Characteristics of Older Adults Who Were Early Adopters of Medical Cannabis in the Florida Medical Marijuana Use Registry
Abstract
1. Introduction
2. Methods
Data Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
References
- National Conference of State Legislatures (NCSL). State Medical Marijuana Laws. Available online: http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx (accessed on 9 June 2019).
- Denham, B.E. Attitudes toward legalization of marijuana in the United States, 1986–2016: Changes in determinants of public opinion. Int. J. Drug Policy 2019, 71, 78–90. [Google Scholar] [CrossRef] [PubMed]
- Cerda, M.; Wall, M.; Keyes, K.M.; Galea, S.; Hasin, D. Medical marijuana laws in 50 states: Investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug Alcohol Depend. 2012, 120, 22–27. [Google Scholar] [CrossRef]
- Number of Legal Medical Marijuana Patients. Available online: https://medicalmarijuana.procon.org/view.resource.php?resourceID=005889 (accessed on 9 June 2019).
- Compton, W.M.; Han, B.; Hughes, A.; Jones, C.M.; Blanco, C. Use of marijuana for medical purposes among adults in the United States. JAMA 2017, 317, 209–211. [Google Scholar] [CrossRef]
- Wong, S.S.; Wilens, T.E. Medical Cannabinoids in children and adolescents: A systematic review. Pediatrics 2017, 140, 295. [Google Scholar] [CrossRef] [PubMed]
- Sexton, M.; Cuttler, C.; Finnell, J.S.; Mischley, L.K. A Cross-sectional survey of medical cannabis users: Patterns of use and perceived efficacy. Cannabis Cannabinoid Res. 2016, 1, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Lucas, P.; Walsh, Z. Medical cannabis access, use, and substitution for prescription opioids and other substances: A survey of authorized medical cannabis patients. Int. J. Drug Policy 2017, 42, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Han, B.H.; Sherman, S.; Mauro, P.M.; Martins, S.S.; Rotenberg, J.; Palamar, J.J. Demographic trends among older cannabis users in the United States, 2006–2013. Addiction 2017, 112, 516–525. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.A.; Ilgen, M.A.; Jannausch, M.; Bohnert, K.M. Comparing adults who use cannabis medically with those who use recreationally: Results from a national sample. Addict. Behav. 2016, 61, 99–103. [Google Scholar] [CrossRef]
- Dai, H.; Richter, K.P. A national survey of marijuana use among us adults with medical conditions, 2016–2017. JAMA Netw. Open 2019, 2, e1911936. [Google Scholar] [CrossRef]
- Ellis, J.D.; Resko, S.M.; Szechy, K.; Smith, R.; Early, T.J. Characteristics associated with attitudes toward marijuana legalization in Michigan. J. Psychoact. Drugs 2019, 51, 1–8. [Google Scholar] [CrossRef]
- Briscoe, J.; Casarett, D. Medical marijuana use in older adults. J. Am. Geriatr. Soc. 2018, 66, 859–863. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, S.L.; Striley, C.W. Marijuana use among adults 50 years or older in the 21st century. Gerontol. Geriatr. Med. 2018, 4. [Google Scholar] [CrossRef] [PubMed]
- Guy, W. Clinical global impression (CGI). Available online: https://www.psywellness.com.sg/docs/CGI.pdf (accessed on 20 January 2020).
- Sativex(R). Delta-9-Tetrahydrocannabinol and Cannabidiol; GW Pharma: Cambridge, UK, 2005. [Google Scholar]
- Hall, W.; Renstrom, M.; Poznyak, V. (Eds.) The Health and Social Effects of Nonmedical Cannabis Use; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Hall, W.; Weier, M. Assessing the public health impacts of legalizing recreational cannabis use in the USA. Clin. Pharm. 2015, 97, 607–615. [Google Scholar] [CrossRef] [PubMed]
- Resko, S.; Ellis, J.; Early, T.J.; Szechy, K.A.; Rodriguez, B.; Agius, E. Understanding public attitudes toward cannabis legalization: Qualitative findings from a statewide survey. Subst. Use Misuse 2019, 54, 1247–1259. [Google Scholar] [CrossRef]
- Volkow, N.D.; Baler, R.D.; Compton, W.M.; Weiss, S.R. Adverse health effects of marijuana use. N. Engl. J. Med. 2014, 370, 2219–2227. [Google Scholar] [CrossRef]
- Whiting, P.F.; Wolff, R.F.; Deshpande, S.; Di Nisio, M.; Duffy, S.; Hernandez, A.V.; Keurentjes, J.C.; Lang, S.; Misso, K.; Ryder, S.; et al. Cannabinoids for medical use: A systematic review and meta-analysis. JAMA 2015, 313, 2456–2473. [Google Scholar] [CrossRef]
- ElSohly, M.A.; Radwan, M.M.; Gul, W.; Chandra, S.; Galal, A. Phytochemistry of cannabis sativa L. Prog. Chem. Org. Nat. Prod. 2017, 103, 1–36. [Google Scholar] [CrossRef]
- Elsohly, M.A.; Slade, D. Chemical constituents of marijuana: The complex mixture of natural cannabinoids. Life Sci. 2005, 78, 539–548. [Google Scholar] [CrossRef]
- Jiang, R.; Yamaori, S.; Takeda, S.; Yamamoto, I.; Watanabe, K. Identification of cytochrome P450 enzymes responsible for metabolism of cannabidiol by human liver microsomes. Life Sci. 2011, 89, 165–170. [Google Scholar] [CrossRef]
- Brown, J.D.; Winterstein, A.G. Potential adverse drug events and drug-drug interactions with medical and consumer cannabidiol (CBD) use. J. Clin. Med. 2019, 8, 989. [Google Scholar] [CrossRef]
- Bergamaschi, M.M.; Queiroz, R.H.; Zuardi, A.W.; Crippa, J.A. Safety and side effects of cannabidiol, a cannabis sativa constituent. Curr. Drug. Saf. 2011, 6, 237–249. [Google Scholar] [CrossRef] [PubMed]
- Iffland, K.; Grotenhermen, F. An update on safety and side effects of cannabidiol: A review of clinical data and relevant animal studies. Cannabis Cannabinoid Res. 2017, 2, 139–154. [Google Scholar] [CrossRef] [PubMed]
- GW Research Ltd. Drug Approval Package: Epidiolex (Cannabidiol). Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2018/210365Orig1s000TOC.cfm (accessed on 9 June 2019).
- Brown, J.D. Potential adverse drug events with tetrahydrocannabinol (THC) due to drug–drug interactions. J. Clin. Med. 2020, 9, 919. [Google Scholar] [CrossRef] [PubMed]
- Corsonello, A.; Pedone, C.; Incalzi, R.A. Age-related pharmacokinetic and pharmacodynamic changes and related risk of adverse drug reactions. Curr. Med. Chem. 2010, 17, 571–584. [Google Scholar] [CrossRef]
- Trifiro, G.; Spina, E. Age-related changes in pharmacodynamics: Focus on drugs acting on central nervous and cardiovascular systems. Curr. Drug Metab. 2011, 12, 611–620. [Google Scholar] [CrossRef]
- Dowling, G.J.; Weiss, S.R.; Condon, T.P. Drugs of abuse and the aging brain. Neuropsychopharmacology 2008, 33, 209–218. [Google Scholar] [CrossRef]
- Qato, D.M.; Alexander, G.C.; Conti, R.M.; Johnson, M.; Schumm, P.; Lindau, S.T. Use of prescription and over-the-counter medications and dietary supplements among older adults in the united states. JAMA 2008, 300, 2867–2878. [Google Scholar] [CrossRef]
- Schneider, K.L.; Kastenmuller, K.; Weckbecker, K.; Bleckwenn, M.; Bohme, M.; Stingl, J.C. Potential drug-drug interactions in a cohort of elderly, polymedicated primary care patients on antithrombotic treatment. Drugs Aging 2018, 35, 559–568. [Google Scholar] [CrossRef]
- Tulner, L.R.; Frankfort, S.V.; Gijsen, G.J.; van Campen, J.P.; Koks, C.H.; Beijnen, J.H. Drug-drug interactions in a geriatric outpatient cohort: Prevalence and relevance. Drugs Aging 2008, 25, 343–355. [Google Scholar] [CrossRef]
- Nobili, A.; Pasina, L.; Tettamanti, M.; Lucca, U.; Riva, E.; Marzona, I.; Monesi, L.; Cucchiani, R.; Bortolotti, A.; Fortino, I.; et al. Potentially severe drug interactions in elderly outpatients: Results of an observational study of an administrative prescription database. J. Clin. Pharm. 2009, 34, 377–386. [Google Scholar] [CrossRef]
- Johnell, K.; Klarin, I. The relationship between number of drugs and potential drug-drug interactions in the elderly: A study of over 600,000 elderly patients from the Swedish prescribed drug register. Drug Saf. 2007, 30, 911–918. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.D.; Hutchison, L.C.; Li, C.; Painter, J.T.; Martin, B.C. Predictive validity of the beers and screening tool of older persons’ potentially inappropriate prescriptions (STOPP) criteria to detect adverse drug events, hospitalizations, and emergency department visits in the United States. J. Am. Geriatr. Soc. 2016, 64, 22–30. [Google Scholar] [CrossRef] [PubMed]
- American geriatrics society 2019 updated AGS beers criteria(R) for potentially inappropriate medication use in older adults. J. Am. Geriatr. Soc. 2019, 67, 674–694. [CrossRef]
- O’Mahony, D.; O’Sullivan, D.; Byrne, S.; O’Connor, M.N.; Ryan, C.; Gallagher, P. STOPP/START criteria for potentially inappropriate prescribing in older people: Version 2. Age Ageing 2015, 44, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Rudolph, J.L.; Salow, M.J.; Angelini, M.C.; McGlinchey, R.E. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch. Intern. Med. 2008, 168, 508–513. [Google Scholar] [CrossRef]
- Budnitz, D.S.; Pollock, D.A.; Weidenbach, K.N.; Mendelsohn, A.B.; Schroeder, T.J.; Annest, J.L. National surveillance of emergency department visits for outpatient adverse drug events. JAMA 2006, 296, 1858–1866. [Google Scholar] [CrossRef]
- Budnitz, D.S.; Shehab, N.; Kegler, S.R.; Richards, C.L. Medication use leading to emergency department visits for adverse drug events in older adults. Ann. Intern. Med. 2007, 147, 755–765. [Google Scholar] [CrossRef]
- Gurwitz, J.H.; Field, T.S.; Harrold, L.R.; Rothschild, J.; Debellis, K.; Seger, A.C.; Cadoret, C.; Fish, L.S.; Garber, L.; Kelleher, M.; et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA 2003, 289, 1107–1116. [Google Scholar] [CrossRef]
- Budnitz, D.S.; Lovegrove, M.C.; Shehab, N.; Richards, C.L. Emergency hospitalizations for adverse drug events in older Americans. N. Engl. J. Med. 2011, 365, 2002–2012. [Google Scholar] [CrossRef]
- Brown, J.D.; Painter, J.; Li, C.; Hutchison, L.C.; Martin, B. Adverse drug events in the elderly occurring in emergency, inpatient, and outpatient departments in an administrative claims database. Value Health 2014, 17, A155. [Google Scholar] [CrossRef][Green Version]
- Hanlon, J.T.; Schmader, K.E.; Koronkowski, M.J.; Weinberger, M.; Landsman, P.B.; Samsa, G.P.; Lewis, I.K. Adverse drug events in high risk older outpatients. J. Am. Geriatr. Soc. 1997, 45, 945–948. [Google Scholar] [CrossRef] [PubMed]
- Poudel, D.R.; Acharya, P.; Ghimire, S.; Dhital, R.; Bharati, R. Burden of hospitalizations related to adverse drug events in the USA: A retrospective analysis from large inpatient database. Pharm. Drug Saf. 2017, 26, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Riaz, M.; Brown, J.D. Association of adverse drug events with hospitalization outcomes and costs in older adults in the USA using the nationwide readmissions database. Pharm. Med. 2019, 33, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Winterstein, A.G.; Sauer, B.C.; Hepler, C.D.; Poole, C. Preventable drug-related hospital admissions. Ann. Pharm. 2002, 36, 1238–1248. [Google Scholar] [CrossRef] [PubMed]
- Von Laue, N.C.; Schwappach, D.L.; Koeck, C.M. The epidemiology of preventable adverse drug events: A review of the literature. Wien. Klin. Wochenschr. 2003, 115, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, L.A.; Winterstein, A.G.; Sondergaard, B.; Haugbolle, L.S.; Melander, A. Systematic review of the incidence and characteristics of preventable adverse drug events in ambulatory care. Ann. Pharm. 2007, 41, 1411–1426. [Google Scholar] [CrossRef]
- Kanjanarat, P.; Winterstein, A.G.; Johns, T.E.; Hatton, R.C.; Gonzalez-Rothi, R.; Segal, R. Nature of preventable adverse drug events in hospitals: A literature review. Am. J. Health Syst. Pharm. 2003, 60, 1750–1759. [Google Scholar] [CrossRef]
| Age Group | ||||
|---|---|---|---|---|
| Characteristic, N (%) | Total (N = 4447) | 50–64 Years (N = 2662) | 65–74 Years (N = 1238) | 75+ Years (N = 547) |
| Age, mean (SD) | 63.4 (9.17) | 57.3 (4.17) | 68.8 (2.71) | 80.9 (5.37) |
| Race | ||||
| White | 3893 (87.5) | 2290 (86.0) | 1115 (90.1) | 488 (89.2) |
| Black | 157 (3.5) | 118 (4.4) | 29 (2.3) | *** |
| Hispanic, Latino or Spanish | 203 (4.6) | 121 (4.6) | 52 (4.2) | 30 (5.5) |
| Other/Unknown ‡ | 194 (4.4) | 133 (5.0) | 42 (3.4) | 19 (3.5) |
| Patient condition assessed by provider | ||||
| Normal, not at all ill | 195 (4.4) | 111 (4.1) | 61 (4.9) | 23 (4.2) |
| Borderline ill | 99 (2.2) | 59 (2.2) | 20 (1.6) | 20 (3.7) |
| Mildly ill | 588 (13.2) | 359 (13.5) | 167 (13.5) | 62 (11.3) |
| Moderately ill | 1909 (42.9) | 1150 (43.2) | 512 (41.4) | 247 (45.1) |
| Markedly ill | 1156 (26.0) | 715 (26.9) | 317 (25.6) | 124 (22.7) |
| Severely ill | 412 (9.3) | 224 (8.4) | 130 (10.5) | 58 (10.6) |
| Among the most extremely ill | 88 (2.0) | 44 (1.7) | 31 (2.5) | 13 (2.4) |
| History of substance use | ||||
| Alcohol | 628 (14.1) | 406 (15.3) | 160 (12.9) | 62 (11.3) |
| Smoking | 444 (10.0) | 323 (12.1) | 202 (8.2) | 20 (3.7) |
| Illicit drugs | 162 (3.6) | 118 (4.4) | 42 (3.4) | *** |
| Cannabis type ordered ± | ||||
| Medical cannabis | 1481 (33.3) | 926 (34.8) | 409 (33.1) | 146 (26.7) |
| Low-THC cannabis | 2000 (45.0) | 1172 (44.0) | 534 (43.1) | 294 (53.7) |
| Both low-THC and medical cannabis | 966 (21.7) | 564 (21.2) | 295 (23.8) | 107 (19.6) |
| Planned order duration | ||||
| <1 month | 469 (10.6) | 288 (10.8) | 110 (8.9) | 71 (13.0) |
| 1–3 months | 1919 (43.2) | 1209 (45.4) | 515 (41.6) | 195 (35.7) |
| 3–12 months | 382 (8.6) | 238 (8.9) | 109 (8.8) | 35 (6.4) |
| >12 months or indefinitely | 1343 (30.2) | 739 (27.8) | 406 (32.8) | 198 (36.2) |
| Not specified | 334 (7.5) | 188 (7.1) | 98 (7.9) | 48 (8.8) |
| Age Group | ||||
|---|---|---|---|---|
| Chief Complaint †, N (%) | Total (N = 7548) | 50–64 Years (N = 2662) | 65–74 Years (N = 1238) | 75+ Years (N = 547) |
| Musculoskeletal disorders and spasms | 2154 (48.4) | 1348 (50.6) | 534 (43.1) | 272 (49.7) |
| Cancer | 691 (15.5) | 350 (13.2) | 235 (19.0) | 106 (19.4) |
| Epilepsy or seizures | 130 (2.9) | 93 (3.5) | 30 (2.4) | *** |
| Glaucoma | 87 (2.0) | 41 (1.5) | 30 (2.4) | 16 (2.9) |
| Autoimmune or immune disorders ± | 142 (3.2) | 104 (3.9) | 29 (2.3) | *** |
| Post-traumatic stress disorder (PTSD) | 444 (10.0) | 298 (11.2) | 136 (11.0) | *** |
| Amyotrophic lateral sclerosis (ALS) | 24 (0.5) | *** | *** | *** |
| Crohn’s disease | 52 (1.2) | 33 (1.2) | 15 (1.2) | *** |
| Parkinson’s disease | 201 (4.5) | 51 (1.9) | 92 (7.4) | 58 (10.6) |
| Multiple sclerosis (MS) | 121 (2.7) | *** | *** | *** |
| Chronic pain | 2019 (45.4) | 1242 (46.7) | 520 (42.0) | 257 (47.0) |
| Back, spine, or neck conditions | 696 (15.7) | 475 (17.8) | 147 (11.9) | 74 (13.5) |
| Major brain and head injuries | 149 (3.4) | *** | *** | *** |
| Gastrointestinal conditions | 225 (5.1) | 137 (5.2) | 69 (5.6) | 19 (3.5) |
| Headaches or migraines | 461 (10.4) | 318 (12.0) | 93 (7.5) | 50 (9.1) |
| Other nervous system and neurological disorders | 486 (10.9) | 269 (10.1) | 123 (9.9) | 94 (17.2) |
| Psychological disorders (excl. PTSD) | 589 (13.2) | 376 (14.1) | 158 (12.8) | 55 (10.1) |
| Sleep disorders | 310 (7.0) | 199 (7.5) | 82 (6.6) | 29 (5.3) |
| Others | 35 (0.8) | *** | *** | *** |
| Age Group | ||||
|---|---|---|---|---|
| Medication Class, N (%) | Total (N = 4447) | 50–64 Years (N = 2662) | 65–74 Years (N = 1238) | 75+ Years (N = 547) |
| Number of medications per patient, mean (SD), IQR | 2.4 (2.54) 3 (0–4) | 2.4 (2.52) 3 (0–4) | 2.4 (2.57) 3 (0–4) | 2.3 (2.58) 3 (0–4) |
| Antidepressants | 1060 (23.8) | 670 (25.2) | 289 (23.4) | 101 (18.5) |
| Antipsychotics | 128 (2.9) | 82 (3.1) | 35 (2.8) | 11 (2.0) |
| Anxiolytics and benzodiazepines | 1046 (23.5) | 674 (25.3) | 285 (23.0) | 87 (15.9) |
| Mood stabilizers | 37 (0.8) | *** | *** | *** |
| Stimulants and amphetamines | 124 (2.8) | *** | *** | *** |
| Hypnotics and sedatives | 292 (6.6) | 168 (6.3) | 98 (7.9) | 26 (4.8) |
| Opioids ± | 1271 (28.6) | 863 (32.4) | 296 (23.9) | 112 (20.5) |
| Non-opioid analgesics | 861 (19.4) | 512 (19.2) | 229 (18.5) | 120 (21.9) |
| Skeletal muscle relaxants | 611 (13.7) | 458 (17.2) | 127 (10.3) | 26 (4.8) |
| Other musculoskeletal agents †† | 133 (3.0) | 73 (2.7) | 38 (3.1) | 22 (4.0) |
| Anticonvulsants and antiepileptics | 760 (17.1) | 496 (18.6) | 176 (14.2) | 88 (16.1) |
| Anti-Parkinson | 162 (3.6) | 58 (2.2) | 69 (5.6) | 35 (6.4) |
| Other neurological agents ±± | 71 (1.6) | 39 (1.5) | 21 (1.7) | 11 (2.0) |
| Antiemetics | 200 (4.5) | 128 (4.8) | 56 (4.5) | 16 (2.9) |
| Other GI agents | 217 (4.9) | 135 (5.1) | 58 (4.7) | 24 (4.4) |
| Cardiovascular agents | 1241 (27.9) | 623 (23.4) | 417 (33.7) | 201 (36.8) |
| Antidiabetic agents | 271 (6.1) | 147 (5.5) | 92 (7.4) | 32 (5.9) |
| Hematologic agents | 126 (2.8) | 52 (2.0) | 51 (4.1) | 23 (4.2) |
| Hormonal agents and steroids | 596 (13.4) | 319 (12.0) | 198 (16.0) | 79 (14.4) |
| Genitourinary agents | 264 (5.9) | 99 (3.7) | 100 (8.1) | 65 (11.9) |
| Respiratory agents | 181 (4.1) | 90 (3.4) | 60 (4.9) | 31 (5.7) |
| Chemotherapeutic agents | 102 (2.3) | *** | *** | *** |
| Autoimmune agents | 75 (1.7) | *** | *** | *** |
| Antivirals incl. HIV medications | 40 (0.9) | *** | *** | *** |
| Anti-infective agents | 50 (1.1) | *** | *** | *** |
| Ophthalmic and glaucoma medications | 51 (1.2) | 17 (0.6) | 18 (1.5) | 16 (2.9) |
| OTC medications, vitamins, supplements and others | 348 (8.2) | 204 (7.6) | 111 (9.0) | 48 (8.8) |
| Total (N = 1225) | Yes (%) |
|---|---|
| Follow-Up Question Since Last Treatment Visit | |
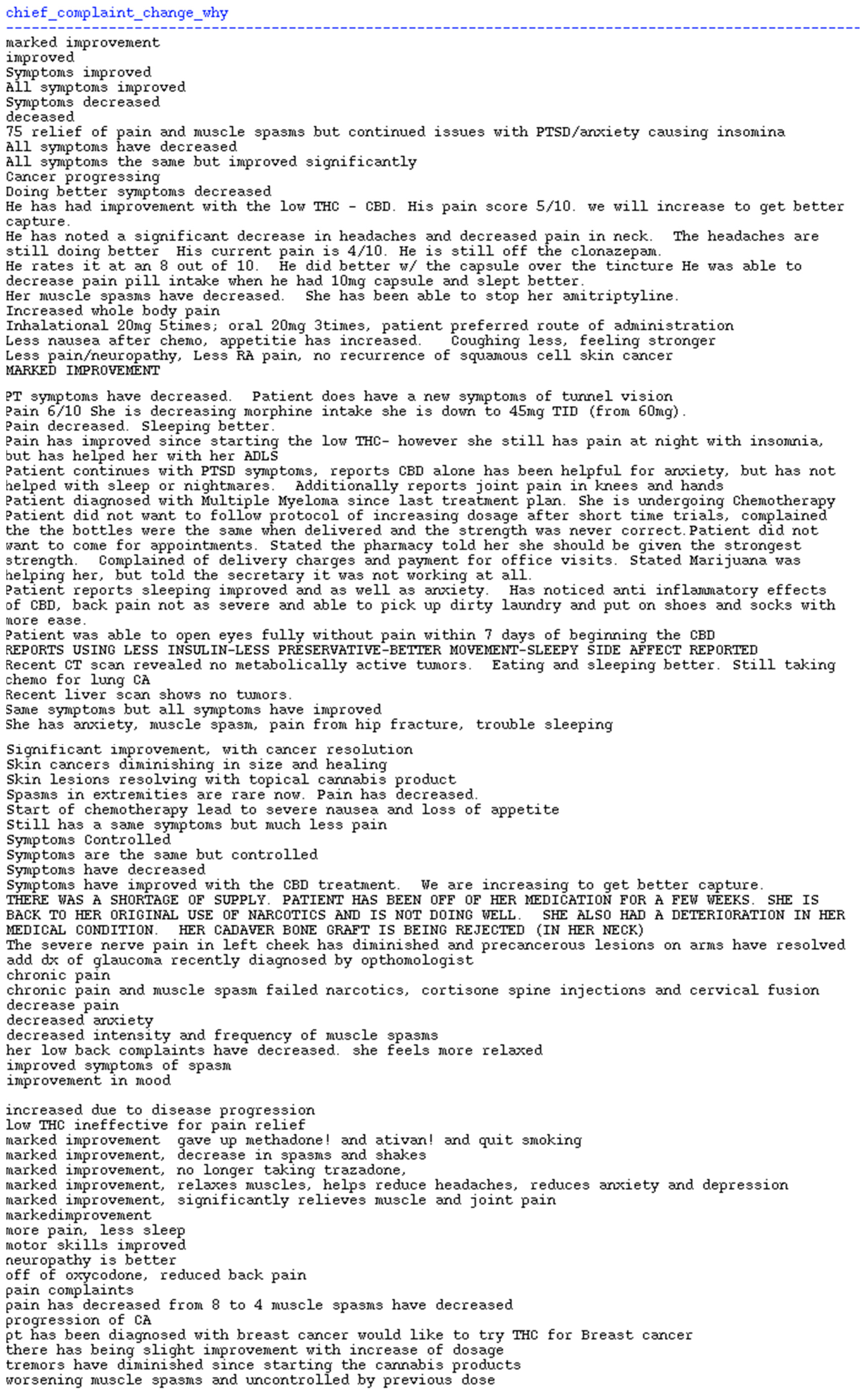
| Changes in chief complaint since last visit? | 10.0% |
| Changes in alcohol, smoking, or illicit drug use since last visit? † | 1.4% |
| Changes in comorbidities since last visit? | 1.7% |
| Hospitalizations since last visit? | 2.9% |
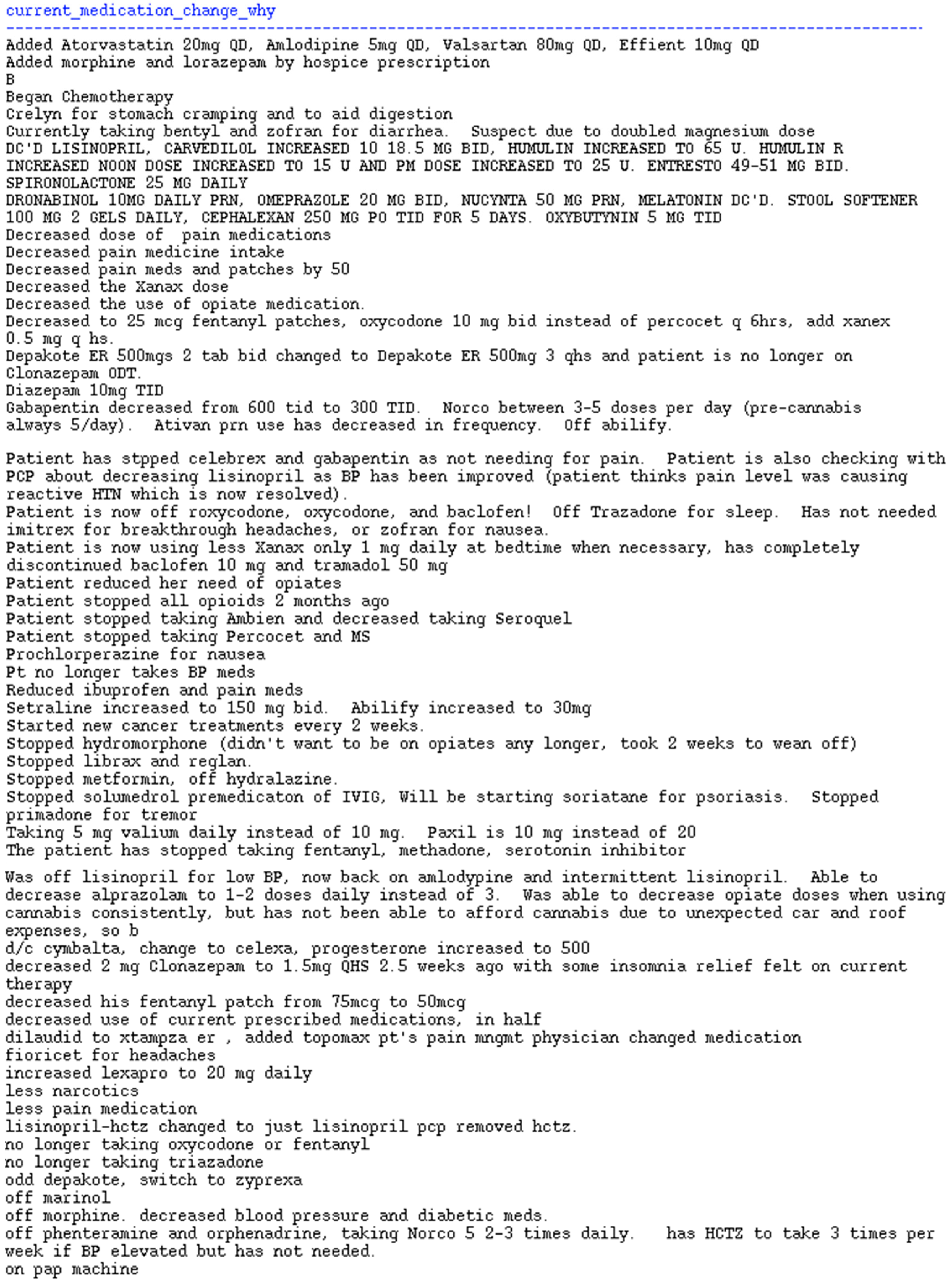
| Changes in current medications since last visit? | 10.0% |
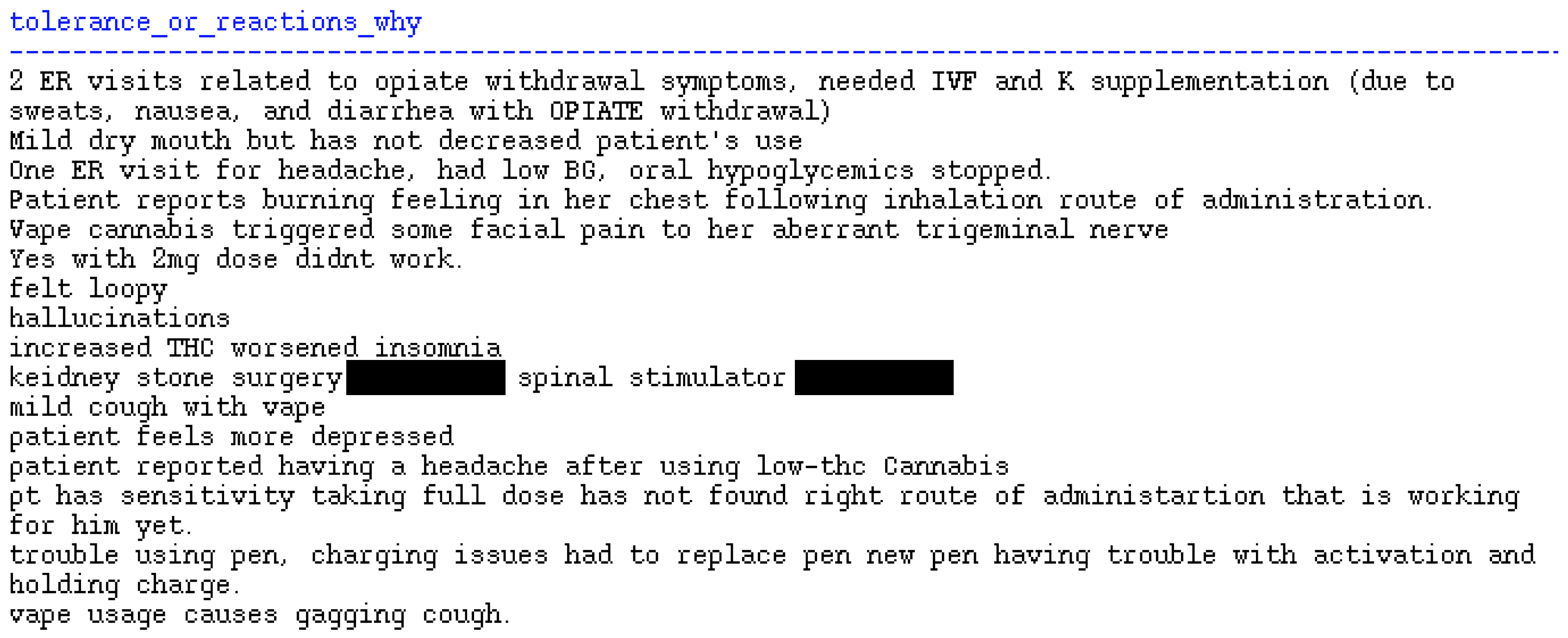
| Were there indicators of reaction to cannabis since last visit? ‡ | 2.0% |
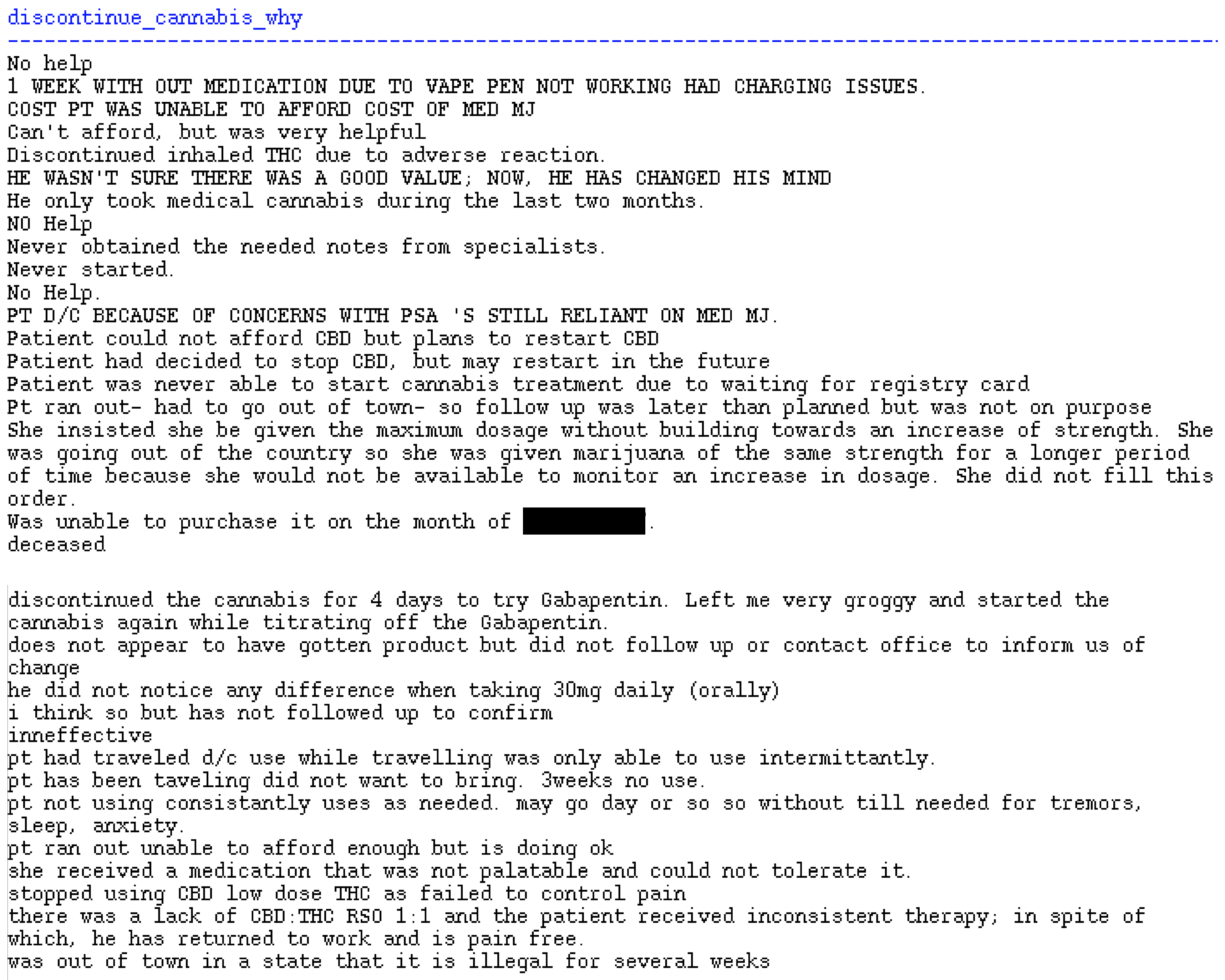
| Did the patient discontinue cannabis use? | 4.6% |
| Patient Condition Since the Initiation of Treatment Compared to Condition Initially Assessed | |
| Very much improved | 10.8% |
| Much improved | 31.4% |
| Minimally improved | 30.5% |
| No change from baseline | 24.7% |
| Minimally worse | 1.4% |
| Much worse | 0.9% |
| Very much worse | 0.4% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brown, J.D.; Costales, B.; van Boemmel-Wegmann, S.; Goodin, A.J.; Segal, R.; Winterstein, A.G. Characteristics of Older Adults Who Were Early Adopters of Medical Cannabis in the Florida Medical Marijuana Use Registry. J. Clin. Med. 2020, 9, 1166. https://doi.org/10.3390/jcm9041166
Brown JD, Costales B, van Boemmel-Wegmann S, Goodin AJ, Segal R, Winterstein AG. Characteristics of Older Adults Who Were Early Adopters of Medical Cannabis in the Florida Medical Marijuana Use Registry. Journal of Clinical Medicine. 2020; 9(4):1166. https://doi.org/10.3390/jcm9041166
Chicago/Turabian StyleBrown, Joshua D., Brianna Costales, Sascha van Boemmel-Wegmann, Amie J. Goodin, Richard Segal, and Almut G. Winterstein. 2020. "Characteristics of Older Adults Who Were Early Adopters of Medical Cannabis in the Florida Medical Marijuana Use Registry" Journal of Clinical Medicine 9, no. 4: 1166. https://doi.org/10.3390/jcm9041166
APA StyleBrown, J. D., Costales, B., van Boemmel-Wegmann, S., Goodin, A. J., Segal, R., & Winterstein, A. G. (2020). Characteristics of Older Adults Who Were Early Adopters of Medical Cannabis in the Florida Medical Marijuana Use Registry. Journal of Clinical Medicine, 9(4), 1166. https://doi.org/10.3390/jcm9041166






