Implementing Supported Self-Management in Community-Based Stroke Care: A Secondary Analysis of Nurses’ Perspectives
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
2.2. Study Participants
2.3. Study Instruments (Focus Groups and Telephone Interviews)
2.4. Data Analysis
2.5. Secondary Analysis
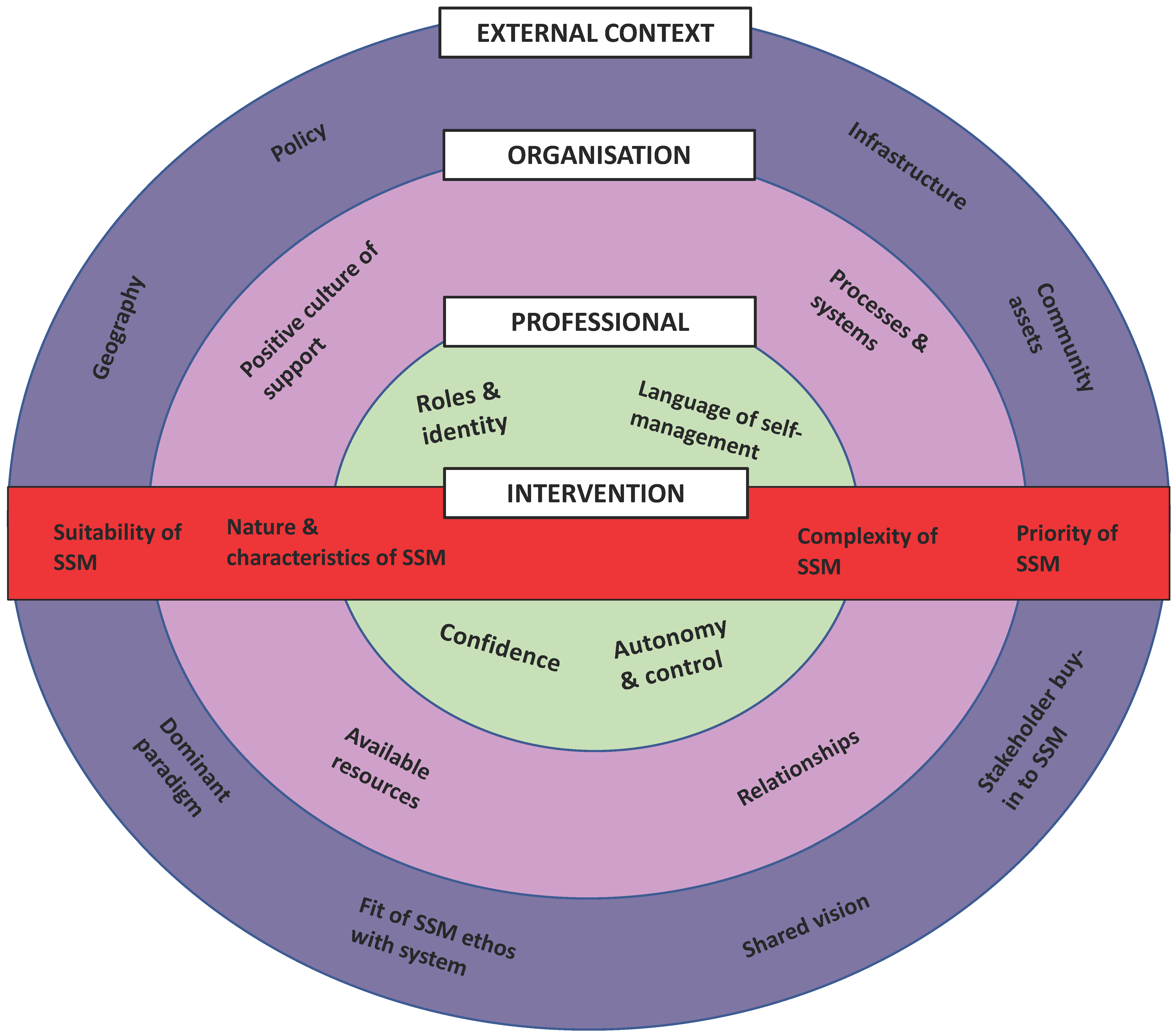
3. Results
3.1. External Context
“I don’t know enough about it (what the policy says) but I have been discussing it (SSM) with patients and referring patients and whatever and I’m sitting here thinking this is what we do anyway…I think we are kind of doing it you know?”(N2)
“It is my job…a chief part of my job is promoting self-management…and hoping that the end result would be that the patient would be able to self-manage at the end of our advice and support period.”(N5)
“I suppose for an inexperienced nurse (guidance on implementing SMS) would be useful but I think when you have been doing the job for as long as I have then it’s kind of natural you know, you wouldn’t really need a tool because you are able to know yourself with the experience that you have got. I wouldn’t feel that I needed (to use an assessment tool) because I just naturally ask things as anyway as part of my assessment.”(N6)
“There is obviously pressure to get people through the system in a quicker way and being able to self-manage. That arguably takes time to get folk to the stage so that doesn’t quite fit with the model of ‘getting in and getting out’ in a very short time and I think communication and therapeutic relationships are really important.”(N4)
“What hinders us is the lack of resources and services that are in (NHS Board name) and how remote our caseload is. You’ve got some people that live in (city) that have got access to services everywhere which is fantastic…then you’ve got patients fifty miles away that can’t access anything. Small villages and towns which don’t offer anything at all is a severe barrier (to implementing SMS).”(N6)
“It is confusing what’s out there though because every political boundary you cross over be it north, south, there will always be this bickering between them and you get better this and that but there’s so much out there that you really don’t know everything that is available and then maybe if a different government comes in they will change the boundaries again and they will change their names. You think you have this knowledge up here (pointing to head) and then you go back to get the telephone number and the contact that you had, and they have all changed.”(N7)
3.2. Organisation
“That’s one thing with this team, we are all quite happy. We’ve been doing the same job for a long time. I think there’s a lot of clinical support here so you can bounce ideas off people because it’s difficult at times. We phone each other up; any queries we would just ask each other.”(N10)
“It’s not consistent though…if you spoke to some other areas some stroke nurses do feel very isolated with a caseload and maybe even as part of a team. They’re having to cope with sometimes very challenging issues.”(N12)
“Our follow up is a year post discharge so I tell them what we would like to achieve by the end of that year and then I maybe see them five times in that year. It’s (SMS) relevant all the way through (SMS) but I don’t do much at the start. I would be seeing them again three months post discharge and I would say it is quite relevant then. It’s very difficult for when we come to discharge a patient, you will find that they will keep contacting you you know, and that’s not really what we are about. Basically, we are about self-management which means that they would need to be able to go and contact the resources and support services themselves. The end result of (my job) would be that the patient would be able to self-manage by the end of our advice and support period.”(N5)
“All the information that we’ve (given) about SSM, it’s really time consuming and everything that we tend to do…we’re on a timescale all day…and you’ve got so many visits, you need to try and get back for a clinic and I’m just constantly watching the time. We can easily be there half an hour, three quarters of an hour sometimes…but you can be there longer…and you come out and you still haven’t done everything that you need to do. I’m just thinking of the time that it takes to realistically do this with (SSM) with so many patients.”(N2)
“What we do ourselves is a lot you know so by the time we have gone over everything that we would like to offer after they have just had a stroke and then having to start talking to them about (self-management), then it’s going to affect our workload and the time that we have. It will impact on the length of visits in that we can’t fit as many people in. If it’s something we are going to have to facilitate, it’s going to have an impact on our time.”(N5)
3.3. Professionals
“We have guidelines that we want them to be able to achieve, given our experience and knowledge of stroke patients. We have an idea of what we want that patient to be able to do. We have to decide if they are being realistic you know or unrealistic, I suppose. Sometimes people think that they need things they don’t. Sometimes people are very unrealistic.”(N5)
“As nurses, we’ve not been used to patients self-managing, so we’ve probably put a lot of people in that role (of being dependent) because we have to make it better. We were programmed to step in there and do everything from the basics to washing, right up to dressings and things and to stand back, it’s difficult. They have to be able to do that (be independent) and we (nurses) have to let them go and let them be independent themselves”(N10)
“I think that stroke nurses perhaps have to recognize that you can’t fix everything. I would say when we started out in this role, we went out to fix it. It’s gradually changing but that’s the biggest problem and always was; you want to fix it.”(N12)
“We have to…decide if they (people) are being realistic you know, or are they being unrealistic I suppose. Sometimes people think that they need things they don’t.”(N5)
“You’ve got people that are motivated and want to do it (SSM) and you’ve got other people that don’t and that’s what they’ve been like prior to their stroke so they are not going to move on”(N10)
“People will try and test them out (self-management strategies). As long as it’s safe, sometimes you have to allow them to try that and you know, actually they will learn from it”(N4)
“We have had this one man that wanted to get back and ride a horse or a motorbike and his expectations were that he would be able to do that and give him his due, at the end of it he had an adapted quad bike and things. He raised the level far higher than any therapist would have through that he would have achieved because we err on the side of risk assessment.”(N10)
3.4. Intervention
“A lot of it is educating…educating the patient on what we would say are the risk factors so that they have knowledge of why they should be helping themselves to stop smoking, drink less and take more activity.”(N8)
“It (SSM) is about shared responsibility. I think sometimes what self-management is not is when people think it’s about getting on with it yourself and on you go. It’s very much about support and shared support. It’s about personal responsibility and being part of that and to a certain extent in control of the choices and options you make on your recovery.”(N11)
“If it’s the likes of smoking cessation, they will follow through if they are ready to do that, but I suppose that is a nice and neat intervention on a specific issue.”(N4)
“It depends on the patient because we are primarily over 65′s…a lot of them are widows or on their own and some don’t have families. I kind of think (I will be) softer and just do it for them sort of thing rather than encouraging them to (self-management) you know? We would probably just do it for them you know?”(N1)
“To try and keep a stroke patient’s concentration for long is very difficult because I find myself, after about thirty minutes, you have lost them because they can’t concentrate for any long period of time. And if you’ve got patients with communication problems, which there is quite a lot of, I think they’d be put off. Sometimes people are very unrealistic; the stroke has maybe damaged something that has made them think that they can do something, and they can’t. If it’s safe, then you will let them try and if it’s not safe then we need to come up with the information so they start understanding why they can’t do something.”(N5)
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- The Stroke Association. State of the Nation; Stroke Association: London, UK, 2018. [Google Scholar]
- Gallacher, K.I.; Batty, G.D.; McLean, G.; Mercer, S.W.; Guthrie, B.; May, C.R.; Langhorne, P.; Mair, F.S. Stroke, multimorbidity and polypharmacy in a nationally representative sample of 1,424,378 patients in Scotland: Implications for treatment burden. BMC Med. 2014, 12, 151. [Google Scholar] [CrossRef]
- Averbe, L.; Avis, S.; Chrichton, S.; Wolfe, C.D.; Rudd, A.G. The long-term outcomes of depression up to 10 years after stroke; the South London Stroke Register. J. Neurol. Neurosurg. Psychiatry 2014, 85, 514–521. [Google Scholar] [CrossRef] [PubMed]
- Pollock, A.; St George, B.; Fenton, M.; Firkins, L. Top 10 research priorities relating to life after stroke- consensus from stroke survivors, caregivers, and health professionals. Int. J. Stroke 2011, 9, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Rowat, A.; St George, B.; Cowey, E.; Booth, J.; Lawrence, M. Top ten research priorities relating to stroke nursing: A rigorous approach to establish a national nurse-led research agenda. J. Adv. Nurs. 2016, 72, 2831–2848. [Google Scholar] [CrossRef] [PubMed]
- Jones, F.; Riazi, A. Self-efficacy and self-management after stroke: A systematic review. Disabil. Rehabil. 2011, 33, 797–810. [Google Scholar] [CrossRef]
- Lennon, S.; McKenna, S.; Jones, F. Self-management programmes for people post stroke: A systematic review. Clin. Rehabil. 2013, 27, 867–878. [Google Scholar] [CrossRef]
- Warner, G.; Packer, T.; Villeneuve, M.; Audulv, A.; Versnel, J. A systematic review of the effectiveness of stroke self-management programs for improving function and participation outcomes: Self-management programs for stroke survivors. Disabil. Rehabil. 2015, 37, 2141–2163. [Google Scholar] [CrossRef]
- Fryer, C.E.; Luker, J.A.; McDonnell, M.N.; Hillier, S.L. Self-management programmes for quality of life in people with stroke. Cochrane Database Syst. Rev. 2016, 8, CD010442. [Google Scholar] [CrossRef]
- De Iongh, A.; Fagan, P.; Fenner, J.; Kidd, L. A Practical Guide to Self-Management Support; The Health Foundation: London, UK, 2015. [Google Scholar]
- Kidd, L.; Lawrence, M.; Booth, J.; Rowat, A.; Russell, S. Development and evaluation of a nurse-led, tailored stroke self-management intervention. BMC Health Serv. Res. 2015, 15, 359. [Google Scholar] [CrossRef]
- Rudd, A.G.; Bowen, A.; Young, G.; James, M.A. The latest national clinical guideline for stroke. Clin. Med. 2017, 17, 154–155. [Google Scholar] [CrossRef]
- Scottish Government. Scottish Stroke Improvement Plan; Scottish Government: Edinburgh, UK, 2014.
- Stroke Alliance for Europe. Burden of Stroke in Europe; Kings College: London, UK, 2018. [Google Scholar]
- Gallacher, K.; May, C.R.; Langhorne, P.; Mair, F. A Conceptual Model of Treatment Burden and Patient Capacity in Stroke. BMC Fam. Pract. 2018, 19, 9. [Google Scholar] [CrossRef] [PubMed]
- Demain, S.; Boger, E.; Latter, S.; Hankins, M.; Kennedy, A.; Foster, C.; Jones, F.; Kellar, I. What are the outcomes of self-management that matter to stakeholders? Study protocol for the Self-Management VOICED project. Work. Pap. Health Sci. 2014, 1, 7. Available online: https://www.southampton.ac.uk/assets/centresresearch/documents/wphs/EBWhat%20are%20the%20outcomes(2).pdf (accessed on 1 April 2020).
- Boger, E.; Ellis, J.; Latter, S.; Foster, C.; Kennedy, A.; Jones, F.; Fenerty, V.; Kellar, I.; Demain, S. Self-Management and Self-Management Support Outcomes: A Systematic Review and Mixed Research Synthesis of Stakeholder Views. PLoS ONE 2015, 10, e0130990. [Google Scholar] [CrossRef] [PubMed]
- Kulnik, S.; Poestges, H.; Brimicombe, L.; Hammond, J.; Jones, F. Implementing an interprofessional model of self-management support across a community workforce: A mixed-methods evaluation study. J. Interprof. Care 2017, 31, 75–84. [Google Scholar] [CrossRef]
- Jones, F.; Gage, H.; Drummond, A.; Bhalla, A.; Grant, R.; Lennon, S.; McKevitt, C.; Riazi, A.; Liston, M. Feasibility study of an integrated stroke self-management programme: A cluster-randomised controlled trial. BMJ Open 2016, 6, e008900. [Google Scholar] [CrossRef]
- Sadler, E.; Wolfe, C.D.A.; Jones, F.; McKevitt, C. Exploring stroke survivors’ and physiotherapists’ views of self-management after stroke: A qualitative study in the UK. BMJ Open 2017, 7, e011631. [Google Scholar] [CrossRef]
- Wray, F.; Clarke, D.; Foster, A. Post-stroke self-management interventions: A systematic review of effectiveness and investigation of the inclusion of stroke survivors with aphasia. Disabil. Rehabil. 2018, 40, 1237–1251. [Google Scholar] [CrossRef]
- Parke, H.L.; Epiphaniou, E.; Pearce, G.; Taylor, S.J.C.; Sheikh, A.; Griffiths, C.J. Self-Management Support Interventions for Stroke Survivors: A Systematic Meta-Review. PLoS ONE 2015, 10, e0131448. [Google Scholar] [CrossRef]
- Jones, F.; McKevitt, C.; Riazi, A.; Liston, M. How is rehabilitation with and without an integrated self-management approach perceived by UK community-dwelling stroke survivors? A qualitative process evaluation to explore implementation and contextual variations. BMJ Open 2017, 7, e014109. [Google Scholar] [CrossRef]
- Fletcher, S.; Kulnik, S.T.; Demain, S.; Jones, F. The problem with self-management: Problematizing self-management and power using a Foucauldian lens in the context of stroke care and rehabilitation. PLoS ONE 2019, 14, e0218517. [Google Scholar] [CrossRef]
- NHS National Services Scotland. Scottish Stroke Improvement Programme 2016 Report; ISD Scotland: Edinburgh, UK, 2016. [Google Scholar]
- Gallacher, K.; Morrison, D.; Jani, B.; Macdonald, S.; May, C.R.; Montori, V.M.; Erwin, P.J.; Batty, G.D.; Eton, D.T.; Langhorne, P.; et al. Uncovering Treatment Burden as a Key Concept for Stroke Care: A Systematic Review of Qualitative Research. PLoS Med. 2013, 10, e1001473. [Google Scholar] [CrossRef] [PubMed]
- Lau, R.; Stevenson, F.; Nio Ong, B.; Dziedzic, K.; Treweek, S.; Eldridge, S.; Everitt, H.; Kennedy, A.; Qureshi, N.; Rodgers, A.; et al. Achieving change in primary care—causes of the evidence to practice gap: Systematic review of reviews. Implement Sci. 2016, 11, 40. [Google Scholar] [CrossRef] [PubMed]
- Scholl, I.; LaRussa, A.; Hahlweg, P.; Kobrin, S.; Elwyn, G. Organizational- and system-level characteristics that influence implementation of shared decision-making and strategies to address them—A scoping review. Implement Sci. 2018, 13, 40. [Google Scholar] [CrossRef] [PubMed]
- Coles, E.; Wells, M.; Maxwell, M.; Harris, F.M.; Anderson, J.; Gray, N.M.; Milner, G.; MacGillivray, S. The influence of contextual factors on healthcare quality improvement initiatives: What works, for whom and in what setting? Protocol for a realist review. Syst. Rev. 2017, 6, 168. [Google Scholar] [CrossRef]
- Lewis, J.; McNaughton Nicholls, C. Design Issues. In Qualitative Research Practice: A Guide for Social Science Students and Researchers, 2nd ed.; Ritchie, J., Lewis, J., McNaughton Nicholls, C., Ormston, R., Eds.; Sage: London, UK, 2014; pp. 47–76. [Google Scholar]
- Hibbard, J.; Stockard, J.; Mahoney, E.R.; Tusler, M. Development of the Patient Activation Measure (PAM): Conceptualising and measuring activation in patients and consumers. Health Serv. Res. 2004, 39, 1005–1026. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psych. 2006, 3, 77–101. Available online: http://eprints.uwe.ac.uk/11735 (accessed on 1 April 2020). [CrossRef]
- Mudge, S.; Stretton, C.; Kayes, N. Are physiotherapists comfortable with person-centred practice? An autoethographic insight. Disabil. Rehabil. 2014, 36, 457–463. [Google Scholar] [CrossRef]
- Mudge, S.; Kayes, N.; McPherson, K. Who is in control? Clinician’s views on their role in self-management approaches: A qualitative metasynthesis. BMJ Open 2015, 5, e007413. [Google Scholar] [CrossRef]
- Morgan, H.M.; Entwistle, V.A.; Cribb, A.; Christmas, S.; Owens, J.; Skea, Z.C.; Watt, I.S. We need to talk about purpose: A critical interpretive synthesis of health and social care professionals’ approaches to self-management support for people with long-term conditions. Health Expect. 2017, 20, 243–259. [Google Scholar] [CrossRef]
- Morris, J.H.; Oliver, T.; Kroll, T.; Joice, S.; Williams, B. From physical and functional to continuity with pre-stroke self and participation in valued activities: A qualitative exploration of stroke survivors’, carers’ and physiotherapists’ perceptions of physical activity after stroke. Disabil. Rehabil. 2015, 37, 64–77. [Google Scholar] [CrossRef]
- Hughes, S.; Lewis, S.; Willis, K.; Rogers, A.; Wyke, S.; Smith, L. The experience of facilitators and participants of long-term condition self-management group programmes: A qualitative synthesis. Patent Educ. Couns. 2017, 100, 2244–2254. [Google Scholar] [CrossRef]
- Franklin, M.; Lewis, S.; Willis, K.; Rogers, A.; Venville, A.; Smith, L. Controlled, constrained or flexible? How self-management goals are shaped by patient-provider interactions. Qual. Health Res. 2018, 1. [Google Scholar] [CrossRef]
- Bossy, D.; Knutsen, I.; Rogers, A.; Foss, C. Moving between ideologies in self-management support–a qualitative study. Health Expect. 2019, 22, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Parker, J.; Mawson, S.; Mountain, G.; Nasr, N.; Davies, R.; Zheng, H. The provision of feedback through computer-based technology to promote self-managed post-stroke rehabilitation in the home. Disabil. Rehabil. Assist. Technol. 2014, 9, 529–538. [Google Scholar] [CrossRef] [PubMed]
- Paul, L.; Wyke, S.; Brewster, S.; Sattar, N.; Gill, J.R.; Alexander, G.; Rafferty, D.; McFadyen, A.K.; Ramsay, A.; Drybus, A.; et al. Increasing physical activity in stroke survivors using STARFISH, an interactive mobile phone application: A pilot study. Top. Stroke Rehabil. 2016, 23, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Paul, L.; Renfrew, L.; Freeman, J.; Murray, H.; Weller, B.; Mattison, P.; McConnachie, A.; Heggie, R.; Wu, O.; Coulter, H.; et al. Web-based physiotherapy for people affected by multiple sclerosis: A single blind, randomized controlled feasibility study. Clin. Rehabil. 2019, 33, 473–484. [Google Scholar] [CrossRef]
- Ortiz-Fernández, L.; Sagastagoya Zabala, J.; Gutiérrez-Ruiz, A.; Imaz-Ayo, N.; Alava-Menica, A.; Arana-Arri, E. Efficacy and Usability of eHealth Technologies in Stroke Survivors for Prevention of a New Stroke and Improvement of Self-Management: Phase III Randomized Control Trial. Methods Protoc. 2019, 13, 50. [Google Scholar] [CrossRef]
- Long-Sutehall, T.; Sque, M.; Addington-Hall, J. Secondary analysis of qualitative data: A valuable method for exploring sensitive issues with an elusive population? J. Res. Nurs. 2010, 16, 335–344. [Google Scholar] [CrossRef]
- Ploeg, J.; Wong, S.T.; Hassani, K.; Yous, M.L.; Fortin, M.; Kendall, C.; Liddy, C.; Markle Reid, M.; Petrovic, B.; Dionne, E.; et al. Contextual factors influencing the implementation of innovations in community-based primary health care: The experience of 12 Canadian research teams. Prim. Health Care Res. Dev. 2019, 20, 1–13. [Google Scholar] [CrossRef]
| Participant ID | Sex | Length of Time Qualified | Number of Years in Current Post | Highest Educational Qualification |
|---|---|---|---|---|
| N1 | Female | 11 years | 3 years | Bachelor’s Degree |
| N2 | Female | 25 years | 8 years | Diploma in Nursing |
| N3 | Male | 38 years | 13 years | Bachelor’s Degree |
| N4 | Female | 17 years | 2 years | Master’s Degree |
| N5 | Female | 16 years | 9 years | Bachelor’s Degree |
| N6 | Female | 12 years | 4 years | Bachelor’s Degree |
| N7 | Female | 21 years | 9 years | Bachelor’s Degree |
| N8 | Female | 28 years | <1 year | Diploma in Nursing |
| N9 | Female | 22 years | 6 years | Bachelor’s Degree |
| N10 | Female | 26 years | 10 years | Diploma in Nursing |
| N11 | Male | 25 years | 8 years | Master’s Degree |
| N12 | Female | 11 years | 5 years | Bachelor’s Degree |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kidd, L.; Booth, J.; Lawrence, M.; Rowat, A. Implementing Supported Self-Management in Community-Based Stroke Care: A Secondary Analysis of Nurses’ Perspectives. J. Clin. Med. 2020, 9, 985. https://doi.org/10.3390/jcm9040985
Kidd L, Booth J, Lawrence M, Rowat A. Implementing Supported Self-Management in Community-Based Stroke Care: A Secondary Analysis of Nurses’ Perspectives. Journal of Clinical Medicine. 2020; 9(4):985. https://doi.org/10.3390/jcm9040985
Chicago/Turabian StyleKidd, Lisa, Joanne Booth, Maggie Lawrence, and Anne Rowat. 2020. "Implementing Supported Self-Management in Community-Based Stroke Care: A Secondary Analysis of Nurses’ Perspectives" Journal of Clinical Medicine 9, no. 4: 985. https://doi.org/10.3390/jcm9040985
APA StyleKidd, L., Booth, J., Lawrence, M., & Rowat, A. (2020). Implementing Supported Self-Management in Community-Based Stroke Care: A Secondary Analysis of Nurses’ Perspectives. Journal of Clinical Medicine, 9(4), 985. https://doi.org/10.3390/jcm9040985





