Adult Migraine Hospital Admission Trends in Finland: A Nationwide Registry Study
Abstract
1. Introduction
2. Methods
2.1. Data Collection
2.2. Statistical Analyses
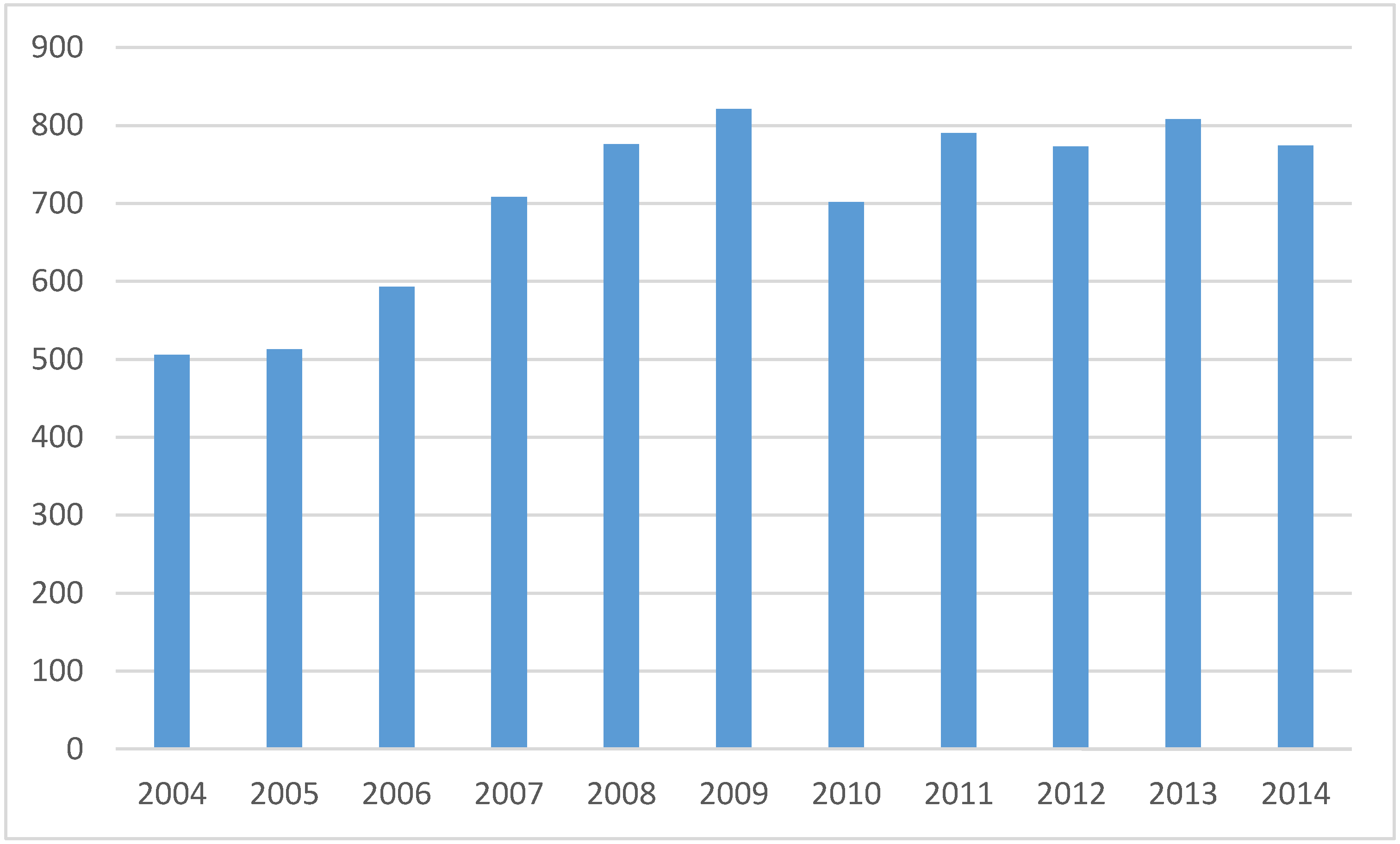
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- GBD 2016 Headache Collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018, 17, 954–976. [Google Scholar] [CrossRef]
- Vo, P.; Fang, J.; Bilitou, A.; Laflamme, A.K.; Gupta, S. Patients’ perspective on the burden of migraine in Europe: A cross-sectional analysis of survey data in France, Germany, Italy, Spain, and the United Kingdom. J. Headache Pain 2018, 19, 82. [Google Scholar] [CrossRef] [PubMed]
- Bonafede, M.; Sapra, S.; Shah, N.; Tepper, S.; Cappell, K.; Desai, P. Direct and Indirect Healthcare Resource Utilization and Costs among Migraine Patients in the United States. Headache 2018, 58, 700–714. [Google Scholar] [CrossRef] [PubMed]
- Steiner, T.J.; Stovner, L.J.; Katsarava, Z.; Lainez, J.M.; Lampl, C.; Lantéri-Minet, M.; Rastenyte, D.; de la Torre, E.R.; Tassorelli, C.; Barré, J.; et al. The impact of headache in Europe: Principal results of the Eurolight project. J. Headache Pain 2014, 15, 31. [Google Scholar] [CrossRef] [PubMed]
- Stang, P.E.; Osterhaus, J.T.; Celentano, D.D. Migraine. Patterns of healthcare use. Neurology 1994, 44, S47–S55. [Google Scholar] [PubMed]
- Korolainen, M.A.; Kurki, S.; Lassenius, M.I.; Toppila, I.; Costa-Scharplatz, M.; Purmonen, T.; Nissilä, M. Burden of migraine in Finland: Health care resource use, sick-leaves and comorbidities in occupational health care. J. Headache Pain 2019, 20, 13. [Google Scholar] [CrossRef] [PubMed]
- Nadarajan, V.; Perry, R.J.; Johnson, J.; Werring, D.J. Transient ischaemic attacks: Mimics and chameleons. Pract. Neurol. 2014, 14, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Terrin, A.; Toldo, G.; Ermani, M.; Mainardi, F.; Maggioni, F. When migraine mimics stroke: A systematic review. Cephalalgia 2018, 38, 2068–2078. [Google Scholar] [CrossRef] [PubMed]
- Liberman, A.L.; Prabhakaran, S. Stroke Chameleons and Stroke Mimics in the Emergency Department. Curr. Neurol. Neurosci. Rep. 2017, 17, 15. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef] [PubMed]
- Nuotio, J.; Oikonen, M.; Magnussen, C.G.; Jokinen, E.; Laitinen, T.; Hutri-Kähönen, N.; Kähönen, M.; Lehtimäki, T.; Taittonen, L.; Tossavainen, P.; et al. Cardiovascular risk factors in 2011 and secular trends since 2007: The Cardiovascular Risk in Young Finns Study. Scand. J. Public Health 2014, 42, 563–571. [Google Scholar] [CrossRef] [PubMed]
- Borodulin, K.; Vartiainen, E.; Peltonen, M.; Jousilahti, P.; Juolevi, A.; Laatikainen, T.; Männistö, S.; Salomaa, V.; Sundvall, J.; Puska, P. Forty-year trends in cardiovascular risk factors in Finland. Eur. J. Public Health 2015, 25, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Korja, M.; Lehto, H.; Juvela, S.; Kaprio, J. Incidence of subarachnoid hemorrhage is decreasing together with decreasing smoking rates. Neurology 2016, 87, 1118–1123. [Google Scholar] [CrossRef] [PubMed]
- Modi, S.Y.; Dharaiya, D.; Katramados, A.M.; Mitsias, P. Predictors of Prolonged Hospital Stay in Status Migrainosus. Neurohospitalist 2016, 6, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Magalhães, J.E.; Sampaio Rocha-Filho, P.A. Migraine and cerebrovascular diseases: Epidemiology, pathophysiological, and clinical considerations. Headache 2018, 58, 1277–1286. [Google Scholar] [CrossRef] [PubMed]
- Coutts, S.B.; Moreau, F.; Asdaghi, N.; Boulanger, J.M.; Camden, M.C.; Campbell, B.C.; Demchuk, A.M.; Field, T.S.; Goyal, M.; Krause, M.; et al. Rate and Prognosis of Brain Ischemia in Patients with Lower-Risk Transient or Persistent Minor Neurologic Events. JAMA Neurol 2019, 76, 1439–1445. [Google Scholar] [CrossRef] [PubMed]
- Sipilä, J.O.; Posti, J.P.; Ruuskanen, J.O.; Rautava, P.; Kytö, V. Stroke hospitalization trends of the working-aged in Finland. PLoS ONE 2018, 13, e0201633. [Google Scholar] [CrossRef] [PubMed]
- Organisation for Economic Co-Operation and Development Statistics. Available online: https://stats.oecd.org/index.aspx?queryid=30183# (accessed on 11 October 2019).
- Sund, R. Quality of the Finnish Hospital Discharge Register: A systematic review. Scand. J. Public Health 2012, 40, 505–515. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sipilä, J.O.T.; Ruuskanen, J.O.; Rautava, P.; Kytö, V. Adult Migraine Hospital Admission Trends in Finland: A Nationwide Registry Study. J. Clin. Med. 2020, 9, 320. https://doi.org/10.3390/jcm9020320
Sipilä JOT, Ruuskanen JO, Rautava P, Kytö V. Adult Migraine Hospital Admission Trends in Finland: A Nationwide Registry Study. Journal of Clinical Medicine. 2020; 9(2):320. https://doi.org/10.3390/jcm9020320
Chicago/Turabian StyleSipilä, Jussi O.T., Jori O. Ruuskanen, Päivi Rautava, and Ville Kytö. 2020. "Adult Migraine Hospital Admission Trends in Finland: A Nationwide Registry Study" Journal of Clinical Medicine 9, no. 2: 320. https://doi.org/10.3390/jcm9020320
APA StyleSipilä, J. O. T., Ruuskanen, J. O., Rautava, P., & Kytö, V. (2020). Adult Migraine Hospital Admission Trends in Finland: A Nationwide Registry Study. Journal of Clinical Medicine, 9(2), 320. https://doi.org/10.3390/jcm9020320





