The Wearable Cardioverter-Defibrillator: Experience in 153 Patients and a Long-Term Follow-Up
Abstract
1. Introduction
2. Methods
2.1. Patient Recruitment
2.2. The Wearable Cardioverter-Defibrillator (WCD)
2.3. Baseline and Follow-Up Data Collection
2.4. Endpoints and Definitions
2.5. Statistics
3. Results
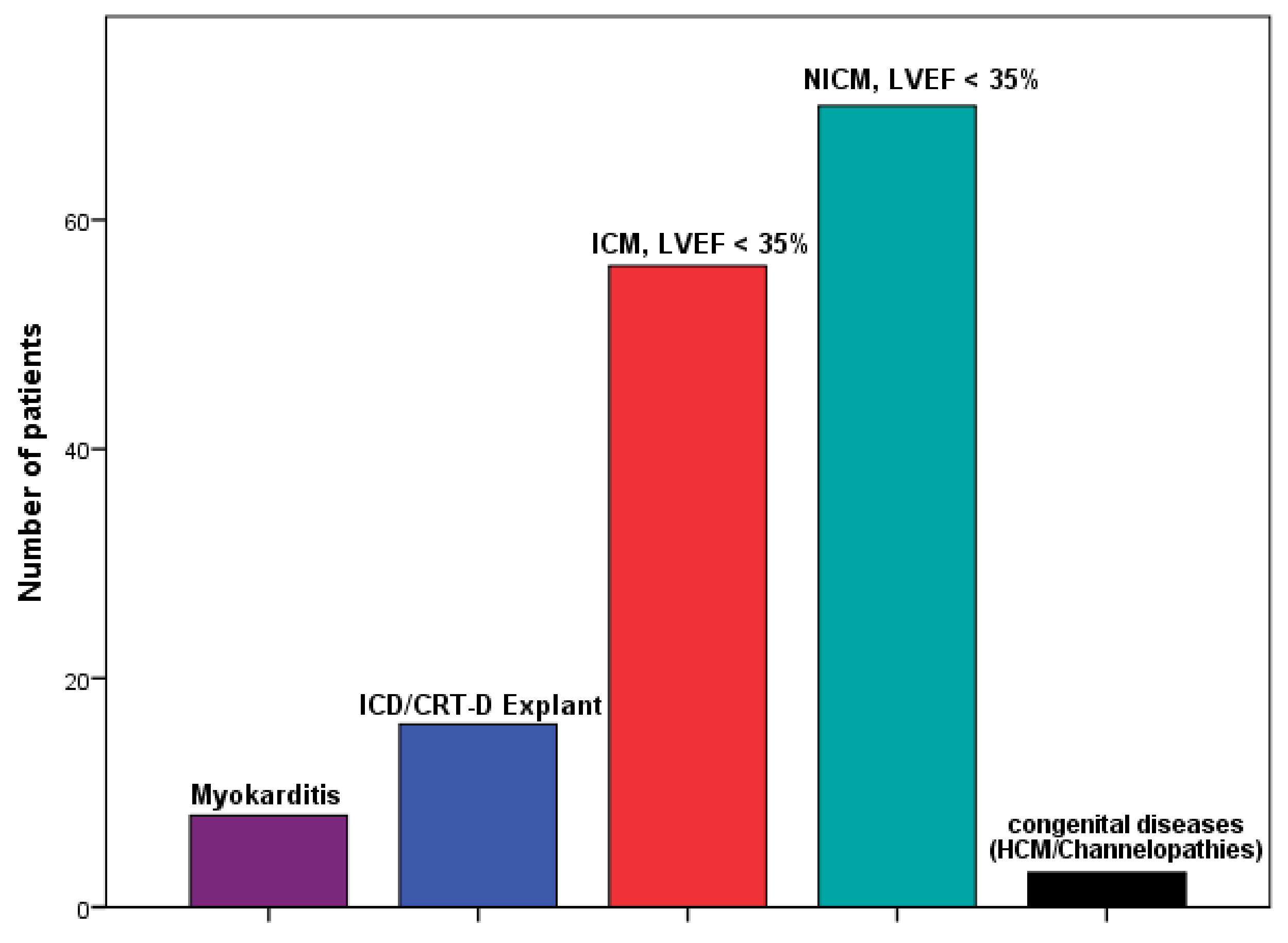
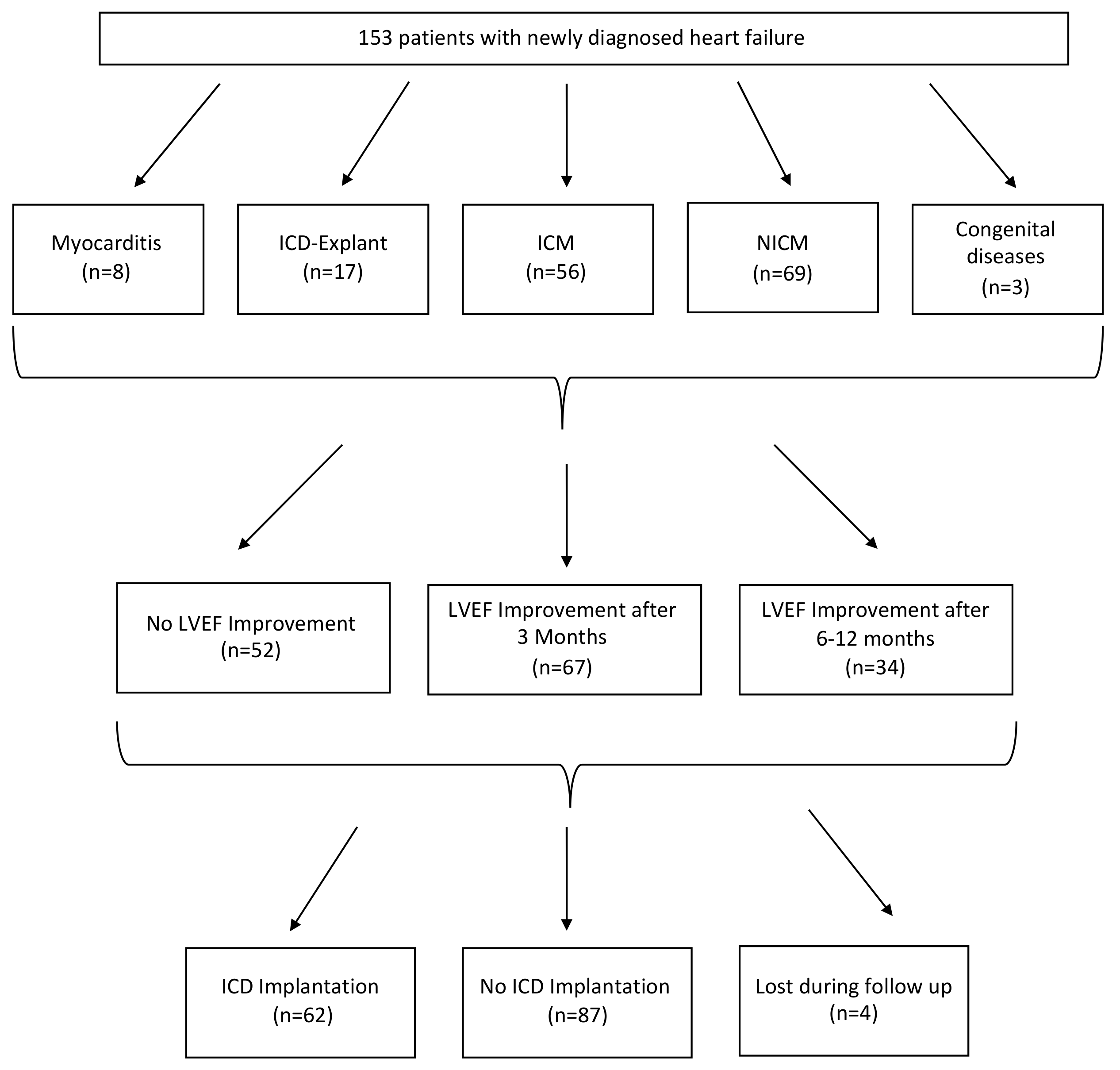
3.1. Patients Baseline Characteristics
3.2. WCD Data
3.3. Long-Term Follow-Up
3.3.1. Echocardiography Data
3.3.2. ECG Data
3.3.3. Rhythm
3.3.4. Laboratory Value
3.3.5. Device Implantation After WCD Use
3.3.6. Arrhythmic Events During Long-Term Follow-Up
3.3.7. All-Cause Mortality
3.3.8. Rehospitalizations during long term follow up
4. Discussion
Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Priori, S.G.; Lundqvist, C.B. European Society of Cardiology Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death summarized by co-chairs. Eur. Heart J. 2015, 36, 2757–2762. [Google Scholar]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Rev. Esp. Cardiol. (Engl. Ed.) 2016, 69, 1167. [Google Scholar]
- Adabag, S.; Therneau, T.M.; Gersh, B.J.; Weston, S.A.; Roger, V.L.; Roger, V.L. Sudden Death After Myocardial Infarction. JAMA 2008, 300, 2022–2029. [Google Scholar] [CrossRef]
- Burns, R.J.; Gibbons, R.J.; Yi, Q.; Roberts, R.S.; Miller, T.D.; Schaer, G.L.; Anderson, J.L.; Yusuf, S. CORE Study Investigators The relationships of left ventricular ejection fraction, end-systolic volume index and infarct size to six-month mortality after hospital discharge following myocardial infarction treated by thrombolysis. J. Am. Coll. Cardiol. 2002, 39, 30–36. [Google Scholar] [CrossRef]
- Solomon, S.D.; Zelenkofske, S.; McMurray, J.J.; Finn, P.V.; Velazquez, E.; Ertl, G.; Harsanyi, A.; Rouleau, J.L.; Maggioni, A.; Kober, L.; et al. Sudden death in patients with myocardial infarction and left ventricular dysfunction, heart failure, or both. N. Engl. J. Med. 2005, 352, 2581–2588. [Google Scholar] [CrossRef]
- Steinbeck, D.M.G.; Andresen, D.; Seidl, K.; Brachmann, J.; Hoffmann, E.; Wojciechowski, D.; Kornacewicz-Jach, Z.; Sredniawa, B.; Lupkovics, G.; Hofgartner, F.; et al. Defibrillator Implantation Early after Myocardial Infarction. N. Engl. J. Med. 2009, 361, 1427–1436. [Google Scholar] [CrossRef]
- Hohnloser, S.H.; Kuck, K.H.; Dorian, P.; Roberts, R.S.; Hampton, J.R.; Hatala, R.; Fain, E.; Gent, M.; Connolly, S. Prophylactic Use of an Implantable Cardioverter–Defibrillator after Acute Myocardial Infarction. N. Engl. J. Med. 2004, 351, 2481–2488. [Google Scholar] [CrossRef]
- Duncker, D.; König, T.; Hohmann, S.; Bauersachs, J.; Veltmann, C. Avoiding Untimely Implantable Cardioverter/Defibrillator Implantation by Intensified Heart Failure Therapy Optimization Supported by the Wearable Cardioverter/Defibrillator—The PROLONG Study. J. Am. Heart Assoc. 2017, 6. [Google Scholar] [CrossRef]
- Duncker, D.; König, T.; Hohmann, S.; Bauersachs, J.; Veltmann, C. Ventricular arrhythmias in patients with newly diagnosed nonischemic cardiomyopathy: Insights from the PROLONG study. Clin. Cardiol. 2017, 40, 586–590. [Google Scholar] [CrossRef]
- Duncker, D.; Haghikia, A.; König, T.; Hohmann, S.; Gutleben, K.-J.; Westenfeld, R.; Oswald, H.; Klein, H.; Bauersachs, J.; Hilfiker-Kleiner, D.; et al. Risk for ventricular fibrillation in peripartum cardiomyopathy with severely reduced left ventricular function-value of the wearable cardioverter/defibrillator. Eur. J. Heart Fail. 2014, 16, 1331–1336. [Google Scholar] [CrossRef]
- Elkayam, U. Clinical Characteristics of Peripartum Cardiomyopathy in the United States: Diagnosis, prognosis, and management. J. Am. Coll. Cardiol. 2011, 58, 659–670. [Google Scholar] [CrossRef]
- McNamara, D.M.; Elkayam, U.; Alharethi, R.; Damp, J.; Hsich, E.; Ewald, G.; Modi, K.; Alexis, J.D.; Ramani, G.V.; Semigran, M.J.; et al. Clinical Outcomes for Peripartum Cardiomyopathy in North America: Results of the IPAC Study (Investigations of Pregnancy-Associated Cardiomyopathy). J. Am. Coll. Cardiol. 2015, 66, 905–914. [Google Scholar] [CrossRef]
- Pillarisetti, J.; Kondur, A.; Alani, A.; Reddy, M.; Reddy, M.; Vacek, J.; Weiner, C.P.; Ellerbeck, E.; Schreiber, T.; Lakkireddy, D. Peripartum Cardiomyopathy: Predictors of recovery and current state of implantable cardioverter-defibrillator use. J. Am. Coll. Cardiol. 2014, 63, 2831–2839. [Google Scholar] [CrossRef]
- Bauersachs, J.; Arrigo, M.; Hilfiker-Kleiner, D.; Veltmann, C.; Coats, A.J.; Crespo-Leiro, M.G.; De Boer, R.A.; Van Der Meer, P.; Maack, C.; Mouquet, F.; et al. Current management of patients with severe acute peripartum cardiomyopathy: Practical guidance from the Heart Failure Association of the European Society of Cardiology Study Group on peripartum cardiomyopathy. Eur. J. Heart Fail. 2016, 18, 1096–1105. [Google Scholar] [CrossRef]
- Køber, L.; Thune, J.J.; Nielsen, O.W.; Haarbo, J.; Videbæk, L.; Korup, E.; Jensen, G.; Hildebrandt, P.; Steffensen, F.H.; Bruun, N.E.; et al. Defibrillator Implantation in Patients with Nonischemic Systolic Heart Failure. N. Engl. J. Med. 2016, 375, 1221–1230. [Google Scholar] [CrossRef]
- Chung, M.K.; Szymkiewicz, S.J.; Shao, M.; Niebauer, M.J.; Lindsay, B.D.; Tchou, P.J. Aggregate national experience with the wearable cardioverter-defibrillator: Event rates, compliance, and survival. J. Am. Coll. Cardiol. 2010, 55, 194–203. [Google Scholar] [CrossRef]
- Kutyifa, V.; Moss, A.J.; Klein, H.; Biton, Y.; McNitt, S.; MacKecknie, B.; Zareba, W.; Goldenberg, I. Use of the wearable cardioverter defibrillator in high-risk cardiac patients: Data from the Prospective Registry of Patients Using the Wearable Cardioverter Defibrillator (WEARIT-II Registry). Circulation 2015, 132, 1613–1619. [Google Scholar] [CrossRef]
- Wäßnig, N.K.; Günther, M.; Quick, S.; Pfluecke, C.; Rottstädt, F.; Szymkiewicz, S.J.; Ringquist, S.; Strasser, R.H.; Speiser, U. Experience With the Wearable Cardioverter-Defibrillator in Patients at High Risk for Sudden Cardiac Death. Circulation 2016, 134, 635–643. [Google Scholar] [CrossRef]
- Feldman, A.M.; Klein, H.; Tchou, P.; Murali, S.; Hall, W.J.; Mancini, N.; Boehmer, J.; Harvey, M.; Heilman, M.S.; Szymkiewicz, S.J.; et al. Use of a Wearable Defibrillator in Terminating Tachyarrhythmias in Patients at High Risk for Sudden Death:. Results of WEARIT/BIROAD. Pacing Clin. Electrophysiol. 2004, 27, 4–9. [Google Scholar] [CrossRef]
- Kutyifa, V.; Moss, A.J.; Klein, H.; McNitt, S.; Zareba, W.; Goldenberg, I. One-year follow-up of the prospective registry of patients using the wearable defibrillator (WEARIT-II Registry). Pacing Clin. Electrophysiol. 2018, 41, 1307–1313. [Google Scholar] [CrossRef]
- Olgin, J.E.; Pletcher, M.J.; Vittinghoff, E.; Wranicz, J.; Malik, R.; Morin, D.P.; Zweibel, S.; Buxton, A.E.; Elayi, C.S.; Chung, E.H.; et al. Wearable Cardioverter-Defibrillator after Myocardial Infarction. N. Engl. J. Med. 2018, 379, 1205–1215. [Google Scholar] [CrossRef] [PubMed]
- Klein, H.; Goldenberg, I.; Moss, A.J. Risk stratification for implantable cardioverter defibrillator therapy: The role of the wearable cardioverter-defibrillator. Eur. Heart J. 2013, 34, 2230–2242. [Google Scholar] [CrossRef] [PubMed]
- Swedberg, K.; Komajda, M.; Böhm, M.; Borer, J.S.; Ford, I.; Dubost-Brama, A.; Lerebours, G.; Tavazzi, L. Ivabradine and outcomes in chronic heart failure (SHIFT): A randomised placebo-controlled study. Lancet 2010, 376, 875–885. [Google Scholar] [CrossRef]
- Auricchio, A.; Klein, H.; Geller, C.J.; Reek, S.; Heilman, M.; Szymkiewicz, S.J. Clinical efficacy of the wearable cardioverter-defibrillator in acutely terminating episodes of ventricular fibrillation. Am. J. Cardiol. 1998, 81, 1253–1256. [Google Scholar] [CrossRef]
- Shen, L.; Jhund, P.S.; McMurray, J.J.V. Declining Risk of Sudden Death in Heart Failure. N. Engl. J. Med. 2017, 377, 1794–1795. [Google Scholar] [CrossRef]
- Singh, M.; Wang, N.C.; Jain, S.K.; Voigt, A.; Saba, S.; Adelstein, E.C. Utility of the Wearable Cardioverter-Defibrillator in Patients With Newly Diagnosed Cardiomyopathy: A Decade-Long Single-Center Experience. J. Am. Coll. Cardiol. 2015, 66, 2607–2613. [Google Scholar] [CrossRef]
- Beiert, T.; Malotki, R.; Kraemer, N.; Stöckigt, F.; Linhart, M.; Nickenig, G.; Schrickel, J.W.; Andrié, R.P. A real world wearable cardioverter defibrillator experience—Very high appropriate shock rate in ischemic cardiomyopathy patients at a European single-center. J. Electrocardiol. 2017, 50, 603–609. [Google Scholar] [CrossRef]
| Variables | (n = 153) |
|---|---|
| Demographics | |
| Age, mean ± SD *(years) | 60 ± 14 |
| Female, n (%) | 35 (23) |
| Indication for WCD use, n (%) | |
| Myocarditis | 8 (5) |
| ICD */CRT-D * Explant | 16 (10) |
| ICM *, LVEF * < 35% | 56 (37) |
| NICM *, LVEF < 35% | 70 (46) |
| Congenital diseases | 3 (2) |
| Clinic parameter | |
| Cadiogenic shock at event, n (%) | 13 (8) |
| Pulmonary edema, n (%) | 14 (9) |
| Days of hospitalization, mean ± SD | 15.8 ± 11.9 |
| Former significant VT */VF * prior to WCD use, n (%) | 26 (17) |
| Medical history, n (%) | |
| Former CIED explanted | 7 (5) |
| History of CAD * | 61 (40) |
| History of myocardial infarction | 48 (31) |
| History of CABG * | 11 (7) |
| Moderately severe CKD/Dialysis * | 20 (13) |
| History of CHF * | 23 (15) |
| History of Atrial fibrillation/flutter | 37 (24) |
| History of TIA/stroke * | 9 (6) |
| Cardiovascular Risk Factors, n (%) | |
| Smoking | 67 (44) |
| Diabetes mellitus | 31 (20) |
| Overweight (BMI > 25 kg/m2) * | 106 (69) |
| Lipidemia | 67 (44) |
| Hypertension | 87 (57) |
| COPD * | 16 (11) |
| Family history of cardiovascular disease | 42 (28) |
| Variables | (n = 153) |
|---|---|
| Wear time of WCD | |
| Average wear time, h/day | 21.45 ± 3.52 |
| Wear days, mean ± SD * | 65.1 ± 42 |
| Wear days, Median (IQR *) | 60 (30–91) |
| WCD Shocks | |
| Appropriate shock, n (%) | 6 (4) |
| Inappropriate shock, n (%) | 1 (0.7) |
| Number of inhibitions, mean ± SD | 12.28 ± 33 |
| Arrhythmic episodes during WCD use (n = 153), n (%) | |
| None | 143 (94) |
| Ventricular tachycardia | 5 (3) |
| Ventricular fibrillation | 1 (0.7) |
| Others | 4 (2) |
| Reason for stopping WCD use, n (%) | |
| Improved LVEF * | 77 (50) |
| Cardiac electronic device implantation | 56 (37) |
| Incompliance | 12 (8) |
| Death 1 | 2 (1) |
| Decision pending | 1 (0.7) |
| Other reasons | 5 (3) |
| Echocardiography data | |
| Not changed LVEF, n (%) | 49 (32) |
| Declined LVEF, n (%) | 3 (2) |
| Improved LVEF in first 3 months, n (%) | 67 (44) |
| Improved LVEF after 6–12 months, n (%) | 34 (22) |
| Bundle Branch Block, n (%) | |
| None | 108 (71) |
| LBBB * | 25 (16) |
| RBBB * | 17 (11) |
| Sinus arrest/complete AV-Block | 2 (1) |
| Fascicular block | 1 (0.7) |
| Device implantation after WCD use, n (%) | |
| No | 87 (58) |
| Yes | 62 (42) |
| Died before implantation 1 | 2 (1) |
| Patient denied | 2 (1) |
| Device type, n (%) | |
| None | 87 (58) |
| Transvenous ICD * | 13 (9) |
| CRT-D * | 12 (8) |
| S-ICD * | 37 (24) |
| Reported shocks post device implantation, n (%) | |
| No | 54 (87) |
| Yes | 8 (13) |
| Arrhythmic episodes post device implantation, n (%) | |
| Sustained VT * | 10 (16) |
| VF * | 2 (3) |
| Non sustained VT * | 16 (26) |
| Death during follow up period, n (%) | |
| No | 134 (90) |
| Yes | 15 (10) |
| Rehospitalization over mean follow up, more than one reason possible, n (%) | |
| No | 41 (27) |
| Yes | 102 (67) |
| Unknown | 10 (7) |
| Cardiovascular cause | 84 (55) |
| Congestive heart failure | 10 (7) |
| Atrial fibrillation | 2 (1) |
| Stroke cause | 6 (4) |
| VT/VF * cause | 9 (6) |
| Any other cause | 38 (25) |
| Variables | Baseline | After 3 Months | After 6–12 Months | p Value for Comparison | |
|---|---|---|---|---|---|
| Echocardiography Data | Baseline vs. 3 months | Baseline vs. 6–12 months | |||
| LVEF *, mean ± SD * | 28.61 ± 10.15 | 36.94 ± 11.3 | 40.96 ± 12.68 | < 0.001 | < 0.001 |
| ECG Data, mean ± SD | |||||
| QRS duration (ms) | 109.81 ± 30.77 | 107.70 ± 27.53, n = 124 | 109.36 ± 28.03, n = 122 | 0.702 | 0.211 |
| QTc duration (ms) | 460.04 ± 54.47 | 445.39 ± 40.86, n = 124 | 449.55 ± 39.92, n = 122 | 0.003 | 0.182 |
| PQ-interval (ms) | 165.13 ± 26.13 | 169.86 ± 30.76, n = 124 | 164.41 ± 25.88, n = 122 | 0.946 | 0.797 |
| Rhythm, n (%) | |||||
| Sinus Rhythm | 133 (87) | 105/124 (85) | 99/122 (81) | 0.639 | 0.127 |
| AV-Block I | 13 (9) | 7/124 (6) | 5/122 (4) | 0.198 | 0.071 |
| Pacemaker Rhythm | 4 (3) | 8/124 (7) | 15/122 (13) | 0.06 | <0.01 |
| Ventricular Fibrillation | 1 (0.7) | 0/124 (0) | 0/122 (0) | ||
| Atrial Fibrillation | 12 (8) | 10/124 (8) | 8/122 (7) | 0.416 | 1.000 |
| Laboratory values (ng/L) | |||||
| Elevated Pro-BNP, n (%) | 84 (55) | 65 (43) | 43 (28) | 0.039 | 0.001 |
| BNP, mean ± SD, (median) | 7732.63 ± 7148.99 | 2099.03 ± 3688.02 | 2542.28 ± 8987.36 | 0.011 | 0.283 |
| Death After | ICD Implantation, n = 62, (%) | No ICD, n = 87, (%) | p-Value 1 |
|---|---|---|---|
| 1 year | 1 (2) | 4 (5) | 0.40 |
| 2 years | 1 (2) | 5 (6) | 0.40 |
| 3 years | 5 (8) | 5 (6) | 0.74 |
| 4 years | 8 (13) | 5 (6) | 0.15 |
| During WCD use | 0 (0) | 2/91 (2) | 0.51 |
| overall | 8 (13) | 7 (8) | 0.48 |
| Death After | ICM, n = 56 (%) | NCIM, n = 70 (%) | Others, n = 23 (%) | All, n = 149 (%) | p-Value 1 |
|---|---|---|---|---|---|
| 1 Year | 2 (4) | 4 (6) | 1 (4) | 7 (5) | 0.69 |
| 2 Years | 3 (5) | 4 (6) | 1 (4) | 8 (5) | 1.00 |
| 3 Years | 6 (11) | 4 (6) | 1 (4) | 11 (7) | 0.34 |
| 4 Years | 7 (13) | 4 (6) | 2 (9) | 13 (9) | 0.21 |
| During WCD Use | 1 (2) | 0 (0) | 1 (4) | 2 (1) | 0.44 |
| Overall | 8 (14) | 4 (6) | 3 * (13) | 15 (10) | 0.13 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosenkaimer, S.L.; El-Battrawy, I.; Dreher, T.C.; Gerhards, S.; Röger, S.; Kuschyk, J.; Borggrefe, M.; Akin, I. The Wearable Cardioverter-Defibrillator: Experience in 153 Patients and a Long-Term Follow-Up. J. Clin. Med. 2020, 9, 893. https://doi.org/10.3390/jcm9030893
Rosenkaimer SL, El-Battrawy I, Dreher TC, Gerhards S, Röger S, Kuschyk J, Borggrefe M, Akin I. The Wearable Cardioverter-Defibrillator: Experience in 153 Patients and a Long-Term Follow-Up. Journal of Clinical Medicine. 2020; 9(3):893. https://doi.org/10.3390/jcm9030893
Chicago/Turabian StyleRosenkaimer, Stephanie L., Ibrahim El-Battrawy, Tobias C. Dreher, Stefan Gerhards, Susanne Röger, Jürgen Kuschyk, Martin Borggrefe, and Ibrahim Akin. 2020. "The Wearable Cardioverter-Defibrillator: Experience in 153 Patients and a Long-Term Follow-Up" Journal of Clinical Medicine 9, no. 3: 893. https://doi.org/10.3390/jcm9030893
APA StyleRosenkaimer, S. L., El-Battrawy, I., Dreher, T. C., Gerhards, S., Röger, S., Kuschyk, J., Borggrefe, M., & Akin, I. (2020). The Wearable Cardioverter-Defibrillator: Experience in 153 Patients and a Long-Term Follow-Up. Journal of Clinical Medicine, 9(3), 893. https://doi.org/10.3390/jcm9030893





