Associations between Clinical Symptoms and Degree of Ossification in Patients with Cervical Ossification of the Posterior Longitudinal Ligament: A Prospective Multi-Institutional Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Methods
2.2. Clinical Evaluations
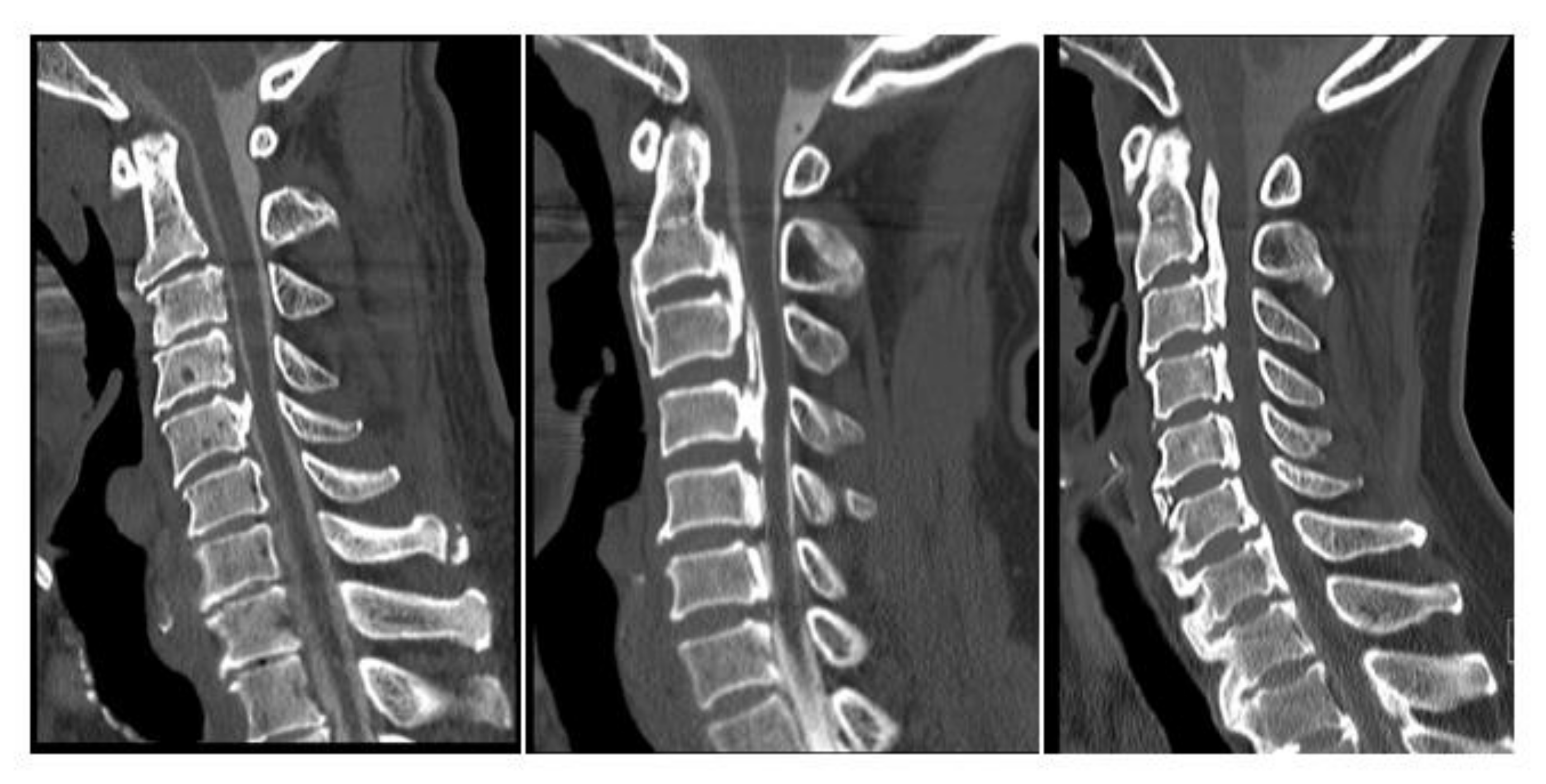
2.3. Radiologic Evaluations
2.4. Statistical Analysis
3. Results
3.1. Demographic Data
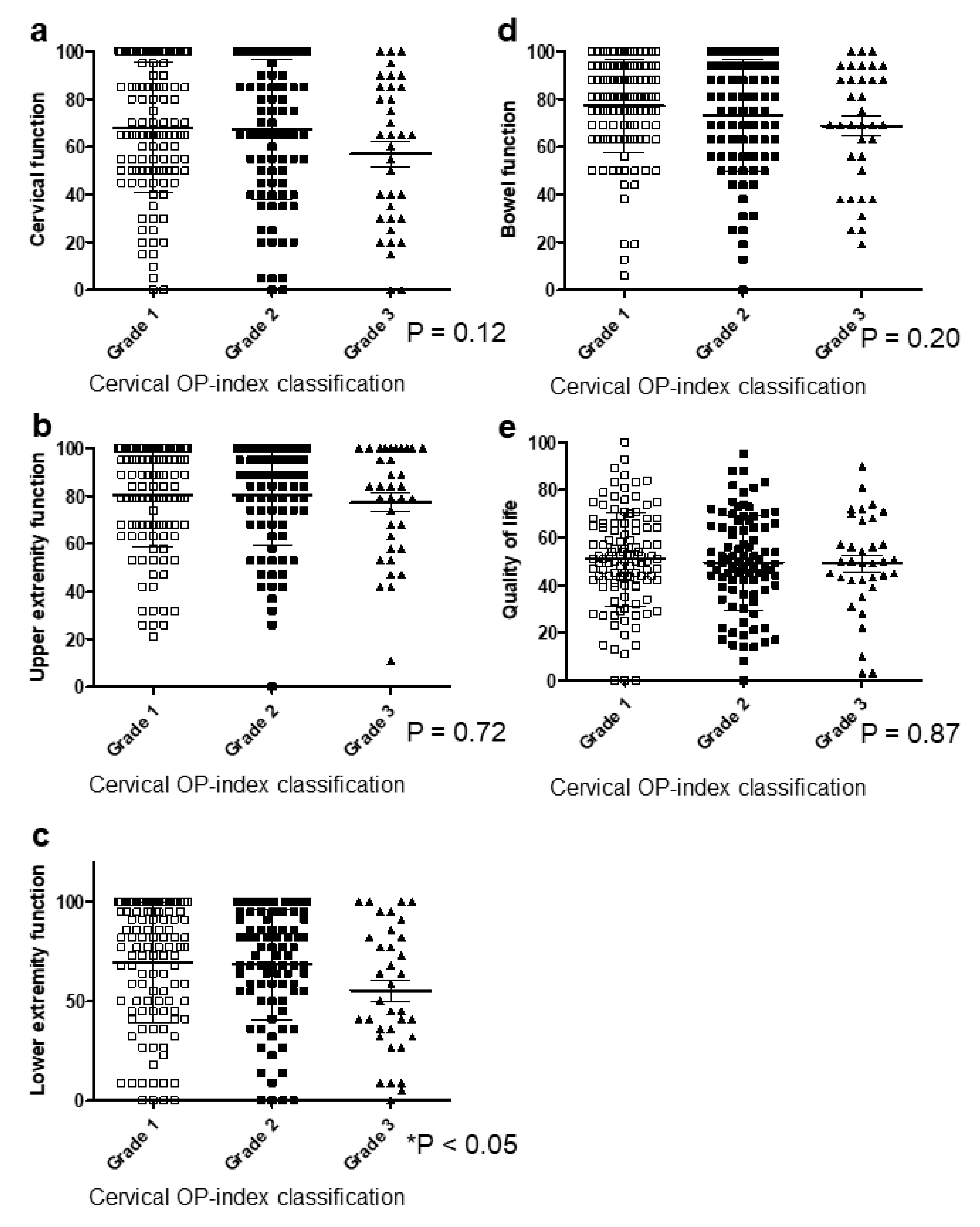
3.2. Cervical OP-Index Grade Was Not Associated with Body Pain in Patients with Cervical OPLL
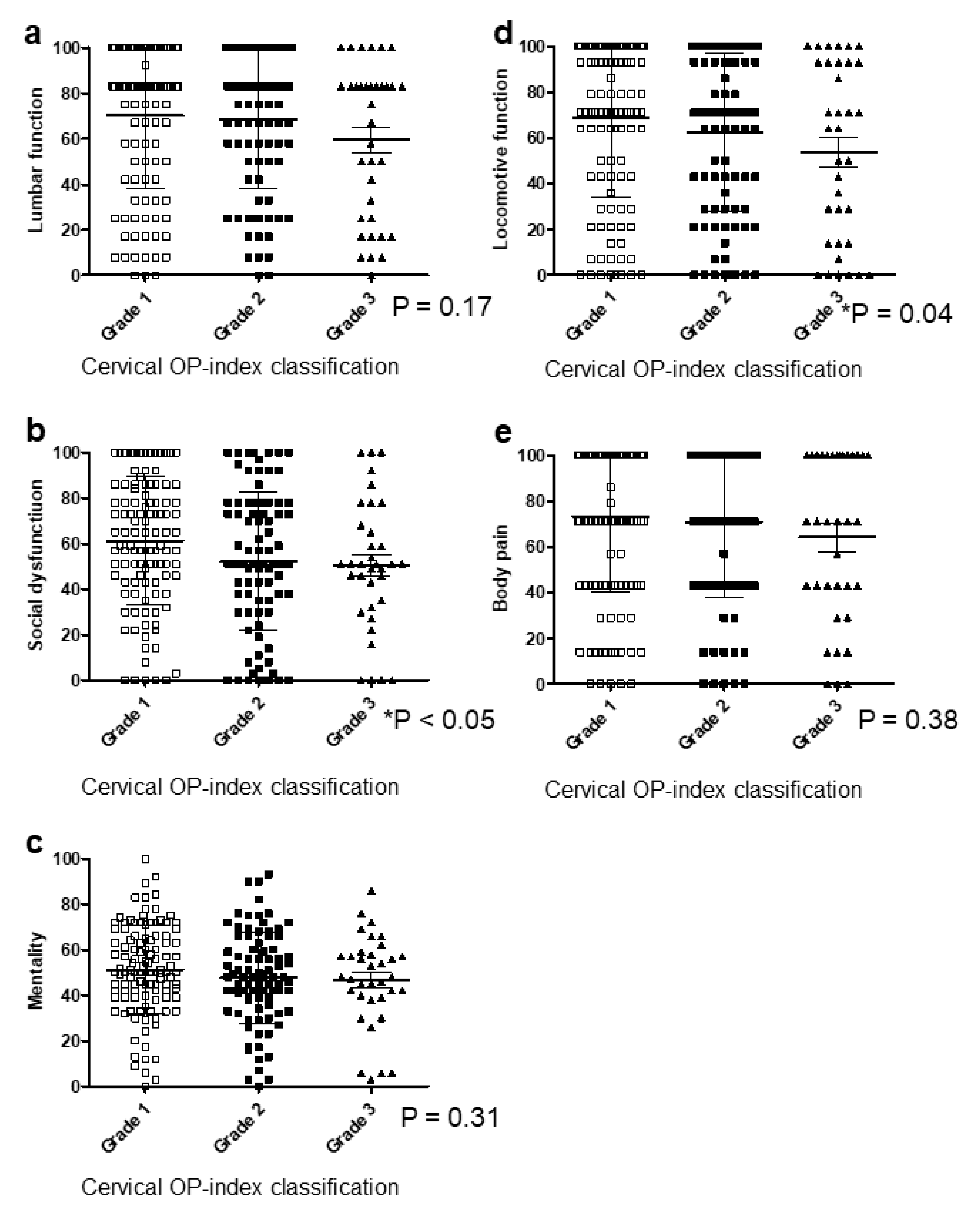
3.3. Cervical OP-Index Grade Was Associated with Lower Extremity Function, Social Dysfunction, and Locomotive Function
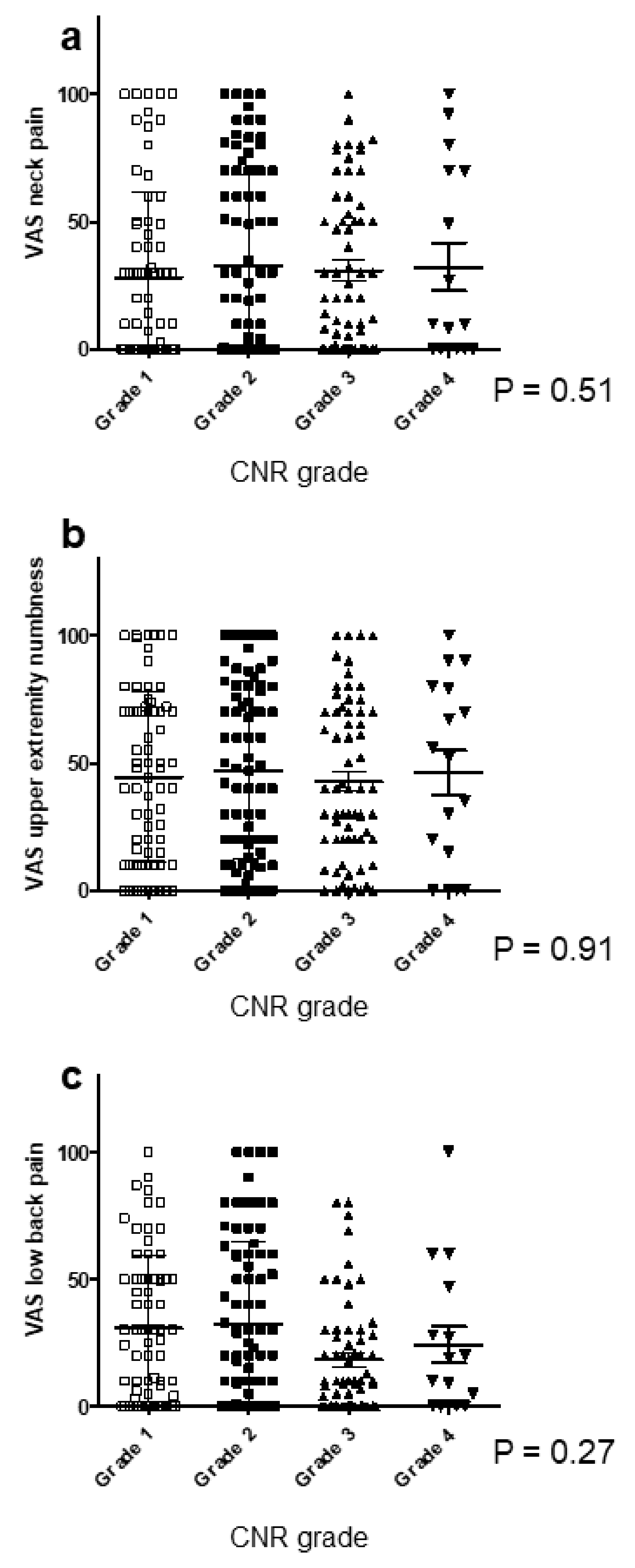
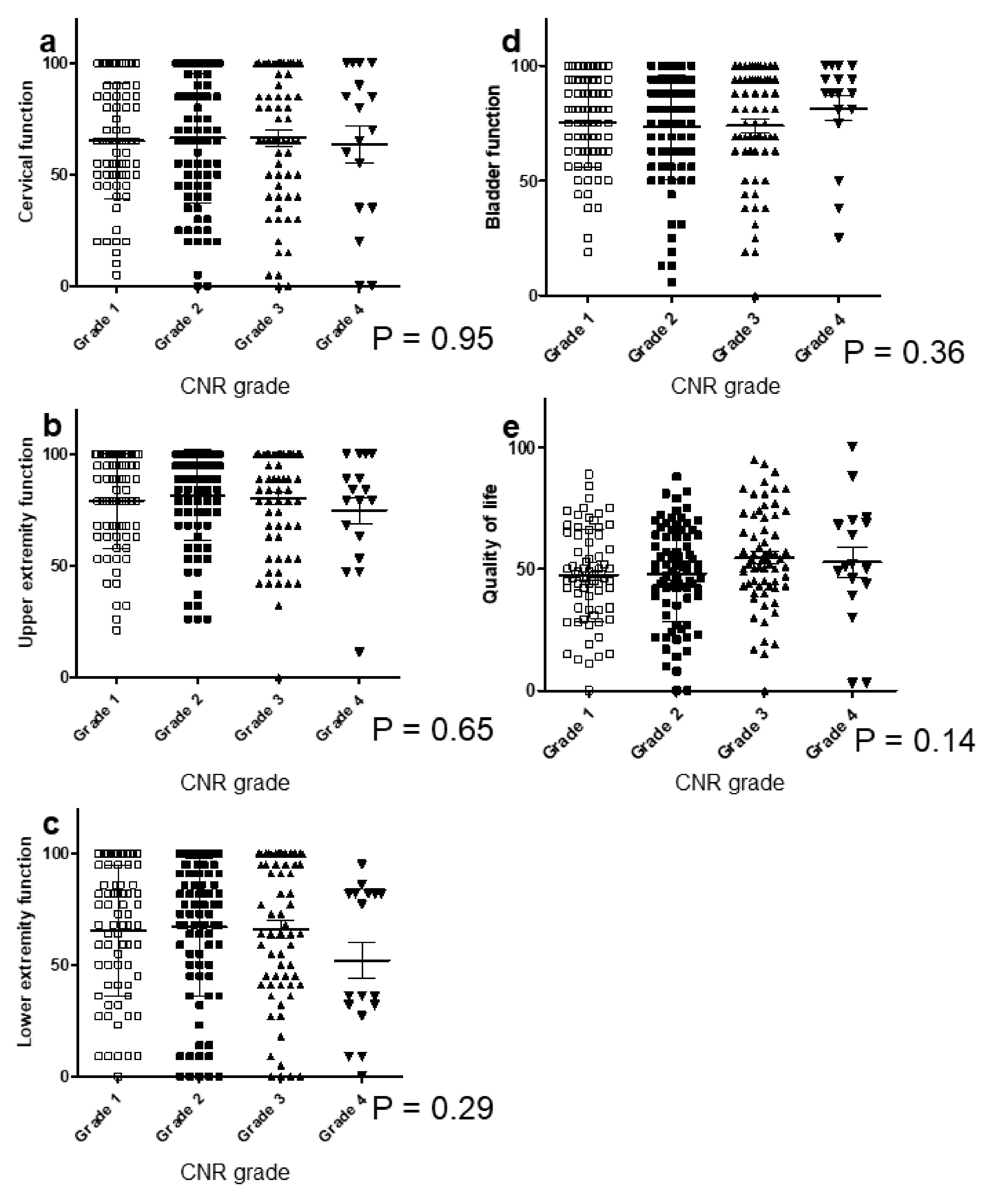
3.4. CNR in the Cervical Spine Did Not Correlate with Clinical Symptoms
3.5. Cervical OP-Index Grade Correlates with Whole-Spine Radiologic Findings
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bakhsh, W.; Saleh, A.; Yokogawa, N.; Gruber, J.; Rubery, P.T.; Mesfin, A. Cervical ossification of the posterior longitudinal ligament: A computed tomography-based epidemiological study of 2917 patients. Glob. Spine J. 2019, 9, 820–825. [Google Scholar] [CrossRef] [PubMed]
- Epstein, N. The surgical management of ossification of the posterior longitudinal ligament in 51 patients. J. Spinal Disord. 1993, 6, 432–454. [Google Scholar] [CrossRef] [PubMed]
- Fujimori, T.; Le, H.; Ziewacz, J.E.; Chou, D.; Mummaneni, P.V. Is there a difference in range of motion, neck pain, and outcomes in patients with ossification of posterior longitudinal ligament versus those with cervical spondylosis, treated with plated laminoplasty? Neurosurg. Focus 2013, 35, E9. [Google Scholar] [CrossRef] [PubMed]
- Fukui, M.; Chiba, K.; Kawakami, M.; Kikuchi, S.; Konno, S.; Miyamoto, M.; Seichi, A.; Shimamura, T.; Shirado, O.; Taguchi, T.; et al. JOA back pain evaluation questionnaire (JOABPEQ)/JOA cervical myelopathy evaluation questionnaire (JOACMEQ). The report on the development of revised versions 16 April 2007. J. Orthop. Sci. 2009, 14, 348–365. [Google Scholar] [CrossRef] [PubMed]
- Hirai, T.; Yoshii, T.; Iwanami, A.; Takeuchi, K.; Mori, K.; Yamada, T.; Wada, K.; Koda, M.; Matsuyama, Y.; Takeshita, K.; et al. Prevalence and distribution of ossified lesions in the whole spine of patients with cervical ossification of the posterior longitudinal ligament a multicenter study (JOSL CT study). PLoS ONE 2016, 11, e0160117. [Google Scholar] [CrossRef]
- Hirai, T.; Yoshii, T.; Nagoshi, N.; Takeuchi, K.; Mori, K.; Ushio, S.; Iwanami, A.; Yamada, T.; Seki, S.; Tsuji, T.; et al. Distribution of ossified spinal lesions in patients with severe ossification of the posterior longitudinal ligament and prediction of ossification at each segment based on the cervical OP index classification: A multicenter study (JOSL CT study). BMC Musculoskelet. Disord. 2018, 19, 107. [Google Scholar] [CrossRef]
- Hirai, T.; Yoshii, T.; Ushio, S.; Mori, K.; Maki, S.; Katsumi, K.; Nagoshi, N.; Takeuchi, K.; Furuya, T.; Watanabe, K.; et al. Clinical characteristics in patients with ossification of the posterior longitudinal ligament: A prospective multi-institutional cross-sectional study. Sci. Rep. 2020, 10, 5532. [Google Scholar] [CrossRef]
- Ito, K.; Yukawa, Y.; Machino, M.; Kato, F. Spinal cord cross-sectional area during flexion and extension in the patients with cervical ossification of posterior longitudinal ligament. Eur. Spine J. 2013, 22, 2564–2568. [Google Scholar] [CrossRef]
- Kameyama, T.; Hashizume, Y.; Ando, T.; Takahashi, A.; Yanagi, T.; Mizuno, J. Spinal cord morphology and pathology in ossification of the posterior longitudinal ligament. Brain 1995, 118, 263–278. [Google Scholar] [CrossRef]
- Karanicolas, P.J.; Bhandari, M.; Kreder, H.; Moroni, A.; Richardson, M.; Walter, S.D.; Norman, G.R.; Guyatt, G.H. Evaluating agreement: Conducting a reliability study. J. Bone Joint Surg. Am. 2009, 91, 99–106. [Google Scholar] [CrossRef]
- Kawaguchi, Y.; Nakano, M.; Yasuda, T.; Seki, S.; Hori, T.; Kimura, T. Ossification of the posterior longitudinal ligament in not only the cervical spine, but also other spinal regions: Analysis using multidetector computed tomography of the whole spine. Spine 2013, 38, E1477–E1482. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, Y.; Nakano, M.; Yasuda, T.; Seki, S.; Hori, T.; Suzuki, K.; Makino, H.; Kimura, T. Characteristics of ossification of the spinal ligament; incidence of ossification of the ligamentum flavum in patients with cervical ossification of the posterior longitudinal ligament—Analysis of the whole spine using multidetector CT. J. Orthop. Sci. 2016, 21, 439–445. [Google Scholar] [CrossRef]
- Matsumoto, M.; Chiba, K.; Toyama, Y.; Takeshita, K.; Seichi, A.; Nakamura, K.; Arimizu, J.; Fujibayashi, S.; Hirabayashi, S.; Hirano, T.; et al. Surgical results and related factors for ossification of posterior longitudinal ligament of the thoracic spine: A multi-institutional retrospective study. Spine 2008, 33, 1034–1041. [Google Scholar] [CrossRef] [PubMed]
- Matsunaga, S.; Sakou, T. Ossification of the posterior longitudinal ligament of the cervical spine: Etiology and natural history. Spine 2012, 37, E309–E314. [Google Scholar] [CrossRef] [PubMed]
- Matsunaga, S.; Sakou, T.; Taketomi, E.; Komiya, S. Clinical course of patients with ossification of the posterior longitudinal ligament: A minimum 10-year cohort study. J. Neurosurg. 2004, 100, 245–248. [Google Scholar] [CrossRef]
- Matsuoka, T.; Yamaura, I.; Kurosa, Y.; Nakai, O.; Shindo, S.; Shinomiya, K. Long-term results of the anterior floating method for cervical myelopathy caused by ossification of the posterior longitudinal ligament. Spine 2001, 26, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Mori, K.; Yoshii, T.; Hirai, T.; Iwanami, A.; Takeuchi, K.; Yamada, T.; Seki, S.; Tsuji, T.; Fujiyoshi, K.; Furukawa, M.; et al. Prevalence and distribution of ossification of the supra/interspinous ligaments in symptomatic patients with cervical ossification of the posterior longitudinal ligament of the spine: A CT-based multicenter cross-sectional study. BMC Musculoskelet. Disord. 2016, 17, 492. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, H.; Uchida, K.; Takayasu, M.; Ushida, T. A nationwide survey of spinal cord-related pain syndrome in Japan: Clinical characteristics and treatment. Spine Surg. Relat. Res. 2019, 3, 319–326. [Google Scholar] [CrossRef]
- Nishimura, S.; Nagoshi, N.; Iwanami, A.; Takeuchi, A.; Hirai, T.; Yoshii, T.; Takeuchi, K.; Mori, K.; Yamada, T.; Seki, S.; et al. Prevalence and distribution of diffuse idiopathic skeletal hyperostosis on whole-spine computed tomography in patients with cervical ossification of the poosterior longitudinal ligament: A multicenter study. Clin. Spine Surg. 2018, 31, E460–E465. [Google Scholar] [CrossRef]
- Oga, M.; Mashima, T.; Iwakuma, T.; Sugioka, Y. Dysphagia complications in ankylosing spinal hyperostosis and ossification of the posterior longitudinal ligament. Roentgenographic findings of the developmental process of cervical osteophytes causing dysphagia. Spine 1993, 18, 391–394. [Google Scholar] [CrossRef]
- Park, S.; Lee, D.H.; Ahn, J.; Cho, J.H.; Lee, S.K.; Kim, K.J.; Park, J.H.; Hwang, C.J.; Park, J.W.; Lee, C.S. How does ossification of posterior longitudinal ligament progress in conservatively managed patients? Spine 2020, 45, 234–243. [Google Scholar] [CrossRef] [PubMed]
- Sakai, K.; Okawa, A.; Takahashi, M.; Arai, Y.; Kawabata, S.; Enomoto, M.; Kato, T.; Hirai, T.; Shinomiya, K. Five-year follow-up evaluation of surgical treatment for cervical myelopathy caused by ossification of the posterior longitudinal ligament: A prospective comparative study of anterior decompression and fusion with floating method versus laminoplasty. Spine 2012, 37, 367–376. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, E.; Ono, A.; Yokoyama, T.; Wada, K.; Tanaka, T.; Kumagai, G.; Iwasaki, H.; Takahashi, I.; Umeda, T.; Nakaji, S.; et al. Prevalence and symptom of ossification of posterior longitudinal ligaments in the Japanese general population. J. Orthop. Sci. 2014, 19, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Shinomiya, K.; Furuya, K.; Sato, R.; Okamoto, A.; Kurosa, Y.; Fuchioka, M. Electrophysiologic diagnosis of cervical OPLL myelopathy using evoked spinal cord potentials. Spine 1988, 13, 1225–1233. [Google Scholar] [CrossRef]
- Yoshii, T.; Egawa, S.; Hirai, T.; Kaito, T.; Mori, K.; Koda, M.; Chikuda, H.; Hasegawa, T.; Imagama, S.; Yoshida, M.; et al. A systematic review and meta-analysis comparing anterior decompression with fusion and posterior laminoplasty for cervical ossification of the posterior longitudinal ligament. J. Orthop. Sci. 2020, 25, 58–65. [Google Scholar] [CrossRef]
- Yoshii, T.; Hirai, T.; Iwanami, A.; Nagoshi, N.; Takeuchi, K.; Mori, K.; Yamada, T.; Seki, S.; Tsuji, T.; Fujiyoshi, K.; et al. Co-existence of ossification of the nuchal ligament is associated with severity of ossification in the whole spine in patients with cervical ossification of the posterior longitudinal ligament—A multi-center CT study. J. Orthop. Sci. 2019, 24, 35–41. [Google Scholar] [CrossRef]
- Yoshii, T.; Sakai, K.; Hirai, T.; Yamada, T.; Inose, H.; Kato, T.; Enomoto, M.; Tomizawa, S.; Kawabata, S.; Arai, Y.; et al. Anterior decompression with fusion versus posterior decompression with fusion for massive cervical ossification of the posterior longitudinal ligament with a ≥50% canal occupying ratio: A multicenter retrospective study. Spine J. 2016, 16, 1351–1357. [Google Scholar] [CrossRef]
- Yoshimura, N.; Nagata, K.; Muraki, S.; Oka, H.; Yoshida, M.; Enyo, Y.; Kagotani, R.; Hashizume, H.; Yamada, H.; Ishimoto, Y.; et al. Prevalence and progression of radiographic ossification of the posterior longitudinal ligament and associated factors in the Japanese population: A 3-year follow-up of the ROAD study. Osteoporos. Int. 2014, 25, 1089–1098. [Google Scholar] [CrossRef]



| Grade 1 (n = 113) | Grade 2 (n = 90) | Grade 3 (n = 36) | p | |
|---|---|---|---|---|
| Age (years) | 62.7 ± 11.9 | 64.9 ± 12.3 | 65.3 ± 13.4 | 0.88 |
| Sex (M/F) | 75/38 | 65/25 | 23/13 | 0.08 |
| Diabetes mellitus (%) | 18.6% | 31.1% | 27.8% | 0.12 |
| BMI | 25.3 ± 4.2 | 26.5 ± 4.5 | 26.4 ± 5.3 | 0.74 |
| Cervical JOA score | 12.4 ± 3.5 | 12.4 ± 3.2 | 11.6 ± 3.6 | 0.21 |
| Prevalence of symptoms | ||||
| Neck pain | 65.5% | 54.4% | 48.7% | 0.15 |
| Back pain | 25.7% | 26.7% | 38.9% | 0.13 |
| Low back pain | 50.4% | 60% | 47.2% | 0.21 |
| OP-index | ||||
| Thoracic spine | 1.1 ± 2.8 | 2.6 ± 4.2 | 4.3 ± 0.8 | <0.001 |
| Lumbar spine | 0.1 ± 0.9 | 0.7 ± 1.7 | 0.8 ± 1.5 | 0.02 |
| Whole spine | 4.7 ± 3.6 | 10.5 ± 5.7 | 16.1 ± 1.2 | <0.001 |
| DISH grade | 0.4 ± 0.8 | 1.0 ± 1.1 | 1.5 ± 1.2 | <0.001 |
| Grade 1 (n = 71) | Grade 2 (n = 82) | Grade 3 (n = 62) | Grade 4 (n = 17) | p | |
|---|---|---|---|---|---|
| Age (years) | 63.4 ± 12.6 | 65.4 ± 10.8 | 64.0 ± 13.6 | 59.0 ± 11.9 | 0.14 |
| Male (M/F) | 45/26 | 56/26 | 46/16 | 13/4 | 0.10 |
| Diabetes mellitus (%) | 16.9% | 31.7% | 24.2% | 35.3% | 0.17 |
| BMI | 25.5 ± 4.6 | 26.3 ± 4.5 | 25.4 ± 4.2 | 27.4 ± 4.8 | 0.11 |
| Cervical JOA score | 12.3 ± 3.0 | 12.4 ± 3.2 | 11.6 ± 3.6 | 11.9 ± 3.3 | 0.07 |
| Prevalence of symptoms | |||||
| Neck pain | 53.5% | 59.8% | 67.7% | 70.6% | 0.14 |
| Back pain | 19.7% | 34.1% | 29.0% | 29.4% | 0.11 |
| Low back pain | 50.7% | 50% | 59.7% | 70.6% | 0.17 |
| OP-index | |||||
| Cervical spine | 3.7 ± 2.3 | 6.5 ± 3.0 | 7.2 ± 3.0 | 7.5 ± 3.0 | 0.02 |
| Thoracic spine | 1.1 ± 2.6 | 2.5 ± 4.5 | 2.8 ± 4.4 | 2.2 ± 3.2 | 0.24 |
| Lumbar spine | 0.2 ± 0.8 | 0.5 ± 1.2 | 0.8 ± 1.7 | 0.6 ± 1.6 | 0.08 |
| Whole spine | 5.0 ± 3.9 | 9.5 ± 6.6 | 10.7 ± 6.7 | 10.6 ± 6.1 | 0.07 |
| DISH grade | 0.3 ± 0.8 | 1.0 ± 1.1 | 1.2 ± 1.1 | 0.5 ± 0.8 | 0.19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hirai, T.; Yoshii, T.; Ushio, S.; Hashimoto, J.; Mori, K.; Maki, S.; Katsumi, K.; Nagoshi, N.; Takeuchi, K.; Furuya, T.; et al. Associations between Clinical Symptoms and Degree of Ossification in Patients with Cervical Ossification of the Posterior Longitudinal Ligament: A Prospective Multi-Institutional Cross-Sectional Study. J. Clin. Med. 2020, 9, 4055. https://doi.org/10.3390/jcm9124055
Hirai T, Yoshii T, Ushio S, Hashimoto J, Mori K, Maki S, Katsumi K, Nagoshi N, Takeuchi K, Furuya T, et al. Associations between Clinical Symptoms and Degree of Ossification in Patients with Cervical Ossification of the Posterior Longitudinal Ligament: A Prospective Multi-Institutional Cross-Sectional Study. Journal of Clinical Medicine. 2020; 9(12):4055. https://doi.org/10.3390/jcm9124055
Chicago/Turabian StyleHirai, Takashi, Toshitaka Yoshii, Shuta Ushio, Jun Hashimoto, Kanji Mori, Satoshi Maki, Keiichi Katsumi, Narihito Nagoshi, Kazuhiro Takeuchi, Takeo Furuya, and et al. 2020. "Associations between Clinical Symptoms and Degree of Ossification in Patients with Cervical Ossification of the Posterior Longitudinal Ligament: A Prospective Multi-Institutional Cross-Sectional Study" Journal of Clinical Medicine 9, no. 12: 4055. https://doi.org/10.3390/jcm9124055
APA StyleHirai, T., Yoshii, T., Ushio, S., Hashimoto, J., Mori, K., Maki, S., Katsumi, K., Nagoshi, N., Takeuchi, K., Furuya, T., Watanabe, K., Nishida, N., Nishimura, S., Watanabe, K., Kaito, T., Kato, S., Nagashima, K., Koda, M., Ito, K., ... Kawaguchi, Y. (2020). Associations between Clinical Symptoms and Degree of Ossification in Patients with Cervical Ossification of the Posterior Longitudinal Ligament: A Prospective Multi-Institutional Cross-Sectional Study. Journal of Clinical Medicine, 9(12), 4055. https://doi.org/10.3390/jcm9124055









