Treatment of Somatosensory Tinnitus: A Randomized Controlled Trial Studying the Effect of Orofacial Treatment as Part of a Multidisciplinary Program
Abstract
1. Introduction
2. Methods
2.1. Patients
2.2. Intervention
2.2.1. Information and Advice
2.2.2. Orofacial Treatment
2.3. Study Design
2.4. Outcome Measures
2.4.1. Primary Outcome Measure
2.4.2. The Secondary Outcome Measures
2.5. Sample Size and Power
2.6. Randomization and Blinding
2.7. Ethical Approval and Consent
2.8. Statistics
3. Results
3.1. Patients
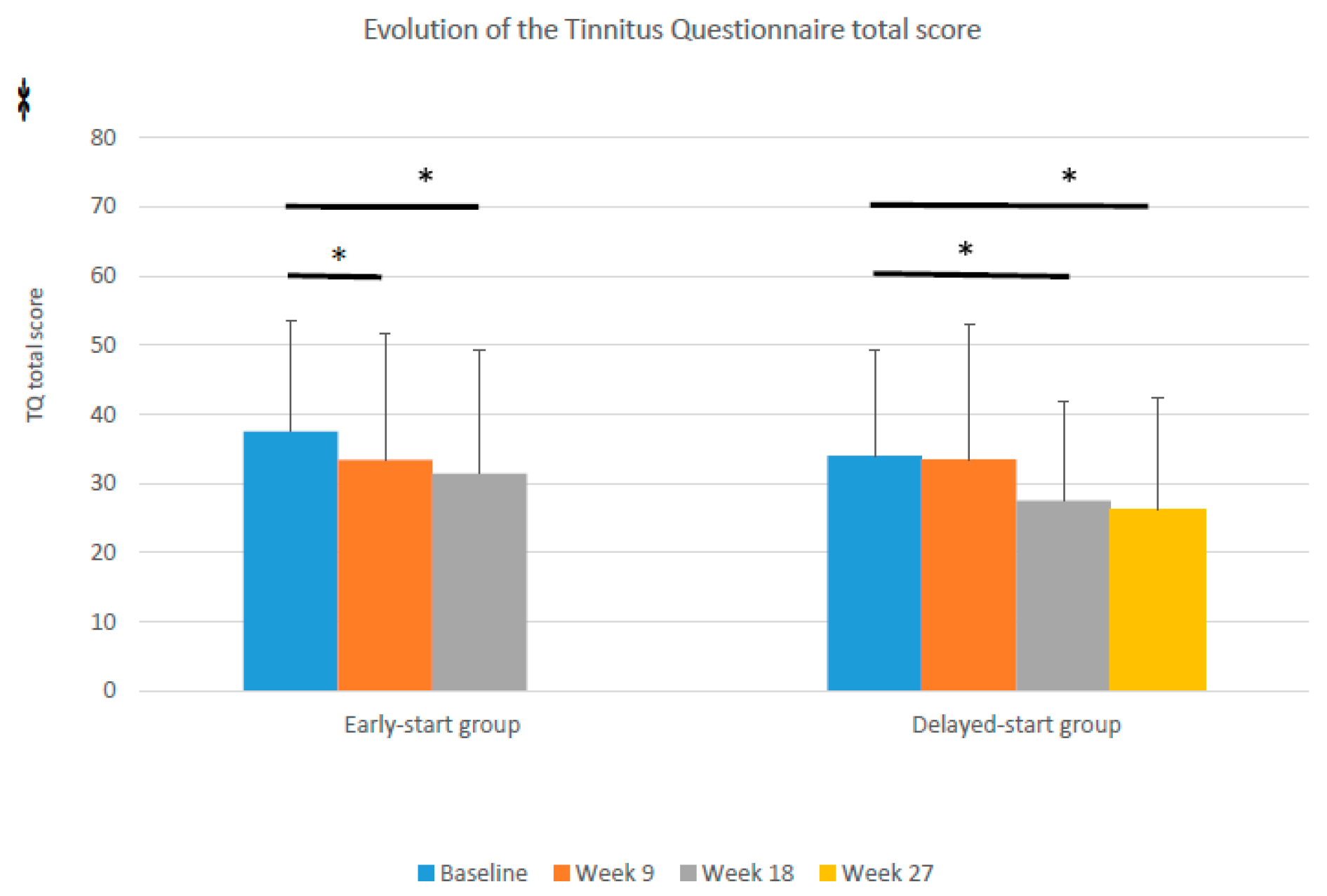
3.2. TQ Responses to Treatment (Primary Outcome)
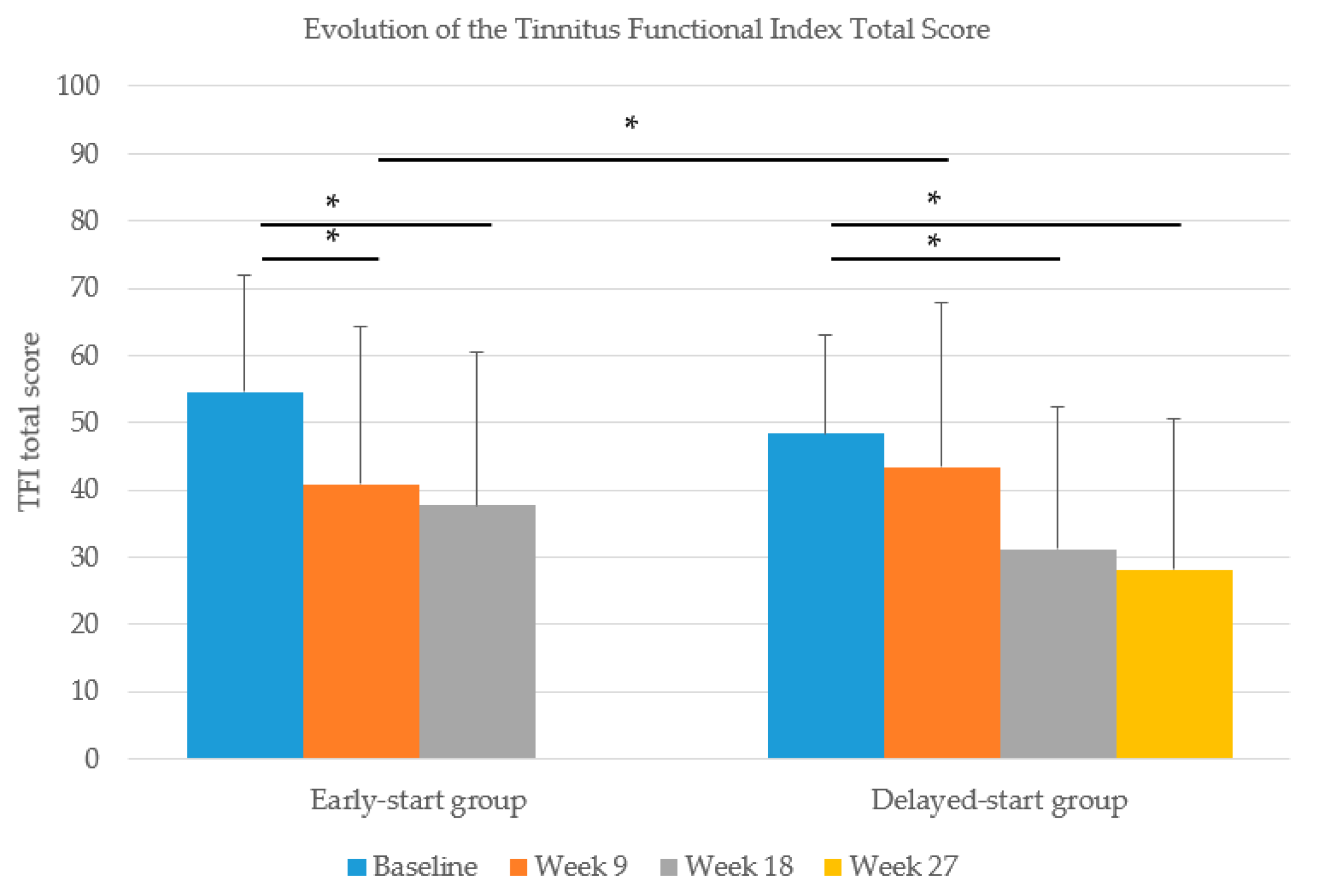
3.3. TFI Responses to Treatment (Secondary Outcome)
3.4. Clinically Relevant Improvement
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Baguley, D.; McFerran, D.; Hall, D. Tinnitus. Lancet 2013, 382, 1600–1607. [Google Scholar] [CrossRef]
- Cima, R.F.F.; Mazurek, B.; Haider, H.; Kikidis, D.; Lapira, A.; Noreña, A.; Hoare, D.J. A multidisciplinary European guideline for tinnitus: Diagnostics, assessment, and treatment. HNO 2019, 67, 10–42. [Google Scholar] [CrossRef] [PubMed]
- Teachey, W.S.; Wijtmans, E.H.; Cardarelli, F.; A Levine, R. Tinnitus of myofascial origin. Int. Tinnitus J. 2012, 17, 73–76. [Google Scholar]
- Saldanha, A.D.; Hilgenberg, P.B.; Pinto, L.M.; Conti, P.C. Are temporomandibular disorders and tinnitus associated? CRANIO 2012, 30, 166–171. [Google Scholar] [CrossRef]
- Michiels, S.; Harrison, S.; Vesala, M.; Schlee, W.; Aslam, M.S.; Carvalho, D. The Presence of Physical Symptoms in Patients with Tinnitus: International Web-Based Survey. Interact. J. Med. Res. 2019, 8, e14519. [Google Scholar] [CrossRef]
- Michiels, S.; Sanchez, T.G.; Oron, Y.; Gilles, A.; Haider, H.; Erlandsson, S.; Bechter, K.; Vielsmeier, V.; Biesinger, E.; Nam, E.-C.; et al. Diagnostic Criteria for Somatosensory Tinnitus: A Delphi Process and Face-to-Face Meeting to Establish Consensus. Trends Hear. 2018, 22, 2331216518796403. [Google Scholar] [CrossRef]
- Michiels, S.; De Hertogh, W.; Truijen, S.; Van De Heyning, P. Physical therapy treatment in patients suffering from cervicogenic somatic tinnitus: Study protocol for a randomized controlled trial. Trials 2014, 15, 297. [Google Scholar] [CrossRef][Green Version]
- Ralli, M.; Greco, A.; Turchetta, R.; Altissimi, G.; De Vincentiis, M.; Cianfrone, G. Somatosensory tinnitus: Current evidence and future perspectives. J. Int. Med Res. 2017, 45, 933–947. [Google Scholar] [CrossRef]
- Kanold, P.O.; Young, E.D. Proprioceptive Information from the Pinna Provides Somatosensory Input to Cat Dorsal Cochlear Nucleus. J. Neurosci. 2001, 21, 7848–7858. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Leketas, M.; Šaferis, V.; Kubilius, R.; Cervino, G.; Bramanti, E.; Cicciù, M. Oral Behaviors and Parafunctions. J. Craniofacial Surg. 2017, 28, 1933–1938. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, S.E.F.; Ohrbach, R. Self-Report of Waking-State Oral Parafunctional Behaviors in the Natural Environment. J. Oral Facial Pain Headache 2016, 30, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Olivo, M.; Ferronato, G.; Marchese, R.; Martini, A.; Nardini, L.G. Prevalence of tinnitus in patients with different temporomandibular disorders symptoms. Int. Tinnitus J. 2015, 19, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Lam, D.K.; Lawrence, H.P.; Tenenbaum, H.C. Aural symptoms in temporomandibular disorder patients attending a craniofacial pain unit. J. Orofac. Pain 2001, 15, 146–157. [Google Scholar]
- Erlandsson, S.I.; Rubinstein, B.; Carlsson, S.G. Tinnitus: Evaluation of biofeedback and stomatognathic treatment. Br. J. Audiol. 1991, 25, 151–161. [Google Scholar] [CrossRef]
- Tullberg, M.; Ernberg, M. Long-term effect on tinnitus by treatment of temporomandibular disorders: A two-year follow-up by questionnaire. Acta Odontol. Scand. 2006, 64, 89–96. [Google Scholar] [CrossRef]
- Bosel, C.; Mazurek, B.; Haupt, H.; Peroz, I. Chronic tinnitus and craniomandibular disorders. Effectiveness of functional therapy on perceived tinnitus distress. HNO 2008, 56, 707–713. [Google Scholar]
- Michiels, S.; Naessens, S.; Van De Heyning, P.; Braem, M.; Visscher, C.M.; Gilles, A.; De Hertogh, W. The Effect of Physical Therapy Treatment in Patients with Subjective Tinnitus: A Systematic Review. Front. Mol. Neurosci. 2016, 10, 545. [Google Scholar] [CrossRef]
- Michiels, S.; Nieste, E.; Van De Heyning, P.; Braem, M.; Visscher, C.; Topsakal, V.; Gilles, A.; Jacquemin, L.; De Hertogh, W. Does Conservative Temporomandibular Therapy Affect Tinnitus Complaints? A Systematic Review. J. Oral Facial Pain Headache 2019, 33, 308–317. [Google Scholar] [CrossRef]
- Van De Heyning, P.; Gilles, A.; Rabau, S.; Van Rompaey, V. Subjective tinnitus assessment and treatment in clinical practice. Curr. Opin. Otolaryngol. Head Neck Surg. 2015, 23, 369–375. [Google Scholar] [CrossRef]
- Meikle, M.B.; Henry, J.A.; Griest, S.E.; Stewart, B.J.; Abrams, H.B.; McArdle, R.; Myers, P.J.; Newman, C.W.; Sandridge, S.; Turk, D.C.; et al. The tinnitus functional index: Development of a new clinical measure for chronic, intrusive tinnitus. Ear Hear. 2012, 33, 153–176. [Google Scholar] [CrossRef] [PubMed]
- De Laat, A.; Meuleman, H.; Stevens, A.; Verbeke, G. Correlation between cervical spine and temporomandibular disorders. Clin. Oral Investig. 1998, 2, 54–57. [Google Scholar] [CrossRef] [PubMed]
- Calixtre, L.B.; Grüninger, B.L.D.S.; Haik, M.N.; Alburquerque-Sendín, F.; Oliveira, A.B. Effects of cervical mobilization and exercise on pain, movement and function in subjects with temporomandibular disorders: A single group pre-post test. J. Appl. Oral Sci. 2016, 24, 188–197. [Google Scholar] [CrossRef] [PubMed]
- De Wijer, A.; Steenks, M.; De Leeuw, J.; Bosman, F.; Helders, P. Symptoms of the cervical spine in temporomandibular and cervical spine disorders. J. Oral Rehabil. 1996, 23, 742–750. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R. Critical Commentary 2: Reliability and Validity of the DC/TMD Axis I. J. Oral Facial Pain Headache 2018, 32, 22–24. [Google Scholar] [CrossRef]
- Gil-Martinez, A.; Paris-Alemany, A.; López-De-Uralde-Villanueva, I.; La Touche, R. Management of pain in patients with temporomandibular disorder (TMD): Challenges and solutions. J. Pain Res. 2018, 11, 571–587. [Google Scholar] [CrossRef]
- Michiels, S.; Van Der Wal, A.C.; Nieste, E.; Van De Heyning, P.; Braem, M.; Visscher, C.; Topsakal, V.; Gilles, A.; Jacquemin, L.; Hesters, M.; et al. Conservative therapy for the treatment of patients with somatic tinnitus attributed to temporomandibular dysfunction: Study protocol of a randomised controlled trial. Trials 2018, 19, 554. [Google Scholar] [CrossRef]
- Zeman, F.; Koller, M.; Schecklmann, M.; Langguth, B.; Landgrebe, M. Tinnitus assessment by means of standardized self-report questionnaires: Psychometric properties of the Tinnitus Questionnaire (TQ), the Tinnitus Handicap Inventory (THI), and their short versions in an international and multi-lingual sample. Heal. Qual. Life Outcomes 2012, 10, 128. [Google Scholar] [CrossRef]
- Jacquemin, L.; Mertens, G.; Van De Heyning, P.; Vanderveken, O.M.; Topsakal, V.; De Hertogh, W.; Michiels, S.; Van Rompaey, V.; Gilles, A.; Laure, J.; et al. Sensitivity to change and convergent validity of the Tinnitus Functional Index (TFI) and the Tinnitus Questionnaire (TQ): Clinical and research perspectives. Hear. Res. 2019, 382, 107796. [Google Scholar] [CrossRef]
- Jacquemin, L.; Mertens, G.; Van De Heyning, P.; Vanderveken, O.M.; Topsakal, V.; De Hertogh, W.; Michiels, S.; Beyers, J.; Moyaert, J.; Van Rompaey, V.; et al. An Exploratory Study on the Use of Event-Related Potentials as an Objective Measure of Auditory Processing and Therapy Effect in Patients with Tinnitus: A Transcranial Direct Current Stimulation Study. Otol. Neurotol. 2019, 40, e868–e875. [Google Scholar] [CrossRef]
- Cima, R.F.F. Bothersome tinnitus: Cognitive behavioral perspectives. HNO 2018, 66, 369–374. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Early-Start Group | Delayed-Start Group | Total | p Value | Statistic Test | Value | Df |
|---|---|---|---|---|---|---|---|
| Number of subjects | 40 | 40 | 80 | ||||
| Gender male/female | 18/22 (45%/55%) | 24/16 (60%/40%) | 42/38 (53%/47%) | 0.168 | Chi-square | 1.805 | 1 |
| Age in years (SD) | 46 (13) | 45 (15) | 45 (14) | 0.769 | t-test | 0.294 | 78 |
| TQ (SD) | 37 (16) | 34 (15) | 36 (16) | 0.345 | t-test | 0.951 | 75 |
| TFI (SD) | 55 (17) | 48(15) | 52 (16) | 0.086 | t-test | 1.741 | 78 |
| TQ degree | |||||||
| % degree 1 | 30% | 49% | 39% | ||||
| % degree 2 | 40% | 30% | 35% | 0.376 | Chi-square | 3.105 | 3 |
| % degree 3 | 15% | 13% | 14% | ||||
| % degree 4 | 15% | 8% | 12% | ||||
| VAS mean loudness tinnitus right ear (SD) | 50 (30) | 49 (25) | 49 (27) | 0.835 | t-test | 0.209 | 78 |
| VAS mean loudness tinnitus left ear (SD) | 46 (31) | 45 (26) | 45 (28) | 0.858 | t-test | 0.180 | 78 |
| TMD pain screener (percentage < 3/percentage ≥ 3) | 35%/65% | 35%/65% | 40%/60% | 0.272 | Chi-square | 7.561 | 6 |
| HQ (SD) | 17 (8) | 19 (9) | 18 (8) | 0.958 | t-test | −0.053 | 76 |
| HADS anxiety (SD) | 9 (4) | 8 (4) | 9 (4) | 0.076 | t-test | 1.695 | 77 |
| HADS depression (SD) | 7 (5) | 5 (4) | 6 (5) | 0.257 | t-test | 1.429 | 75 |
| Fletcher index left (SD) | 13 (17) | 11 (11) | 13 (17) | 0.725 | t-test | 0.135 | 78 |
| Fletcher index right (SD) | 11 (10) | 13 (14) | 11 (12) | 0.359 | t-test | −1.254 | 76 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
van der Wal, A.; Michiels, S.; Van de Heyning, P.; Braem, M.; Visscher, C.M.; Topsakal, V.; Gilles, A.; Jacquemin, L.; Van Rompaey, V.; De Hertogh, W. Treatment of Somatosensory Tinnitus: A Randomized Controlled Trial Studying the Effect of Orofacial Treatment as Part of a Multidisciplinary Program. J. Clin. Med. 2020, 9, 705. https://doi.org/10.3390/jcm9030705
van der Wal A, Michiels S, Van de Heyning P, Braem M, Visscher CM, Topsakal V, Gilles A, Jacquemin L, Van Rompaey V, De Hertogh W. Treatment of Somatosensory Tinnitus: A Randomized Controlled Trial Studying the Effect of Orofacial Treatment as Part of a Multidisciplinary Program. Journal of Clinical Medicine. 2020; 9(3):705. https://doi.org/10.3390/jcm9030705
Chicago/Turabian Stylevan der Wal, Annemarie, Sarah Michiels, Paul Van de Heyning, Marc Braem, Corine M. Visscher, Vedat Topsakal, Annick Gilles, Laure Jacquemin, Vincent Van Rompaey, and Willem De Hertogh. 2020. "Treatment of Somatosensory Tinnitus: A Randomized Controlled Trial Studying the Effect of Orofacial Treatment as Part of a Multidisciplinary Program" Journal of Clinical Medicine 9, no. 3: 705. https://doi.org/10.3390/jcm9030705
APA Stylevan der Wal, A., Michiels, S., Van de Heyning, P., Braem, M., Visscher, C. M., Topsakal, V., Gilles, A., Jacquemin, L., Van Rompaey, V., & De Hertogh, W. (2020). Treatment of Somatosensory Tinnitus: A Randomized Controlled Trial Studying the Effect of Orofacial Treatment as Part of a Multidisciplinary Program. Journal of Clinical Medicine, 9(3), 705. https://doi.org/10.3390/jcm9030705







