Comparison of Machine Learning Computed Tomography-Based Fractional Flow Reserve and Coronary CT Angiography-Derived Plaque Characteristics with Invasive Resting Full-Cycle Ratio
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Population
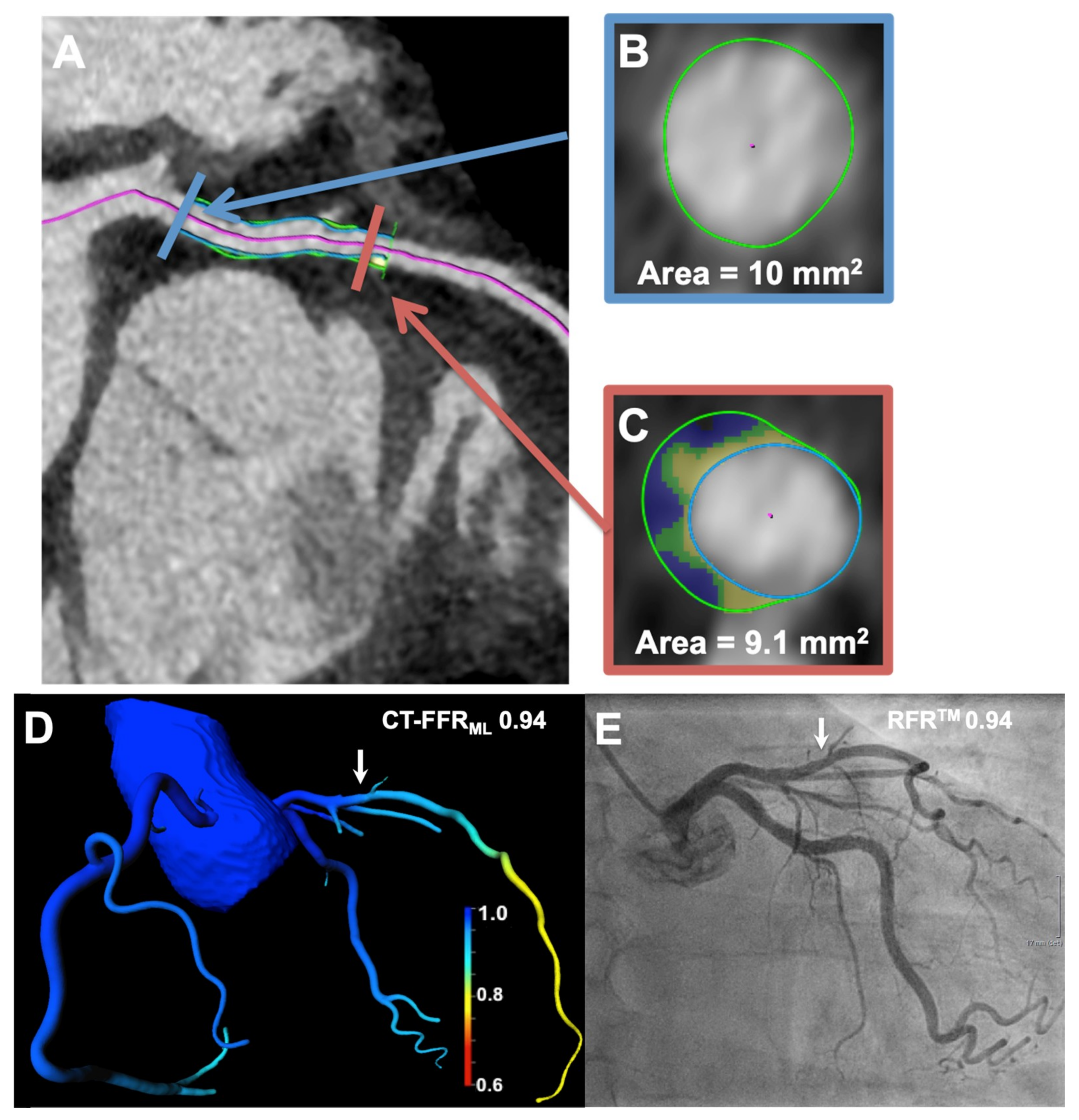
2.2. Acquisition and Analysis of cCTA Datasets
2.3. Analysis of Machine Learning Computed Tomography-Based Fractional Flow Reserve and Computed Tomographic Morphological Plaque Characteristics
2.4. Invasive Coronary Angiography and Resting Full Cycle Ratio Measurement
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chang, H.J.; Lin, F.Y.; Lee, S.E.; Andreini, D.; Bax, J.; Cademartiri, F.; Chinnaiyan, K.; Chow, B.J.W.; Conte, E.; Cury, R.C.; et al. Coronary Atherosclerotic Precursors of Acute Coronary Syndromes. J. Am. Coll. Cardiol. 2018, 71, 2511–2522. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Renker, M.; Schoepf, U.J.; Wichmann, J.L.; Fuller, S.R.; Rier, J.D.; Bayer, R.R., 2nd; Steinberg, D.H.; De Cecco, C.N.; Baumann, S. Diagnostic value of quantitative stenosis predictors with coronary CT angiography compared to invasive fractional flow reserve. Eur. J. Radiol. 2015, 84, 1509–1515. [Google Scholar] [CrossRef] [PubMed]
- Tesche, C.; De Cecco, C.N.; Caruso, D.; Baumann, S.; Renker, M.; Mangold, S.; Dyer, K.T.; Varga-Szemes, A.; Baquet, M.; Jochheim, D.; et al. Coronary CT angiography derived morphological and functional quantitative plaque markers correlated with invasive fractional flow reserve for detecting hemodynamically significant stenosis. J. Cardiovasc. Comput. Tomogr. 2016, 10, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Renker, M.; Schoepf, U.J.; Becher, T.; Krampulz, N.; Kim, W.; Rolf, A.; Mollmann, H.; Hamm, C.W.; Henzler, T.; Borggrefe, M.; et al. Computed tomography in patients with chronic stable angina: Fractional flow reserve measurement. Herz 2017, 42, 51–57. [Google Scholar] [CrossRef]
- Baumann, S.; Renker, M.; Schoepf, U.J. Coronary Computed Tomography-Based Fractional Flow Reserve: A Rapidly Developing Field. Jama Cardiol. 2018, 3, 87. [Google Scholar] [CrossRef]
- Baumann, S.; Wang, R.; Schoepf, U.J.; Steinberg, D.H.; Spearman, J.V.; Bayer, R.R., 2nd; Hamm, C.W.; Renker, M. Coronary CT angiography-derived fractional flow reserve correlated with invasive fractional flow reserve measurements--initial experience with a novel physician-driven algorithm. Eur. Radiol. 2015, 25, 1201–1207. [Google Scholar] [CrossRef]
- Coenen, A.; Kim, Y.H.; Kruk, M.; Tesche, C.; De Geer, J.; Kurata, A.; Lubbers, M.L.; Daemen, J.; Itu, L.; Rapaka, S.; et al. Diagnostic Accuracy of a Machine-Learning Approach to Coronary Computed Tomographic Angiography-Based Fractional Flow Reserve: Result From the MACHINE Consortium. Circ. Cardiovasc. Imaging 2018, 11, e007217. [Google Scholar] [CrossRef]
- Tesche, C.; De Cecco, C.N.; Baumann, S.; Renker, M.; McLaurin, T.W.; Duguay, T.M.; Bayer, R.R., 2nd; Steinberg, D.H.; Grant, K.L.; Canstein, C.; et al. Coronary CT Angiography-derived Fractional Flow Reserve: Machine Learning Algorithm versus Computational Fluid Dynamics Modeling. Radiology 2018, 288, 64–72. [Google Scholar] [CrossRef]
- Yu, M.; Lu, Z.; Li, W.; Wei, M.; Yan, J.; Zhang, J. CT morphological index provides incremental value to machine learning based CT-FFR for predicting hemodynamically significant coronary stenosis. Int. J. Cardiol. 2018, 265, 256–261. [Google Scholar] [CrossRef]
- Renker, M.; Schoepf, U.J.; Wang, R.; Meinel, F.G.; Rier, J.D.; Bayer, R.R., 2nd; Mollmann, H.; Hamm, C.W.; Steinberg, D.H.; Baumann, S. Comparison of diagnostic value of a novel noninvasive coronary computed tomography angiography method versus standard coronary angiography for assessing fractional flow reserve. Am. J. Cardiol. 2014, 114, 1303–1308. [Google Scholar] [CrossRef]
- Baumann, S.; Hirt, M.; Schoepf, U.J.; Rutsch, M.; Tesche, C.; Renker, M.; Golden, J.W.; Buss, S.J.; Becher, T.; Bojara, W.; et al. Correlation of machine learning computed tomography-based fractional flow reserve with instantaneous wave free ratio to detect hemodynamically significant coronary stenosis. Clin. Res. Cardiol. Off. J. Ger. Card. Soc. 2019. [Google Scholar] [CrossRef] [PubMed]
- Gotberg, M.; Christiansen, E.H.; Gudmundsdottir, I.J.; Sandhall, L.; Danielewicz, M.; Jakobsen, L.; Olsson, S.E.; Ohagen, P.; Olsson, H.; Omerovic, E.; et al. Instantaneous Wave-free Ratio versus Fractional Flow Reserve to Guide PCI. New Engl. J. Med. 2017, 376, 1813–1823. [Google Scholar] [CrossRef] [PubMed]
- Xaplanteris, P.; Fournier, S.; Pijls, N.H.J.; Fearon, W.F.; Barbato, E.; Tonino, P.A.L.; Engstrom, T.; Kaab, S.; Dambrink, J.H.; Rioufol, G.; et al. Five-Year Outcomes with PCI Guided by Fractional Flow Reserve. New Engl. J. Med. 2018, 379, 250–259. [Google Scholar] [CrossRef] [PubMed]
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2018. [Google Scholar] [CrossRef]
- Davies, J.E.; Sen, S.; Dehbi, H.M.; Al-Lamee, R.; Petraco, R.; Nijjer, S.S.; Bhindi, R.; Lehman, S.J.; Walters, D.; Sapontis, J.; et al. Use of the Instantaneous Wave-free Ratio or Fractional Flow Reserve in PCI. New Engl. J. Med. 2017, 376, 1824–1834. [Google Scholar] [CrossRef]
- Svanerud, J.; Ahn, J.M.; Jeremias, A.; van ’t Veer, M.; Gore, A.; Maehara, A.; Crowley, A.; Pijls, N.H.J.; De Bruyne, B.; Johnson, N.P.; et al. Validation of a novel non-hyperaemic index of coronary artery stenosis severity: The Resting Full-cycle Ratio (VALIDATE RFR) study. EuroIntervention 2018, 14, 806–814. [Google Scholar] [CrossRef]
- Lee, J.M.; Choi, K.H.; Park, J.; Hwang, D.; Rhee, T.M.; Kim, J.; Park, J.; Kim, H.Y.; Jung, H.W.; Cho, Y.K.; et al. Physiological and Clinical Assessment of Resting Physiological Indexes. Circulation 2019, 139, 889–900. [Google Scholar] [CrossRef]
- Bittencourt, M.S.; Hulten, E.; Polonsky, T.S.; Hoffman, U.; Nasir, K.; Abbara, S.; Di Carli, M.; Blankstein, R. European Society of Cardiology-Recommended Coronary Artery Disease Consortium Pretest Probability Scores More Accurately Predict Obstructive Coronary Disease and Cardiovascular Events Than the Diamond and Forrester Score: The Partners Registry. Circulation 2016, 134, 201–211. [Google Scholar] [CrossRef]
- Leipsic, J.; Abbara, S.; Achenbach, S.; Cury, R.; Earls, J.P.; Mancini, G.J.; Nieman, K.; Pontone, G.; Raff, G.L. SCCT guidelines for the interpretation and reporting of coronary CT angiography: A report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J. Cardiovasc. Comput. Tomogr. 2014, 8, 342–358. [Google Scholar] [CrossRef]
- van Rosendael, A.R.; Shaw, L.J.; Xie, J.X.; Dimitriu-Leen, A.C.; Smit, J.M.; Scholte, A.J.; van Werkhoven, J.M.; Callister, T.Q.; DeLago, A.; Berman, D.S.; et al. Superior Risk Stratification With Coronary Computed Tomography Angiography Using a Comprehensive Atherosclerotic Risk Score. Jacc Cardiovasc. Imaging 2019. [Google Scholar] [CrossRef]
- Agatston, A.S.; Janowitz, W.R.; Hildner, F.J.; Zusmer, N.R.; Viamonte, M., Jr.; Detrano, R. Quantification of coronary artery calcium using ultrafast computed tomography. J. Am. Coll Cardiol. 1990, 15, 827–832. [Google Scholar] [CrossRef]
- Wang, R.; Baumann, S.; Schoepf, U.J.; Meinel, F.G.; Rier, J.D.; Morris, J.Z.; Mollmann, H.; Hamm, C.W.; Steinberg, D.H.; Renker, M. Comparison of quantitative stenosis characteristics at routine coronary computed tomography angiography with invasive fractional flow reserve for assessing lesion-specific ischemia. J. Cardiovasc. Comput. Tomogr. 2015, 9, 546–552. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, S.; Ropers, D.; Hoffmann, U.; MacNeill, B.; Baum, U.; Pohle, K.; Brady, T.J.; Pomerantsev, E.; Ludwig, J.; Flachskampf, F.A.; et al. Assessment of coronary remodeling in stenotic and nonstenotic coronary atherosclerotic lesions by multidetector spiral computed tomography. J. Am. Coll. Cardiol. 2004, 43, 842–847. [Google Scholar] [CrossRef] [PubMed]
- Norgaard, B.L.; Leipsic, J.; Gaur, S.; Seneviratne, S.; Ko, B.S.; Ito, H.; Jensen, J.M.; Mauri, L.; De Bruyne, B.; Bezerra, H.; et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: The NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J. Am. Coll. Cardiol. 2014, 63, 1145–1155. [Google Scholar] [CrossRef]
- Escaned, J.; Echavarria-Pinto, M.; Garcia-Garcia, H.M.; van de Hoef, T.P.; de Vries, T.; Kaul, P.; Raveendran, G.; Altman, J.D.; Kurz, H.I.; Brechtken, J.; et al. Prospective Assessment of the Diagnostic Accuracy of Instantaneous Wave-Free Ratio to Assess Coronary Stenosis Relevance: Results of ADVISE II International, Multicenter Study (ADenosine Vasodilator Independent Stenosis Evaluation II). Jacc Cardiovasc. Interv. 2015, 8, 824–833. [Google Scholar] [CrossRef]
- Meijboom, W.B.; Meijs, M.F.; Schuijf, J.D.; Cramer, M.J.; Mollet, N.R.; van Mieghem, C.A.; Nieman, K.; van Werkhoven, J.M.; Pundziute, G.; Weustink, A.C.; et al. Diagnostic accuracy of 64-slice computed tomography coronary angiography: A prospective, multicenter, multivendor study. J. Am. Coll. Cardiol. 2008, 52, 2135–2144. [Google Scholar] [CrossRef]
- Patel, M.R.; Peterson, E.D.; Dai, D.; Brennan, J.M.; Redberg, R.F.; Anderson, H.V.; Brindis, R.G.; Douglas, P.S. Low diagnostic yield of elective coronary angiography. New Engl. J. Med. 2010, 362, 886–895. [Google Scholar] [CrossRef]
- Patel, M.R.; Dai, D.; Hernandez, A.F.; Douglas, P.S.; Messenger, J.; Garratt, K.N.; Maddox, T.M.; Peterson, E.D.; Roe, M.T. Prevalence and predictors of nonobstructive coronary artery disease identified with coronary angiography in contemporary clinical practice. Am. Heart J. 2014, 167, 846–852.e842. [Google Scholar] [CrossRef]
- Baumann, S.; Ozdemir, G.H.; Tesche, C.; Schoepf, U.J.; Golden, J.W.; Becher, T.; Hirt, M.; Weiss, C.; Renker, M.; Akin, I.; et al. Coronary CT angiography derived plaque markers correlated with invasive instantaneous flow reserve for detecting hemodynamically significant coronary stenoses. Eur. J. Radiol. 2019, 122, 108744. [Google Scholar] [CrossRef]
- Min, J.K.; Leipsic, J.; Pencina, M.J.; Berman, D.S.; Koo, B.K.; van Mieghem, C.; Erglis, A.; Lin, F.Y.; Dunning, A.M.; Apruzzese, P.; et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. Jama 2012, 308, 1237–1245. [Google Scholar] [CrossRef]
- Koo, B.K.; Erglis, A.; Doh, J.H.; Daniels, D.V.; Jegere, S.; Kim, H.S.; Dunning, A.; DeFrance, T.; Lansky, A.; Leipsic, J.; et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J. Am. Coll. Cardiol. 1997, 58, 1989–1997. [Google Scholar] [CrossRef]
- Driessen, R.S.; de Waard, G.A.; Stuijfzand, W.J.; Raijmakers, P.G.; Danad, I.; Bom, M.J.; Min, J.K.; Leipsic, J.A.; Ahmadi, A.; van de Ven, P.M.; et al. Adverse Plaque Characteristics Relate More Strongly With Hyperemic Fractional Flow Reserve and Instantaneous Wave-Free Ratio Than With Resting Instantaneous Wave-Free Ratio. Jacc Cardiovasc. Imaging 2019. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Mean Value ± Standard Deviation, Frequency (%) or Interquartile Range |
|---|---|
| Age (years) | 68 ± 12 |
| Men | 23 (70%) |
| Body mass index (kg/m2) | 29 ± 5 |
| Pretest probability (%) + | 57 ± 19 |
| Cardiovascular Risk Factors | |
| Hypertension * | 26 (78%) |
| Hyperlipidemia † | 18 (54%) |
| Diabetes mellitus | 8 (24%) |
| Family history of coronary artery disease | 8 (24%) |
| Current smoker | 4 (12%) |
| Coronary Computed Tomography | |
| Agatston score | 800 (35–3608) |
| Luminal stenosis > 70% | 14 (32%) |
| Leiden cCTA risk score | 12 ± 5 |
| CT-FFRML ≤ 0.80 π | 13 (30%) |
| Invasive Coronary Catheter Angiography | |
| Left anterior descending coronary artery π | 26 (59%) |
| Left circumflex coronary artery π | 10 (23%) |
| Right coronary artery π | 8 (18%) |
| RFRTM ≤ 0.89 π | 14 (32%) |
| Parameter | All Lesions | Lesions RFRTM > 0.89 | LesionsRFRTM ≤ 0.89 | p-Value |
|---|---|---|---|---|
| Number of Lesions | 44 | 30 | 14 | - |
| Morphological computed tomographic morphological plaque characteristics | ||||
| LL/MLD4 | 11.0 ± 6.2 | 8.8 ± 4.0 | 15.7 ± 7.6 | 0.0016 * |
| MLD (mm) | 1.8 ± 0.8 | 2.0 ± 0.8 | 1.4 ± 0.7 | 0.0038 * |
| Degree of luminal diameter stenosis (%) | 50.3 ± 28.6 | 42.9 ± 26.3 | 66.4 ± 27.4 | 0.0063 * |
| MLA (mm2) | 4.8 ± 3.5 | 5.5 ± 3.4 | 3.5 ± 3.3 | 0.0078 * |
| cCTA stenosis > 50% | 26 | 14 | 12 | 0.0141 * |
| cCTA stenosis > 70% | 14 | 6 | 8 | 0.0341 * |
| TPV (mm3) | 116.1 ± 76.2 | 101.4 ± 66.3 | 147.5 ± 88.5 | 0.0989 |
| VV (mm3) | 200.7 ± 117.0 | 189.0 ± 115.7 | 225.7 ± 120.0 | 0.3710 |
| LL (mm) | 17.0 ± 7.4 | 16.5 ± 8.1 | 18.2 ± 5.7 | 0.4421 |
| Functional computed tomographic morphological plaque characteristics | ||||
| CT-FFRML | 0.87 ± 0.14 | 0.94 ± 0.05 | 0.72 ± 0.15 | <0.0001 ** |
| RI | 1.20 ± 0.28 | 1.12 ± 0.23 | 1.38 ± 0.29 | 0.0062 * |
| CCO | 0.13 ± 0.12 | 0.14 ± 0.13 | 0.13 ± 0.08 | 0.6770 |
| Per Lesion (n = 44) | ||||||
|---|---|---|---|---|---|---|
| Sensitivity (%) (95% CI) | Specificity (%) (95% CI) | PPV (%) (95% CI) | NPV (%) (95% CI) | Accuracy (%) (95% CI) | AUC (95% CI) | |
| Morphological Computed Tomographic Morphological Plaque Characteristics | ||||||
| LL/MLD4 | 71 (42–92) | 77 (58–90) | 59 (33–82) | 85 (66–96) | 75 (60–87) | 0.80 (0.64–0.96) |
| MLD (mm2) | 64 (35–87) | 80 (61–92) | 60 (32–84) | 83 (64–94) | 75 (59–87) | 0.77 (0.62–0.93) |
| Degree of luminal diameter stenosis (%) | 71 (42–92) | 77 (58–90) | 59 (33–82) | 85 (66–96) | 75 (59–87) | 0.75 (0.58–0.94) |
| MLA (mm2) | 71 (42–92) | 80 (61–92) | 62 (35–85) | 86 (67–96) | 77 (62–88) | 0.75 (0.57–0.94) |
| cCTA (<50%) | 86 (57–98) | 53 (34–72) | 46 (27–67) | 89 (65–98) | 63 (48–78) | 0.69 (0.56–0.83) |
| cCTA (<70%) | 57 (29–82) | 80 (61–92) | 57 (29–82) | 80 (61–92) | 73 (57–85) | 0.69 (0.53–0.84) |
| Functional Computed Tomographic Morphological Plaque Characteristics | ||||||
| CT-FFRML | 86 (57–98) | 97 (88–99) | 92 (74–99) | 94 (79–99) | 93 (81–98) | 0.90 (0.75–1.00) |
| RI | 71 (42–92) | 67 (47–83) | 50 (27–73) | 83 (63–95) | 68 (52–81) | 0.76 (0.61–0.91) |
| Per Patient (n = 33) | ||||||
| Morphological Computed Tomographic Morphological Plaque Characteristics | ||||||
| LL/MLD4 | 75 (73–94) | 71 (48–84) | 60 (32–84) | 83 (59–96) | 73 (55–87) | 0.78 (0.57–0.99) |
| MLA (mm2) | 67 (35–90) | 71 (48–89) | 57 (29–82) | 79 (54–94) | 70 (51–84) | 0.70 (0.48–0.93) |
| MLD (mm2) | 58 (28–85) | 71 (48–89) | 54 (25–81) | 75 (51–91) | 67 (48–82) | 0.70 (0.50–0.90) |
| Degree of luminal diameter stenosis (%) | 67 (35–93) | 67 (43–85) | 53 (27–79) | 78 (52–94) | 67 (48–82) | 0.68 (0.46–0.89) |
| cCTA (<50%) | 83 (52–98) | 62 (39–82) | 44 (23–65) | 80 (44–98) | 55 (36–72) | 0.60 (0.45–0.76) |
| cCTA (<70%) | 50 (21–79) | 71 (48–89) | 50 (21–79) | 71 (48–88) | 64 (45–80) | 0.60 (0.42–0.78) |
| Functional Computed Tomographic Morphological Plaque Characteristics | ||||||
| CT-FFRML | 83 (52–98) | 95 (76–99) | 91 (59–99) | 91 (71–99) | 91 (76–98) | 0.87 (0.70–1.00) |
| RI | 67 (35–90) | 52 (30–74) | 44 (21–69) | 73 (45–92) | 58 (39–74) | 0.70 (0.51–0.89) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baumann, S.; Hirt, M.; Rott, C.; Özdemir, G.H.; Tesche, C.; Becher, T.; Weiss, C.; Hetjens, S.; Akin, I.; Schoenberg, S.O.; et al. Comparison of Machine Learning Computed Tomography-Based Fractional Flow Reserve and Coronary CT Angiography-Derived Plaque Characteristics with Invasive Resting Full-Cycle Ratio. J. Clin. Med. 2020, 9, 714. https://doi.org/10.3390/jcm9030714
Baumann S, Hirt M, Rott C, Özdemir GH, Tesche C, Becher T, Weiss C, Hetjens S, Akin I, Schoenberg SO, et al. Comparison of Machine Learning Computed Tomography-Based Fractional Flow Reserve and Coronary CT Angiography-Derived Plaque Characteristics with Invasive Resting Full-Cycle Ratio. Journal of Clinical Medicine. 2020; 9(3):714. https://doi.org/10.3390/jcm9030714
Chicago/Turabian StyleBaumann, Stefan, Markus Hirt, Christina Rott, Gökce H. Özdemir, Christian Tesche, Tobias Becher, Christel Weiss, Svetlana Hetjens, Ibrahim Akin, Stefan O. Schoenberg, and et al. 2020. "Comparison of Machine Learning Computed Tomography-Based Fractional Flow Reserve and Coronary CT Angiography-Derived Plaque Characteristics with Invasive Resting Full-Cycle Ratio" Journal of Clinical Medicine 9, no. 3: 714. https://doi.org/10.3390/jcm9030714
APA StyleBaumann, S., Hirt, M., Rott, C., Özdemir, G. H., Tesche, C., Becher, T., Weiss, C., Hetjens, S., Akin, I., Schoenberg, S. O., Borggrefe, M., Janssen, S., Overhoff, D., & Lossnitzer, D. (2020). Comparison of Machine Learning Computed Tomography-Based Fractional Flow Reserve and Coronary CT Angiography-Derived Plaque Characteristics with Invasive Resting Full-Cycle Ratio. Journal of Clinical Medicine, 9(3), 714. https://doi.org/10.3390/jcm9030714






