Assessment of the Short-Term Effects after High-Inductive Electromagnetic Stimulation of Pelvic Floor Muscles: A Randomized, Sham-Controlled Study
Abstract
1. Introduction
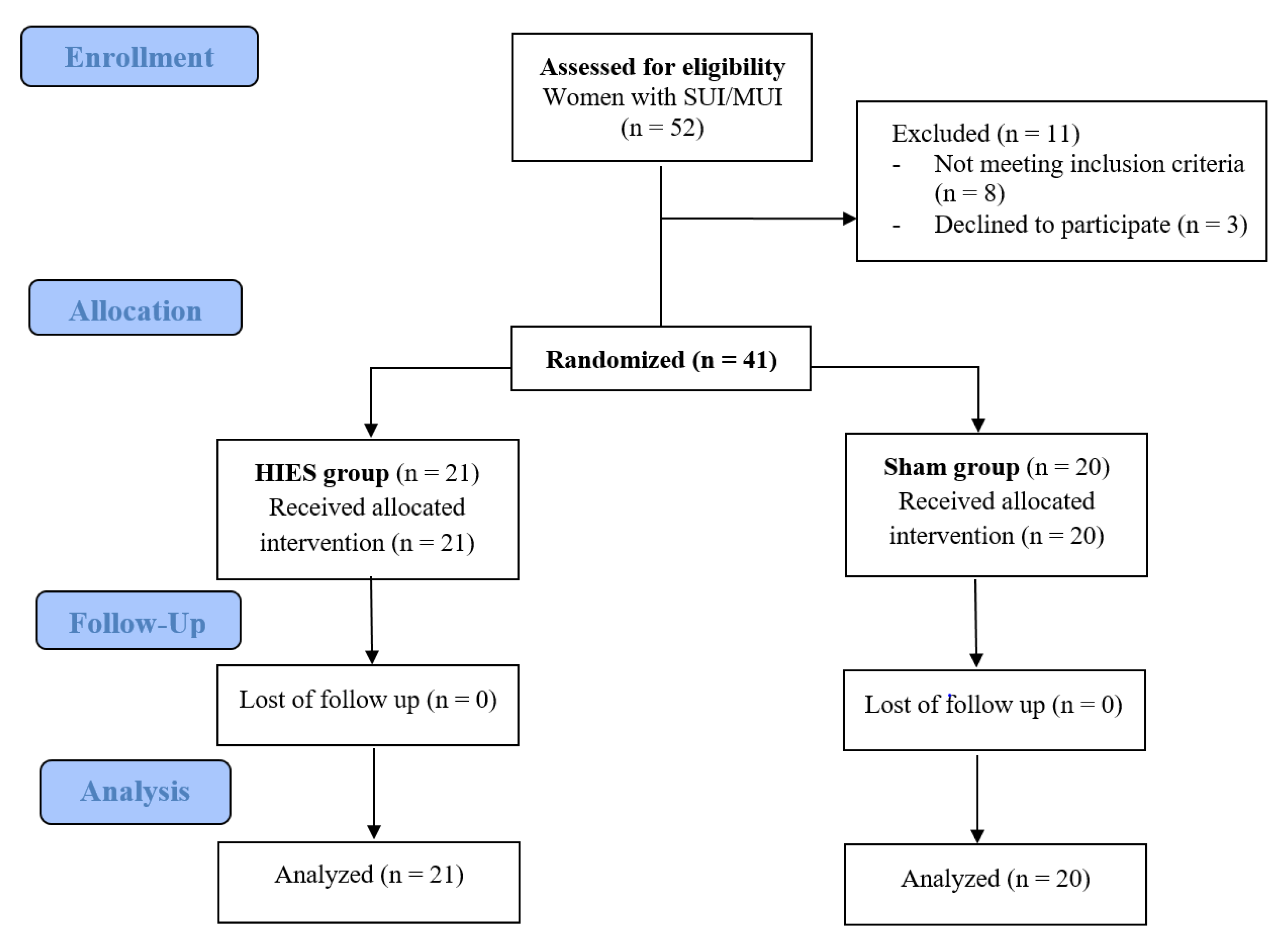
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Aguilar-Zavala, H.; Pérez-Luque, E.L.; Luna-Martínez, F.; Bassol-Mayagoitia, S.; Canto-de-Cetina, T.; López-Conesa, M.; Malacara, J.M. Symptoms at postmenopause: Genetic and psychosocial factors. Menopause 2012, 19, 1140–1145. [Google Scholar] [CrossRef]
- Lee, J. The menopause: Effects on the pelvic floor, symptoms and treatment options. Nurs. Times 2009, 105, 22–24. [Google Scholar]
- Schnatz, P.F.; Banever, A.E.; Greene, J.F.; O’Sullivan, D.M. Pilot study of menopause symptoms in a clinic population. Menopause 2005, 12, 623–629. [Google Scholar] [CrossRef]
- Menezes, M.; Pereira, M.; Hextall, A. Predictors of female urinary incontinence at midlife and beyond. Maturitas 2010, 65, 167–171. [Google Scholar] [CrossRef]
- Palacios, S.; Henderson, V.W.; Siseles, N.; Tan, D.; Villaseca, P. Age of menopause and impact of climacteric symptoms by geographical region. Climacteric J. Int. Menopause Soc. 2010, 13, 419–428. [Google Scholar] [CrossRef]
- Bø, K. Evidence-Based Physical Therapy for the Pelvic Floor: Bridging Science and Clinical Practice, 1e, 1st ed.; Churchill Livingstone: Edinburg, TX, USA, 2007; ISBN 978-0-443-10146-5. [Google Scholar]
- Nygaard, C.C.; Betschart, C.; Hafez, A.A.; Lewis, E.; Chasiotis, I.; Doumouchtsis, S.K. Impact of menopausal status on the outcome of pelvic floor physiotherapy in women with urinary incontinence. Int. Urogynecol. J. 2013, 24, 2071–2076. [Google Scholar] [CrossRef]
- Aukee, P.; Penttinen, J.; Airaksinen, O. The effect of aging on the electromyographic activity of pelvic floor muscles. A comparative study among stress incontinent patients and asymptomatic women. Maturitas 2003, 44, 253–257. [Google Scholar] [CrossRef]
- Ayeleke, R.O.; Hay-Smith, E.J.C.; Omar, M.I. Pelvic floor muscle training added to another active treatment versus the same active treatment alone for urinary incontinence in women. Cochrane Database Syst. Rev. 2013, 11, CD010551. [Google Scholar]
- Balmforth, J.R.; Mantle, J.; Bidmead, J.; Cardozo, L. A prospective observational trial of pelvic floor muscle training for female stress urinary incontinence. BJU Int. 2006, 98, 811–817. [Google Scholar] [CrossRef]
- Goldberg, R.P.; Sand, P.K. Electromagnetic pelvic floor stimulation: Applications for the gynecologist. Obstet. Gynecol. Surv. 2000, 55, 715–720. [Google Scholar] [CrossRef]
- Przedborska, A.; Misztal, M.; Raczkowski, J.W. Assessment of the Therapeutic Effectiveness of Deep Electromagnetic Stimulation in Patients with Chronic Low Back Pain. Ortop. Traumatol. Rehabil. 2015, 17, 531–541. [Google Scholar] [CrossRef]
- Silantyeva, E.; Zarkovic, D.; Astafeva, E.; Soldatskaia, R.; Orazov, M.; Belkovskaya, M.; Kurtser, M. Academician of the Russian Academy of Sciences A Comparative Study on the Effects of High-Intensity Focused Electromagnetic Technology and Electrostimulation for the Treatment of Pelvic Floor Muscles and Urinary Incontinence in Parous Women: Analysis of Posttreatment Data. Female Pelvic Med. Reconstr. Surg. 2019. [Google Scholar]
- Samuels, J.B.; Pezzella, A.; Berenholz, J.; Alinsod, R. Safety and Efficacy of a Non-Invasive High-Intensity Focused Electromagnetic Field (HIFEM) Device for Treatment of Urinary Incontinence and Enhancement of Quality of Life. Lasers Surg. Med. 2019, 51, 760–766. [Google Scholar] [CrossRef]
- Pereira, V.S.; Escobar, A.C.; Driusso, P. Effects of physical therapy in older women with urinary incontinence: A systematic review. Rev. Bras. Fisioter. São Carlos São Paulo Braz. 2012, 16, 463–468. [Google Scholar] [CrossRef]
- Chêne, G.; Mansoor, A.; Jacquetin, B.; Mellier, G.; Douvier, S.; Sergent, F.; Aubard, Y.; Seffert, P. Female urinary incontinence and intravaginal electrical stimulation: An observational prospective study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 170, 275–280. [Google Scholar] [CrossRef]
- Correia, G.N.; Pereira, V.S.; Hirakawa, H.S.; Driusso, P. Effects of surface and intravaginal electrical stimulation in the treatment of women with stress urinary incontinence: Randomized controlled trial. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 173, 113–118. [Google Scholar] [CrossRef]
- Joussain, C.; Denys, P. Electrical management of neurogenic lower urinary tract disorders. Ann. Phys. Rehabil. Med. 2015, 58, 245–250. [Google Scholar] [CrossRef]
- Bø, K. Pelvic floor muscle training in treatment of female stress urinary incontinence, pelvic organ prolapse and sexual dysfunction. World J. Urol. 2012, 30, 437–443. [Google Scholar] [CrossRef]
- Bø, K.; Herbert, R.D. There is not yet strong evidence that exercise regimens other than pelvic floor muscle training can reduce stress urinary incontinence in women: A systematic review. J. Physiother. 2013, 59, 159–168. [Google Scholar] [CrossRef]
- Fistonić, N.; Fistonić, I.; Guštek, Š.F.; Turina, I.S.B.; Marton, I.; Vižintin, Z.; Kažič, M.; Hreljac, I.; Perhavec, T.; Lukač, M. Minimally invasive, non-ablative Er:YAG laser treatment of stress urinary incontinence in women-a pilot study. Lasers Med. Sci. 2016, 31, 635–643. [Google Scholar] [CrossRef]
- Ogrinc, U.B.; Senčar, S.; Lenasi, H. Novel minimally invasive laser treatment of urinary incontinence in women. Lasers Surg. Med. 2015, 47, 689–697. [Google Scholar] [CrossRef]
- Mansor, M.S.F.; Abas, W.A.B.W.; Mahadi, W.N.L.W. Study of Electromagnetic Field (EMF) on the Human Muscle Activity: A Preliminary Study. In 4th Kuala Lumpur International Conference on Biomedical Engineering 2008; Osman, D.N.A.A., Ibrahim, D.F., Abas, D.W.A.B.W., Rahman, H.S.A., Ting, D.H.-N., Eds.; IFMBE Proceedings; Springer: Berlin/Heidelberg, Germany, 2008; pp. 254–257. ISBN 978-3-540-69138-9. [Google Scholar]
- Bergman, J.; Robertson, J.R.; Elia, G. Effects of a magnetic field on pelvic floor muscle function in women with stress urinary incontinence. Altern. Ther. Health Med. 2004, 10, 70–72. [Google Scholar]
- Gilling, P.J.; Wilson, L.C.; Westenberg, A.M.; McAllister, W.J.; Kennett, K.M.; Frampton, C.M.; Bell, D.F.; Wrigley, P.M.; Fraundorfer, M.R. A double-blind randomized controlled trial of electromagnetic stimulation of the pelvic floor vs sham therapy in the treatment of women with stress urinary incontinence. BJU Int. 2009, 103, 1386–1390. [Google Scholar] [CrossRef]
- Yokoyama, T.; Nishiguchi, J.; Watanabe, T.; Nose, H.; Nozaki, K.; Fujita, O.; Inoue, M.; Kumon, H. Comparative study of effects of extracorporeal magnetic innervation versus electrical stimulation for urinary incontinence after radical prostatectomy. Urology 2004, 63, 264–267. [Google Scholar] [CrossRef]
- But, I. Conservative treatment of female urinary incontinence with functional magnetic stimulation. Urology 2003, 61, 558–561. [Google Scholar] [CrossRef]
- Lo, T.-S.; Tseng, L.-H.; Lin, Y.-H.; Liang, C.-C.; Lu, C.-Y.; Pue, L.B. Effect of extracorporeal magnetic energy stimulation on bothersome lower urinary tract symptoms and quality of life in female patients with stress urinary incontinence and overactive bladder. J. Obstet. Gynaecol. Res. 2013, 39, 1526–1532. [Google Scholar] [CrossRef]
- REMED | Salus-Talent. Available online: http://remed.kr/products/pain-control/salus-talent/ (accessed on 10 June 2016).
- Ptaszkowski, K.; Zdrojowy, R.; Slupska, L.; Bartnicki, J.; Dembowski, J.; Halski, T.; Paprocka-Borowicz, M. Assessment of bioelectrical activity of pelvic floor muscles depending on the orientation of the pelvis in menopausal women with symptoms of stress urinary incontinence: Continued observational study. Eur. J. Phys. Rehabil. Med. 2017, 53, 564–574. [Google Scholar]
- Ptaszkowski, K.; Paprocka-Borowicz, M.; Słupska, L.; Bartnicki, J.; Dymarek, R.; Rosińczuk, J.; Heimrath, J.; Dembowski, J.; Zdrojowy, R. Assessment of bioelectrical activity of synergistic muscles during pelvic floor muscles activation in postmenopausal women with and without stress urinary incontinence: A preliminary observational study. Clin. Interv. Aging 2015, 10, 1521–1528. [Google Scholar] [CrossRef]
- Halski, T.; Słupska, L.; Dymarek, R.; Bartnicki, J.; Halska, U.; Król, A.; Paprocka-Borowicz, M.; Dembowski, J.; Zdrojowy, R.; Ptaszkowski, K. Evaluation of bioelectrical activity of pelvic floor muscles and synergistic muscles depending on orientation of pelvis in menopausal women with symptoms of stress urinary incontinence: A preliminary observational study. BioMed Res. Int. 2014, 2014, 274938. [Google Scholar] [CrossRef]
- Avery, K.; Donovan, J.; Peters, T.J.; Shaw, C.; Gotoh, M.; Abrams, P. ICIQ: A brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol. Urodyn. 2004, 23, 322–330. [Google Scholar] [CrossRef]
- Lim, R.; Liong, M.L.; Leong, W.S.; Khan, N.A.K.; Yuen, K.H. Magnetic stimulation for stress urinary incontinence: Study protocol for a randomized controlled trial. Trials 2015, 16, 279. [Google Scholar] [CrossRef] [PubMed]
- Galloway, N.T.; El-Galley, R.E.; Sand, P.K.; Appell, R.A.; Russell, H.W.; Carlan, S.J. Extracorporeal magnetic innervation therapy for stress urinary incontinence. Urology 1999, 53, 1108–1111. [Google Scholar] [CrossRef]
- Galloway, N.T.; El-Galley, R.E.; Sand, P.K.; Appell, R.A.; Russell, H.W.; Carlin, S.J. Update on extracorporeal magnetic innervation (EXMI) therapy for stress urinary incontinence. Urology 2000, 56, 82–86. [Google Scholar] [CrossRef]
- Morren, G.L.; Walter, S.; Lindehammar, H.; Hallböök, O.; Sjödahl, R. Evaluation of the sacroanal motor pathway by magnetic and electric stimulation in patients with fecal incontinence. Dis. Colon Rectum 2001, 44, 167–172. [Google Scholar] [CrossRef]
- Unsal, A.; Saglam, R.; Cimentepe, E. Extracorporeal magnetic stimulation for the treatment of stress and urge incontinence in women--results of 1-year follow-up. Scand. J. Urol. Nephrol. 2003, 37, 424–428. [Google Scholar] [CrossRef]
- Groenendijk, P.M.; Halilovic, M.; Chandi, D.D.; Heesakkers, J.P.F.A.; Voorham-Van Der Zalm, P.J.; Lycklama Anijeholt, A.A.B. Extracorporeal magnetic innervation therapy: Assessment of clinical efficacy in relation to urodynamic parameters. Scand. J. Urol. Nephrol. 2008, 42, 433–436. [Google Scholar] [CrossRef]
- Doğanay, M.; Kilic, S.; Yilmaz, N. Long-term effects of extracorporeal magnetic innervations in the treatment of women with urinary incontinence: Results of 3-year follow-up. Arch. Gynecol. Obstet. 2010, 282, 49–53. [Google Scholar] [CrossRef]
- Bakar, Y.; Cinar Özdemir, O.; Ozengin, N.; Duran, B. The use of extracorporeal magnetic innervation for the treatment of stress urinary incontinence in older women: A pilot study. Arch. Gynecol. Obstet. 2011, 284, 1163–1168. [Google Scholar] [CrossRef]
- Yamanishi, T.; Homma, Y.; Nishizawa, O.; Yasuda, K.; Yokoyama, O. SMN-X Study Group Multicenter, randomized, sham-controlled study on the efficacy of magnetic stimulation for women with urgency urinary incontinence. Int. J. Urol. Off. J. Jpn. Urol. Assoc. 2014, 21, 395–400. [Google Scholar]
- Alves, F.K.; Riccetto, C.; Adami, D.B.V.; Marques, J.; Pereira, L.C.; Palma, P.; Botelho, S. A pelvic floor muscle training program in postmenopausal women: A randomized controlled trial. Maturitas 2015, 81, 300–305. [Google Scholar] [CrossRef]

| Quantitative Variables | HIES Group (n = 21) | Sham Group (n = 20) | p-Value 1 | |||
|---|---|---|---|---|---|---|
| Me | Q1–Q3 | Me | Q1–Q3 | |||
| Age (years) | 53 | 44–56 | 50 | 38–59 | 0.13 | |
| Weight (kg) | 64 | 61–69 | 64 | 57–73 | 0.91 | |
| Height (m) | 1.64 | 1.63–1.66 | 1.66 | 1.64–1.70 | 0.26 | |
| BMI (kg/m2) | 24 | 22–26 | 24 | 22–26 | 0.84 | |
| Occurrence of urinary incontinence symptoms (years) | 8 | 5–10 | 5 | 2–7 | 0.052 | |
| ICIQ-UI SF score | 6 | 5–8 | 8 | 4–10 | 0.51 | |
| Qualitative Variables | n | % | n | % | p-Value 2 | |
| Kind of work | Physical | 2 | 10 | 3 | 15 | 0.86 |
| Mental | 11 | 52 | 10 | 50 | ||
| Physical/Mental | 8 | 38 | 7 | 35 | ||
| Number of deliveries | 0 | 2 | 10 | 2 | 10 | 0.97 |
| 1 | 4 | 19 | 5 | 25 | ||
| 2 | 13 | 62 | 11 | 55 | ||
| 3 | 2 | 10 | 2 | 10 | ||
| sEMG Activity of PFM (µV) | Measurement | HIES Group | Sham Group | p-Value 1 | ||
|---|---|---|---|---|---|---|
| Me | Q1–Q3 | Me | Q1–Q3 | |||
| Rest Tone (initial) | Baseline | 3.9 | 3.1–5.1 | 3.3 | 2.8–4.1 | 0.20 |
| After | 4.3 | 3.3–5.0 | 2.9 | 2.6–4.4 | 0.08 | |
| 1-h FU | 4.1 | 3.5–4.9 | 3.3 | 2.4–4.8 | 0.10 | |
| p-value 2 | 0.49 | 0.79 | ||||
| Contraction | Baseline | 10.1 | 8.3–12.3 | 9.4 | 7.5–11.7 | 0.54 |
| After | 11.7 | 9.7–13.8 | 10.5 | 8.3–12.1 | 0.047 | |
| 1-h FU | 12.0 | 10.1–13.9 | 11.0 | 8.0–12.0 | 0.017 | |
| p-value 2 | <0.001 | 0.89 | ||||
| Quick flicks | Baseline | 10.6 | 8.5–13.5 | 10.5 | 8.1–12.1 | 0.82 |
| After | 12.1 | 9.7–14.9 | 10.0 | 8.8–12.9 | 0.20 | |
| 1-h FU | 12.4 | 10.1–15.3 | 11.1 | 8.6–12.0 | 0.08 | |
| p-value 2 | 0.005 | 0.19 | ||||
| Static hold | Baseline | 10.1 | 8.3–12.3 | 9.4 | 7.5–11.7 | 0.54 |
| After | 10.6 | 9.0–14.7 | 10.0 | 8.0–13.7 | 0.58 | |
| 1-h FU | 10.7 | 9.1–14.1 | 11.1 | 8.6–12 | 0.57 | |
| p-value 2 | 0.12 | 0.55 | ||||
| Rest tone (last) | Baseline | 4.0 | 3.1–5.4 | 2.9 | 2.4–4.8 | 0.15 |
| After | 3.5 | 2.8–4.5 | 3.2 | 2.5–4.2 | 0.45 | |
| 1-h FU | 2.9 | 2.4–4.8 | 3.3 | 2.5–3.6 | 0.31 | |
| p-value 2 | 0.72 | 0.89 | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ptaszkowski, K.; Malkiewicz, B.; Zdrojowy, R.; Ptaszkowska, L.; Paprocka-Borowicz, M. Assessment of the Short-Term Effects after High-Inductive Electromagnetic Stimulation of Pelvic Floor Muscles: A Randomized, Sham-Controlled Study. J. Clin. Med. 2020, 9, 874. https://doi.org/10.3390/jcm9030874
Ptaszkowski K, Malkiewicz B, Zdrojowy R, Ptaszkowska L, Paprocka-Borowicz M. Assessment of the Short-Term Effects after High-Inductive Electromagnetic Stimulation of Pelvic Floor Muscles: A Randomized, Sham-Controlled Study. Journal of Clinical Medicine. 2020; 9(3):874. https://doi.org/10.3390/jcm9030874
Chicago/Turabian StylePtaszkowski, Kuba, Bartosz Malkiewicz, Romuald Zdrojowy, Lucyna Ptaszkowska, and Malgorzata Paprocka-Borowicz. 2020. "Assessment of the Short-Term Effects after High-Inductive Electromagnetic Stimulation of Pelvic Floor Muscles: A Randomized, Sham-Controlled Study" Journal of Clinical Medicine 9, no. 3: 874. https://doi.org/10.3390/jcm9030874
APA StylePtaszkowski, K., Malkiewicz, B., Zdrojowy, R., Ptaszkowska, L., & Paprocka-Borowicz, M. (2020). Assessment of the Short-Term Effects after High-Inductive Electromagnetic Stimulation of Pelvic Floor Muscles: A Randomized, Sham-Controlled Study. Journal of Clinical Medicine, 9(3), 874. https://doi.org/10.3390/jcm9030874






