Classifying Ectopia Lentis in Marfan Syndrome into Five Grades of Increasing Severity
Abstract
1. Introduction
2. Experimental Section
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Von Kodolitsch, Y.; Robinson, P.N. Marfan syndrome: An update of genetics, medical and surgical management. Heart 2007, 93, 755–760. [Google Scholar] [CrossRef] [PubMed]
- Dean, J.C. Marfan syndrome: Clinical diagnosis and management. Eur. J. Hum. Genet. 2007, 15, 724–733. [Google Scholar] [CrossRef] [PubMed]
- Maumenee, I.H. The eye in the Marfan syndrome. Trans. Am. Phthalmol. Soc. 1981, 79, 684–733. [Google Scholar]
- Dietz, H.C.; Cutting, G.R. Marfan syndrome caused by a recurrent de novo missense mutation in the fibrillin gene. Nature 1991, 352, 337–339. [Google Scholar] [CrossRef] [PubMed]
- De Paepe, A.; Devereux, R.B. Revised diagnostic criteria for the Marfan syndrome. Am. Med. Genet. 1996, 62, 417–426. [Google Scholar] [CrossRef]
- Loeys, B.L.; Dietz, H.C. The revised Ghent nosology for the Marfan syndrome. J. Med. Genet. 2010, 47, 476–485. [Google Scholar] [CrossRef]
- Robinson, P.N.; Arteaga-Solis, E. The molecular genetics of Marfan syndrome and related disorders. J. Med. Genet. 2006, 43, 769–787. [Google Scholar] [CrossRef]
- Loeys, B.L.; Nuytinck, L. Genotype and phenotype analysis of 171 patients referred for molecular study of the fibrillin-1 gene FBN1 because of suspected Marfan syndrome. Arch. Intern. Med. 2001, 161, 2447–2454. [Google Scholar] [CrossRef]
- Sakai, L.Y.; Keene, D.R. Fibrillin, a new 350-kD glycoprotein, is a component of extracellular microfibrils. J. Cell Biol. 1986, 103, 2499–2509. [Google Scholar] [CrossRef]
- Hollister, D.W.; Godfrey, M. Immunohistologic abnormalities of the microfibrillar-fiber system in the Marfan syndrome. N. Eng. J. Med. 1990, 323, 152–159. [Google Scholar] [CrossRef]
- Nemet, A.Y.; Assia, E.I. Current concepts of ocular manifestations in Marfan syndrome. Surv. Ophthalmol. 2006, 51, 561–575. [Google Scholar] [CrossRef] [PubMed]
- Ashworth, J.L.; Kielty, C.M. Fibrillin and the eye. Br. J. Ophthahlmol. 2000, 84, 1312–1317. [Google Scholar] [CrossRef] [PubMed]
- Mir, S.; Wheatley, H.M. A comparative histologic study of the fibrillin microfibrillar system in the lens capsule of normal subjects and subjects with Marfan syndrome. Investig. Ophthalmol. Vis. Sci. 1998, 39, 84–93. [Google Scholar]
- Ashworth, J.L.; Murphy, G. Fibrillin degradation by matrix metalloproteinases: Implications for connective tissue remodelling. Biochem. J. 1999, 15, 171–181. [Google Scholar] [CrossRef]
- Loeys, B. The search for genotype/phenotype correlation in Marfan syndrome: To be or not to be? Eur. Heart J. 2016, 37, 3291–3293. [Google Scholar] [CrossRef] [PubMed]
- Sakai, Y.S.; Keene, D.R. FBN1: The disease-causing gene for Marfan syndrome and other genetic disorders. Gene 2016, 592, 279–291. [Google Scholar] [CrossRef] [PubMed]
- Baudhuin, L.; Kotzer, K. Increased frequency of FBN1 truncating and splicing variants in Marfan syndrome patients with aortic events. Genet. Med. 2015, 17, 177–187. [Google Scholar] [CrossRef]
- Franken, R.; Groenink, M. Genotype impacts survival in Marfan syndrome. Eur. Heart J. 2016, 37, 3285–3290. [Google Scholar] [CrossRef]
- Kinori, M.; Wehrli, S. Biometry characteristics in adults and children with Marfan syndrome: From the Marfan eye consortium of Chicago. Am. J. Ophthalmol. 2017, 177, 144–149. [Google Scholar] [CrossRef]
- Fuchs, J. Marfan syndrome and other systemic disorders with congenital ectopia lentis. A Danish national survey. Acta Paediatr. 1997, 86, 947–952. [Google Scholar] [CrossRef]
- Chandra, A.; Banerjee, P.J. Grading in ectopia lentis (GEL): A novel classification system. Br. J. Ophthalmol. 2013, 97, 7. [Google Scholar] [CrossRef] [PubMed]
- Waiswol, M.; Kasahara, N. Lens subluxation grading system: Predictive value for ectopia lentis surgical outcomes. Einstein 2009, 7, 81–87. [Google Scholar]
- De Saint Jean, M.; Bogotean, D. Marfan syndrome diagnosis by ophthalmologist. Predictive value of ectopia lentis in a genotyped population. ARVO Ann. Meet. Abstr. 2003, 44, 813. [Google Scholar]
- Traboulsi, E.I.; Apte, S.S. Ectopia Lentis and Associated Systemic Disease. Genetic Diseases of the Eye, 2nd ed.; Oxford University Press: Oxford, UK, 2011; pp. 689–711. [Google Scholar]
- Wang, X.; Dong, J. Effect of pupil dilation on biometric measurements and intracular lens power calculations in schoolchildren. PLoS ONE 2018, 13, e0203677. [Google Scholar] [CrossRef]
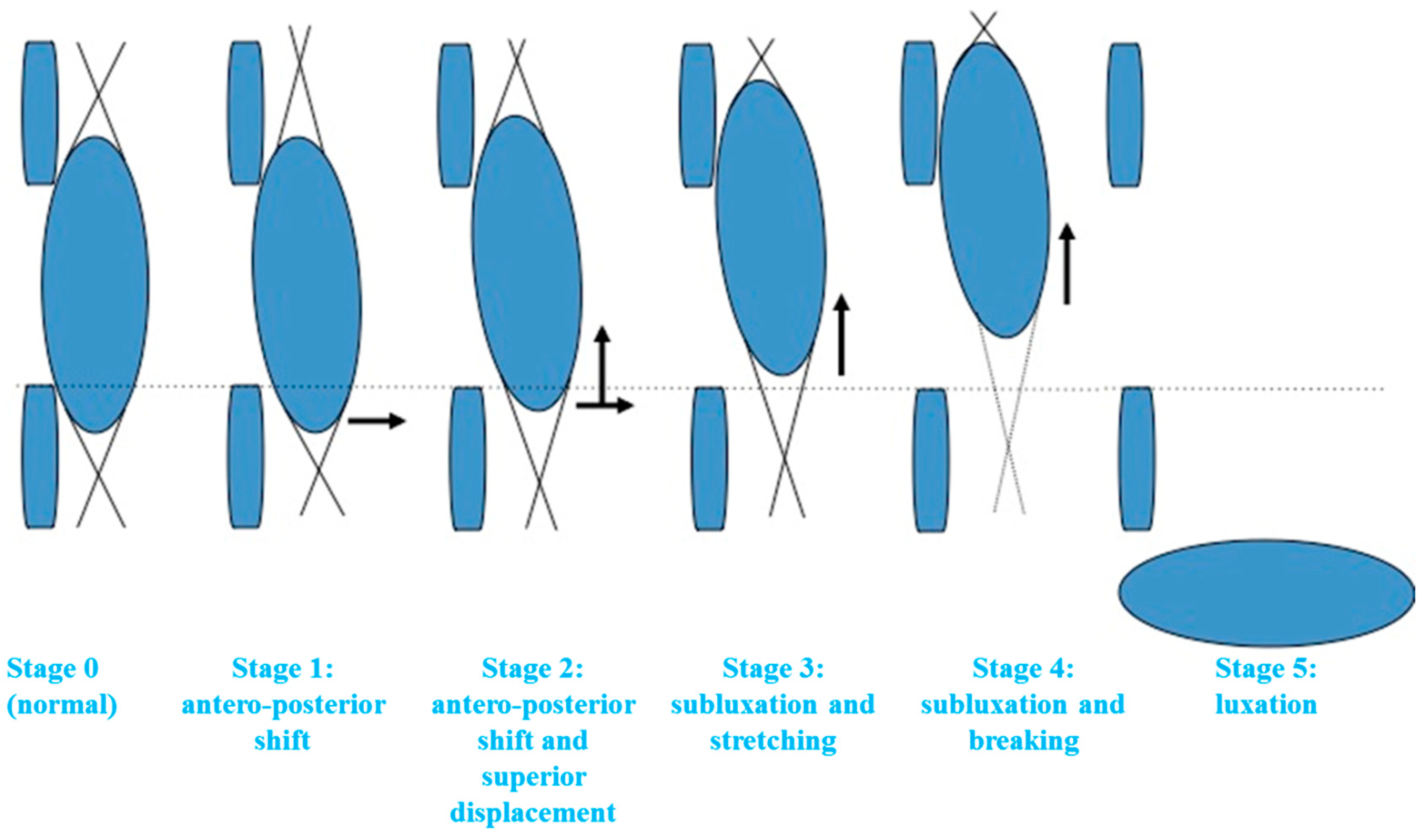
| Eye in Primary Position | Gaze Directed Down | |
|---|---|---|
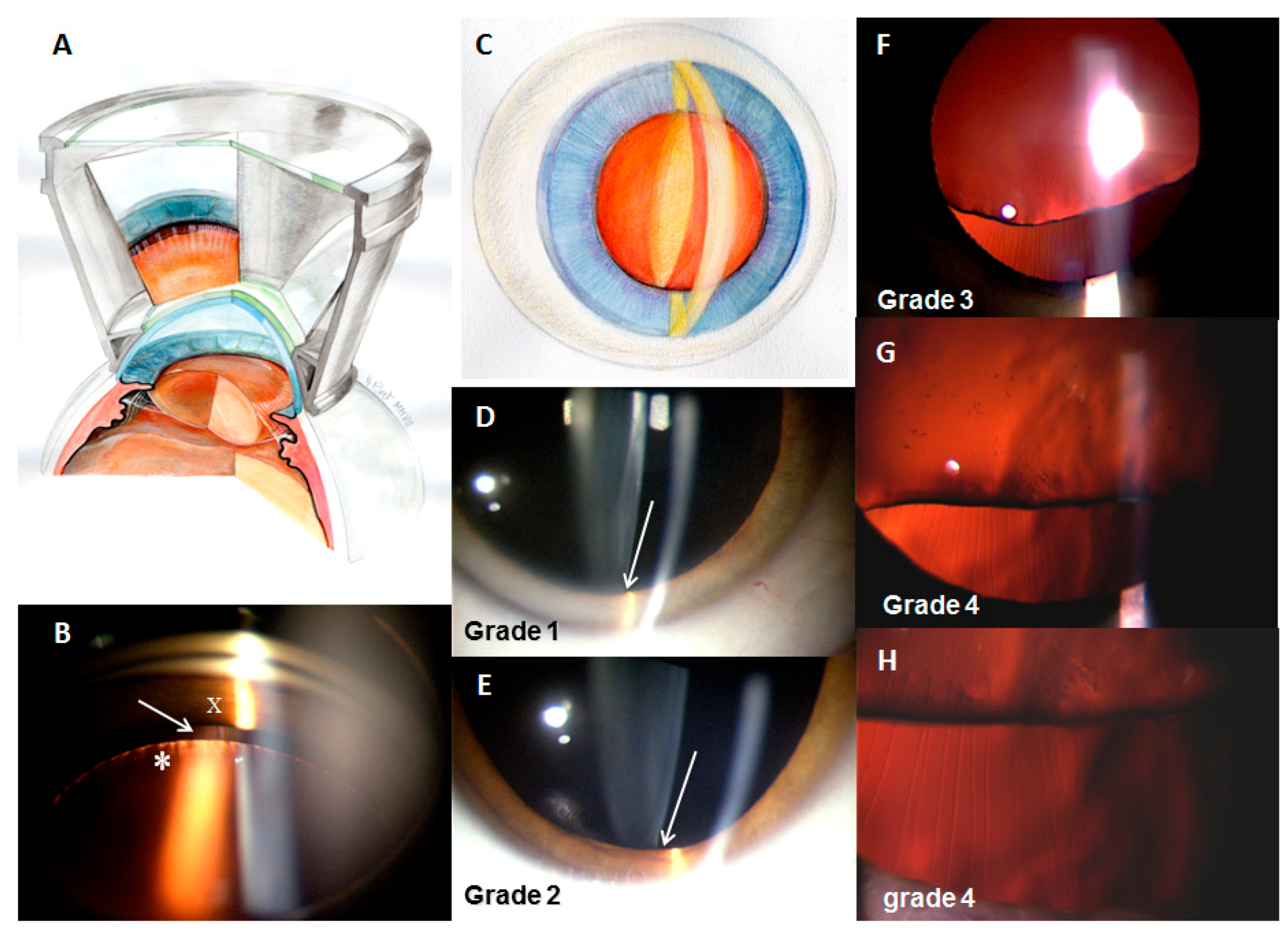
| Grade 1 (Figure 2D) Minimal shift | Anteroposterior shift in the inferior equatorial part of the lens resulting in a minimal space in an inferior position, between the posterior surface of the iris and the anterior wall of the equatorial part of the lens. No visualization of the equatorial zonular fibers. | Visualization of a space and sometimes of some zonular fibers |
| Grade 2 (Figure 2E) Shift and superior displacement | Anteroposterior displacement of the inferior part of the lens was associated with its superior displacement. Peripheral adherence of the zonule on the inferior part of the lens became visible, whereas it is normally masked by the iris. The inferior part of the lens was not visible in primary gaze. | Visualization of the equatorial part of the lens |
| Grade 3 (Figure 2F) Subluxation and stretching | Evident superior displacement of the lens with visualization of the equatorial part. Inferior zonular fibers are stretched but not broken, well seen on direct retina reflection. The density of fibers appears normal. Visual acuity can be deteriorated. | – |
| Grade 4 (Figure 2G,H) Subluxation and breaking | Breaking of some zonular fibers; the few unbroken fibers adopt a wavy appearance. Density of the fibers decrease. Inferior side of the lens becomes irregular because of modification of zonular tension. We were sometimes able to observe phacodonesis with the ocular movements. | – |
| Grade 5 Total luxation | Lens can be visualized in the vitreous, at the peripheral inferior region. | – |
| Overall | MFS Group | Control Group | |
|---|---|---|---|
| Number (n) | 110 | 74 | 36 |
| Sex (M/F) | 56/54 | 39/35 | 17/19 |
| Mean age at examination | – | 25.3 (3.8–54.8) | 38.5 (7.9–64.4) |
| Grade | MFS Group n = 74 (%) | Mean Age at Examination (Min–Max) | Control Group n = 36 (%) | Mean Age at Examination (Min–Max) |
|---|---|---|---|---|
| Normal (0) | 11 (14.8) | 35 (14–55) | 30 (83.3) | 30 (8–64) |
| 1 | 15 (20.3) | 28 (7–52) | 6 (16.7) | 21 (15–40) |
| 2 | 24 (32.4) | 25 (6–46) | 0 (0) | – |
| 3 | 17 (23.0) | 19 (6–47) | 0 (0) | – |
| 4 | 7 (9.5) | 20 (4–31) | 0 (0) | – |
| 5 | 0 (0) | – | 0 (0) | – |
| Total EL | 63 (85.1) | 23 (4–52) | 6 (16.7) | 21 (15–40) |
| Sensitivity | Specificity | Predictive Values | ||||
|---|---|---|---|---|---|---|
| Thresholds | n | % (CI *) | n | % (CI *) | Positive % (CI *) | Negative % (CI *) |
| ≥grade 3 | 24/74 | 32.4 (22–44.3) | 36/36 | 100 (90.3–100) | 100 (85.8–100) | 41.9 (31.3–53) |
| ≥grade 2 | 48/74 | 64.9 (52.9–75.6) | 36/36 | 100 (90.3–100) | 100 (92.6–100) | 58.1 (44.8–70.5) |
| ≥grade 1 | 63/74 | 85.1 (75–92.3) | 30/36 | 83.3 (67.2–93.6) | 91.3 (82–96.7) | 73.2 (57.1–85.8) |
| Initial Grade | Number of Patients (Percentage) with Follow Up in the Center | Ophthalmic Evolution Number of Patients (Age at Initial Examination) and Evolution |
|---|---|---|
| Grade 0 (n = 11) | n = 6 (54%) | 3 patients (14, 41, 43 yo) = no change (3, 7, and 10 years after initial examination) |
| 1 patient (55 yo) = glaucoma | ||
| 1 patient (14 yo) = grade 1 (9 years after initial examination) | ||
| 1 patient (17 yo) = grade 2 (10 years after initial examination) | ||
| Grade 1 (n = 15) | n = 10 (67%) | 7 patients (7 to 30 y) = no change (2 to 7 years after initial examination) |
| 1 patient (52 yo) = grade 2 (5 years after initial examination) | ||
| 1 patient (18 yo) = grade 3 (5 years after initial examination) | ||
| 1 patient (48 yo) = EL surgery (following a chock, 5 years after initial examination) | ||
| Grade 2 (n = 24) | n = 14 (58%) | 12 patients (6 to 35 yo) = no change (1 to 12 years after initial examination) |
| 2 patients (20, 22 yo) = grade 3 (6 years after initial examination) | ||
| Grade 3 (n = 17) | n = 17 (100%) | 12 patients (6 to 33 yo) = no change (2 to 8 years after initial examination) |
| 1 patient (47 yo) = cataract (3 years after initial examination) | ||
| 1 patient (9 yo) = grade 4 (8 years after initial examination) | ||
| 1 patient (17 yo) = RD surgery (2 years after initial examination) | ||
| 2 patients (13, 16 yo) = EL surgery (1 and 2 years after initial examination) | ||
| Grade 4 (n = 7) | n = 7 (100%) | 3 patients (25, 28, 30 yo) = no change (4, 6, and 9 years after initial examination) |
| 2 patients (4, 17 yo) = EL surgery (1 year after initial examination for both) | ||
| 2 patients (7, 31 yo) = RD surgery (4 and 6 years after initial examination) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zech, J.-C.; Putoux, A.; Decullier, E.; Fargeton, A.-E.; Edery, P.; Plauchu, H.; Dupuis-Girod, S. Classifying Ectopia Lentis in Marfan Syndrome into Five Grades of Increasing Severity. J. Clin. Med. 2020, 9, 721. https://doi.org/10.3390/jcm9030721
Zech J-C, Putoux A, Decullier E, Fargeton A-E, Edery P, Plauchu H, Dupuis-Girod S. Classifying Ectopia Lentis in Marfan Syndrome into Five Grades of Increasing Severity. Journal of Clinical Medicine. 2020; 9(3):721. https://doi.org/10.3390/jcm9030721
Chicago/Turabian StyleZech, Jean-Christophe, Audrey Putoux, Evelyne Decullier, Anne-Emmanuelle Fargeton, Patrick Edery, Henri Plauchu, and Sophie Dupuis-Girod. 2020. "Classifying Ectopia Lentis in Marfan Syndrome into Five Grades of Increasing Severity" Journal of Clinical Medicine 9, no. 3: 721. https://doi.org/10.3390/jcm9030721
APA StyleZech, J.-C., Putoux, A., Decullier, E., Fargeton, A.-E., Edery, P., Plauchu, H., & Dupuis-Girod, S. (2020). Classifying Ectopia Lentis in Marfan Syndrome into Five Grades of Increasing Severity. Journal of Clinical Medicine, 9(3), 721. https://doi.org/10.3390/jcm9030721





