Epigenetic Alterations Associated with the Overall Survival and Recurrence Free Survival among Oral Squamous Cell Carcinoma Patients
Abstract
1. Introduction
2. Methods
Statistical Analysis
3. Results
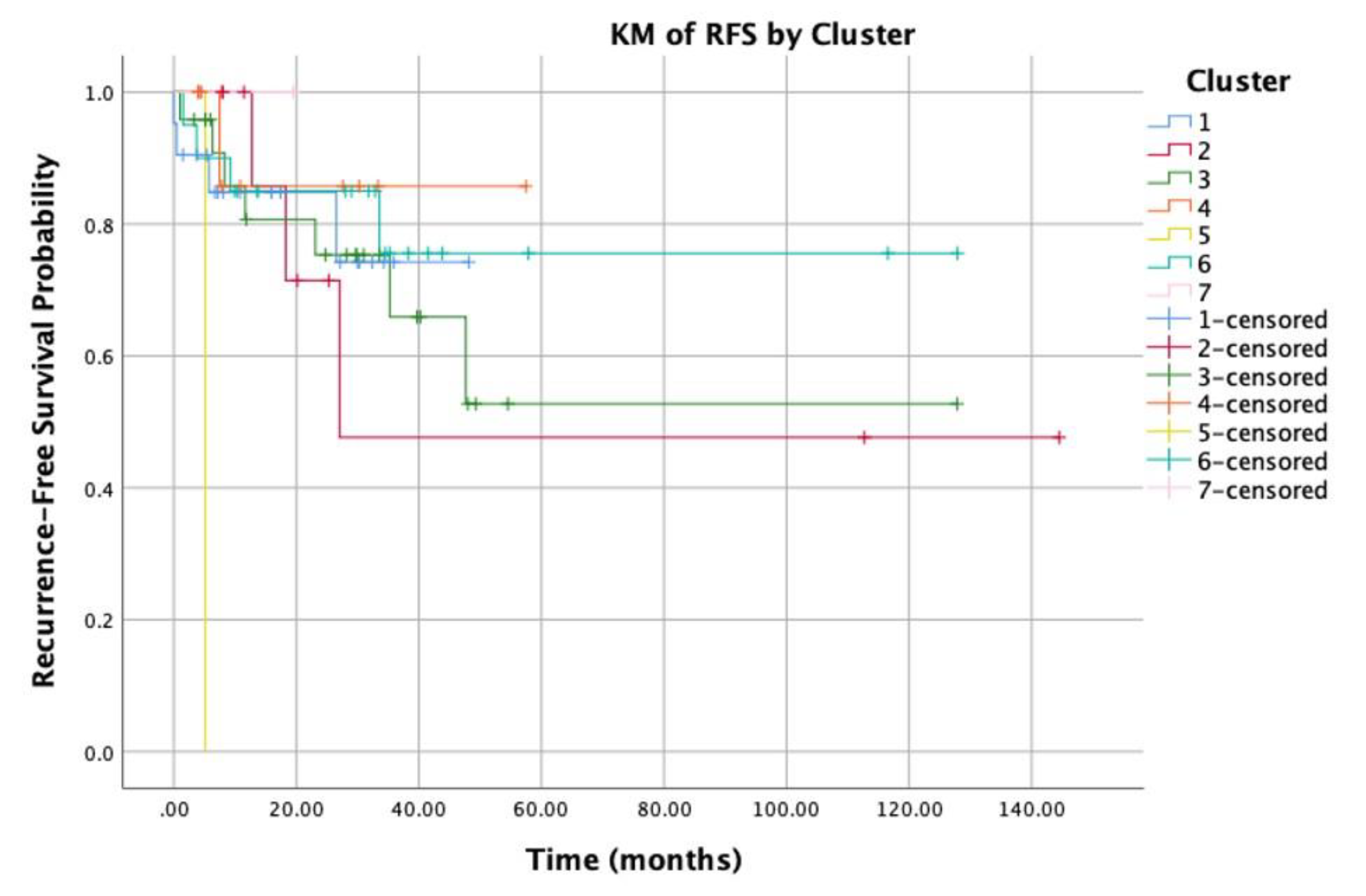
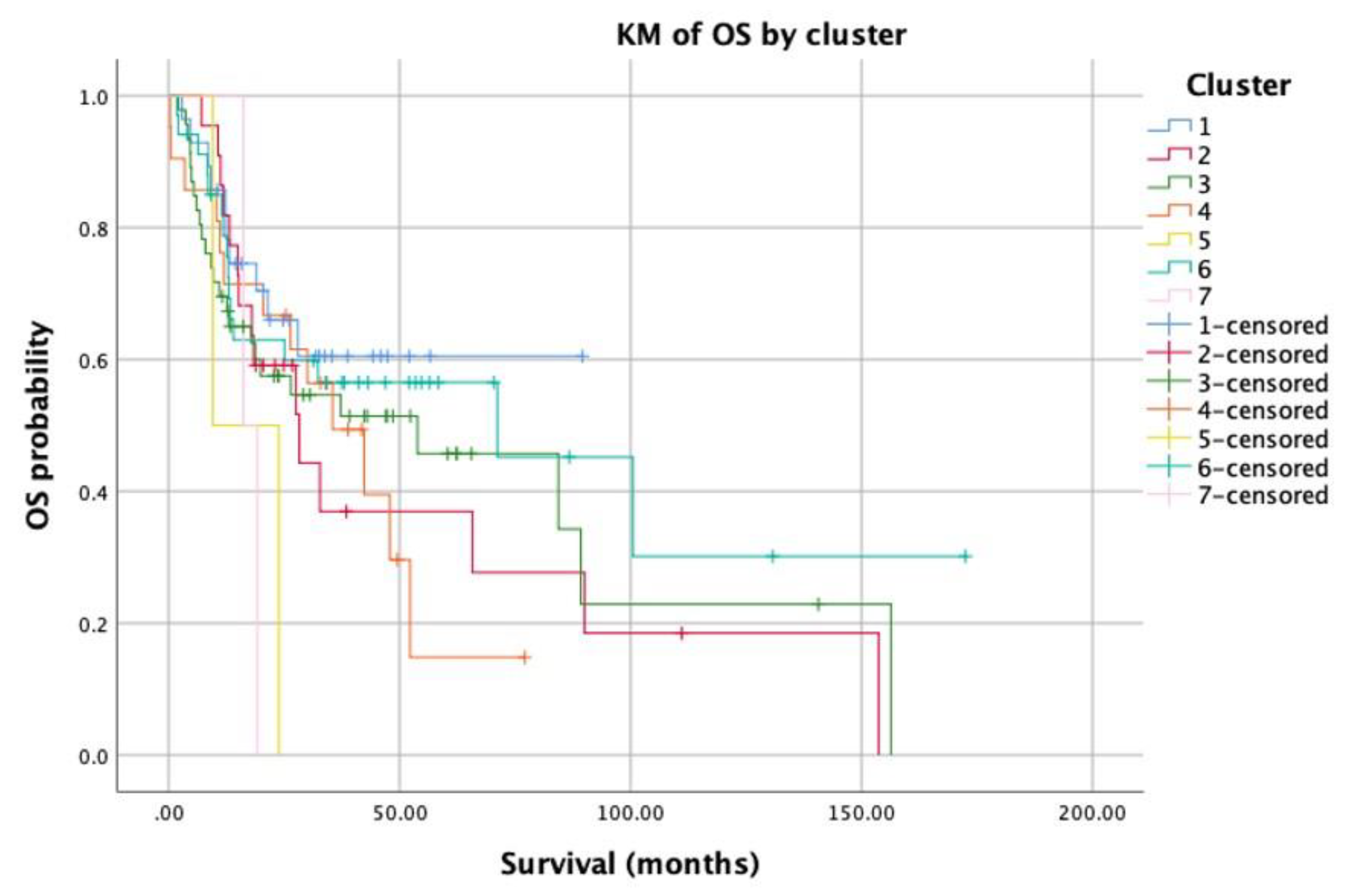
3.1. Clusters Analysis
3.2. Correlation between Clusters Pattern and Demographic, Pathological, and Clinical Features
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Paolino, G.; Didona, D.; Macrì, G.; Calvieri, S.; Mercuri, S.R. Nasopharyngeal Melanoma. In Noncutaneous Melanoma [Internet]; Scott, J.F., Gerstenblith, M.R., Eds.; Codon Publications: Brisbane, Australia, 2018; Chapter 4. Available online: https://www.ncbi.nlm.nih.gov/books/NBK506987/ (accessed on 18 March 2020). [CrossRef]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA. Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Lacko, M.; Braakhuis, B.J.M.; Sturgis, E.M.; Boedeker, C.C.; Suárez, C.; Rinaldo, A.; Ferlito, A.; Takes, R.P. Genetic Susceptibility to Head and Neck Squamous Cell Carcinoma. Int. J. Radiat. Oncol. 2014, 89, 38–48. [Google Scholar] [CrossRef]
- Stransky, N.; Egloff, A.M.; Tward, A.D.; Kostic, A.D.; Cibulskis, K.; Sivachenko, A.; Kryukov, G.V.; Lawrence, M.; Sougnez, C.; Mckenna, A.; et al. The mutational landscape of head and neck squamous cell carcinoma. Science (80-) 2012, 333, 1157–1160. [Google Scholar] [CrossRef]
- Leemans, C.R.; Braakhuis, B.J.M.; Brakenhoff, R.H. The molecular biology of head and neck cancer. Nat. Rev. Cancer 2011, 11, 9–22. [Google Scholar] [CrossRef]
- Lindsay, C.; Seikaly, H.; Biron, V.L. Epigenetics of oropharyngeal squamous cell carcinoma: Opportunities for novel chemotherapeutic targets. J. Otolaryngol. Head Neck Surg. 2017, 46, 1–10. [Google Scholar] [CrossRef]
- Irimie, A.I.; Ciocan, C.; Gulei, D.; Mehterov, N.; Atanasov, A.G.; Dudea, D.; Berindan-Neagoe, I. Current insights into oral cancer epigenetics. Int. J. Mol. Sci. 2018, 19, 670. [Google Scholar] [CrossRef]
- Joo, Y.H.; Cho, J.K.; Koo, B.S.; Kwon, M.; Kwon, S.K.; Kwon, S.Y.; Kim, M.S.; Kim, J.K.; Kim, H.; Nam, I.; et al. Guidelines for the surgical management of oral cancer: Korean society of thyroid-head and neck surgery. Clin. Exp. Otorhinolaryngol. 2019, 12, 107–144. [Google Scholar] [PubMed]
- Pfister, D.G.; Spencer, S.; Brizel, D.M.; Burtness, B.; Busse, P.M.; Caudell, J.J.; Cmelak, A.J.; Colevas, A.D.; Dunphy, F.; Eisele, D.W.; et al. Head and neck cancers, version 2.2014. JNCCN J. Natl. Compr. Cancer Netw. 2014, 12, 1454–1487. [Google Scholar] [CrossRef] [PubMed]
- Di Taranto, G.; Chen, S.H.; Elia, R.; Sitpahul, N.; Chan, J.C.Y.; Losco, L.; Cigna, E.; Ribuffo, D.; Chen, H.C. Outcomes following head neck free flap reconstruction requiring interposition vein graft or vascular bridge flap. Head Neck 2019, 41, 2914–2920. [Google Scholar] [CrossRef] [PubMed]
- Jain, P.V.; Sharan, R.; Manikantan, K.; Clark, G.M.; Chatterjee, S.; Mallick, I.; Roy, P.; Arun, P. Redefining adequate margins in oral squamous cell carcinoma: Outcomes from close and positive margins. Eur. Arch. Oto-Rhino-Laryngol. 2020, 277, 1155–1165. [Google Scholar] [CrossRef] [PubMed]
- Chi, A.C.; Day, T.A.; Neville, B.W. Oral cavity and oropharyngeal squamous cell carcinoma-an update. CA. Cancer J. Clin. 2015, 65, 401–421. [Google Scholar] [CrossRef] [PubMed]
- Jenuwein, T.; Allis, C.D. Translating the histone code. Science (80-) 2001, 293, 1074–1080. [Google Scholar] [CrossRef]
- Berger, S.L.; Kouzarides, T.; Shiekhattar, R.; Shilatifard, A. An operational definition of epigenetics. Genes Dev. 2009, 23, 781–783. [Google Scholar] [CrossRef] [PubMed]
- Pfister, S.X.; Ashworth, A. Marked for death: Targeting epigenetic changes in cancer. Nat. Rev. Drug Discov. 2017, 16, 241–263. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, H.P.; Barbash, O.; Creasy, C.L. Targeting epigenetic modifications in cancer therapy: Erasing the roadmap to cancer. Nat. Med. 2019, 25, 403–418. [Google Scholar] [CrossRef]
- Ideker, T.; Sharan, R. Protein networks in disease. Genome Res. 2008, 18, 644–652. [Google Scholar] [CrossRef]
- Chen, J.; Aronow, B.J.; Jegga, A.G. Disease candidate gene identification and prioritization using protein interaction networks. BMC Bioinform. 2009, 10, 1–14. [Google Scholar]
- Franke, L.; Van Bakel, H.; Fokkens, L.; De Jong, E.D.; Egmont-Petersen, M.; Wijmenga, C. Reconstruction of a functional human gene network, with an application for prioritizing positional candidate genes. Am. J. Hum. Genet. 2006, 78, 1011–1025. [Google Scholar] [CrossRef]
- Oti, M.; Snel, B.; Huynen, M.A.; Brunner, H.G. Predicting disease genes using protein-protein interactions. J. Med. Genet. 2006, 43, 691–698. [Google Scholar] [CrossRef]
- Pujana, M.A.; Han, J.D.J.; Starita, L.M.; Stevens, K.N.; Tewari, M.; Ahn, J.S.; Rennert, G.; Moreno, V.; Kirchhoff, T.; Gold, B.; et al. Network modeling links breast cancer susceptibility and centrosome dysfunction. Nat. Genet. 2007, 39, 1338–1349. [Google Scholar] [CrossRef]
- Lim, J.; Hao, T.; Shaw, C.; Patel, A.J.; Szabó, G.; Rual, J.F.; Fisk, C.J.; Li, N.; Smolyar, A.; Hill, D.E.; et al. A Protein-Protein Interaction Network for Human Inherited Ataxias and Disorders of Purkinje Cell Degeneration. Cell 2006, 125, 801–814. [Google Scholar] [CrossRef] [PubMed]
- The Cancer Genome Atlas data portal. Available online: https://www.cancer.gov (accessed on 1 February 2020).
- Broad Genepattern: NMFConsensus. Available online: https://cloud.genepattern.org (accessed on 1 February 2020).
- Lawrence, M.S.; Sougnez, C.; Lichtenstein, L.; Cibulskis, K.; Lander, E.; Gabriel, S.B.; Getz, G.; Ally, A.; Balasundaram, M.; Birol, I.; et al. Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature 2015, 517, 576–582. [Google Scholar]
- R Silhouette Package. Available online: http://stat.ethz.ch/R-manual/R-patched/library/cluster/html/silhouette.html (accessed on 1 February 2020).
- Edge, S.B.; Compton, C.C. The american joint committee on cancer: The 7th edition of the AJCC cancer staging manual and the future of TNM. Ann. Surg. Oncol. 2010, 17, 1471–1474. [Google Scholar] [CrossRef] [PubMed]
- Naganuma, K.; Hatta, M.; Ikebe, T.; Yamazaki, J. Epigenetic alterations of the keratin 13 gene in oral squamous cell carcinoma. BMC Cancer 2014, 14, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zhang, Y.; Loomis, M.M.; Upton, M.P.; Lohavanichbutr, P.; Houck, J.R.; Doody, D.R.; Mendez, E.; Futran, N.; Schwartz, S.M.; et al. Genome-wide loss of heterozygosity and DNA copy number aberration in HPVNegative oral squamous cell carcinoma and their associations with disease-specific survival. PLoS ONE 2015, 10, e0135074. [Google Scholar]
- Melchers, L.J.; Clausen, M.J.A.M.; Mastik, M.F.; Slagter-Menkema, L.; Van Der Wal, J.E.; Wisman, G.B.A.; Roodenburg, J.L.N.; Schuuring, E. Identification of methylation markers for the prediction of nodal metastasis in oral and oropharyngeal squamous cell carcinoma. Epigenetics 2015, 10, 850–860. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, I.P.; Caramelo, F.; Esteves, L.; Oliveira, C.; Marques, F.; Barroso, L.; Melo, J.B.; Carreira, I.M. Genomic and epigenetic signatures associated with survival rate in oral squamous cell carcinoma patients. J. Cancer 2018, 9, 1885–1895. [Google Scholar] [CrossRef]
- Ai, L.; Vo, Q.N.; Zuo, C.; Li, L.; Ling, W.; Suen, J.Y.; Hanna, E.; Brown, K.D.; Fan, C.Y. Ataxia-Telangiectasia-Mutated (ATM) Gene in Head and Neck Squamous Cell Carcinoma: Promoter Hypermethylation with Clinical Correlation in 100 Cases. Cancer Epidemiol. Biomarkers Prev. 2004, 13, 150–156. [Google Scholar] [CrossRef]
- Ribeiro, I.P.; Caramelo, F.; Marques, F.; Domingues, A.; Mesquita, M.; Barroso, L.; Prazeres, H.; Julião, M.J.; Baptista, I.P.; Ferreira, A.; et al. WT1, MSH6, GATA5 and PAX5 as epigenetic oral squamous cell carcinoma biomarkers—A short report. Cell. Oncol. 2016, 39, 573–582. [Google Scholar] [CrossRef]
- Hayashi, M.; Guerrero-Preston, R.; Sidransky, D.; Kochz, W.M. Paired box 5 methylation detection by droplet digital PCR for ultra-sensitive deep surgical margins analysis of head and neck squamous cell carcinoma. Cancer Prev. Res. 2015, 8, 1017–1026. [Google Scholar] [CrossRef]
- Lipp, J.J.; Marvin, M.C.; Shokat, K.M.; Guthrie, C. SR protein kinases promote splicing of nonconsensus introns. Nat. Struct. Mol. Biol. 2015, 22, 611–617. [Google Scholar] [CrossRef]
- Kimura, K.; Wakamatsu, A.; Suzuki, Y.; Ota, T.; Nishikawa, T.; Yamashita, R.; Yamamoto, J.; Sekine, M.; Tsuritani, K.; Wakaguri, H.; et al. Diversification of transcriptional modulation: Large-scale identification and characterization of putative alternative promoters of human genes. Genome Res. 2006, 16, 55–65. [Google Scholar] [CrossRef] [PubMed]
- Dunham, A.; Matthews, L.H.; Burton, J.; Ashurst, J.L.; Howe, K.L.; Ashcroft, K.J.; Beare, D.M.; Burford, D.C.; Hunt, S.E.; Griffiths-Jones, S.; et al. The DNA sequence and analysis of human chromosome 13. Nature 2004, 428, 522–528. [Google Scholar] [CrossRef] [PubMed]
- Toki, S.; Wakai, S.; Sekimizu, M.; Mori, T.; Ichikawa, H.; Kawai, A.; Yoshida, A. PAX7 immunohistochemical evaluation of Ewing sarcoma and other small round cell tumours. Histopathology 2018, 73, 645–652. [Google Scholar] [CrossRef] [PubMed]
- Jia, Z.; Zhang, Z.; Yang, Q.; Deng, C.; Li, D.; Ren, L. Effect of IL2RA and IL2RB gene polymorphisms on lung cancer risk. Int. Immunopharmacol. 2019, 74, 105716. [Google Scholar] [CrossRef] [PubMed]
- Satterwhite, E.; Sonoki, T.; Willis, T.G.; Harder, L.; Nowak, R.; Arriola, E.L.; Liu, H.; Price, H.P.; Gesk, S.; Steinemann, D.; et al. The BCL11 gene family: Involvement of BCL11A in lymphoid malignancies. Blood 2001, 98, 3413–3420. [Google Scholar] [CrossRef] [PubMed]
- Dai, Y.; Wang, M.; Wu, H.; Xiao, M.; Liu, H.; Zhang, D. Loss of FOXN3 in colon cancer activates beta-catenin/TCF signaling and promotes the growth and migration of cancer cells. Oncotarget 2017, 8, 9783–9793. [Google Scholar] [CrossRef]
- Lübbert, M.; Suciu, S.; Hagemeijer, A.; Rüter, B.; Platzbecker, U.; Giagounidis, A.; Selleslag, D.; Labar, B.; Germing, U.; Salih, H.R.; et al. Decitabine improves progression-free survival in older high-risk MDS patients with multiple autosomal monosomies: Results of a subgroup analysis of the randomized phase III study 06011 of the EORTC Leukemia Cooperative Group and German MDS Study Group. Ann. Hematol. 2016, 95, 191–199. [Google Scholar] [CrossRef]
- Fenaux, P.; Mufti, G.J.; Hellström-Lindberg, E.; Santini, V.; Gattermann, N.; Germing, U.; Sanz, G.; List, A.F.; Gore, S.; Seymour, J.F.; et al. Azacitidine prolongs overall survival compared with conventional care regimens in elderly patients with low bone marrow blast count acute myeloid leukemia. J. Clin. Oncol. 2010, 28, 562–569. [Google Scholar] [CrossRef]
- Stewart, D.J.; Issa, J.P.; Kurzrock, R.; Nunez, M.I.; Jelinek, J.; Hong, D.; Oki, Y.; Guo, Z.; Gupta, S.; Wistuba, I.I. Decitabine effect on tumor global DNA methylation and other parameters in a phase I trial in refractory solid tumors and lymphomas. Clin. Cancer Res. 2009, 15, 3881–3888. [Google Scholar] [CrossRef]
- Fenaux, P.; Mufti, G.J.; Hellstrom-Lindberg, E.; Santini, V.; Finelli, C.; Giagounidis, A.; Schoch, R.; Gattermann, N.; Sanz, G.; List, A.; et al. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: A randomised, open-label, phase III study. Lancet Oncol. 2009, 10, 223–232. [Google Scholar] [CrossRef]

| Characteristic | Study Cohort | P-value (for Recurrence) |
|---|---|---|
| Num. | 159 | |
| Mean age (± STD) | 62 ± 13 years | 0.3 |
| Male / Female | 105/54 | 0.4 |
| Tobacco exposure | 0.4 | |
| Num. (%) | 82 (51%) | |
| Av. Pack/year | 47 | |
| Alcohol consumption (%) | 101 (63%) | 0.01 |
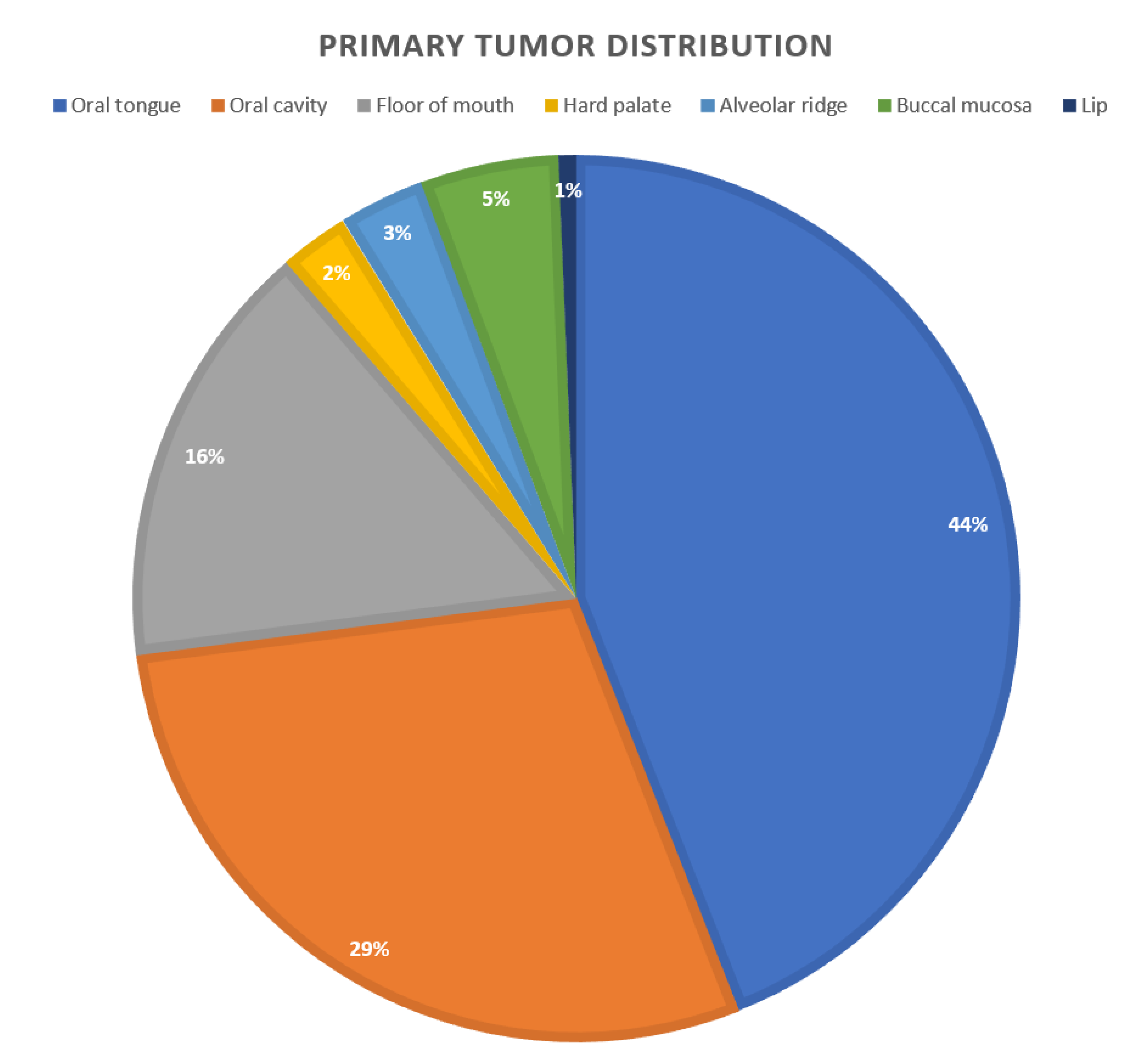
| Primary Tumor Site (%) | 0.03 | |
| Oral tongue | 70 (44%) | |
| Floor of mouth | 25 (15%) | |
| Buccal Mucosa | 7 (4%) | |
| Alveolar ridge | 4 (2%) | |
| Hard Palate | 4 (2%) | |
| Lip | 1 (0.6%) | |
| Oral Cavity * | 25 (15%) | |
| p N staging (by H&E) | 0.4 | |
| N0 (%) | 81 (50%) | |
| N1 (%) | 35 (22%) | |
| N2a (%) | 2 (1%) | |
| N2b (%) | 20 (12%) | |
| N2c (%) | 12 (7%) | |
| N3 (%) | 1 (0.6%) | |
| pT staging | 0.05 | |
| T1 (%) | 9 (5%) | |
| T2 (%) | 54 (33%) | |
| T3 (%) | 45 (28%) | |
| T4a (%) | 50 (31%) | |
| T4b (%) | 1 (0.6%) | |
| TNM staging ** | 0.7 | |
| Stage 1 (%) | 7 (4%) | |
| Stage 2 (%) | 40 (25%) | |
| Stage 3 (%) | 41 (26%) | |
| Stage 4a (%) | 69 (43%) | |
| Stage 4b (%) | 2 (1%) | |
| Surgical Margins status | 0.04 | |
| Negative margins (%) | 126 (79%) | |
| Positive margins (%) | 10 (6%) | |
| Close margins (%) | 16 (10%) | |
| Overall survival (months) | 32 months | 0.01 |
| Gene | P-value | Difference | Cluster |
|---|---|---|---|
| ATP1A4 | 1.57E-51 | 0.21275 | 1 |
| MUC13 | 1.45E-37 | 0.20674 | 1 |
| PWRN1 | 2.34E-37 | 0.20661 | 1 |
| MIR494 | 4.71E-37 | 0.23066 | 1 |
| C3ORF34 | 6.24E-36 | 0.28199 | 1 |
| CA5A | 6.78E-36 | 0.23976 | 1 |
| RASA3 | 2.53E-35 | 0.27976 | 1 |
| NFATC1 | 7.35E-35 | 0.24022 | 1 |
| ATP1A4 | 1.57E-51 | 0.21275 | 1 |
| MUC13 | 1.45E-37 | 0.20674 | 1 |
| NIT2 | 3.24E-62 | −0.3497 | 2 |
| FAM55C | 4.10E-62 | −0.2945 | 2 |
| C17ORF75 | 1.37E-60 | −0.2585 | 2 |
| ADAMTS10 | 3.23E-58 | −0.2637 | 2 |
| HES6 | 2.66E-56 | −0.2276 | 2 |
| BLOC1S1 | 6.73E-56 | −0.2398 | 2 |
| GJA4 | 3.68E-55 | −0.2762 | 2 |
| ZC3H12D | 4.33E-55 | −0.232 | 2 |
| EMX1 | 7.11E-54 | −0.2292 | 2 |
| MYO7A | 1.52E-53 | −0.4031 | 2 |
| C11ORF49 | 2.68E-48 | 0.24034 | 3 |
| HLA−L | 2.73E-48 | 0.31546 | 3 |
| ANKRD11 | 3.18E−48 | −0.251 | 3 |
| RGS17 | 2.04E-43 | 0.26871 | 3 |
| LOC441869 | 2.34E-43 | 0.22858 | 3 |
| SLC22A3 | 2.24E-42 | 0.22055 | 3 |
| HIVEP2 | 5.94E-41 | −0.2035 | 3 |
| CXXC5 | 8.96E-41 | 0.20011 | 3 |
| FOXN3 | 1.94E-40 | 0.27933 | 3 |
| BDKRB1 | 2.53E-40 | 0.2203 | 3 |
| PNMAL2 | 4.20E-40 | 0.3468 | 4 |
| RGS7BP | 5.74E-38 | −0.1932 | 4 |
| GCKR | 8.15E-36 | 0.25594 | 4 |
| PAX7 | 1.77E-33 | 0.34096 | 4 |
| IL2RA | 2.05E-32 | 0.25151 | 4 |
| SHC2 | 1.03E-29 | −0.1744 | 4 |
| LTA | 2.97E-29 | 0.16822 | 4 |
| PRRX2 | 3.59E-29 | 0.17614 | 4 |
| CCL24 | 1.17E-28 | 0.35067 | 4 |
| ODZ2 | 2.75E-28 | 0.28822 | 4 |
| ASAP1 | 1.37E-50 | 0.25071 | 5 |
| AGPAT4 | 6.80E-44 | 0.2505 | 5 |
| ASAP2 | 7.60E-40 | 0.27287 | 5 |
| ATG9B | 1.60E-34 | −0.2079 | 5 |
| ARPC1B | 1.96E-30 | −0.2608 | 5 |
| APBB2 | 2.50E-30 | −0.2005 | 5 |
| ARSG | 1.54E-29 | −0.2827 | 5 |
| BHLHE40 | 1.01E-22 | −0.3006 | 5 |
| ANKH | 1.15E-22 | 0.3368 | 5 |
| C3ORF1 | 2.62E-22 | −0.3024 | 5 |
| FOXN3 | 6.42E-39 | −0.58665 | 6 |
| BASP1 | 6.65E-37 | 0.20106 | 6 |
| ANKRD11 | 4.28E-34 | 0.214 | 6 |
| BIVM | 4.21E-33 | −0.2719 | 6 |
| BCL11A | 6.62E-31 | −0.20825 | 6 |
| CCDC88B | 6.10E-30 | 0.19286 | 6 |
| C7ORF20 | 8.42E-28 | 0.22003 | 6 |
| ABCA13 | 3.15E-27 | −0.248 | 6 |
| CAPN2 | 2.05E-26 | −0.2111 | 6 |
| LHFPL2 | 1.58E-77 | −0.2262 | 7 |
| PAK6 | 4.20E-63 | −0.2863 | 7 |
| SESN3 | 1.13E-52 | −0.213 | 7 |
| LOC728743 | 1.75E-41 | −0.1538 | 7 |
| GNG3 | 8.10E-38 | −0.1653 | 7 |
| CHRNE | 1.70E-35 | −0.2985 | 7 |
| PIK3R1 | 2.38E-34 | −0.1491 | 7 |
| LOC150568 | 6.66E-31 | 0.14291 | 7 |
| PPIE | 8.88E-31 | −0.1251 | 7 |
| MEF2B | 5.36E-26 | −0.1208 | 7 |
| Cluster | Num. (%) | Mean Age (years) | M/F Ratio | Smoking (%) | Alcohol |
|---|---|---|---|---|---|
| 1 | 29 (18%) | 65.44 | 19/9 | 12 (43%) | 18 (64%) |
| 2 | 21 (13%) | 55.47 | 17/5 | 10 (45%) | 16 (72%) |
| 3 | 46 (30%) | 67.55 | 26/20 | 21 (45%) | 27 (59%) |
| 4 | 21 (13%) | 65.95 | 18/3 | 7 (33%) | 14 (67%) |
| 5 | 2 (1%) | 58 | 2/0 | 1 (50%) | 2 (100%) |
| 6 | 34 (21%) | 54.52 | 19/15 | 22 (65%) | 19 (56%) |
| 7 | 2 (1%) | 65.66 | 2/0 | 2 (100%) | 2 (100%) |
| Cluster | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| p T staging: | |||||||
| T1 | 4 (14%) | 1 (4%) | 1 (2%) | 2 (9%) | 0 | 0 | 0 |
| T2 | 10(35%) | 8 (36%) | 12 (26%) | 7 (33%) | 0 | 16 (47%) | 0 |
| T3 | 5 (18%) | 5 (23%) | 18 (39%) | 5 (24%) | 1 (50%) | 8 (24%) | 1 (50%) |
| T4a | 9 (32%) | 8 (36%) | 14 (30%) | 7 (33%) | 1 (50%) | 10 (30%) | 1 (50%) |
| T4b | 0 | 0 | 1 (2%) | 0 | 0 | 0 | 0 |
| p N staging: | |||||||
| N1 | 9 (40%) | 4 (18%) | 8 (17%) | 3 (14%) | 0 | 10 (29%) | 0 |
| N2 | 8 (27%) | 6 (27%) | 11 (24%) | 5 (24%) | 1 (50%) | 6 (18%) | 2 (100%) |
| N3 | 0 | 0 | 1 (2%) | 0 | 0 | 0 | 0 |
| TNM | |||||||
| Stage I | 4 (14%) | 1 (4%) | 0 | 8 (38%) | 0 | 0 | 0 |
| Stage II | 3 (10%) | 7 (32%) | 11 (24%) | 6 (28%) | 0 | 12 (35%) | 0 |
| Stage III | 6 (21%) | 4 (18%) | 13 (28%) | 5 (24%) | 1 (50%) | 9 (26%) | 0 |
| Stage IVa | 15 (54%) | 10 (45%) | 20 (44%) | 0 | 1 (50%) | 13 (38%) | 2 (100%) |
| Stage IVb | 0 | 0 | 2 (4%) | 0 | 0 | 0 | 0 |
| PNI | |||||||
| Yes | 16 (57%) | 6 (27%) | 21 (45%) | 10 (48%) | 1 (50%) | 19 (56%) | 2 (100%) |
| No | 7 (25%) | 11 (50%) | 18 (39%) | 6 (29 %) | 1 (50%) | 10 (29%) | 0 |
| Primary tumor site | |||||||
| Oral tongue | 16 (57%) | 11 (50%) | 23 (50%) | 8 (38%) | 1 (50%) | 21 (62%) | 0 |
| Floor of mouth | 3 (10%) | 3 (13%) | 8 (17%) | 5 (24%) | 0 | 4 (12%) | 0 |
| Hard palate | 3 (10%) | 0 | 1 (2%) | 0 | 0 | 0 | 2 (100%) |
| Alveolar ridge | 2 (7%) | 0 | 1 (2%) | 0 | 0 | 1 (3%) | 0 |
| Buccal mucosa | 0 | 2 (9%) | 3 (6%) | 1 (5%) | 1 (50%) | 2 (6%) | 0 |
| Lip | 0 | 0 | 0 | 1 (5%) | 0 | 0 | 0 |
| Oral cavity | 4 (14%) | 6 (27%) | 10 (21%) | 6 (28%) | 0 | 6 (17%) | 0 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghantous, Y.; Nashef, A.; Abu-Elnaaj, I. Epigenetic Alterations Associated with the Overall Survival and Recurrence Free Survival among Oral Squamous Cell Carcinoma Patients. J. Clin. Med. 2020, 9, 1035. https://doi.org/10.3390/jcm9041035
Ghantous Y, Nashef A, Abu-Elnaaj I. Epigenetic Alterations Associated with the Overall Survival and Recurrence Free Survival among Oral Squamous Cell Carcinoma Patients. Journal of Clinical Medicine. 2020; 9(4):1035. https://doi.org/10.3390/jcm9041035
Chicago/Turabian StyleGhantous, Yasmen, Aysar Nashef, and Imad Abu-Elnaaj. 2020. "Epigenetic Alterations Associated with the Overall Survival and Recurrence Free Survival among Oral Squamous Cell Carcinoma Patients" Journal of Clinical Medicine 9, no. 4: 1035. https://doi.org/10.3390/jcm9041035
APA StyleGhantous, Y., Nashef, A., & Abu-Elnaaj, I. (2020). Epigenetic Alterations Associated with the Overall Survival and Recurrence Free Survival among Oral Squamous Cell Carcinoma Patients. Journal of Clinical Medicine, 9(4), 1035. https://doi.org/10.3390/jcm9041035






