Five Years Outcomes and Predictors of Events in a Single-Center Cohort of Patients Treated with Bioresorbable Coronary Vascular Scaffolds
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. BRS Implantation
2.3. Quantitative Coronary Analysis
2.4. Endpoints
2.5. Statistical Methods
3. Results
3.1. Patient Characteristics
3.2. Lesion Characteristics
3.3. Lesion Treatment and Immediate Angiographic Results
3.4. Follow-Up
3.5. Predictors of Target Lesion Failure
4. Discussion
- -
- the incidence of late adverse events after implantation of a BRS decreases over the time.
- -
- the procedural and angiographic characteristics that could be identified as predictors of negative outcome in the first three years after index procedure do not predict TLF between 4–5 years, and diabetes, a known patient-related risk factor, was the only predictor of TLF between 4–5 years.
4.1. Target Lesion Failure in Stent-Studies
4.2. Predictors of Early and Late Events
4.3. Limitations
5. Significance and Future Perspectives
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Serruys, P.W.; Onuma, Y.; Dudek, D.; Smits, P.C.; Koolen, J.; Chevalier, B.; de Bruyne, B.; Thuesen, L.; McClean, D.; van Geuns, R.J.; et al. Evaluation of the second generation of a bioresorbable everolimus-eluting vascular scaffold for the treatment of de novo coronary artery stenosis: 12-month clinical and imaging outcomes. J. Am. Coll. Cardiol 2011, 58, 1578–1588. [Google Scholar] [CrossRef]
- Polimeni, A.; Anadol, R.; Munzel, T.; Indolfi, C.; De Rosa, S.; Gori, T. Long-term outcome of bioresorbable vascular scaffolds for the treatment of coronary artery disease: A meta-analysis of RCTs. BMC Cardiovasc. Disord. 2017, 17, 147. [Google Scholar] [CrossRef]
- Tamburino, C.; Capranzano, P.; Gori, T.; Latib, A.; Lesiak, M.; Nef, H.; Caramanno, G.; Naber, C.; Mehilli, J.; Di Mario, C.; et al. 1-Year Outcomes of Everolimus-Eluting Bioresorbable Scaffolds Versus Everolimus-Eluting Stents: A Propensity-Matched Comparison of the GHOST-EU and XIENCE V USA Registries. JACC Cardiovasc. Interv. 2016, 9, 440–449. [Google Scholar] [CrossRef]
- Nef, H.M.; Wiebe, J.; Kastner, J.; Mehilli, J.; Muenzel, T.; Naber, C.; Neumann, T.; Richardt, G.; Schmermund, A.; Woehrle, J.; et al. Everolimus-eluting bioresorbable scaffolds in patients with coronary artery disease: Results from the German-Austrian ABSORB RegIstRy (GABI-R). EuroIntervention 2017, 13, 1311–1318. [Google Scholar] [CrossRef]
- Wohrle, J.; Nef, H.M.; Naber, C.; Achenbach, S.; Riemer, T.; Mehilli, J.; Munzel, T.; Schneider, S.; Markovic, S.; Seeger, J.; et al. Predictors of early scaffold thrombosis: Results from the multicenter prospective German-Austrian ABSORB RegIstRy. Coron. Artery Dis. 2018, 29, 389–396. [Google Scholar] [CrossRef]
- Anadol, R.; Gori, T. The mechanisms of late scaffold thrombosis. Clin. Hemorheol. Microcirc. 2017, 67, 343–346. [Google Scholar] [CrossRef]
- Ellis, S.G.; Gori, T.; Serruys, P.W.; Nef, H.; Steffenino, G.; Brugaletta, S.; Munzel, T.; Feliz, C.; Schmidt, G.; Sabate, M.; et al. Clinical, Angiographic, and Procedural Correlates of Very Late Absorb Scaffold Thrombosis: Multistudy Registry Results. JACC Cardiovasc. Interv. 2018, 11, 638–644. [Google Scholar] [CrossRef]
- Gori, T.; Weissner, M.; Gonner, S.; Wendling, F.; Ullrich, H.; Ellis, S.; Anadol, R.; Polimeni, A.; Munzel, T. Characteristics, Predictors, and Mechanisms of Thrombosis in Coronary Bioresorbable Scaffolds: Differences Between Early and Late Events. JACC Cardiovasc. Interv. 2017, 10, 2363–2371. [Google Scholar] [CrossRef]
- Mehilli, J.; Achenbach, S.; Woehrle, J.; Baquet, M.; Riemer, T.; Muenzel, T.; Nef, H.; Naber, C.; Richardt, G.; Zahn, R.; et al. Clinical restenosis and its predictors after implantation of everolimus-eluting bioresorbable vascular scaffolds: Results from GABI-R. EuroIntervention 2017, 13, 1319–1326. [Google Scholar] [CrossRef]
- Puricel, S.; Cuculi, F.; Weissner, M.; Schmermund, A.; Jamshidi, P.; Nyffenegger, T.; Binder, H.; Eggebrecht, H.; Munzel, T.; Cook, S.; et al. Bioresorbable Coronary Scaffold Thrombosis: Multicenter Comprehensive Analysis of Clinical Presentation, Mechanisms, and Predictors. J. Am. Coll. Cardiol. 2016, 67, 921–931. [Google Scholar] [CrossRef]
- Boeder, N.F.; Weissner, M.; Blachutzik, F.; Ullrich, H.; Anadol, R.; Tröbs, M.; Münzel, T.; Hamm, C.W.; Dijkstra, J.; Achenbach, S.; et al. Incidental Finding of Strut Malapposition Is a Predictor of Late and Very Late Thrombosis in Coronary Bioresorbable Scaffolds. J. Clin. Med. 2019, 8, 580. [Google Scholar] [CrossRef]
- Gori, T.; Polimeni, A.; Indolfi, C.; Raber, L.; Adriaenssens, T.; Munzel, T. Predictors of stent thrombosis and their implications for clinical practice. Nat. Rev. Cardiol. 2019, 16, 243–256. [Google Scholar] [CrossRef]
- Dimitriadis, Z.; Polimeni, A.; Anadol, R.; Geyer, M.; Weissner, M.; Ullrich, H.; Munzel, T.; Gori, T. Procedural Predictors for Bioresorbable Vascular Scaffold Thrombosis: Analysis of the Individual Components of the “PSP” Technique. J. Clin. Med. 2019, 8, 93. [Google Scholar] [CrossRef]
- Regazzoli, D.; Latib, A.; Ezhumalai, B.; Tanaka, A.; Leone, P.P.; Khan, S.; Kumar, V.; Rastogi, V.; Ancona, M.B.; Mangieri, A.; et al. Long-term follow-up of BVS from a prospective multicenter registry: Impact of a dedicated implantation technique on clinical outcomes. Int. J. Cardiol. 2018, 270, 113–117. [Google Scholar] [CrossRef]
- Serruys, P.W.; Ormiston, J.; van Geuns, R.J.; de Bruyne, B.; Dudek, D.; Christiansen, E.; Chevalier, B.; Smits, P.; McClean, D.; Koolen, J.; et al. Polylactide Bioresorbable Scaffold Eluting Everolimus for Treatment of Coronary Stenosis: 5-Year Follow-Up. J. Am. Coll. Cardiol. 2016, 67, 766–776. [Google Scholar] [CrossRef]
- Stone, G.W.; Kimura, T.; Gao, R.; Kereiakes, D.J.; Ellis, S.G.; Onuma, Y.; Chevalier, B.; Simonton, C.; Dressler, O.; Crowley, A.; et al. Time-Varying Outcomes With the Absorb Bioresorbable Vascular Scaffold During 5-Year Follow-up: A Systematic Meta-analysis and Individual Patient Data Pooled Study. JAMA Cardiol. 2019, 4, 1261–1269. [Google Scholar] [CrossRef]
- Ryan, T.J.; Bauman, W.B.; Kennedy, J.W.; Kereiakes, D.J.; King, S.B., 3rd; McCallister, B.D.; Smith, S.C., Jr.; Ullyot, D.J. Guidelines for percutaneous transluminal coronary angioplasty. A report of the American Heart Association/American College of Cardiology Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Committee on Percutaneous Transluminal Coronary Angioplasty). Circulation 1993, 88, 2987–3007. [Google Scholar]
- Cutlip, D.E.; Windecker, S.; Mehran, R.; Boam, A.; Cohen, D.J.; van Es, G.A.; Steg, P.G.; Morel, M.A.; Mauri, L.; Vranckx, P.; et al. Academic Research Consortium, Clinical end points in coronary stent trials: A case for standardized definitions. Circulation 2007, 115, 2344–2351. [Google Scholar] [CrossRef]
- Anadol, R.; Lorenz, L.; Weissner, M.; Ullrich, H.; Polimeni, A.; Munzel, T.; Gori, T. Characteristics and outcome of patients with complex coronary lesions treated with bioresorbable scaffolds Three years follow-up in a cohort of consecutive patients. Eurointerv. 2018, 14(9), E1011. [Google Scholar] [CrossRef]
- Pilgrim, T.; Piccolo, R.; Heg, D.; Roffi, M.; Tüller, D.; Muller, O.; Moarof, I.; Siontis, G.C.M.; Cook, S.; Weilenmann, D.; et al. Ultrathin-strut, biodegradable-polymer, sirolimus-eluting stents versus thin-strut, durable-polymer, everolimus-eluting stents for percutaneous coronary revascularisation: 5-year outcomes of the BIOSCIENCE randomised trial. Lancet 2018, 392, 737–746. [Google Scholar] [CrossRef]
- Kufner, S.; Joner, M.; Thannheimer, A.; Hoppmann, P.; Ibrahim, T.; Mayer, K.; Cassese, S.; Laugwitz, K.L.; Schunkert, H.; Kastrati, A.; et al. Ten-Year Clinical Outcomes From a Trial of Three Limus-Eluting Stents With Different Polymer Coatings in Patients With Coronary Artery Disease. Circulation 2019, 139, 325–333. [Google Scholar] [CrossRef]
- Polimeni, A.; Weissner, M.; Schochlow, K.; Ullrich, H.; Indolfi, C.; Dijkstra, J.; Anadol, R.; Münzel, T.; Gori, T. Incidence, Clinical Presentation, and Predictors of Clinical Restenosis in Coronary Bioresorbable Scaffolds. JACC Cardiovasc. Interv. 2017, 10, 1819–1827. [Google Scholar] [CrossRef]
- Anadol, R.; Schnitzler, K.; Lorenz, L.; Weissner, M.; Ullrich, H.; Polimeni, A.; Münzel, T.; Gori, T. Three-Years Outcomes of Diabetic Patients Treated with Coronary Bioresorbable Scaffolds. BMC Cardiovasc. Disord. 2018, 18, 92. [Google Scholar] [CrossRef]
- Ritsinger, V.; Saleh, N.; Lagerqvist, B.; Norhammar, A. High event rate after a first percutaneous coronary intervention in patients with diabetes mellitus: Results from the Swedish coronary angiography and angioplasty registry. Circ. Cardiovasc. Interv. 2015, 8, e002328. [Google Scholar] [CrossRef]
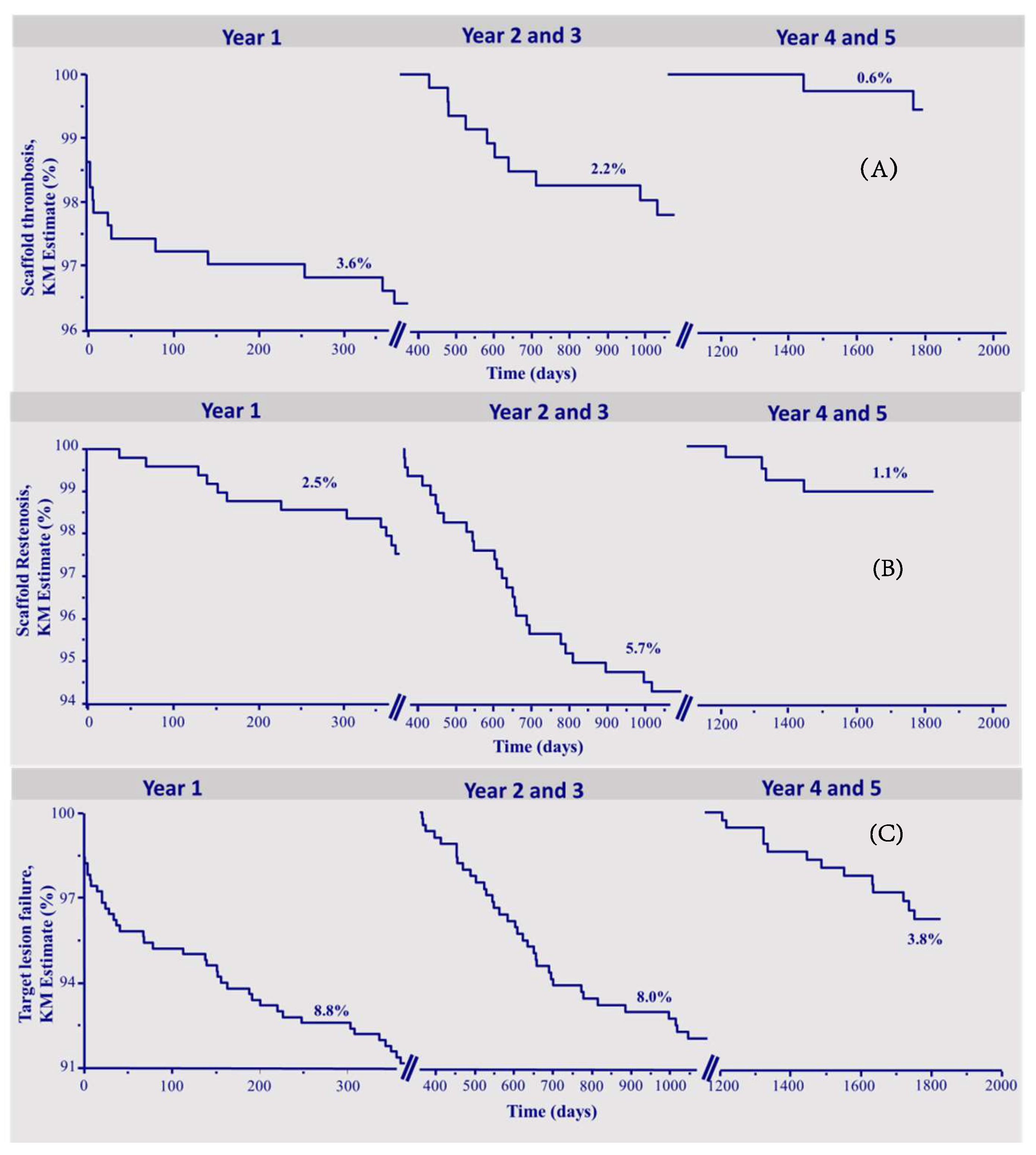

| Within 1 Year | All Patients | Optimal Implantation | Non-Optimal Implantation | p | HR 95% CI |
| ScT | 18 (3.6%) | 2 (1%) | 16 (5.3%) | 0.02 | 5.36 (1.31–8.65) |
| ScR | 12 (2.5%) | 2 (1.0%) | 10 (3.4%) | 0.10 | 3.29 (0.82–8.31) |
| TLF | 44 (8.8%) | 10 (5.1%) | 34 (11.3%) | 0.02 | 2.29 (1.14–3.80) |
| 2–3 years | All Patients | Optimal Implantation | Non-Optimal Implantation | p | HR 95% CI |
| ScT | 10 (2.2%) | 2 (1.1%) | 8 (2.9%) | 0.18 | 2.78 (0.67–8.39) |
| ScR | 26 (5.7%) | 5 (3.7%) | 21 (7.7%) | 0.03 | 2.90 (1.12–5.34) |
| TLF | 35 (8.0%) | 7 (3.9%) | 28 (10.8%) | 0.01 | 2.95 (1.28–4.91) |
| 4–5 years | All Patients | Optimal Implantation | Non-Optimal Implantation | p | HR 95% CI |
| ScT | 2 (0.6%) | 2 (1.4%) | 0 | 0.08 | - |
| ScR | 4 (1.1%) | 2 (1.3%) | 2 (0.9%) | 0.67 | 0.65 (0.09–4.79) |
| TLF | 13 (3.8%) | 5 (3.5%) | 8 (4.0%) | 0.86 | 1.10 (0.36–3.33) |
| Cumulative 5 years | All Patients | Optimal Implantation | Non-Optimal Implantation | p | HR 95% CI |
| ScT | 30 (5.9%) | 6 (3.5%) | 24 (8.1%) | 0.020 | 2.76 (1.33–5.72) |
| ScR | 42 (8.2%) | 9 (5.0%) | 33 (11.6%) | 0.010 | 2.54 (1.37–4.70) |
| TLF | 92 (19.3%) | 22 (12%) | 70 (24.0%) | 0.0005 | 2.30 (1.52–3.48) |
| Max Footprint | HR | p |
| 1 year | 1.06 (1.04–1.08) | <0.0001 |
| 2–3 years | 1.09 (1.06–1.11) | <0.0001 |
| 4–5 years | 1.03 (0.96–1.11) | 0.40 |
| Optimal Implantation | ||
| 1year | 0.44 (0.22–0.88) | 0.02 |
| 2–3 years | 0.34 (0.17–0.66) | <0.01 (0.007) |
| 4–5 years | 0.91 (0.30–2.74) | 0.86 |
| RVD < 2.5 mm | ||
| 1 year | 1.99 (1.03–3.86) | 0.04 |
| 2–3 years | 2.17 (1.05–4.50) | 0.04 |
| 4–5 years | 1.03 (0.23–4.60) | 0.97 |
| RVD > 3.5 mm | ||
| 1 year | 1.13 (0.48–2.67) | 0.78 |
| 2–3 years | 2.33 (1.06–5.12) | 0.04 |
| 4–5 years | 0.64 (0.08–4.89) | 0.67 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anadol, R.; Mühlenhaus, A.; Trieb, A.-K.; Polimeni, A.; Münzel, T.; Gori, T. Five Years Outcomes and Predictors of Events in a Single-Center Cohort of Patients Treated with Bioresorbable Coronary Vascular Scaffolds. J. Clin. Med. 2020, 9, 847. https://doi.org/10.3390/jcm9030847
Anadol R, Mühlenhaus A, Trieb A-K, Polimeni A, Münzel T, Gori T. Five Years Outcomes and Predictors of Events in a Single-Center Cohort of Patients Treated with Bioresorbable Coronary Vascular Scaffolds. Journal of Clinical Medicine. 2020; 9(3):847. https://doi.org/10.3390/jcm9030847
Chicago/Turabian StyleAnadol, Remzi, Annika Mühlenhaus, Ann-Kristin Trieb, Alberto Polimeni, Thomas Münzel, and Tommaso Gori. 2020. "Five Years Outcomes and Predictors of Events in a Single-Center Cohort of Patients Treated with Bioresorbable Coronary Vascular Scaffolds" Journal of Clinical Medicine 9, no. 3: 847. https://doi.org/10.3390/jcm9030847
APA StyleAnadol, R., Mühlenhaus, A., Trieb, A.-K., Polimeni, A., Münzel, T., & Gori, T. (2020). Five Years Outcomes and Predictors of Events in a Single-Center Cohort of Patients Treated with Bioresorbable Coronary Vascular Scaffolds. Journal of Clinical Medicine, 9(3), 847. https://doi.org/10.3390/jcm9030847







