A New Customized Bioactive Glass Filler to Functionalize Resin Composites: Acid-Neutralizing Capability, Degree of Conversion, and Apatite Precipitation
Abstract
1. Introduction
2. Materials and Methods
2.1. Experimental and Reference Materials
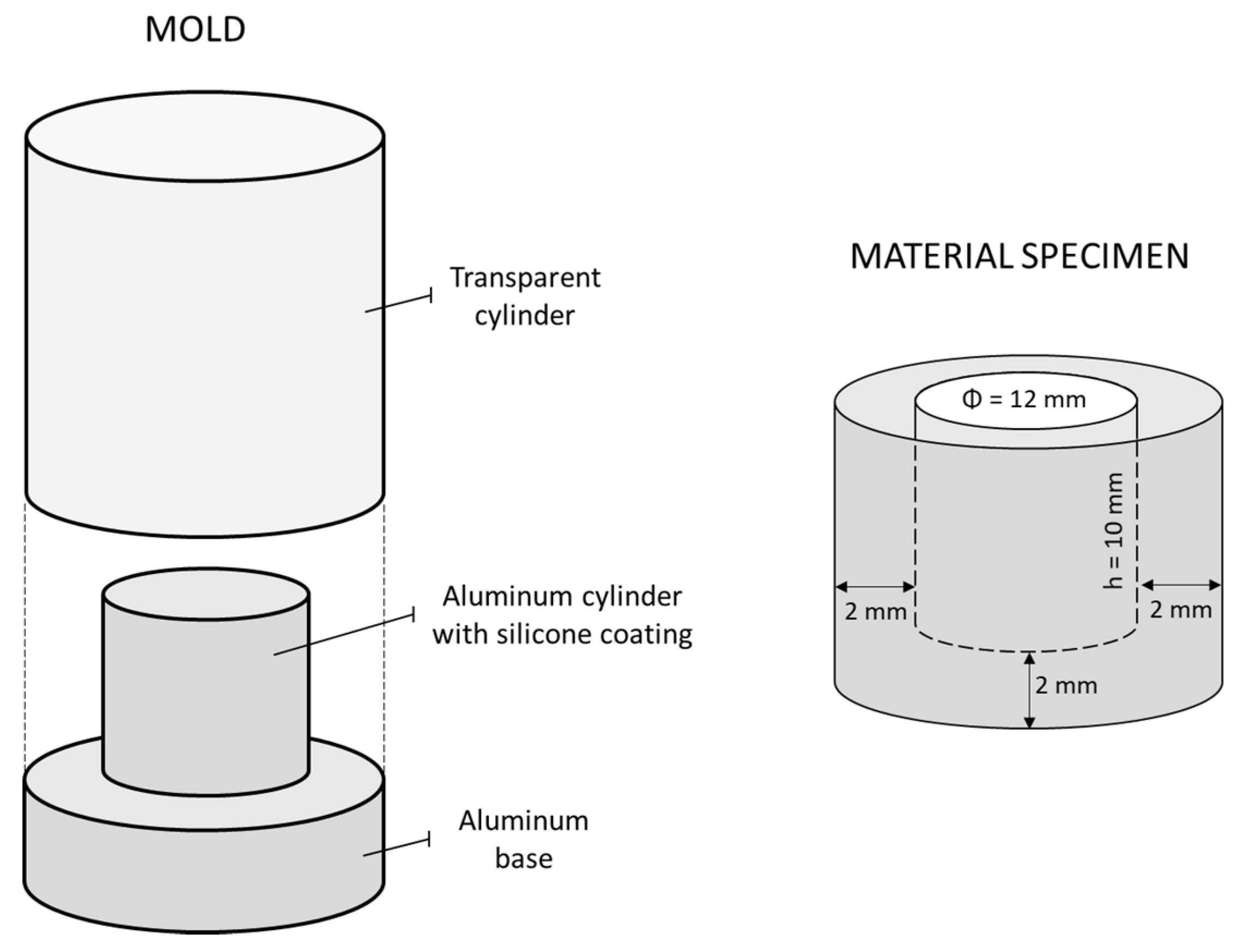
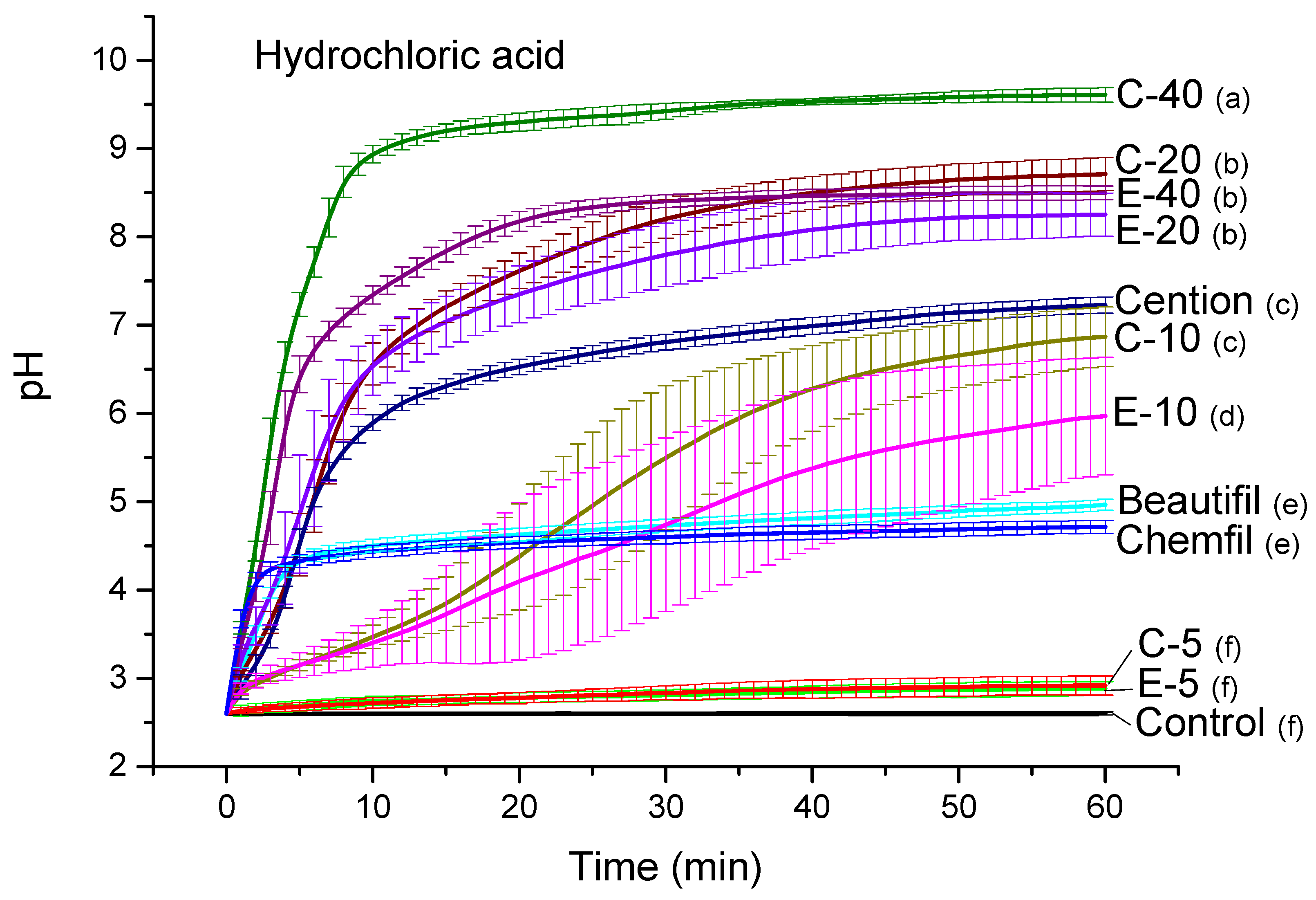
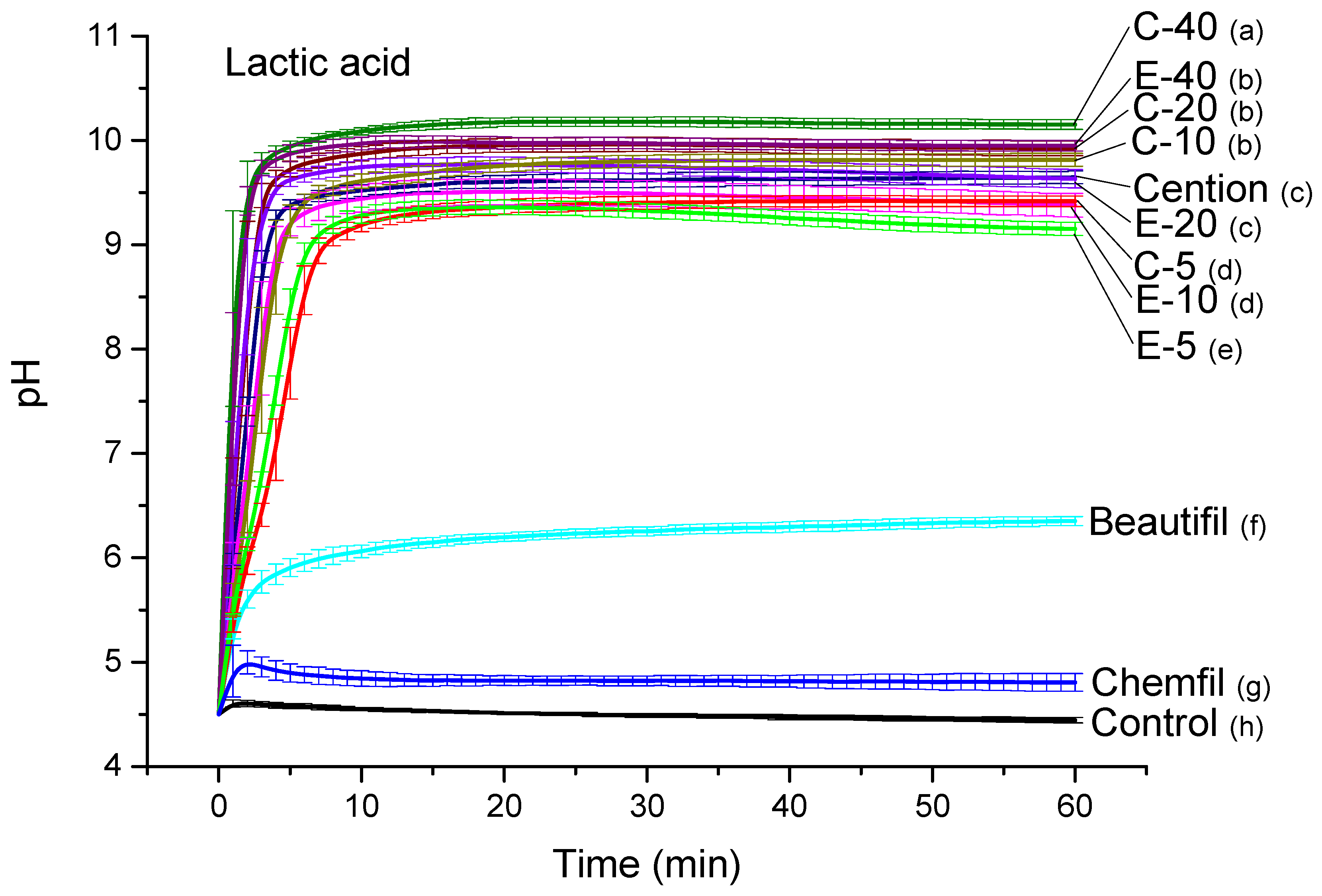
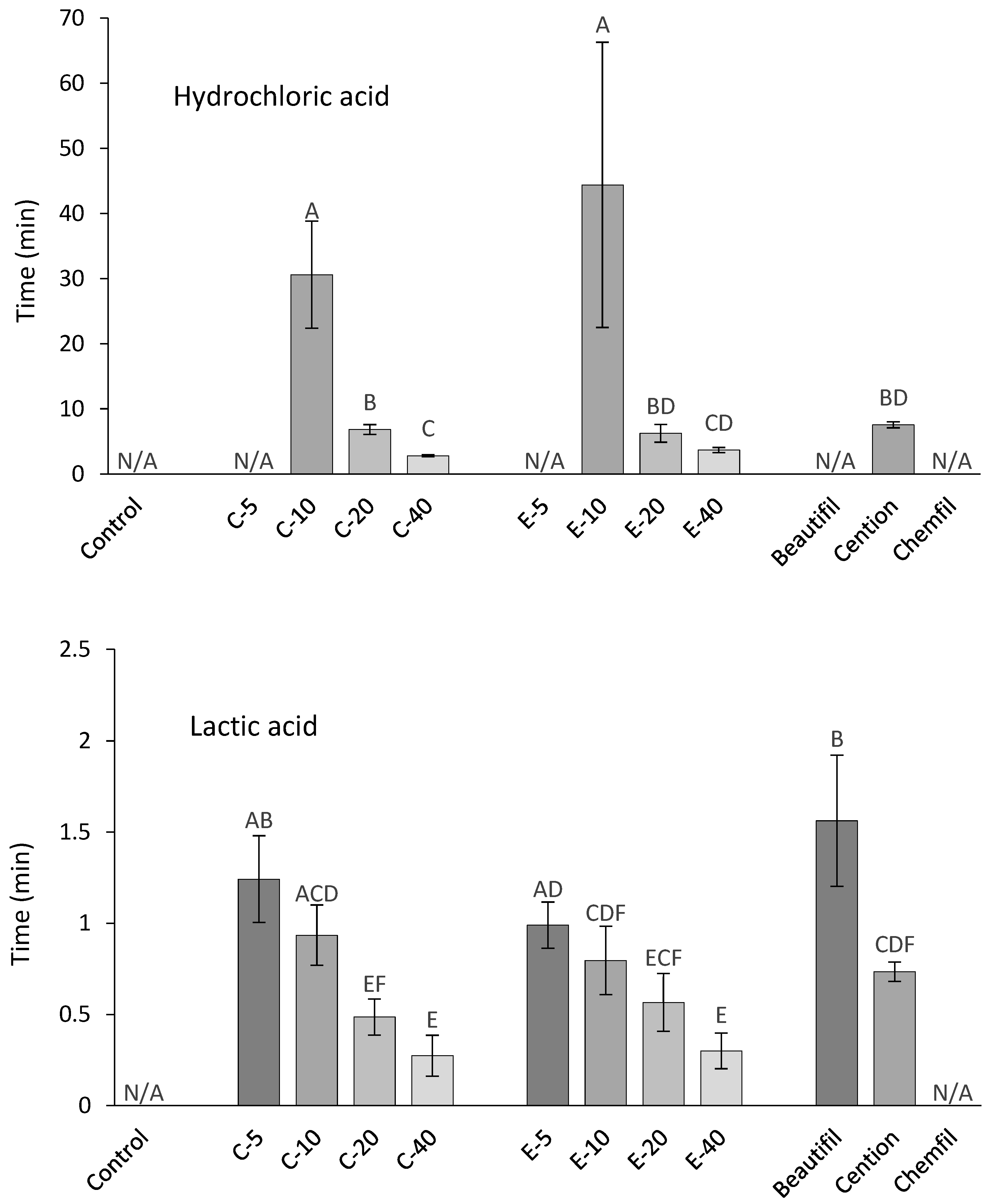
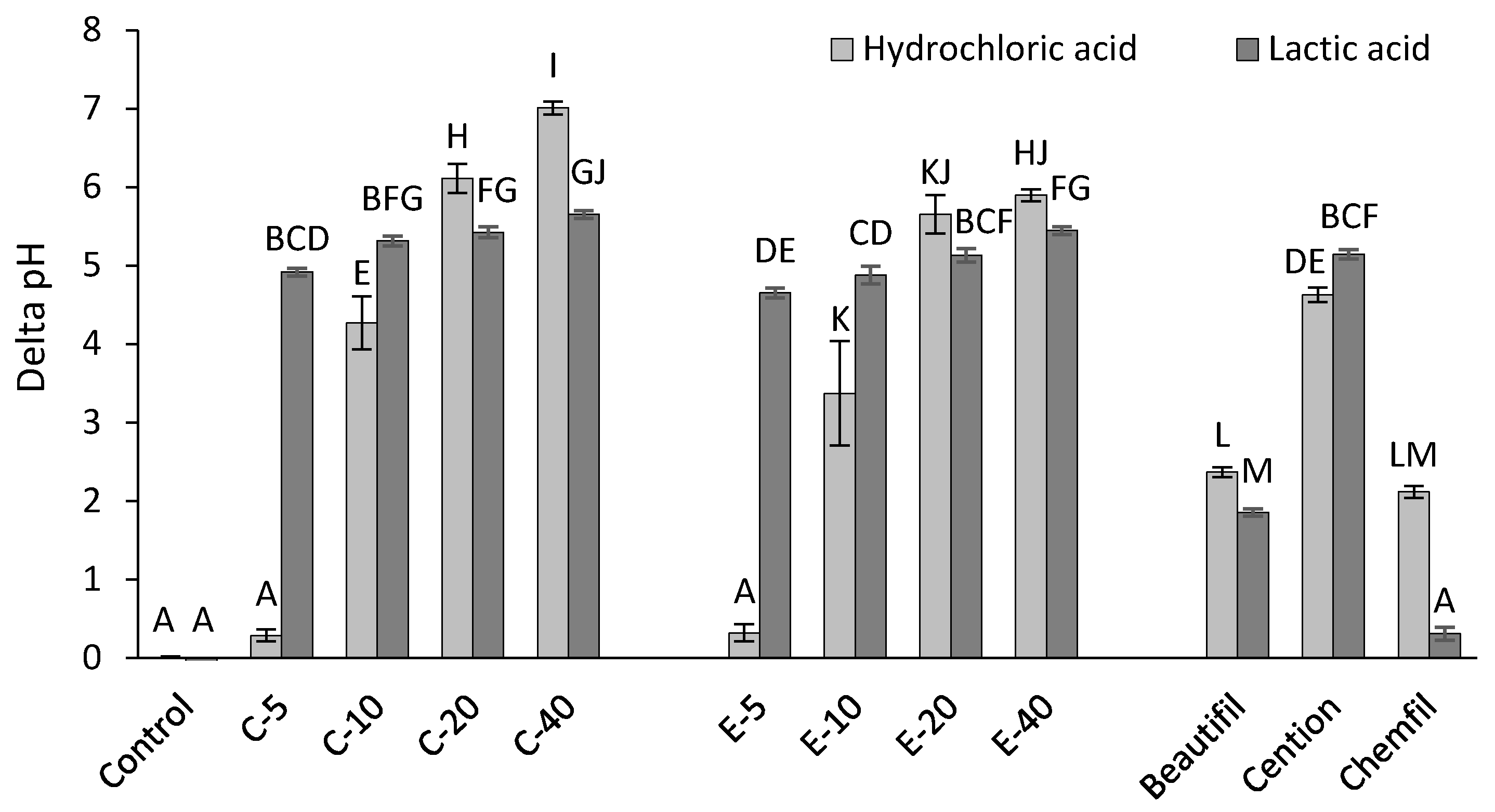
2.2. Acid Neutralization
2.3. Degree of Conversion
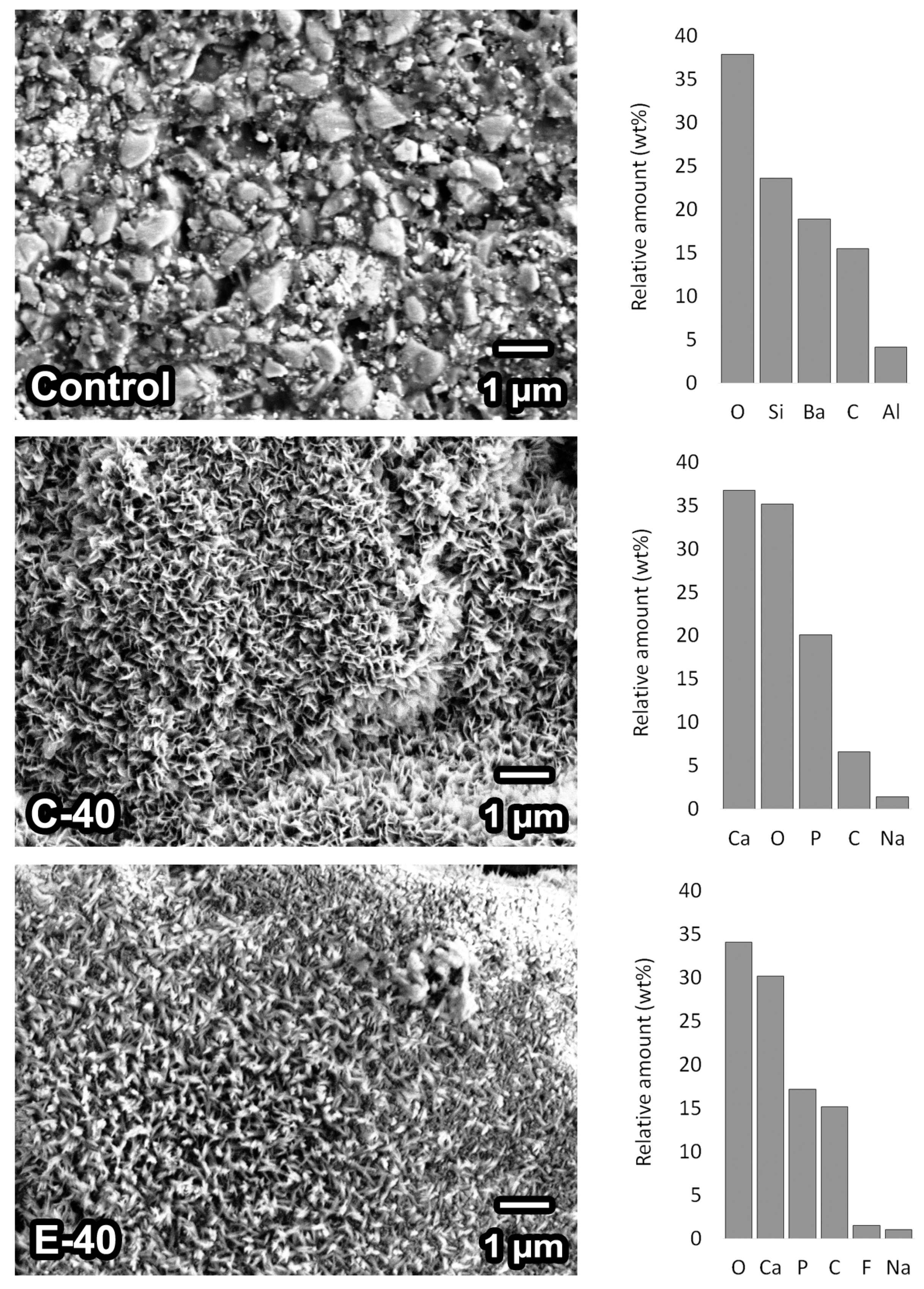
2.4. Scanning Electron Microscopy and Energy-Dispersive X-Ray Spectroscopy
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Nedeljkovic, I.; De Munck, J.; Vanloy, A.; Declerck, D.; Lambrechts, P.; Peumans, M.; Teughels, W.; Van Meerbeek, B.; Van Landuyt, K.L. Secondary caries: Prevalence, characteristics, and approach. Clin. Oral Investig. 2020, 24, 683–691. [Google Scholar] [CrossRef]
- Tauböck, T.T.; Zehnder, M.; Schweizer, T.; Stark, W.J.; Attin, T.; Mohn, D. Functionalizing a dentin bonding resin to become bioactive. Dent. Mater. 2014, 30, 868–875. [Google Scholar] [CrossRef]
- Al-Eesa, N.A.; Wong, F.S.L.; Johal, A.; Hill, R.G. Fluoride containing bioactive glass composite for orthodontic adhesives—Ion release properties. Dent. Mater. 2017, 33, 1324–1329. [Google Scholar] [CrossRef] [PubMed]
- Al-Eesa, N.A.; Johal, A.; Hill, R.G.; Wong, F.S.L. Fluoride containing bioactive glass composite for orthodontic adhesives—Apatite formation properties. Dent. Mater. 2018, 34, 1127–1133. [Google Scholar] [CrossRef] [PubMed]
- Al-Eesa, N.A.; Karpukhina, N.; Hill, R.G.; Johal, A.; Wong, F.S.L. Bioactive glass composite for orthodontic adhesives—Formation and characterisation of apatites using MAS-NMR and SEM. Dent. Mater. 2019, 35, 597–605. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.-Y.; Kwon, J.-S.; Kim, K.-N.; Kim, K.-M. Enamel surface with pit and fissure sealant containing 45S5 bioactive glass. J. Dent. Res. 2016, 95, 550–557. [Google Scholar] [CrossRef] [PubMed]
- Dieckmann, P.; Mohn, D.; Zehnder, M.; Attin, T.; Tauböck, T.T. Light transmittance and polymerization of bulk-fill composite materials doped with bioactive micro-fillers. Materials 2019, 12, 4087. [Google Scholar] [CrossRef] [PubMed]
- Kaur, G.; Pandey, O.P.; Singh, K.; Homa, D.; Scott, B.; Pickrell, G. A review of bioactive glasses: Their structure, properties, fabrication and apatite formation. J. Biomed. Mater. Res. A 2014, 102, 254–274. [Google Scholar] [CrossRef]
- Jones, J.R. Review of bioactive glass: From Hench to hybrids. Acta Biomater. 2013, 9, 4457–4486. [Google Scholar] [CrossRef]
- Zheng, K.; Boccaccini, A.R. Sol-gel processing of bioactive glass nanoparticles: A review. Adv. Colloid Interface Sci. 2017, 249, 363–373. [Google Scholar] [CrossRef]
- Hench, L.L. The story of Bioglass®. J. Mater. Sci. Mater. Med. 2006, 17, 967–978. [Google Scholar] [CrossRef] [PubMed]
- Fuss, M.; Wicht, M.J.; Attin, T.; Derman, S.N.H.; Noack, M.J. Protective buffering capacity of restorative dental materials in vitro. J. Adhes. Dent. 2017, 19, 177–183. [Google Scholar] [PubMed]
- Attin, T.; Becker, K.; Wiegand, A.; Tauböck, T.T.; Wegehaupt, F.J. Impact of laminar flow velocity of different acids on enamel calcium loss. Clin. Oral Investig. 2013, 17, 595–600. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Attin, T.; Wegehaupt, F.J. Impact of erosive conditions on tooth-colored restorative materials. Dent. Mater. 2014, 30, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Wegehaupt, F.J.; Tauböck, T.T.; Attin, T. Durability of the anti-erosive effect of surfaces sealants under erosive abrasive conditions. Acta Odontol. Scand. 2013, 71, 1188–1194. [Google Scholar] [CrossRef] [PubMed]
- Nedeljkovic, I.; De Munck, J.; Slomka, V.; Van Meerbeek, B.; Teughels, W.; Van Landuyt, K.L. Lack of buffering by composites promotes shift to more cariogenic bacteria. J. Dent. Res. 2016, 95, 875–881. [Google Scholar] [CrossRef]
- Waltimo, T.; Brunner, T.J.; Vollenweider, M.; Stark, W.J.; Zehnder, M. Antimicrobial effect of nanometric bioactive glass 45S5. J. Dent. Res. 2007, 86, 754–757. [Google Scholar] [CrossRef]
- Tarle, Z.; Par, M. Degree of Conversion. In Dental Composite Materials for Direct Restorations; Miletic, V., Ed.; Springer International Publishing: Cham, Switzerland, 2018. [Google Scholar]
- Tauböck, T.T.; Marovic, D.; Zeljezic, D.; Steingruber, A.D.; Attin, T.; Tarle, Z. Genotoxic potential of dental bulk-fill resin composites. Dent. Mater. 2017, 33, 788–795. [Google Scholar] [CrossRef]
- Tauböck, T.T.; Jäger, F.; Attin, T. Polymerization shrinkage and shrinkage force kinetics of high- and low-viscosity dimethacrylate- and ormocer-based bulk-fill resin composites. Odontology 2019, 107, 103–110. [Google Scholar] [CrossRef]
- Wegehaupt, F.J.; Tauböck, T.T.; Attin, T.; Belibasakis, G.N. Influence of light-curing mode on the cytotoxicity of resin-based surface sealants. BMC Oral Health 2014, 14, 48. [Google Scholar] [CrossRef]
- Par, M.; Spanovic, N.; Tauböck, T.T.; Attin, T.; Tarle, Z. Degree of conversion of experimental resin composites containing bioactive glass 45S5: The effect of post-cure heating. Sci. Rep. 2019, 9, 17245. [Google Scholar] [CrossRef] [PubMed]
- Par, M.; Spanovic, N.; Bjelovucic, R.; Skenderovic, H.; Gamulin, O.; Tarle, Z. Curing potential of experimental resin composites with systematically varying amount of bioactive glass: Degree of conversion, light transmittance and depth of cure. J. Dent. 2018, 75, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Par, M.; Tarle, Z.; Hickel, R.; Ilie, N. Polymerization kinetics of experimental bioactive composites containing bioactive glass. J. Dent. 2018, 76, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Vallittu, P.K.; Boccaccini, A.R.; Hupa, L.; Watts, D.C. Bioactive dental materials–Do they exist and what does bioactivity mean? Dent. Mater. 2018, 34, 693–694. [Google Scholar] [CrossRef] [PubMed]
- Khvostenko, D.; Hilton, T.J.; Ferracane, J.L.; Mitchell, J.C.; Kruzic, J.J. Bioactive glass fillers reduce bacterial penetration into marginal gaps for composite restorations. Dent. Mater. 2016, 32, 73–81. [Google Scholar] [CrossRef]
- Tiskaya, M.; Al-Eesa, N.A.; Wong, F.S.L.; Hill, R.G. Characterization of the bioactivity of two commercial composites. Dent. Mater. 2019, 35, 1757–1768. [Google Scholar] [CrossRef]
- Par, M.; Tarle, Z.; Hickel, R.; Ilie, N. Mechanical properties of experimental composites containing bioactive glass after artificial aging in water and ethanol. Clin. Oral Investig. 2019, 23, 2733–2741. [Google Scholar] [CrossRef]
- Par, M.; Tarle, Z.; Hickel, R.; Ilie, N. Dentin bond strength of experimental composites containing bioactive glass: Changes during aging for up to 1 year. J. Adhes. Dent. 2018, 20, 325–334. [Google Scholar]
- Price, R.B. The Dental Curing Light. In Dental Composite Materials for Direct Restorations; Miletic, V., Ed.; Springer International Publishing: Cham, Switzerland, 2018. [Google Scholar]
- Da Costa, J.; Goncalves, F.; Ferracane, J. Comparison of two-step versus four-step composite finishing/polishing disc systems: Evaluation of a new two-step composite polishing disc system. Oper. Dent. 2011, 36, 205–212. [Google Scholar] [CrossRef]
- Rueggeberg, F.A.; Hashinger, D.T.; Fairhurst, C.W. Calibration of FTIR conversion analysis of contemporary dental resin composites. Dent. Mater. 1990, 6, 241–249. [Google Scholar] [CrossRef]
- Aina, V.; Bertinetti, L.; Cerrato, G.; Cerruti, M.; Lusvardi, G.; Malavasi, G.; Morterra, C.; Tacconi, L.; Menabue, L. On the dissolution/reaction of small-grain Bioglass® 45S5 and F-modified bioactive glasses in artificial saliva (AS). Appl. Surf. Sci. 2011, 257, 4185–4195. [Google Scholar] [CrossRef]
- Chen, X.; Chen, X.; Brauer, D.S.; Wilson, R.M.; Law, R.V.; Hill, R.G.; Karpukhina, N. Sodium is not essential for high bioactivity of glasses. Int. J. Appl. Glass Sci. 2017, 8, 428–437. [Google Scholar] [CrossRef] [PubMed]
- Itota, T.; Al-Naimi, O.T.; Carrick, T.E.; Yoshiyama, M.; McCabe, J.F. Fluoride release and neutralizing effect by resin-based materials. Oper. Dent. 2005, 30, 522–527. [Google Scholar] [PubMed]
- Kakuda, S.; Sidhu, S.K.; Sano, H. Buffering or non-buffering; an action of pit-and-fissure sealants. J. Dent. 2015, 43, 1285–1289. [Google Scholar] [CrossRef] [PubMed]
- Moreau, J.L.; Sun, L.; Chow, L.C.; Xu, H.H.K. Mechanical and acid neutralizing properties and bacteria inhibition of amorphous calcium phosphate dental nanocomposite. J. Biomed. Mater. Res. B 2011, 98, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, J.W.; Aggarwal, A.; Czarnecka, B.; Limanowska-Shaw, H. The rate of change of pH of lactic acid exposed to glass-ionomer dental cements. Biomaterials 2000, 21, 1989–1993. [Google Scholar] [CrossRef]
- Nicholson, J.W.; Czarnecka, B.; Limanowska-Shaw, H. A preliminary study of the effect of glass-ionomer and related dental cements on the pH of lactic acid storage solutions. Biomaterials 1999, 20, 155–158. [Google Scholar] [CrossRef]
- Yang, S.-Y.; Piao, Y.-Z.; Kim, S.-M.; Lee, Y.-K.; Kim, K.-N.; Kim, K.-M. Acid neutralizing, mechanical and physical properties of pit and fissure sealants containing melt-derived 45S5 bioactive glass. Dent. Mater. 2013, 29, 1228–1235. [Google Scholar] [CrossRef]
- Yang, S.-Y.; Kim, S.-H.; Choi, S.-Y.; Kim, K.-M. Acid neutralizing ability and shear bond strength using orthodontic adhesives containing three different types of bioactive glass. Materials 2016, 9, 125. [Google Scholar] [CrossRef]
- Musanje, L.; Darvell, B.W. Aspects of water sorption from the air, water and artificial saliva in resin composite restorative materials. Dent. Mater. 2003, 19, 414–422. [Google Scholar] [CrossRef]
- Moritsuka, M.; Kitasako, Y.; Burrow, M.F.; Ikeda, M.; Tagami, J.; Nomura, S. Quantitative assessment for stimulated saliva flow rate and buffering capacity in relation to different ages. J. Dent. 2006, 34, 716–720. [Google Scholar] [CrossRef] [PubMed]
- Rankine, C.A.N.; Moreno, E.C.; Vogel, G.L.; Margolis, H.C. Micro-analytical determination of pH, calcium, and phosphate in plaque fluid. J. Dent. Res. 1985, 64, 1275–1280. [Google Scholar] [CrossRef] [PubMed]
- Waltimo, T.; Mohn, D.; Paqué, F.; Brunner, T.J.; Stark, W.J.; Imfeld, T.; Schätzle, M.; Zehnder, M. Fine-tuning of bioactive glass for root canal disinfection. J. Dent. Res. 2009, 88, 235–238. [Google Scholar] [CrossRef] [PubMed]
- Wallace, K.E.; Hill, R.G.; Pembroke, J.T.; Brown, C.J.; Hatton, P.V. Influence of sodium oxide content on bioactive glass properties. J. Mater. Sci. Mater. Med. 1999, 10, 697–701. [Google Scholar] [CrossRef] [PubMed]
- Par, M.; Gamulin, O.; Marovic, D.; Skenderovic, H.; Klaric, E.; Tarle, Z. Conversion and temperature rise of remineralizing composites reinforced with inert fillers. J. Dent. 2016, 48, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Gajewski, V.E.S.; Pfeifer, C.S.; Fróes-Salgado, N.R.G.; Boaro, L.C.C.; Braga, R.R. Monomers used in resin composites: Degree of conversion, mechanical properties and water sorption/solubility. Braz. Dent. J. 2012, 23, 508–514. [Google Scholar] [CrossRef]
- Okuyama, K.; Nakata, T.; Pereira, P.N.R.; Kawamoto, C.; Komatsu, H.; Sano, H. Prevention of artificial caries: Effect of bonding agent, resin composite and topical fluoride application. Oper. Dent. 2006, 31, 135–142. [Google Scholar] [CrossRef]
- Dawes, C. What is the critical pH and why does a tooth dissolve in acid? J. Can. Dent. Assoc. 2003, 69, 722–724. [Google Scholar]

| Bioactive Glass 45S5 | Experimental Fluoride-Containing Bioactive Glass | Inert Barium Glass | Silica | |
|---|---|---|---|---|
| Particle size (d50) | 3 µm | 3 µm | 1 µm | 5–50 nm |
| Composition (wt%) | 45.0% SiO2 24.5% CaO 24.5% Na2O 6.0% P2O5 | 33.5% SiO2 33.0% CaO 10.5% Na2O 11.0% P2O5 12.0% CaF2 | 55.0% SiO2 25.0% BaO 10.0% Al2O3 10.0% B2O3 | >99.8% SiO2 |
| Silanization (wt%) | none | none | 3.2 | 4–6 |
| Manufacturer | Schott, Mainz, Germany | Schott, Mainz, Germany | Schott, Mainz, Germany | Evonik, Hanau, Germany |
| Product name/LOT | G018-144/M111473 | experimental batch | GM27884/Sil13696 | Aerosil R 7200/157020635 |
| Material Designation | Filler Composition (wt%) | Total Filler Ratio (wt%) | |||
|---|---|---|---|---|---|
| Bioactive Glass 45S5 | Experimental Fluoride-Containing Bioactive Glass | Reinforcing Fillers (Inert Barium Glass: Silica = 2:1) | |||
| Control | 0 | 0 | 70 | 70 | |
| C-series | C-5 | 5 | 0 | 65 | 70 |
| C-10 | 10 | 0 | 60 | 70 | |
| C-20 | 20 | 0 | 50 | 70 | |
| C-40 | 40 | 0 | 30 | 70 | |
| E- series | E-5 | 0 | 5 | 65 | 70 |
| E-10 | 0 | 10 | 60 | 70 | |
| E-20 | 0 | 20 | 50 | 70 | |
| E-40 | 0 | 40 | 30 | 70 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Par, M.; Attin, T.; Tarle, Z.; Tauböck, T.T. A New Customized Bioactive Glass Filler to Functionalize Resin Composites: Acid-Neutralizing Capability, Degree of Conversion, and Apatite Precipitation. J. Clin. Med. 2020, 9, 1173. https://doi.org/10.3390/jcm9041173
Par M, Attin T, Tarle Z, Tauböck TT. A New Customized Bioactive Glass Filler to Functionalize Resin Composites: Acid-Neutralizing Capability, Degree of Conversion, and Apatite Precipitation. Journal of Clinical Medicine. 2020; 9(4):1173. https://doi.org/10.3390/jcm9041173
Chicago/Turabian StylePar, Matej, Thomas Attin, Zrinka Tarle, and Tobias T. Tauböck. 2020. "A New Customized Bioactive Glass Filler to Functionalize Resin Composites: Acid-Neutralizing Capability, Degree of Conversion, and Apatite Precipitation" Journal of Clinical Medicine 9, no. 4: 1173. https://doi.org/10.3390/jcm9041173
APA StylePar, M., Attin, T., Tarle, Z., & Tauböck, T. T. (2020). A New Customized Bioactive Glass Filler to Functionalize Resin Composites: Acid-Neutralizing Capability, Degree of Conversion, and Apatite Precipitation. Journal of Clinical Medicine, 9(4), 1173. https://doi.org/10.3390/jcm9041173







