Radiosynoviorthesis after Surgery in the Treatment of Patients with Ankle Pigmented Villonodular Synovitis: A Case Series
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
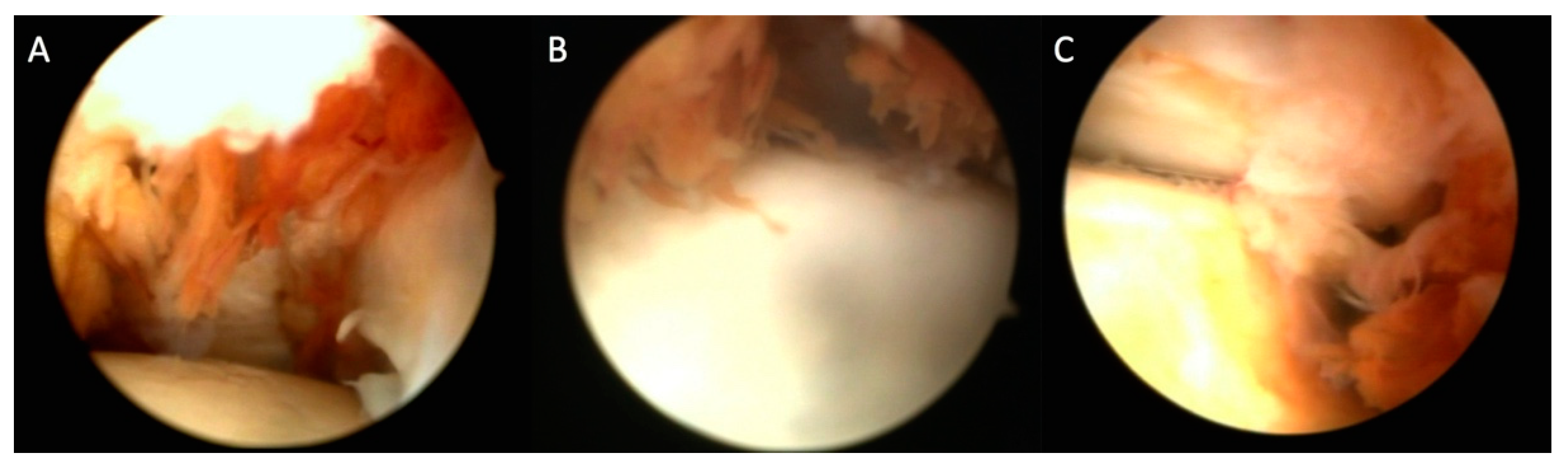
2.2. Synovectomy
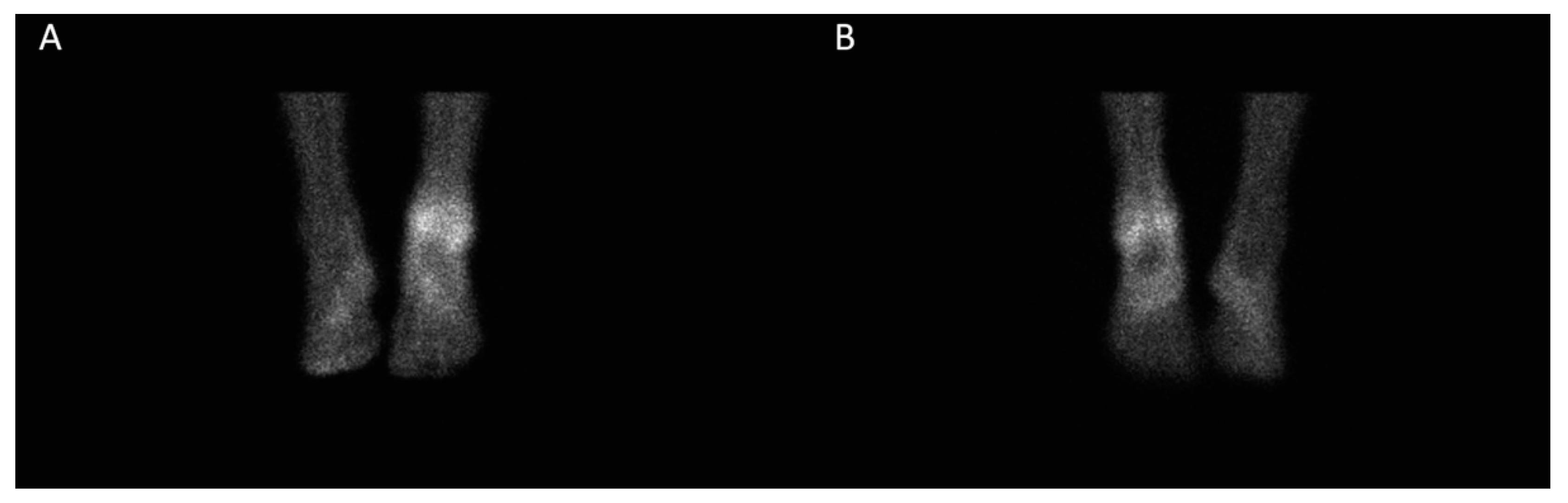
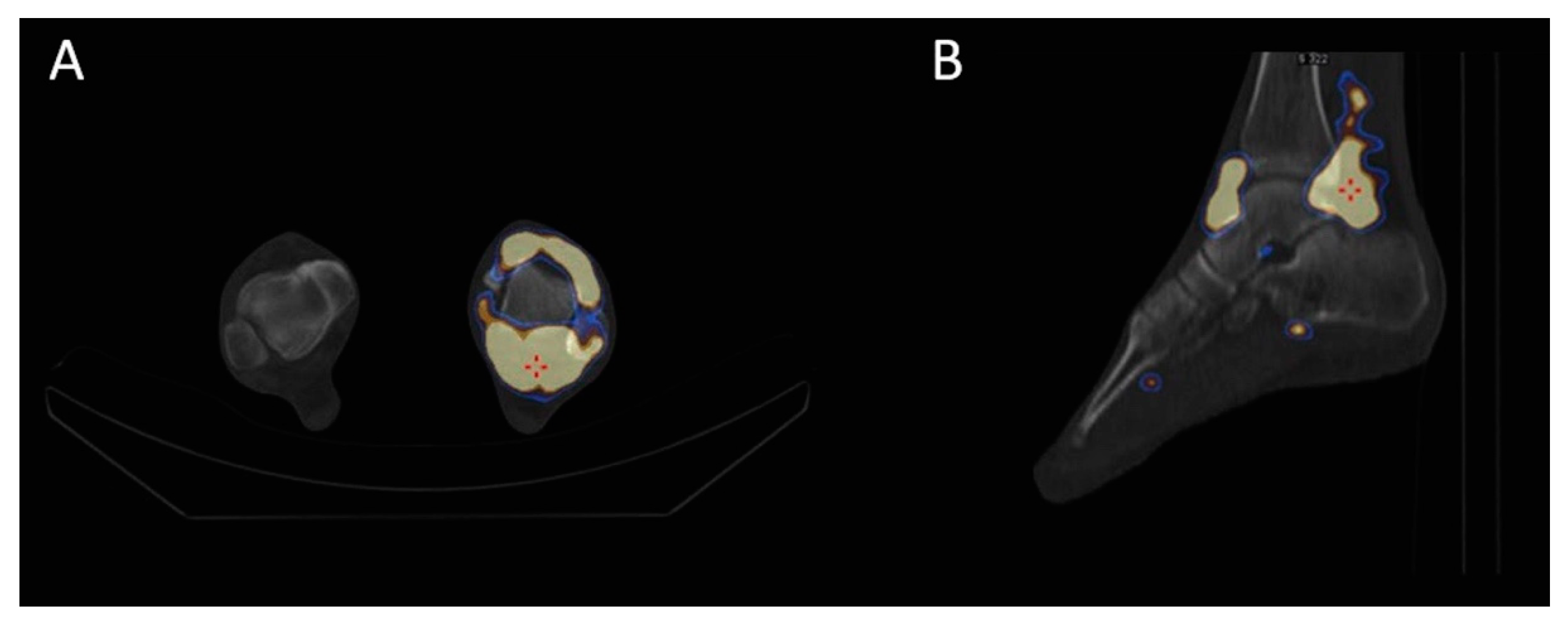
2.3. Radiosynoviorthesis (RSO)
2.4. Follow-Up
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Granowitz, S.P.; D’Antonio, J.; Mankin, H.L. The pathogenesis and long-term end results of pigmented villonodular synovitis. Clin. Orthop. Relat. Res. 1976, 114, 335–351. [Google Scholar]
- Dorwart, R.H.; Genant, H.K.; Johnston, W.H.; Morris, J.M. Pigmented villonodular synovitis of synovial joints: Clinical, pathologic, and radiologic features. AJR Am. J. Roentgenol. 1984, 143, 877–885. [Google Scholar] [CrossRef] [PubMed]
- Sharma, H.; Jane, M.J.; Reid, R. Pigmented villonodular synovitis of the foot and ankle: Forty years of experience from the Scottish bone tumor registry. J. Foot Ankle Surg. 2006, 45, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Rochwerger, A.; Groulier, P.; Curvale, G.; Launay, F. Pigmented villonodular synovitis of the foot and ankle: A report of eight cases. Foot Ankle Int. 1999, 20, 587–590. [Google Scholar] [CrossRef] [PubMed]
- Korim, M.T.; Clarke, D.R.; Allen, P.E.; Richards, C.J.; Ashford, R.U. Clinical and oncological outcomes after surgical excision of pigmented villonodular synovitis at the foot and ankle. Foot Ankle Surg. 2014, 20, 130–134. [Google Scholar] [CrossRef]
- Lee, M.; Mahroof, S.; Pringle, J.; Short, S.C.; Briggs, T.W.; Cannon, S.R. Diffuse pigmented villonodular synovitis of the foot and ankle treated with surgery and radiotherapy. Int. Orthop. 2005, 29, 403–405. [Google Scholar] [CrossRef] [PubMed]
- Tyler, W.K.; Vidal, A.F.; Williams, R.J.; Healey, J.H. Pigmented villonodular synovitis. J. Am. Acad. Orthop. Surg. 2006, 14, 376–385. [Google Scholar] [CrossRef]
- Van der Heijden, L.; Gibbons, C.L.; Dijkstra, P.D.; Kroep, J.R.; van Rijswijk, C.S.; Nout, R.A.; Bradley, K.M.; Athanasou, N.A.; Hogendoorn, P.C.; van de Sande, M.A. The management of diffuse-type giant cell tumour (pigmented villonodular synovitis) and giant cell tumour of tendon sheath (nodular tenosynovitis). J. Bone Joint Surg. Br. 2012, 94, 882–888. [Google Scholar] [CrossRef]
- O’Sullivan, B.; Cummings, B.; Catton, C.; Bell, R.; Davis, A.; Fornasier, V.; Goldberg, R. Outcome following radiation treatment for high-risk pigmented villonodular synovitis. Int. J. Radiat Oncol. Biol. Phys. 1995, 32, 777–786. [Google Scholar] [CrossRef]
- Brien, E.W.; Sacoman, D.M.; Mirra, J.M. Pigmented villonodular synovitis of the foot and ankle. Foot Ankle Int. 2008, 29, 527–533. [Google Scholar] [CrossRef]
- Schnirring-Judge, M.; Lin, B. Pigmented villonodular synovitis of the ankle-radiation therapy as a primary treatment to reduce recurrence: A case report with 8-year follow-up. J. Foot Ankle Surg. 2011, 50, 108–116. [Google Scholar] [CrossRef]
- Shabat, S.; Kollender, Y.; Merimsky, O.; Isakov, J.; Flusser, G.; Nyska, M.; Meller, I. The use of surgery and yttrium 90 in the management of extensive and diffuse pigmented villonodular synovitis of large joints. Rheumatology (Oxford) 2002, 41, 1113–1118. [Google Scholar] [CrossRef]
- Bickels, J.; Isaakov, J.; Kollender, Y.; Meller, I. Unacceptable complications following intra-articular injection of yttrium 90 in the ankle joint for diffuse pigmented villonodular synovitis. J. Bone Joint Surg Am. 2008, 90, 326–328. [Google Scholar] [CrossRef]
- Knut, L. Radiosynoviorthesis in the Therapeutic Management of Arthritis. World J. Nucl. Med. 2015, 14, 10–15. [Google Scholar] [CrossRef]
- Budiman-Mak, E.; Conrad, K.J.; Roach, K.E. The Foot Function Index: A measure of foot pain and disability. J. Clin. Epidemiol. 1991, 44, 561–570. [Google Scholar] [CrossRef]
- Kulig, K.; Reischl, S.F.; Pomrantz, A.B.; Burnfield, J.M.; Mais-Requejo, S.; Thordarson, D.B.; Smith, R.W. Nonsurgical Management of Posterior Tibial Tendon Dysfunction with Orthoses and Resistive Exercise: A Randomized Controlled Trial. Phys. Ther. 2009, 89, 26–37. [Google Scholar] [CrossRef]
- Haefeli, M.; Elfering, A. Pain assessment. Eur. Spine J. 2006, 15 (Suppl. 1), S17–S24. [Google Scholar] [CrossRef]
- Fellinger, K.; Schmid, J. Die lokale Behandlung der rheumatischen Erkrankungen. Wien. Z Inn Med. 1952, 33, 351–363. [Google Scholar]
- Van der Zant, F.M.; Boer, R.O.; Moolenburgh, J.D.; Jahangier, Z.N.; Bijlsma, J.W.; Jacobs, J.W. Radiation synovectomy with (90)Yttrium, (186)Rhenium and (169)Erbium: A systematic literature review with meta-analyses. Clin. Exp. Rheumatol. 2009, 27, 130–139. [Google Scholar]
- Schneider, P.; Farahati, J.; Reiners, C. Radiosynovectomy in rheumatology, orthopedics, and hemophilia. J. Nucl Med. 2005, 46 (Suppl. 1), 48S–54S. [Google Scholar]
- Chen, D.Y.; Lan, J.L.; Chou, S.J. Treatment of pigmented villonodular synovitis with yttrium-90: Changes in immunologic features, Tc-99m uptake measurements, and MR imaging of one case. Clin. Rheumatol 1992, 11, 280–285. [Google Scholar] [CrossRef]
- Kat, S.; Kutz, R.; Elbracht, T.; Weseloh, G.; Kuwert, T. Radiosynoviorthesis in pigmented villonodular synovitis. Nuklearmedizin 2000, 39, 209–213. [Google Scholar] [PubMed]
- Koca, G.; Ozsoy, H.; Atilgan, H.I.; Ozyurt, S.; Demirel, K.; Yiğit, H.; Korkmaz, M.; Baskin, A.; Sakaogullari, A.; Ozdemir, M. A low recurrence rate is possible with a combination of surgery and radiosynovectomy for diffuse pigmented villonodular synovitis of the knee. Clin. Nucl. Med. 2013, 38, 608–615. [Google Scholar] [CrossRef] [PubMed]

| Patient No | Gender | Age | Sport | Time between Synovectomy and RSO | Side-Effects | Duration of Follow-Up (Months) |
|---|---|---|---|---|---|---|
| 1 | F | 20 | rhythmic gymnastics | 3 months | None | 44 |
| 2 | F | 25 | track and field | 3 months | None | 47 |
| 3 | M | 36 | volleyball | 5 months | None | 54 |
| 4 | F | 28 | track and field | 4 months | None | 36 |
| 5 | M | 32 | football (soccer) | 3 months | Pain, edema (3 weeks) | 50 |
| Patient No | FFI Pre-RSO | FFI on January 2020 (Median Follow-Up: 44 Months) |
|---|---|---|
| 1 | 84.5% | 0.5% |
| 2 | 73.0% | 0.5% |
| 3 | 77.0% | 0% |
| 4 | 71% | 0.5% |
| 5 | 84.5% | 6% |
| Patient No | VAS Score Pre-RSO | VAS Score at 2 Months | VAS Score at 6 Months | VAS Score at 12 Months | VAS Score on January 2020 (Median Follow-Up: 44 Months) |
|---|---|---|---|---|---|
| 1 | 5 | 1 | 1 | 0 | 0 |
| 2 | 4 | 3 | 1 | 1 | 1 |
| 3 | 3 | 1 | 0 | 0 | 0 |
| 4 | 4 | 1 | 0 | 1 | 0 |
| 5 | 7 | 6 | 2 | 1 | 1 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iakovou, I.; Symeonidis, P.; Kotrotsios, D.; Giannoula, E.; Sachpekidis, C. Radiosynoviorthesis after Surgery in the Treatment of Patients with Ankle Pigmented Villonodular Synovitis: A Case Series. J. Clin. Med. 2020, 9, 597. https://doi.org/10.3390/jcm9020597
Iakovou I, Symeonidis P, Kotrotsios D, Giannoula E, Sachpekidis C. Radiosynoviorthesis after Surgery in the Treatment of Patients with Ankle Pigmented Villonodular Synovitis: A Case Series. Journal of Clinical Medicine. 2020; 9(2):597. https://doi.org/10.3390/jcm9020597
Chicago/Turabian StyleIakovou, Ioannis, Panagiotis Symeonidis, Dimitrios Kotrotsios, Evanthia Giannoula, and Christos Sachpekidis. 2020. "Radiosynoviorthesis after Surgery in the Treatment of Patients with Ankle Pigmented Villonodular Synovitis: A Case Series" Journal of Clinical Medicine 9, no. 2: 597. https://doi.org/10.3390/jcm9020597
APA StyleIakovou, I., Symeonidis, P., Kotrotsios, D., Giannoula, E., & Sachpekidis, C. (2020). Radiosynoviorthesis after Surgery in the Treatment of Patients with Ankle Pigmented Villonodular Synovitis: A Case Series. Journal of Clinical Medicine, 9(2), 597. https://doi.org/10.3390/jcm9020597







