To Treat or Not to Treat: Importance of Functional Dependence in Deciding Intravenous Thrombolysis of “Mild Stroke” Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Data Collection
2.3. Outcome Measures
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Reeves, M.; Khoury, J.; Alwell, K.; Moomaw, C.; Flaherty, M.; Woo, D.; Khatri, P.; Adeoye, O.; Ferioli, S.; Kissela, N.; et al. Distribution of national institutes of health stroke scale in the Cincinnati/Northern Kentucky stroke study. Stroke 2013, 44, 3211–3213. [Google Scholar] [CrossRef]
- Dhamoon, M.S.; Moon, Y.P.; Paik, M.C.; Boden-Albala, B.; Rundek, T.; Sacco, R.L.; Elkind, M.S. Long-term functional recovery after first ischemic stroke. Stroke 2009, 40, 2805–2811. [Google Scholar] [CrossRef]
- Messé, S.R.; Khatri, P.; Reeves, M.J.; Smith, E.E.; Saver, J.L.; Bhatt, D.L.; Grau-Sepulveda, M.V.; Cox, M.; Peterson, E.D.; Fonarow, G.C.; et al. Why are acute ischemic stroke patients not receiving IV tPA? Results from a national registry. Neurology 2016, 87, 1565–1574. [Google Scholar] [CrossRef]
- Barber, P.A.; Zhang, J.; Demchuk, A.M.; Hill, M.D.; Buchan, A.M. Why are stroke patients excluded from TPA therapy? An analysis of patient eligibility. Neurology 2001, 56, 1015–1020. [Google Scholar] [CrossRef] [PubMed]
- Huisa, B.N.; Raman, R.; Neil, W.; Ernstrom, K.; Hemmen, T. Intravenous tissue plasminogen activator for patients with minor ischemic stroke. J. Stroke Cerebrovasc. Dis. 2012, 21, 732–736. [Google Scholar] [CrossRef] [PubMed]
- Nesi, M.; Lucente, G.; Nencini, P.; Fancellu, L.; Inzitari, D. Aphasia predicts unfavorable outcome in mild ischemic stroke patients and prompts thrombolytic treatment. J. Stroke Cerebrovasc. Dis. 2014, 23, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Urra, X.; Ariño, H.; Llull, L.; Amaro, S.; Obach, V.; Cervera, A.; Chamorro, A. The outcome of patients with mild stroke improves after treatment with systemic thrombolysis. PLoS ONE 2013, 8, e59420. [Google Scholar] [CrossRef] [PubMed]
- Greisenegger, S.; Seyfang, L.; Kiechl, S.; Lang, W.; Ferrari, J. Austrian Stroke Unit Registry Collaborators. Thrombolysis in patients with mild stroke: Results from the Austrian Stroke Unit Registry. Stroke 2014, 45, 765–769. [Google Scholar] [CrossRef]
- Spokoyny, I.; Raman, R.; Ernstrom, K.; Khatri, P.; Meyer, D.M.; Hemmen, T.M.; Meyer, B.C. Defining mild stroke: Outcomes analysis of treated and untreated mild stroke patients. J. Stroke Cerebrovasc. Dis. 2015, 24, 1276–1281. [Google Scholar] [CrossRef]
- Haeberlin, M.I.; Held, U.; Baumgartner, R.W.; Georgiadis, D.; Valko, P.O. Impact of intravenous thrombolysis on functional outcome in patients with mild ischemic stroke without large vessel occlusion or rapidly improving symptoms. Int. J. Stroke 2019. [Google Scholar] [CrossRef]
- Adams, H.P., Jr.; Brott, T.G.; Furlan, A.J.; Gomez, C.R.; Grotta, J.; Helgason, C.M.; Kwiatkowski, T.; Lyden, P.D.; Marler, J.R.; Torner, J.; et al. Guidelines for thrombolytic therapy for acute stroke: A supplement to the guidelines for the management of patients with acute ischemic stroke. A statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke 1996, 27, 1711–1718. [Google Scholar] [PubMed]
- Adams, H.O., Jr.; del Zoppo, G.; Alberts, M.J.; Bhatt, D.L.; Brass, L.; Furlan, A.; Grubb, R.L.; Higashida, R.T.; Jauch, E.C.; Kidwell, C.; et al. American Heart Association, American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups. Guidelines for the early management of adults with ischemic stroke: A guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology Affirms the Value of This Guideline as an Educational Tool for Neurologists. Stroke 2007, 38, 1655–1711. [Google Scholar] [PubMed]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; David, L.; et al. American Heart Association Stroke Council. 2018 guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2018, 49, e46–e110. [Google Scholar] [CrossRef] [PubMed]
- Wendt, M.; Tutuncu, S.; Fiebach, J.B.; Scheitz, J.F.; Audebert, H.J.; Nolte, C.H. Preclusion of ischemic stroke patients from intravenous tissue plasminogen activator treatment for mild symptoms should not be based on low National Institutes of Health Stroke Scale scores. J. Stroke Cerebrovasc. Dis. 2013, 22, 550–553. [Google Scholar] [CrossRef] [PubMed]
- Yeatts, S.D.; Broderick, J.P.; Chatterjee, A.; Jauch, E.C.; Levine, S.R.; Romano, J.G.; Saver, J.L.; Vagal, A.; Purdon, B.; Devenport, J.; et al. Alteplase for the treatment of acute ischemic stroke in patients with low National Institutes of Health Stroke Scale and not clearly disabling deficits (Potential of rtPA for Ischemic Strokes with Mild Symptoms PRISMS): Rationale and design. Int. J. Stroke 2018, 13, 654–661. [Google Scholar] [CrossRef] [PubMed]
- Khatri, P.; Kleindorfer, D.O.; Devlin, T.; Sawyer, R.N.; Starr, M.; Mejilla, J.; Broderick, J.; Chatterjee, A.; Jauch, E.C.; Levine, S.R.; et al. Effect of alteplase vs. aspirin on functional outcome for patients with acute ischemic stroke and minor nondisabling neur logic deficits: The PRISMS randomized clinical trial. JAMA 2018, 320, 156–166. [Google Scholar] [CrossRef]
- Hacke, W.; Kaste, M.; Bluhmki, E.; Brozman, M.; Davalos, A.; Guidetti, D.; Larrue, V.; Lees, K.R.; Medeghri, Z.; Machnig, T.; et al. Thrombolysis with alteplase 3 to 4.5 h after acute ischemic stroke. N. Engl. J. Med. 2008, 359, 1317–1329. [Google Scholar] [CrossRef]
- Fischer, U.; Baumgartner, A.; Arnold, M.; Nedeltchev, K.; Gralla, J.; Marco De Marchis, G.; Kappeler, L.; Mono, M.-L.; Brekenfeld, C.; Schroth, G.; et al. What is a minor stroke? Stroke 2010, 41, 661–666. [Google Scholar] [CrossRef]
- Luengo-Fernandez, R.; Gray, A.M.; Rothwell, P.M. Effect of urgent treatment for transient ischaemic attack and minor stroke on disability and hospital costs (EXPRESS study): A prospective population-based sequential comparison. Lancet Neurol. 2009, 8, 218–219. [Google Scholar] [CrossRef]
- Coutts, S.B.; Hill, M.D.; Campos, C.R.; Choi, Y.B.; Subramaniam, S.; Kosior, J.C.; Demchuk, A.M. Recurrent events in transient ischemic attack and minor stroke. Stroke 2008, 39, 2461–2466. [Google Scholar] [CrossRef]
- Schwartz, J.K.; Capo-Lugo, C.E.; Akinwuntan, A.E.; Roberts, P.; Krishnan, S.; Belagaje, S.R.; Lovic, M.; Burns, S.P.; Hu, X.; Danzl, M.; et al. Classification of mild stroke: A mapping review. Pm&r 2019, 11, 996–1003. [Google Scholar]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Barak, S.; Duncan, P.W. Issues in selecting outcome measures to assess functional recovery after stroke. NeuroRx 2006, 3, 505–524. [Google Scholar] [CrossRef] [PubMed]
- Wardlaw Wardlaw, J.M.; Murray, V.; Berge, E.; del Zoppo, G.J. Thrombolysis for acute ischemic stroke. Cochrane Database Syst. Rev. 2014, 7, CD000213. [Google Scholar]
| IVT+ (n = 113) | IVT– (n = 276) | p | |
|---|---|---|---|
| Demographic data and baseline clinical characteristics | |||
| Age, years | 68.2 ± 12.0 | 68.7 ± 14.2 | 0.7 |
| Males, n (%) | 67 (59.3) | 168 (60.9) | 0.8 |
| NIHSS score at admission, median (IQR) | 3 (2−4) | 2 (1−3) | 0.001 |
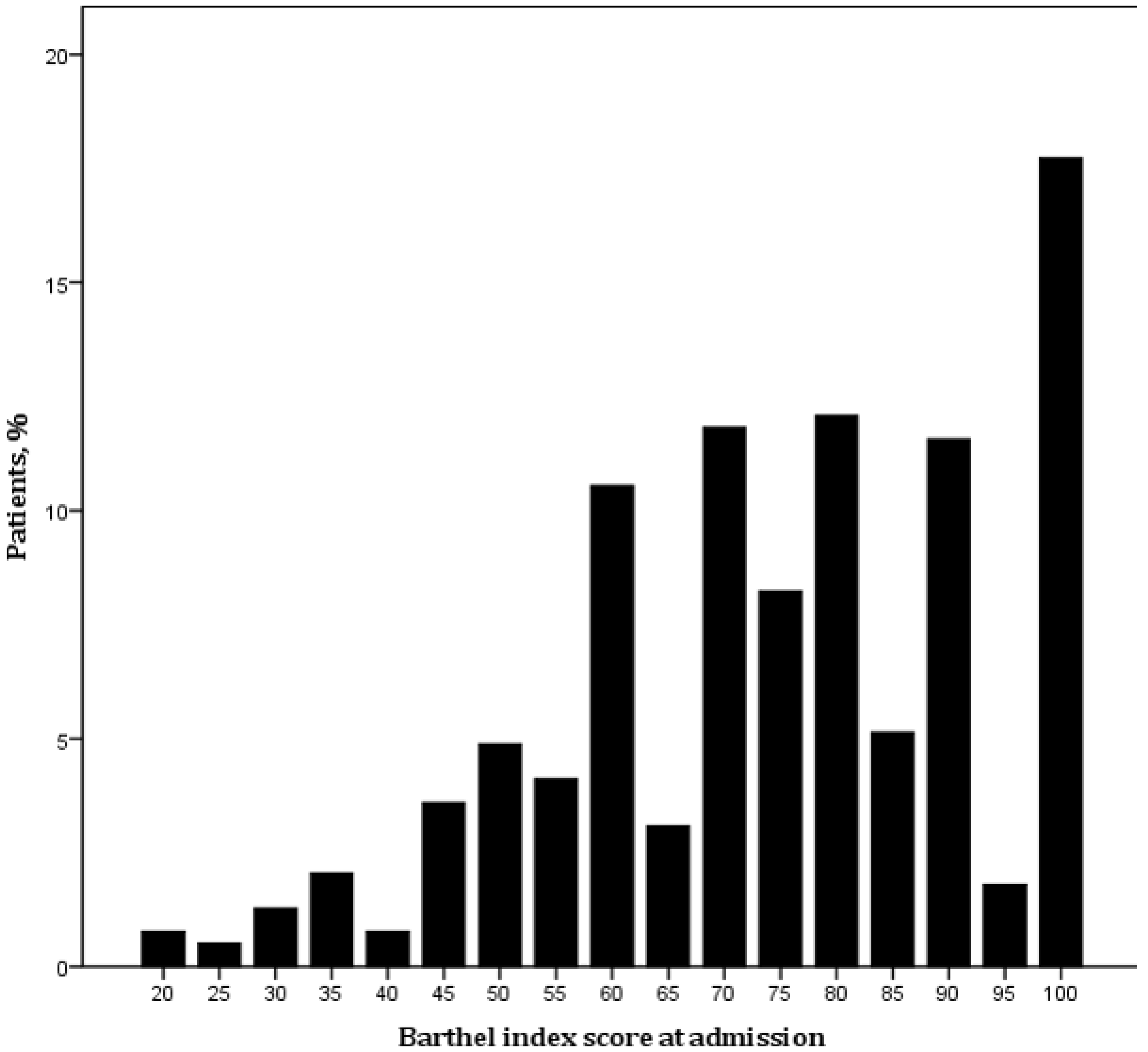
| BI score at admission, median (IQR) | 60 (75−90) | 60 (75−90) | 0.5 |
| Medications prior to onset, n (%) | |||
| Antiplatelet agents | 39 (34.5) | 79 (28.6) | 0.2 |
| Anticoagulant agents | 1 (0.9) | 25 (9.1) | 0.003 |
| Glucose level, mg/dl | 126.4 ± 35.3 | 134.2 ± 64.7 | 0.3 |
| Vascular risk factors | |||
| Previous transient ischemic attack/stroke, n (%) | 15 (13.3) | 45 (16.3) | 0.4 |
| Ischemic heart disease, n (%) | 19 (18.3) | 27 (10.8) | 0.06 |
| Peripheral artery disease, n (%) | 2 (1.9) | 2 (0.8) | 0.6 |
| Obesity, n (%) | 9 (8.7) | 22 (8.8) | 0.9 |
| Atrial fibrillation, n (%) | 19 (16.8) | 67 (24.3) | 0.1 |
| Hypertension, n (%) | 68 (60.2) | 184 (66.7) | 0.2 |
| Diabetes mellitus, n (%) | 17 (15.0) | 63 (22.8) | 0.08 |
| Hypercholesterolemia, n (%) | 43 (38.1) | 102 (37.0) | 0.8 |
| Current smoking, n (%) | 29 (26.1) | 53 (21.1) | 0.3 |
| IVT+ (n = 113) | IVT– (n = 276) | p | |
|---|---|---|---|
| Efficacy endpoints | |||
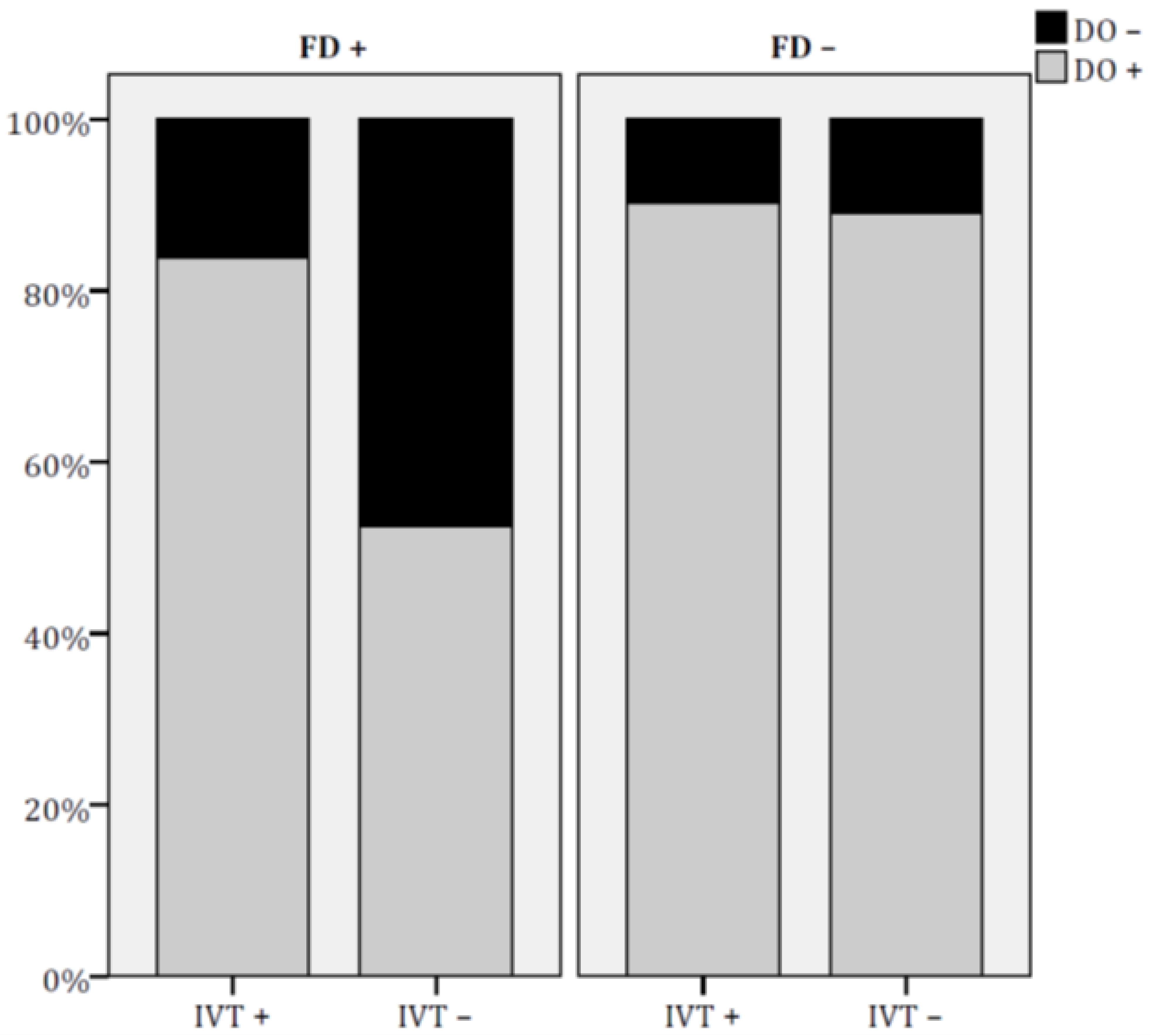
| DO+, n (%) | 98 (86.7) | 195 (70.7) | 0.001 |
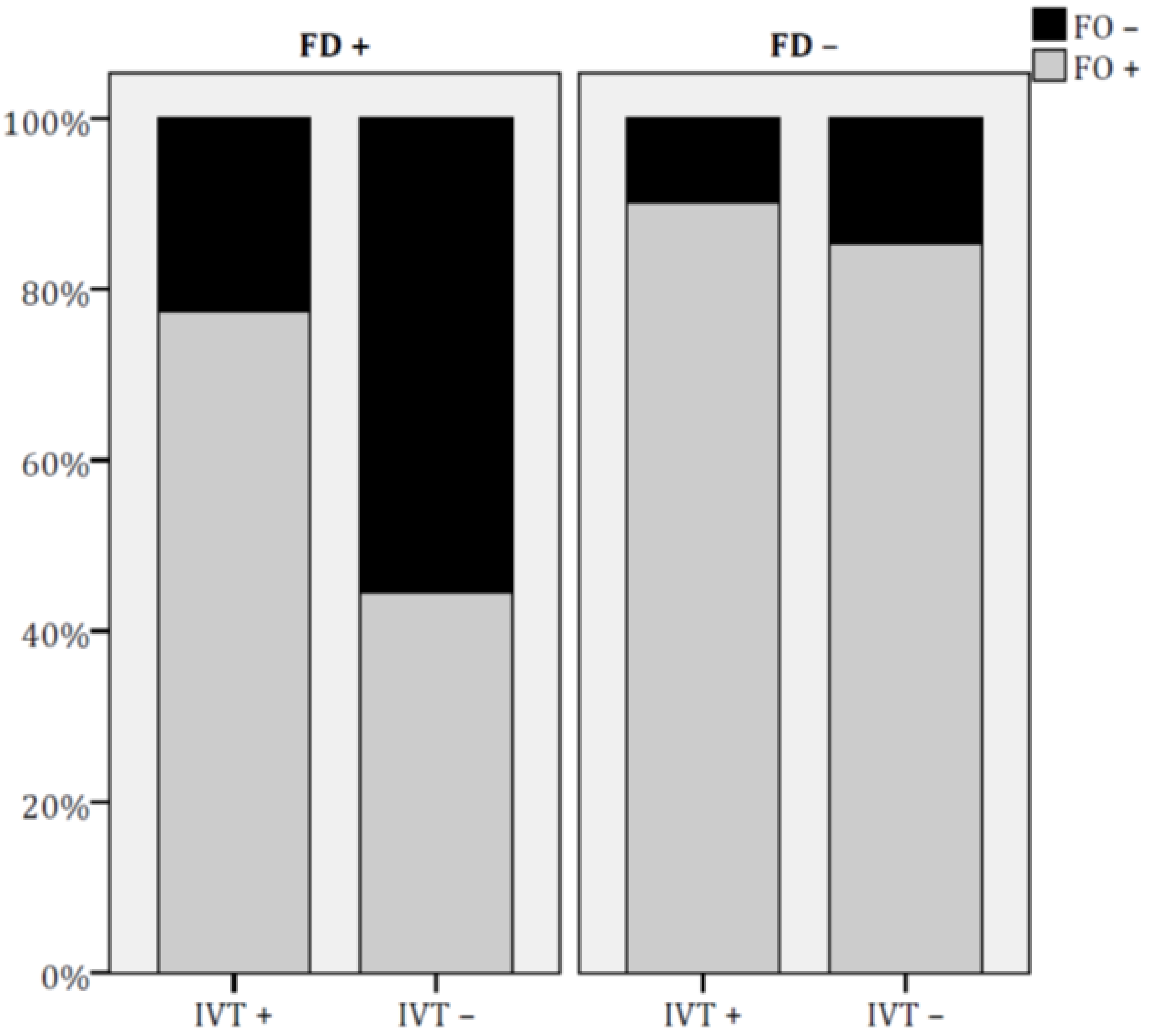
| FO+, n (%) | 94 (83.9) | 179 (65.6) | 0.001 |
| Safety endpoints | |||
| Mortality at 3-months, n (%) | 1 (0.9) | 3 (1.1) | 0.8 |
| sICH, n (%) | 5 (4.4) | 3 (1.1) | 0.03 |
| DO+ | OR | 95% CI | p |
| IVT treatment | |||
| No | 1.00 | ||
| Yes | 3.12 | 1.34−7.27 | 0.008 |
| Age | 0.95 | 0.92−0.98 | 0.003 |
| BI score at admission | 1.06 | 1.04−1.09 | 0.001 |
| FO+ | OR | 95% CI | p |
| IVT treatment | |||
| No | 1.00 | ||
| Yes | 4.70 | 2.38−9.26 | 0.001 |
| Age | 0.98 | 0.96−0.99 | 0.02 |
| NIHSS score at admission | 0.77 | 0.61−0.97 | 0.03 |
| BI score at admission | 1.06 | 1.04−1.07 | 0.001 |
| Diabetes mellitus | |||
| No | 1.00 | ||
| Yes | 0.53 | 0.29−0.98 | 0.04 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Merlino, G.; Smeralda, C.; Lorenzut, S.; Gigli, G.L.; Surcinelli, A.; Valente, M. To Treat or Not to Treat: Importance of Functional Dependence in Deciding Intravenous Thrombolysis of “Mild Stroke” Patients. J. Clin. Med. 2020, 9, 768. https://doi.org/10.3390/jcm9030768
Merlino G, Smeralda C, Lorenzut S, Gigli GL, Surcinelli A, Valente M. To Treat or Not to Treat: Importance of Functional Dependence in Deciding Intravenous Thrombolysis of “Mild Stroke” Patients. Journal of Clinical Medicine. 2020; 9(3):768. https://doi.org/10.3390/jcm9030768
Chicago/Turabian StyleMerlino, Giovanni, Carmelo Smeralda, Simone Lorenzut, Gian Luigi Gigli, Andrea Surcinelli, and Mariarosaria Valente. 2020. "To Treat or Not to Treat: Importance of Functional Dependence in Deciding Intravenous Thrombolysis of “Mild Stroke” Patients" Journal of Clinical Medicine 9, no. 3: 768. https://doi.org/10.3390/jcm9030768
APA StyleMerlino, G., Smeralda, C., Lorenzut, S., Gigli, G. L., Surcinelli, A., & Valente, M. (2020). To Treat or Not to Treat: Importance of Functional Dependence in Deciding Intravenous Thrombolysis of “Mild Stroke” Patients. Journal of Clinical Medicine, 9(3), 768. https://doi.org/10.3390/jcm9030768





