Comparison of Ilizarov Bifocal, Acute Shortening and Relengthening with Bone Transport in the Treatment of Infected, Segmental Defects of the Tibia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Infection Definition
2.4. Tissue Sampling and Surgical Procedures
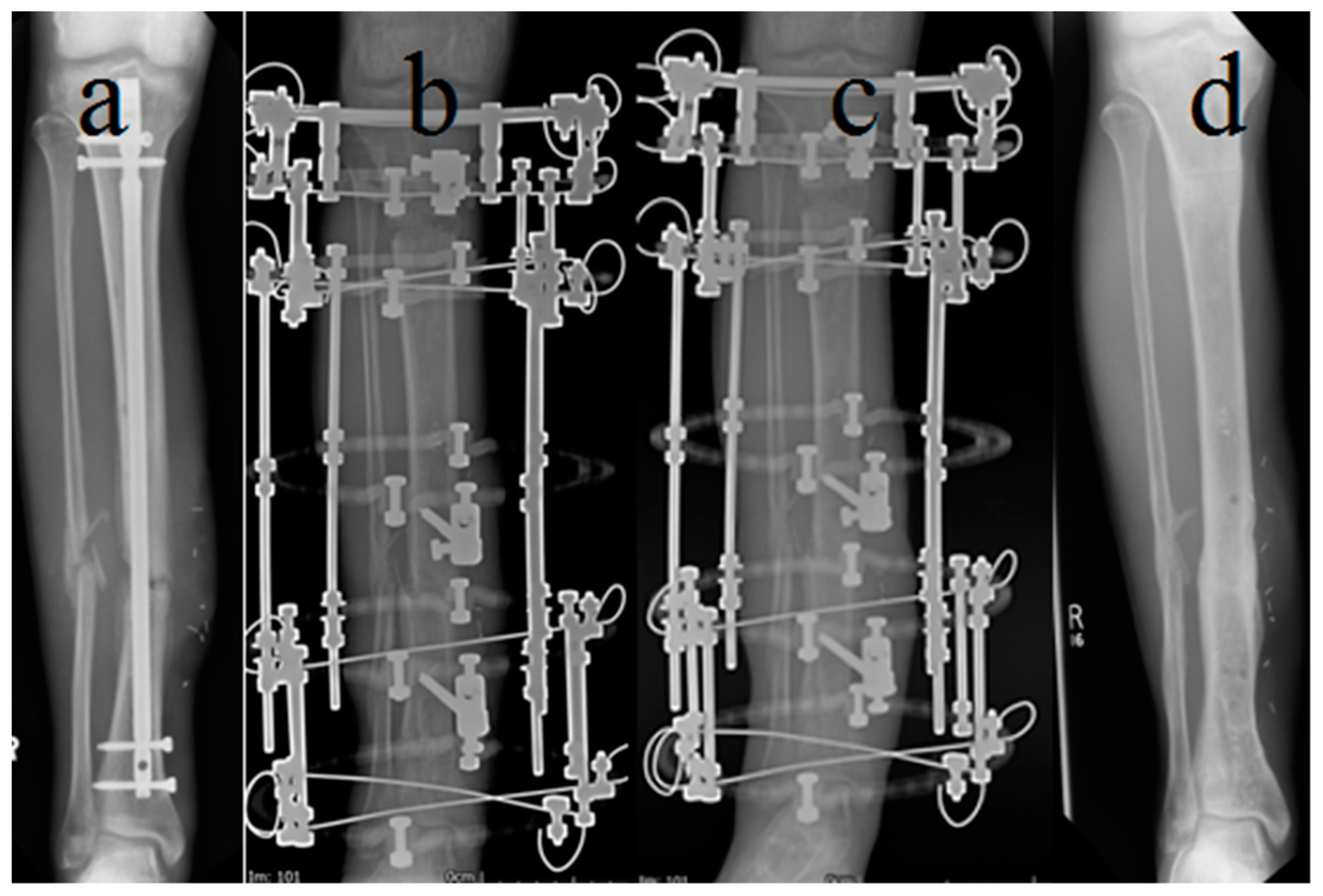
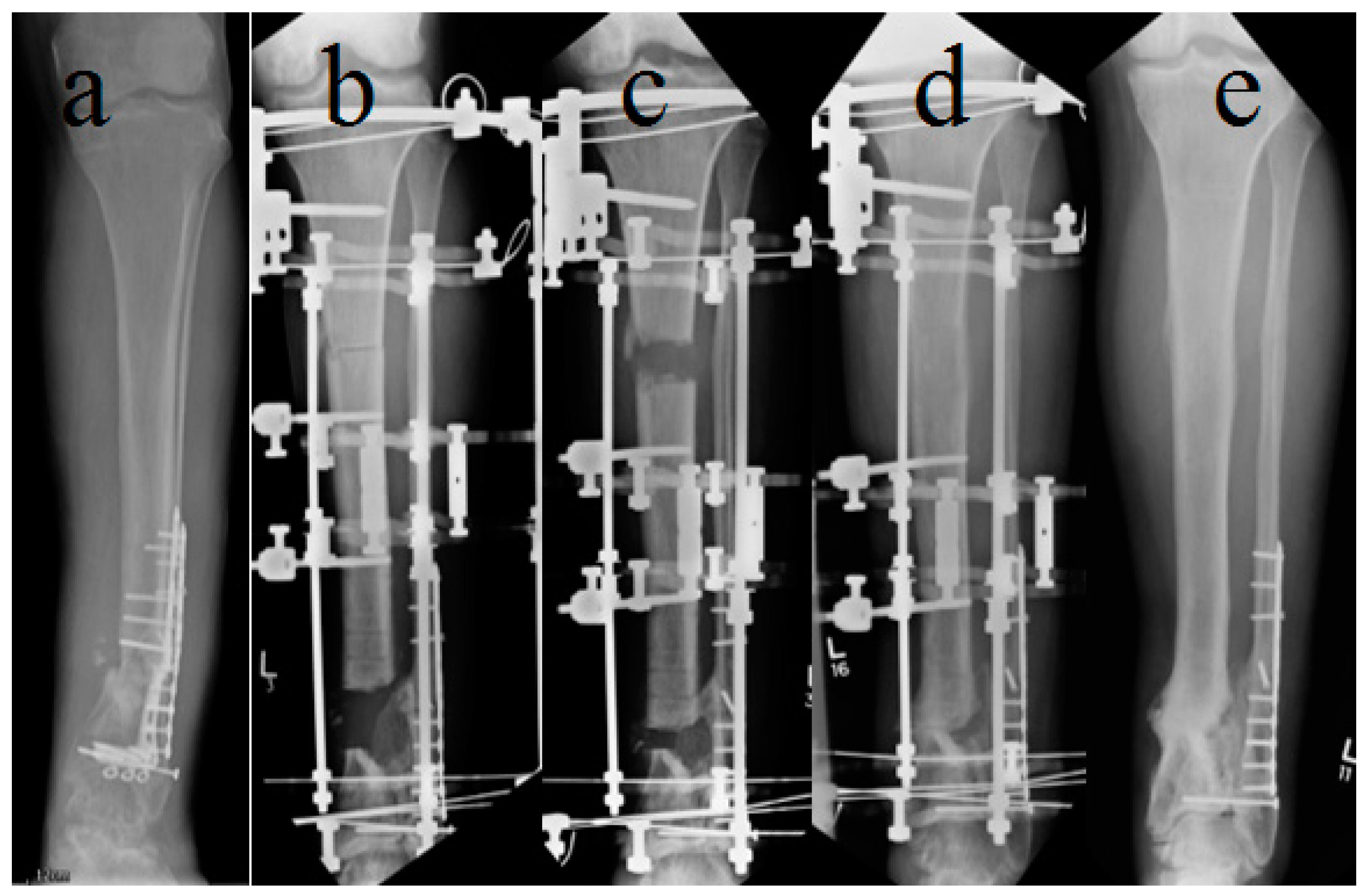
2.5. Standardized Treatment Protocol
2.6. Statistical Analysis
3. Results
3.1. Demographics and Infection Characteristics
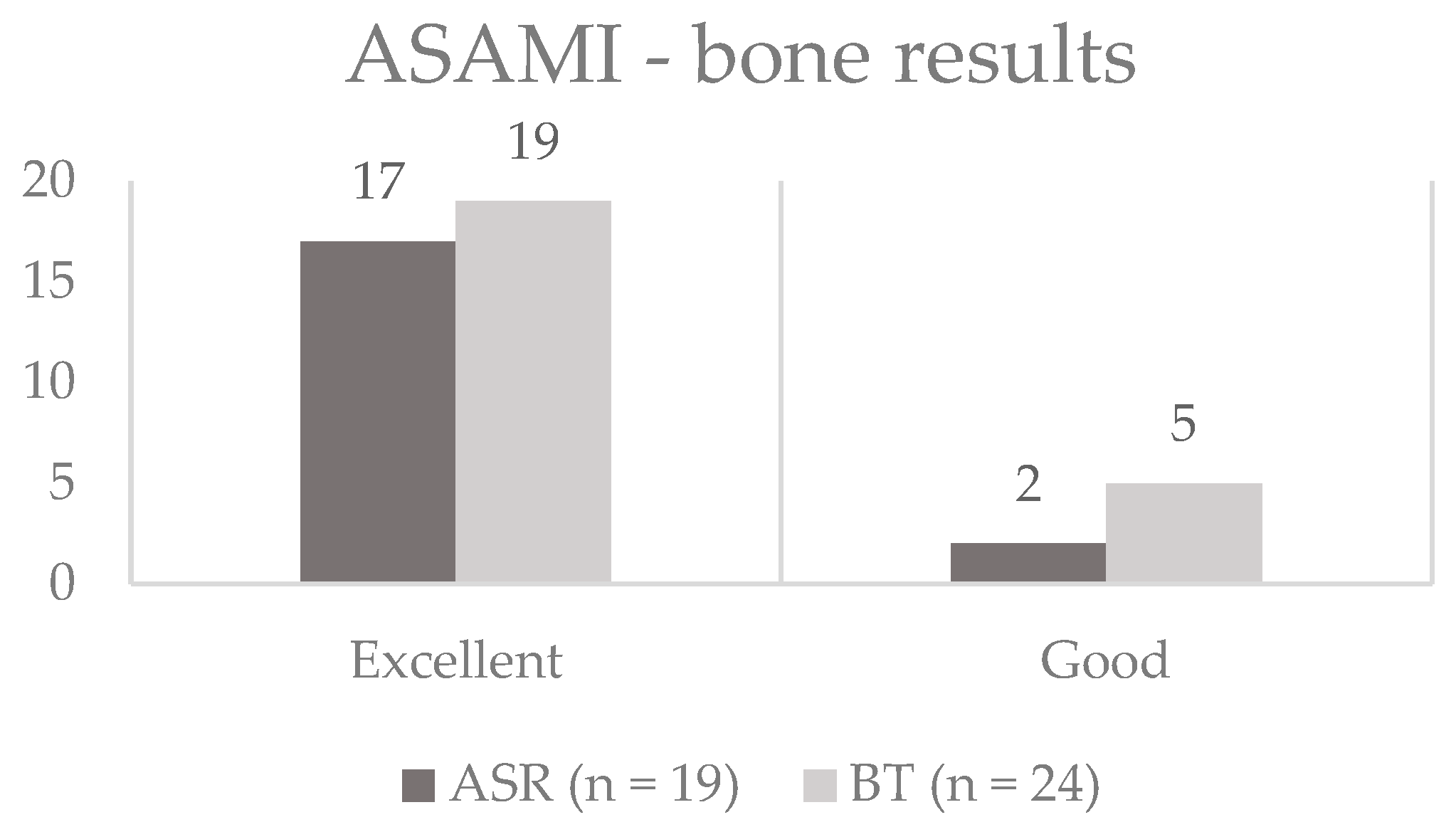
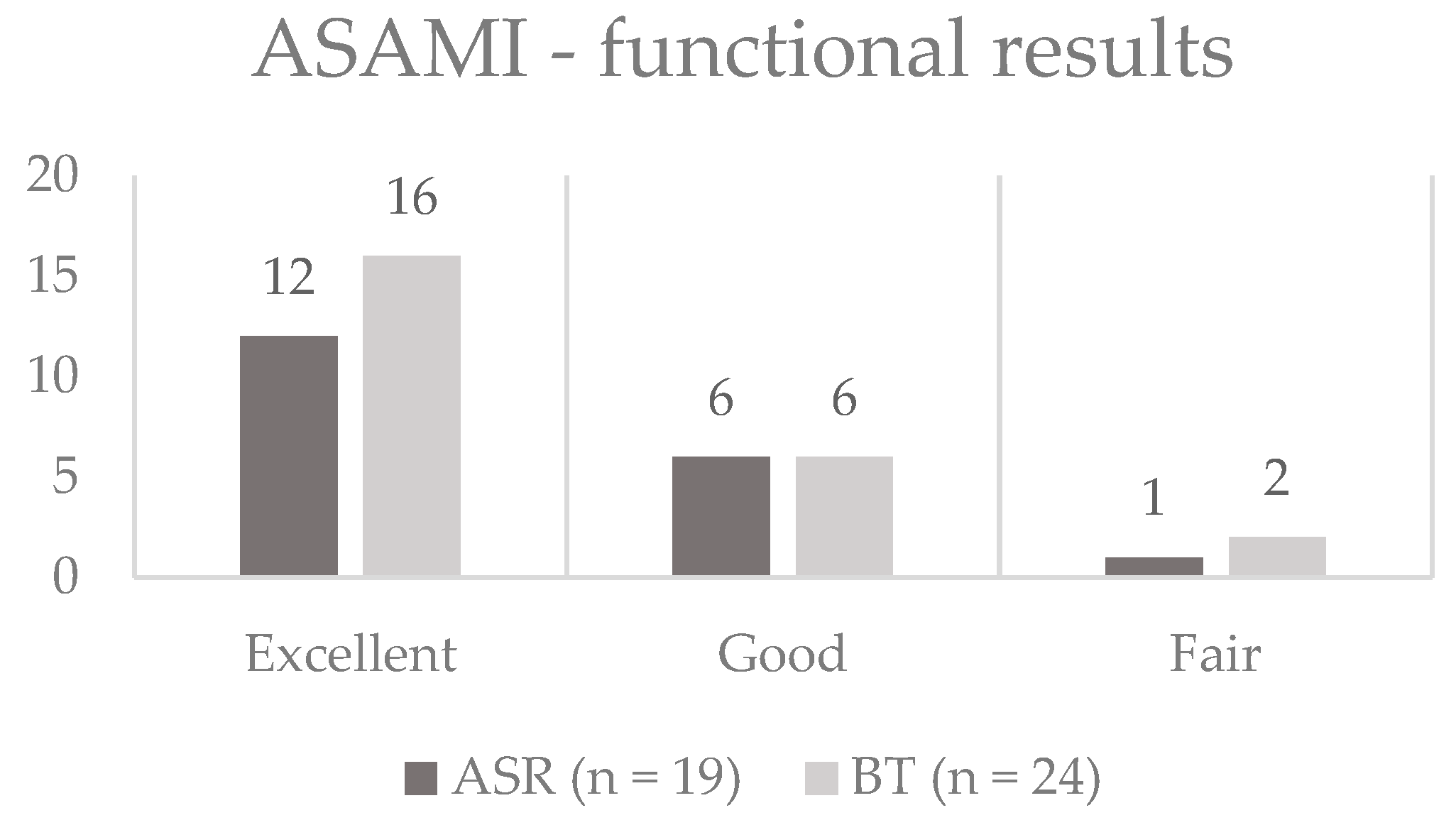
3.2. Outcome
3.3. Unplanned Surgeries during Fixator Time
3.4. Unplanned Surgeries after Fixator Removal
3.5. Other Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cattaneo, R.; Catagni, M.; Johnson, E.E. The treatment of infected nonunions and segmental defects of the tibia by the methods of Ilizarov. Clin. Orthop. Relat. Res. 1992, 280, 143–152. [Google Scholar] [CrossRef]
- Dendrinos, G.K.; Kontos, S.; Lyritsis, E. Use of the Ilizarov technique for treatment of non-union of the tibia associated with infection. J. Bone Jt. Surg. Am. Vol. 1995, 77, 835–846. [Google Scholar] [CrossRef]
- Kocaoglu, M.; Eralp, L.; Rashid, H.U.; Sen, C.; Bilsel, K. Reconstruction of segmental bone defects due to chronic osteomyelitis with use of an external fixator and an intramedullary nail. J. Bone Jt. Surg. Am. Vol. 2006, 88, 2137–2145. [Google Scholar] [CrossRef]
- Metsemakers, W.J.; Kuehl, R.; Moriarty, T.F.; Richards, R.G.; Verhofstad, M.H.J.; Borens, O.; Kates, S.; Morgenstern, M. Infection after fracture fixation: Current surgical and microbiological concepts. Injury 2018, 49, 511–522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antonova, E.; Le, T.K.; Burge, R.; Mershon, J. Tibia shaft fractures: Costly burden of nonunions. Bmc Musculoskelet. Disord. 2013, 14, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Audige, L.; Griffin, D.; Bhandari, M.; Kellam, J.; Ruedi, T.P. Path analysis of factors for delayed healing and nonunion in 416 operatively treated tibial shaft fractures. Clin. Orthop. Relat. Res. 2005, 438, 221–232. [Google Scholar] [CrossRef]
- British Orthopaedic Association & British Association of Plastic, R.A.S. Open Fractures. Available online: https://www.boa.ac.uk/resources/boast-4-pdf.html (accessed on 1 December 2017).
- Harley, B.J.; Beaupre, L.A.; Jones, C.A.; Dulai, S.K.; Weber, D.W. The effect of time to definitive treatment on the rate of nonunion and infection in open fractures. J. Orthop. Trauma 2002, 16, 484–490. [Google Scholar] [CrossRef]
- Malik, M.H.; Harwood, P.; Diggle, P.; Khan, S.A. Factors affecting rates of infection and nonunion in intramedullary nailing. J. Bone Jt. Surg. Br. Vol. 2004, 86, 556–560. [Google Scholar] [CrossRef] [Green Version]
- Nice, National Institute for Health and Care Excellence. Infection Prevention and Control. 2014. Available online: https://www.nice.org.uk/guidance/qs61/resources/infection-prevention-and-control-pdf-2098782603205 (accessed on 17 April 2014).
- Atesalp, A.S.; Komurcu, M.; Basbozkurt, M.; Kurklu, M. The treatment of infected tibial nonunion with aggressive debridement and internal bone transport. Mil. Med. 2002, 167, 978–981. [Google Scholar]
- Maini, L.; Chadha, M.; Vishwanath, J.; Kapoor, S.; Mehtani, A.; Dhaon, B.K. The Ilizarov method in infected nonunion of fractures. Injury 2000, 31, 509–517. [Google Scholar] [CrossRef]
- McHale, K.A.; Ross, A.E. Treatment of infected tibial nonunions with debridement, antibiotic beads, and the Ilizarov method. Mil. Med. 2004, 169, 728–734. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ring, D.; Jupiter, J.B.; Gan, B.S.; Israeli, R.; Yaremchuk, M.J. Infected nonunion of the tibia. Clin. Orthop. Relat. Res. 1999, 302–311. [Google Scholar] [CrossRef] [PubMed]
- McNally, M.; Ferguson, J.; Kugan, R.; Stubbs, D. Ilizarov Treatment Protocols in the Management of Infected Nonunion of the Tibia. J. Orthop. Trauma 2017, 31 (Suppl. S5), S47–S54. [Google Scholar] [CrossRef]
- Yin, P.; Ji, Q.; Li, T.; Li, J.; Li, Z.; Liu, J.; Wang, G.; Wang, S.; Zhang, L.; Mao, Z.; et al. A Systematic Review and Meta-Analysis of Ilizarov Methods in the Treatment of Infected Nonunion of Tibia and Femur. PLoS ONE 2015, 10, e0141973. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.K.K.; Ferguson, J.Y.; Scarborough, M.; McNally, M.A.; Ramsden, A.J. Management of Post-Traumatic Osteomyelitis in the Lower Limb: Current State of the Art. Indian J. Plast. Surg. Off. Publ. Assoc. Plast. Surg. India 2019, 52, 62–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pearson, R.L.; Perry, C.R. The Ilizarov technique in the treatment of infected tibial nonunions. Orthop. Rev. 1989, 18, 609–613. [Google Scholar]
- Eralp, L.; Kocaoglu, M.; Celiktas, M.; Gulsen, M. Is acute compression and distraction superior to segmental bone transport techniques in chronic tibial osteomyelitis? Comparison of Distraction Osteogenesis Techniques. Acta Orthop. Belg. 2016, 82, 599–609. [Google Scholar]
- Khan, M.S.; Rashid, H.; Umer, M.; Qadir, I.; Hafeez, K.; Iqbal, A. Salvage of infected non-union of the tibia with an Ilizarov ring fixator. J. Orthop. Surg. (Hong Kong) 2015, 23, 52–55. [Google Scholar] [CrossRef]
- Paley, D.; Catagni, M.A.; Argnani, F.; Villa, A.; Benedetti, G.B.; Cattaneo, R. Ilizarov treatment of tibial nonunions with bone loss. Clin. Orthop. Relat. Res. 1989, 241, 146–165. [Google Scholar] [CrossRef]
- Tetsworth, K.; Paley, D.; Sen, C.; Jaffe, M.; Maar, D.C.; Glatt, V.; Hohmann, E.; Herzenberg, J.E. Bone transport versus acute shortening for the management of infected tibial non-unions with bone defects. Injury 2017, 48, 2276–2284. [Google Scholar] [CrossRef] [Green Version]
- Weber, B.G.; Cech, O. Pseudarthrosis: Pathophysiology, Biomechanics, Therapy, Results; Grune & Stratton: New York, NY, USA, 1976. [Google Scholar]
- Morgenstern, M.; Athanasou, N.A.; Ferguson, J.Y.; Metsemakers, W.J.; Atkins, B.L.; McNally, M.A. The value of quantitative histology in the diagnosis of fracture-related infection. Bone Jt. J. 2018, 100-b, 966–972. [Google Scholar] [CrossRef] [PubMed]
- Metsemakers, W.J.; Morgenstern, M.; McNally, M.A.; Moriarty, T.F.; McFadyen, I.; Scarborough, M.; Athanasou, N.A.; Ochsner, P.E.; Kuehl, R.; Raschke, M.; et al. Fracture-related infection: A consensus on definition from an international expert group. Injury 2018, 49, 505–510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sigmund, I.K.; McNally, M.C. Diagnosis of bone and joint infections. Orthop. Trauma 2019, 33, 144–152. [Google Scholar] [CrossRef]
- Zhang, Z.; Swanson, W.B.; Wang, Y.H.; Lin, W.; Wang, G. Infection-free rates and Sequelae predict factors in bone transportation for infected tibia: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2018, 19, 442. [Google Scholar] [CrossRef] [Green Version]
- Hatzokos, I.; Stavridis, S.I.; Iosifidou, E.; Karataglis, D.; Christodoulou, A. Autologous bone marrow grafting combined with demineralized bone matrix improves consolidation of docking site after distraction osteogenesis. J. Bone Jt. Surg. Am. Vol. 2011, 93, 671–678. [Google Scholar] [CrossRef]
- Lovisetti, G.; Sala, F. Clinical strategies at the docking site of distraction osteogenesis: Are open procedures superior to the simple compression of Ilizarov? Injury 2013, 44 (Suppl. S1), S58–S62. [Google Scholar] [CrossRef]
- Tetsworth, K.D.; Dlaska, C.E. The art of tibial bone transport using the Ilizarov fixator: The suspension wire technique. Tech. Orthop. 2015, 30, 142–155. [Google Scholar] [CrossRef]
- Ferguson, J.; Diefenbeck, M.; McNally, M. Ceramic Biocomposites as Biodegradable Antibiotic Carriers in the Treatment of Bone Infections. J. Bone Jt. Infect. 2017, 2, 38–51. [Google Scholar] [CrossRef] [Green Version]
- Gordon, L.; Chiu, E.J. Treatment of infected non-unions and segmental defects of the tibia with staged microvascular muscle transplantation and bone-grafting. J. Bone Jt. Surg. Am. Vol. 1988, 70, 377–386. [Google Scholar] [CrossRef]
- Green, S.A. Skeletal defects. A comparison of bone grafting and bone transport for segmental skeletal defects. Clin. Orthop. Relat. Res. 1994, 301, 111–117. [Google Scholar] [CrossRef]
- Le Thua, T.H.; Pham, D.N.; Boeckx, W.; De Mey, A. Vascularized fibular transfer in longstanding and infected large bone defects. Acta Orthop. Belg. 2014, 80, 50–55. [Google Scholar] [PubMed]
- Papineau, L.J.; Alfageme, A.; Dalcourt, J.P.; Pilon, L. Chronic osteomyelitis: Open excision and grafting after saucerization (author’s transl). Int. Orthop. 1979, 3, 165–176. [Google Scholar] [PubMed]
- Bezstarosti, H.; Van Lieshout, E.M.M.; Voskamp, L.W.; Kortram, K.; Obremskey, W.; McNally, M.A.; Metsemakers, W.J.; Verhofstad, M.H.J. Insights into treatment and outcome of fracture-related infection: A systematic literature review. Arch. Orthop. Trauma. Surg. 2019, 139, 61–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tong, K.; Zhong, Z.; Peng, Y.; Lin, C.; Cao, S.; Yang, Y.; Wang, G. Masquelet technique versus Ilizarov bone transport for reconstruction of lower extremity bone defects following posttraumatic osteomyelitis. Injury 2017, 48, 1616–1622. [Google Scholar] [CrossRef] [PubMed]
- McNally, M.A.; Ferguson, J.Y.; Lau, A.C.; Diefenbeck, M.; Scarborough, M.; Ramsden, A.J.; Atkins, B.L. Single-stage treatment of chronic osteomyelitis with a new absorbable, gentamicin-loaded, calcium sulphate/hydroxyapatite biocomposite: A prospective series of 100 cases. Bone Jt. J. 2016, 98-b, 1289–1296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mifsud, M.; Ferguson, J.; Stubbs, D.; Ramsden, A.; McNally, M.A. Outcomes of simultaneous Ilizarov frame reconstruction and free muscle flaps in the management of complex limb infection. Orthop. Proc. 2018, 100-B (Suppl. S8). [Google Scholar] [CrossRef]
| Demographic Data | ASR (n = 20) | BT (n = 27) | p-Value |
|---|---|---|---|
| Patient age (mean) | 48.9 (21–78) | 50.9 (29–75) | 0.738 |
| Bone Defect (cm) | 4.0 (2–5) | 5.9 (3–10) | 0.007 |
| Prior Surgeries per patient | 2.9 (1–5) | 2.7 (1–6) | 0.858 |
| Sinus tract | 8 | 9 | 0.761 |
| Muscle flap | 7 | 10 | 1.000 |
| EF time (months) | 8.8 (5–16) | 10.3 (7–17) | 0.064 |
| EFI (months/cm) | 2.0 (1.3–2.8) | 1.8 (0.9–2.7) | 0.223 |
| Weber–Cech type (n[%]) | |||
| Type C | 1 (5) | 0 (0) | |
| Type D | 4 (20) | 4 (15) | |
| Type E | 3 (15) | 5 (19) | |
| Type F | 12 (60) | 18 (67) |
| Total (n = 47) | ASR (n = 20) | BT (n = 27) | p-Value | |
|---|---|---|---|---|
| Infection-free | 47 (100) | 20 (100) | 27 (100) | 1.000 |
| Union without further surgery | 35 (74) | 18 (90) | 17 (63) | 0.047 |
| Unplanned Reoperation during EF treatment including docking site | 18 (38) | 3 (15) | 15 (56) | 0.006 |
| Unplanned Reoperation during EF treatment excluding docking site | 5 (11) | 3 (15) | 2 (7) | 0.638 |
| Unplanned Reoperation after EF removal | 13 (28) | 3 (15) | 10 (37) | 0.114 |
| Refracture after EF removal | 3 (7) | 2 (11) | 1 (4) | 0.575 |
| Final Infection-free union | 47 (100) | 20 (100) | 27 (100) | 1.000 |
| Total | ASR | BT | p-Value | |
|---|---|---|---|---|
| During EF treatment | ||||
| Fibular Division | 1 (2) | 1 (5) | 0 (0) | 0.426 |
| Insertion of further pins | 1 (2) | 1 (5) | 0 (0) | 0.426 |
| Tethered pin site release | 1 (2) | 1 (5) | 0 (0) | 0.426 |
| Bone grafting only | 4 (9) | 0 (0) | 4 (15) | 0.126 |
| Freshening of docking site | 3 (6) | 0 (0) | 3 (11) | 0.251 |
| Docking Site Realignment | 4 (9) | 0 (0) | 4 (15) | 0.126 |
| Re-Corticotomy | 2 (4) | 0 (0) | 2 (7) | 0.500 |
| BMP only | 2 (4) | 0 (0) | 2 (7) | 0.500 |
| After EF removal | ||||
| Plate only | 4 (9) | 0 (0) | 4 (15) | 0.126 |
| Plating and bone grafting | 1 (2) | 1 (5) | 0 (0) | 0.426 |
| Plating and BMP | 1 (2) | 0 (0) | 1 (4) | 1.000 |
| EF reapplication | 1 (2) | 1 (5) | 0 (0) | 0.426 |
| Intramedullary Nail | 4 (9) | 1 (5) | 3 (11) | 0.626 |
| Ankle Fusion | 2 (4) | 0 (0) | 2 (7) | 0.500 |
| Total | 31 | 6 | 25 | 0.013 |
| Khan et al. [20] | Eralp et al. [19] | Testworth et al. [22] | Present Study | |||||
|---|---|---|---|---|---|---|---|---|
| Study design | prospective | retrospective | retrospective | prospective | ||||
| Number of patients | 24 | 74 | 42 | 47 | ||||
| Procedure | ASR (n = 16) | BT (n = 8) | ASR (n = 45) | BT (n = 29) | ASR (n = 21) | BT (n = 21) | ASR (n = 20) | BT (n = 27) |
| Mean bone defect (cm) | 3.3 (in all patients) | 5.9 | 5.3 | 5.8 | 7.0 | 4.0 | 5.9 | |
| Mean EF time (months) | 8 | 9 | 10 | 10 | 13 | 8.8 | 10.3 | |
| Mean EFI (m/cm) | 4.2 | 1.6 | 2.1 | 1.7 | 1.8 | 2.0 | 1.8 | |
| ASAMI functional | 7 excellent 8 good 1 fair | 1 excellent 4 good 1 fair 1 failure 1 died (advanced liver disease) | 34 excellent 8 good 2 fair1 poor | 22 excellent 3 good 4 poor | 14 excellent 6 good 1 fair | 14 excellent 6 good 1 fair | 12 excellent 7 good 1 fair | 19 excellent 6 good 2 fair |
| ASAMI bone | 6 excellent 9 good 1 fair | 5 good 2 poor 1 died | 35 excellent 8 good 2 fair | 21 excellent 4 good 4 poor | 19 excellent 2 good | 15 excellent 5 good 1 fair | 18 excellent 2 good | 22 excellent 5 good |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sigmund, I.K.; Ferguson, J.; Govaert, G.A.M.; Stubbs, D.; McNally, M.A. Comparison of Ilizarov Bifocal, Acute Shortening and Relengthening with Bone Transport in the Treatment of Infected, Segmental Defects of the Tibia. J. Clin. Med. 2020, 9, 279. https://doi.org/10.3390/jcm9020279
Sigmund IK, Ferguson J, Govaert GAM, Stubbs D, McNally MA. Comparison of Ilizarov Bifocal, Acute Shortening and Relengthening with Bone Transport in the Treatment of Infected, Segmental Defects of the Tibia. Journal of Clinical Medicine. 2020; 9(2):279. https://doi.org/10.3390/jcm9020279
Chicago/Turabian StyleSigmund, Irene K., Jamie Ferguson, Geertje A.M. Govaert, David Stubbs, and Martin A. McNally. 2020. "Comparison of Ilizarov Bifocal, Acute Shortening and Relengthening with Bone Transport in the Treatment of Infected, Segmental Defects of the Tibia" Journal of Clinical Medicine 9, no. 2: 279. https://doi.org/10.3390/jcm9020279
APA StyleSigmund, I. K., Ferguson, J., Govaert, G. A. M., Stubbs, D., & McNally, M. A. (2020). Comparison of Ilizarov Bifocal, Acute Shortening and Relengthening with Bone Transport in the Treatment of Infected, Segmental Defects of the Tibia. Journal of Clinical Medicine, 9(2), 279. https://doi.org/10.3390/jcm9020279





