ drop; 5 drops/day |
| Sung et al., 2014 [35] (Multicenter) | DB | 5 | 167/167 | 28 | reduction of newborns crying and fussing | 50.18 ± 19.06 | 50.90 | 59.28 | L reuteri DSM 17938 | 0.2 × 108 CFU/drop; 5 drops/day |
| Szajewska et al., 2013 [34] (Poland) | DB | 7 | 82/80 | 21 | efficacy in infantile colic | 36.2 ± 12.25 | 60 | 86.25 | L. reuteri DSM 17938 | 108 CFU in 5 drops |
| Reference | Microbiota (Faeces)/Immunological Markers * | Method |
|---|---|---|
| Aloisio et al., 2018 [45] |
| qPCR |
| Baldassare et al., 2018 [46] |
| qPCR/H-NMR |
| Fatheree et al., 2017 [52] |
| NGS/flow cytometry/ELISA |
| Mentula et al., 2009 [48] |
| culture-dependent technique/GC |
| *** Nation et al., 2017 [56] |
| qPCR/T-RFLP/ELISA |
| Nocerino et al., 2020 [54] |
| high-throughput sequencing of 16S rRNA, ELISA, indirect enzyme immunoassays |
| Savino et al., 2010 [57] |
| culture-dependent techniques, enzymatic colorimetric test |
| Savino et al., 2018 [19] |
| qPCR, ELISA |
| Savino et al., 2018a [50] |
| real time PCR/Qpcr |
| Savino et al., 2019 [33] |
| qPCR |
| Sung et al., 2014 [58] |
| 16SrDNA amplification (T-RFLP) ELISA, qPCR |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skonieczna-Żydecka, K.; Janda, K.; Kaczmarczyk, M.; Marlicz, W.; Łoniewski, I.; Łoniewska, B. The Effect of Probiotics on Symptoms, Gut Microbiota and Inflammatory Markers in Infantile Colic: A Systematic Review, Meta-Analysis and Meta-Regression of Randomized Controlled Trials. J. Clin. Med. 2020, 9, 999. https://doi.org/10.3390/jcm9040999
Skonieczna-Żydecka K, Janda K, Kaczmarczyk M, Marlicz W, Łoniewski I, Łoniewska B. The Effect of Probiotics on Symptoms, Gut Microbiota and Inflammatory Markers in Infantile Colic: A Systematic Review, Meta-Analysis and Meta-Regression of Randomized Controlled Trials. Journal of Clinical Medicine. 2020; 9(4):999. https://doi.org/10.3390/jcm9040999
Chicago/Turabian StyleSkonieczna-Żydecka, Karolina, Katarzyna Janda, Mariusz Kaczmarczyk, Wojciech Marlicz, Igor Łoniewski, and Beata Łoniewska. 2020. "The Effect of Probiotics on Symptoms, Gut Microbiota and Inflammatory Markers in Infantile Colic: A Systematic Review, Meta-Analysis and Meta-Regression of Randomized Controlled Trials" Journal of Clinical Medicine 9, no. 4: 999. https://doi.org/10.3390/jcm9040999
APA StyleSkonieczna-Żydecka, K., Janda, K., Kaczmarczyk, M., Marlicz, W., Łoniewski, I., & Łoniewska, B. (2020). The Effect of Probiotics on Symptoms, Gut Microbiota and Inflammatory Markers in Infantile Colic: A Systematic Review, Meta-Analysis and Meta-Regression of Randomized Controlled Trials. Journal of Clinical Medicine, 9(4), 999. https://doi.org/10.3390/jcm9040999







