Efficacy of Combination Chemotherapy Using a Novel Oral Chemotherapeutic Agent, FTD/TPI, with Ramucirumab Murine Version DC101 in a Mouse Syngeneic Cancer Transplantation Model
Abstract
1. Introduction
2. Experimental Section
2.1. Cell Lines and Culture Conditions
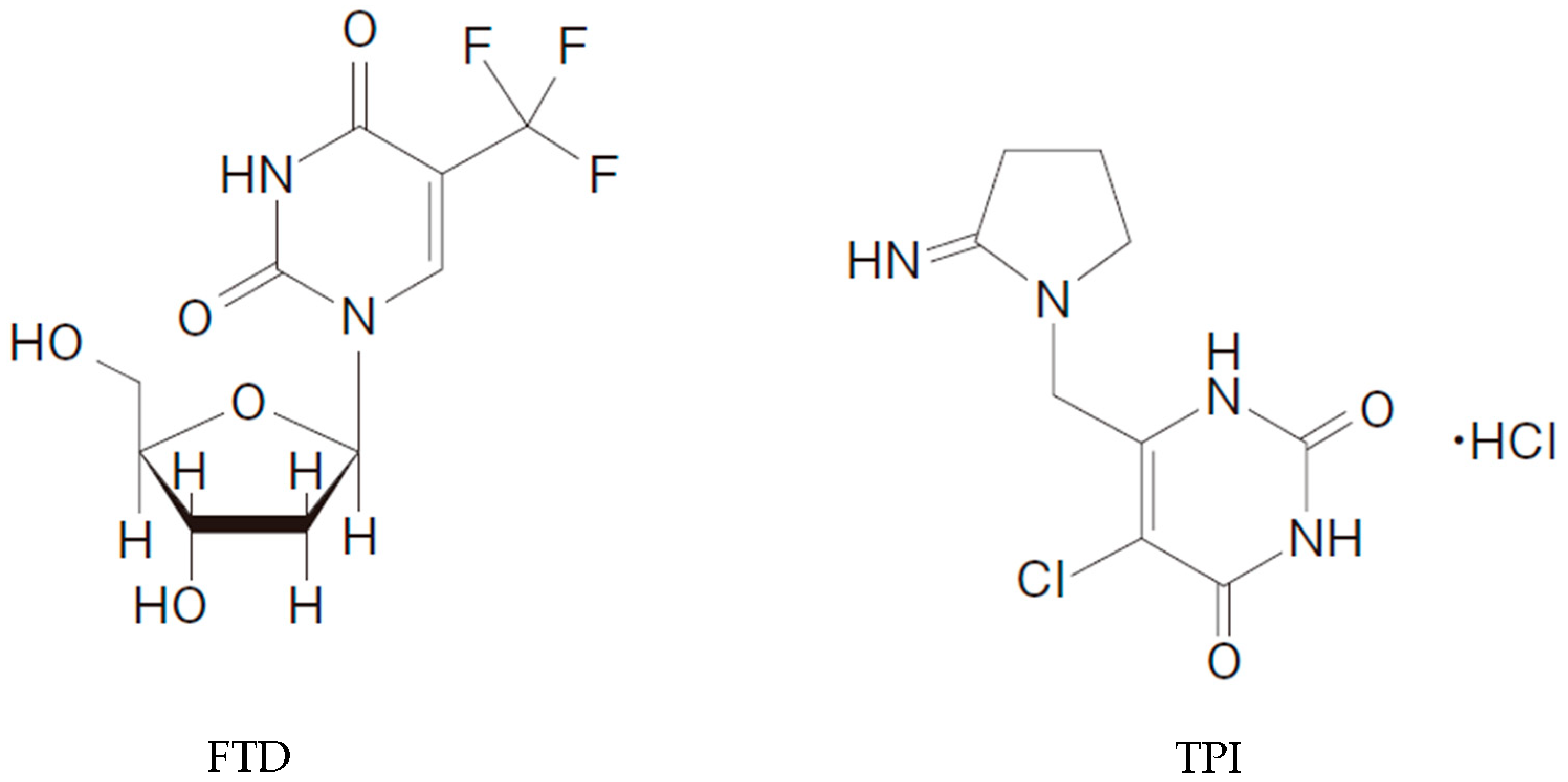
2.2. Chemicals and Antibodies
2.3. Animals
2.4. Antitumor Activity In Vivo
2.5. Flow Cytometry Analysis of Tumor-Infiltrating T Cells
2.6. Immunohistochemistry
2.7. Extraction and Quantification of FTD Incorporated in Tumor DNA
2.8. Statistical Analysis
3. Results
3.1. The Murine Variant of Ramucirumab, DC101, Increases the AntiTumor Efficacy of FTD/TPI
3.2. Increased FTD Levels in Tumor DNA after Combination Treatment with DC101 and FTD/TPI Treatment
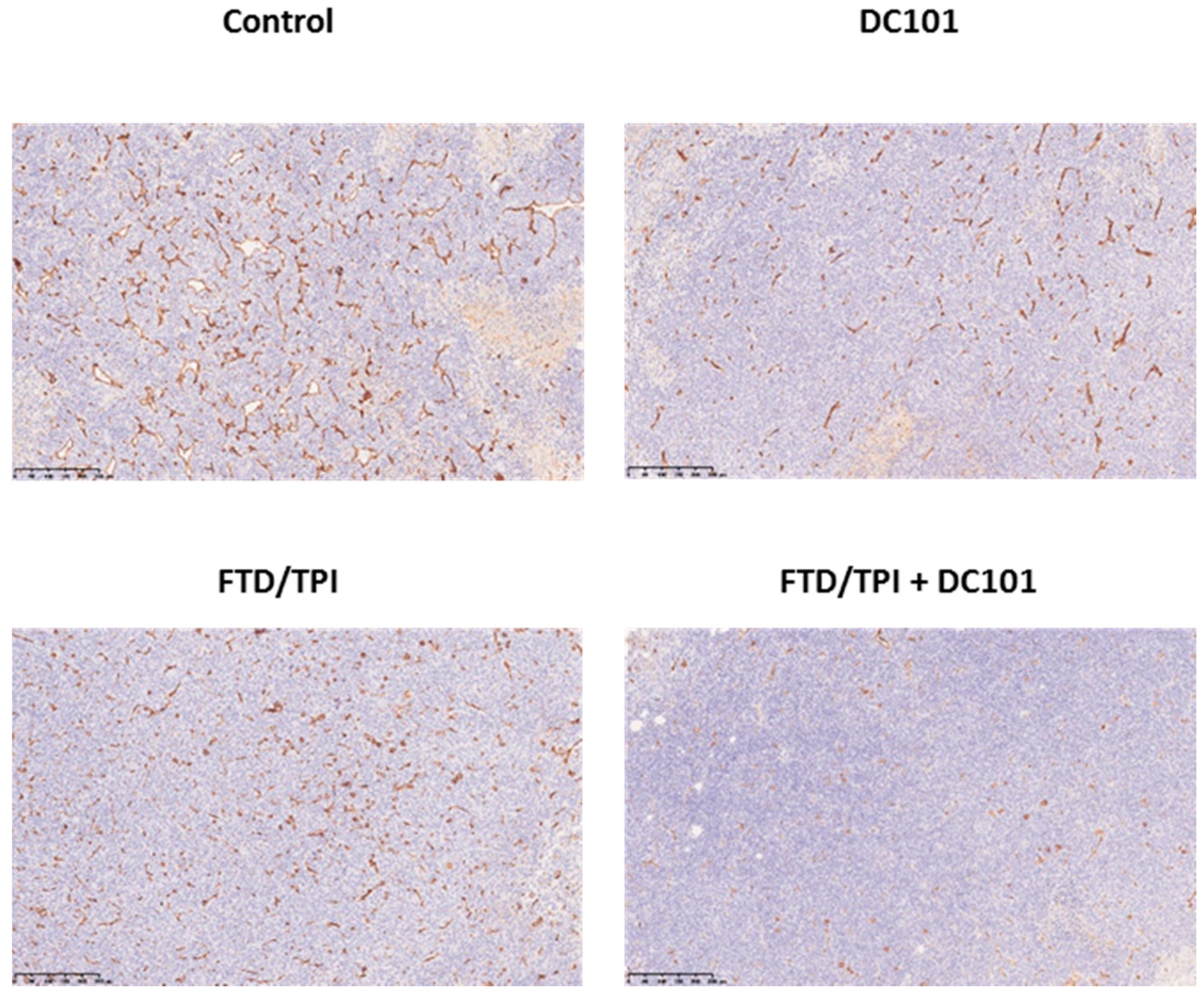
3.3. Tumoral CD31 Levels after Treatment with Antimouse VEGFR-2 Monoclonal Antibody (mAb)
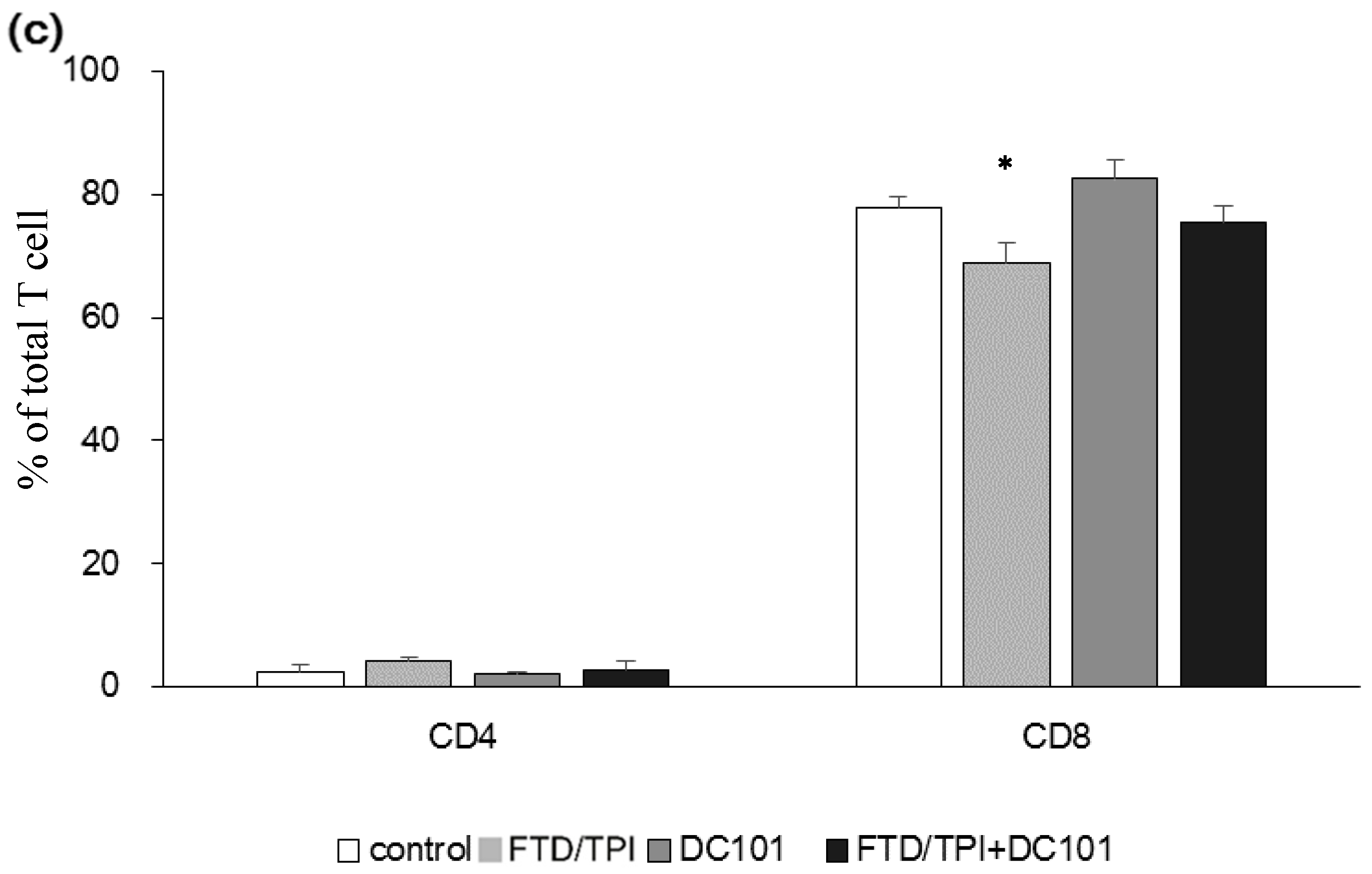
3.4. Abundance of TAM and Tumor-Infiltrating Lymphocytes (TILs) upon Combination Treatment with FTD/TPI and DC101
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Heidelberger, C.; Griesbach, L.; CruZ, O.; Schnitzer, R.J.; Grunberg, E. Fluorinated pyrimidines. VI. Effects of 5-fluorouridine and 5-fluoro-2′-deoxyuridine on transplanted tumors. Proc. Soc. Exp. Biol. Med. 1958, 97, 470–475. [Google Scholar] [CrossRef] [PubMed]
- Reyes, P.; Heidelberger, C. Fluorinated pyrimidines. XXVI. Mammalian thymidylate synthetase: Its mechanism of action and inhibition by fluorinated nucleotides. Mol. Pharmacol. 1965, 1, 14–30. [Google Scholar] [PubMed]
- Fujiwara, Y.; Oki, T.; Heidelberger, C. Fluorinated pyrimidines. XXXVII. Effects of 5-trifluorometh- yl-2′-deoxyuridine on the synthesis of deoxyri- bonucleic acid of mammalian cells in culture. Mol. Pharmacol. 1970, 6, 273–280. [Google Scholar] [PubMed]
- Fukushima, M.; Suzuki, N.; Emura, T.; Yano, S.; Kazuno, H.; Tada, Y.; Yamada, Y.; Asao, T. Structure and activity of specific inhibitors of thymidine phosphorylase to potentiate the function of antitumor 2′-deoxyribonucleosides. Biochem. Pharmacol. 2000, 59, 1227–1236. [Google Scholar] [CrossRef]
- Emura, T.; Suzuki, N.; Yamaguchi, M.; Ohshimo, H.; Fukushima, M. A novel combination antimetabolite, TAS-102, exhibits antitumor activity in FU-resistant human cancer cells through a mechanism involving FTD incorporation in DNA. Int. J. Oncol. 2004, 25, 571–578. [Google Scholar] [CrossRef]
- Mayer, R.J.; Van Cutsem, E.; Falcone, A.; Yoshino, T.; Garcia-Carbonero, R.; Mizunuma, N.; Yamazaki, K.; Shimada, Y.; Tabernero, J.; Komatsu, Y.; et al. Randomized Trial of TAS-102 for Refractory Metastatic Colorectal Cancer. N. Engl. J. Med. 2015, 372, 1909–1919. [Google Scholar] [CrossRef]
- Shitara, K.; Doi, T.; Dvorkin, M.; Mansoor, W.; Arkenau, H.T.; Prokharau, A.; Alsina, M.; Ghidini, M.; Faustino, C.; Gorbunova, V.; et al. Trifluridine/tipiracil versus placebo in patients with heavily pretreated metastatic gastric cancer (TAGS): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2018, 19, 1437–1448. [Google Scholar] [CrossRef]
- Jain, R.K. Normalizing tumor vasculature with anti-angiogenic therapy: A new paradigm for combination therapy. Nat. Med. 2001, 7, 987–989. [Google Scholar] [CrossRef]
- Tsukihara, H.; Nakagawa, F.; Sakamoto, K.; Ishida, K.; Tanaka, N.; Okabe, H.; Uchida, J.; Matsuo, K.; Takechi, T. Efficacy of combination chemotherapy using a novel oral chemotherapeutic agent, TAS-102, together with bevacizumab, cetuximab, or panitumumab on human colorectal cancer xenografts. Oncol. Rep. 2015, 33, 2135–2142. [Google Scholar] [CrossRef]
- Kuboki, Y.; Nishina, T.; Shinozaki, E.; Yamazaki, K.; Shitara, K.; Okamoto, W.; Kajiwara, T.; Matsumoto, T.; Tsushima, T.; Mochizuki, N.; et al. TAS-102 plus bevacizumab for patients with metastatic colorectal cancer refractory to standard therapies (C-TASK FORCE): An investigator-initiated, open-label, single-arm, multicentre, phase 1/2 study. Lancet Oncol. 2017, 18, 1172–1181. [Google Scholar] [CrossRef]
- Pfeiffer, P.; Yilmaz, M.; Möller, S.; Zitnjak, D.; Krogh, M.; Petersen, L.N.; Poulsen, L.Ø.; Winther, S.B.; Thomsen, K.G.; Qvortrup, C. TAS-102 with or without bevacizumab in patients with chemorefractory metastatic colorectal cancer: An investigator-initiated, open-label, randomised, phase 2 trial. Lancet Oncol. 2020, 21, 412–420. [Google Scholar] [CrossRef]
- Kataoka, Y.; Iimori, M.; Fujisawa, R.; Morikawa-Ichinose, T.; Niimi, S.; Wakasa, T.; Saeki, H.; Oki, E.; Miura, D.; Tsurimoto, T.; et al. DNA Replication Stress Induced by Trifluridine Determines Tumor Cell Fate According to p53 Status. Mol. Cancer Res. 2020, 18, 1354–1366. [Google Scholar] [CrossRef]
- Zafarnia, S.; Bzyl-Ibach, J.; Spivak, I.; Li, Y.; Koletnik, S.; Doleschel, D.; Rix, A.; Pochon, S.; Tardy, I.; Koyadan, S.; et al. Nilotinib Enhances Tumor Angiogenesis and Counteracts VEGFR2 Blockade in an Orthotopic Breast Cancer Xenograft Model with Desmoplastic Response. Neoplasia 2017, 19, 896–907. [Google Scholar] [CrossRef] [PubMed]
- Matsuoka, K.; Nakagawa, F.; Kobunai, T.; Takechi, T. Trifluridine/tipiracil overcomes the resistance of human gastric 5-fluorouracil-refractory cells with high thymidylate synthase expression. Oncotarget 2018, 9, 13438–13450. [Google Scholar] [CrossRef] [PubMed]
- Zhao, P.; Wang, Y.; Kang, X.; Wu, A.; Yin, W.; Tang, Y.; Wang, J.; Zhang, M.; Duan, Y.; Huang, Y. Dual-targeting biomimetic delivery for anti-glioma activity: Via remodeling the tumor microenvironment and directing macrophage-mediated immunotherapy. Chem. Sci. 2018, 9, 2674–2689. [Google Scholar] [CrossRef] [PubMed]
- Hilberg, F.; Roth, G.J.; Krssak, M.; Kautschitsch, S.; Sommergruber, W.; Tontsch-Grunt, U.; Garin-Chesa, P.; Bader, G.; Zoephel, A.; Quant, J.; et al. BIBF 1120: Triple angiokinase inhibitor with sustained receptor blockade and good antitumor efficacy. Cancer Res. 2008, 68, 4774–4782. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Takara, K.; Yamakawa, D.; Kidoya, H.; Takakura, N. Apelin as a marker for monitoring the tumor vessel normalization window during antiangiogenic therapy. Cancer Sci. 2016, 107, 36–44. [Google Scholar] [CrossRef]
- Fujimoto, Y.; Nakanishi, R.; Nukatsuka, M.; Matsuoka, K.; Ando, K.; Wakasa, T.; Kitao, H.; Oki, E.; Maehara, Y.; Mori, M. Detection of trifluridine in tumors of patients with metastatic colorectal cancer treated with trifluridine/tipiracil. Cancer Chemother. Pharmacol. 2020, 85, 1029–1038. [Google Scholar] [CrossRef]
- Castle, J.C.; Loewer, M.; Boegel, S.; de Graaf, J.; Bender, C.; Tadmor, A.D.; Boisguerin, V.; Bukur, T.; Sorn, P.; Paret, C.; et al. Immunomic, genomic and transcriptomic characterization of CT26 colorectal carcinoma. BMC Genom. 2014, 15, 1–2. [Google Scholar] [CrossRef]
- Yoshino, T.; Portnoy, D.C.; Obermannová, R.; Bodoky, G.; Prausová, J.; Garcia-Carbonero, R.; Ciuleanu, T.; García-Alfonso, P.; Cohn, A.L.; Van Cutsem, E.; et al. Biomarker analysis beyond angiogenesis: RAS/RAF mutation status, tumour sidedness, and second-line ramucirumab efficacy in patients with metastatic colorectal carcinoma from RAISE-a global phase III study. Ann. Oncol. 2019, 30, 124–131. [Google Scholar] [CrossRef]
- Price, T.J.; Hardingham, J.E.; Lee, C.K.; Weickhardt, A.; Townsend, A.R.; Wrin, J.W.; Chua, A.; Shivasami, A.; Cummins, M.M.; Murone, C.; et al. Impact of kRAS and BRAF gene mutation status on outcomes from the phase III AGITG MAX trial of capecitabine alone or in combination with bevacizumab and mitomycin in advanced colorectal cancer. J. Clin. Oncol. 2011, 29, 2675–2682. [Google Scholar] [CrossRef] [PubMed]
- Tada, Y.; Togashi, Y.; Kotani, D.; Kuwata, T.; Sato, E.; Kawazoe, A.; Doi, T.; Wada, H.; Nishikawa, H.; Shitara, K. Targeting VEGFR2 with Ramucirumab strongly impacts effector/ activated regulatory T cells and CD8+ T cells in the tumor microenvironment. J. Immunother. Cancer 2018, 6, 106. [Google Scholar] [CrossRef] [PubMed]
- Limagne, E.; Thibaudin, M.; Nuttin, L.; Spill, A.; Derangère, V.; Fumet, J.D.; Amellal, N.; Peranzoni, E.; Cattan, V.; Ghiringhelli, F. Trifluridine/tipiracil plus oxaliplatin improves PD-1 blockade in colorectal cancer by inducing immunogenic cell death and depleting macrophages. Cancer Immunol. Res. 2019, 7, 1958–1969. [Google Scholar] [CrossRef] [PubMed]
- Biswas, S.K.; Mantovani, A. Macrophage plasticity and interaction with lymphocyte subsets: Cancer as a paradigm. Nat. Immunol. 2010, 11, 889–896. [Google Scholar] [CrossRef] [PubMed]
- Komohara, Y.; Fujiwara, Y.; Ohnishi, K.; Takeya, M. Tumor-associated macrophages: Potential therapeutic targets for anti-cancer therapy. Adv. Drug Deliv. Rev. 2016, 99, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Awasthi, N.; Schwarz, M.A.; Zhang, C.; Schwarz, R.E. Augmentation of nab-paclitaxel chemotherapy response by mechanistically diverse antiangiogenic agents in preclinical gastric cancer models. Mol. Cancer Ther. 2018, 17, 2353–2364. [Google Scholar] [CrossRef] [PubMed]
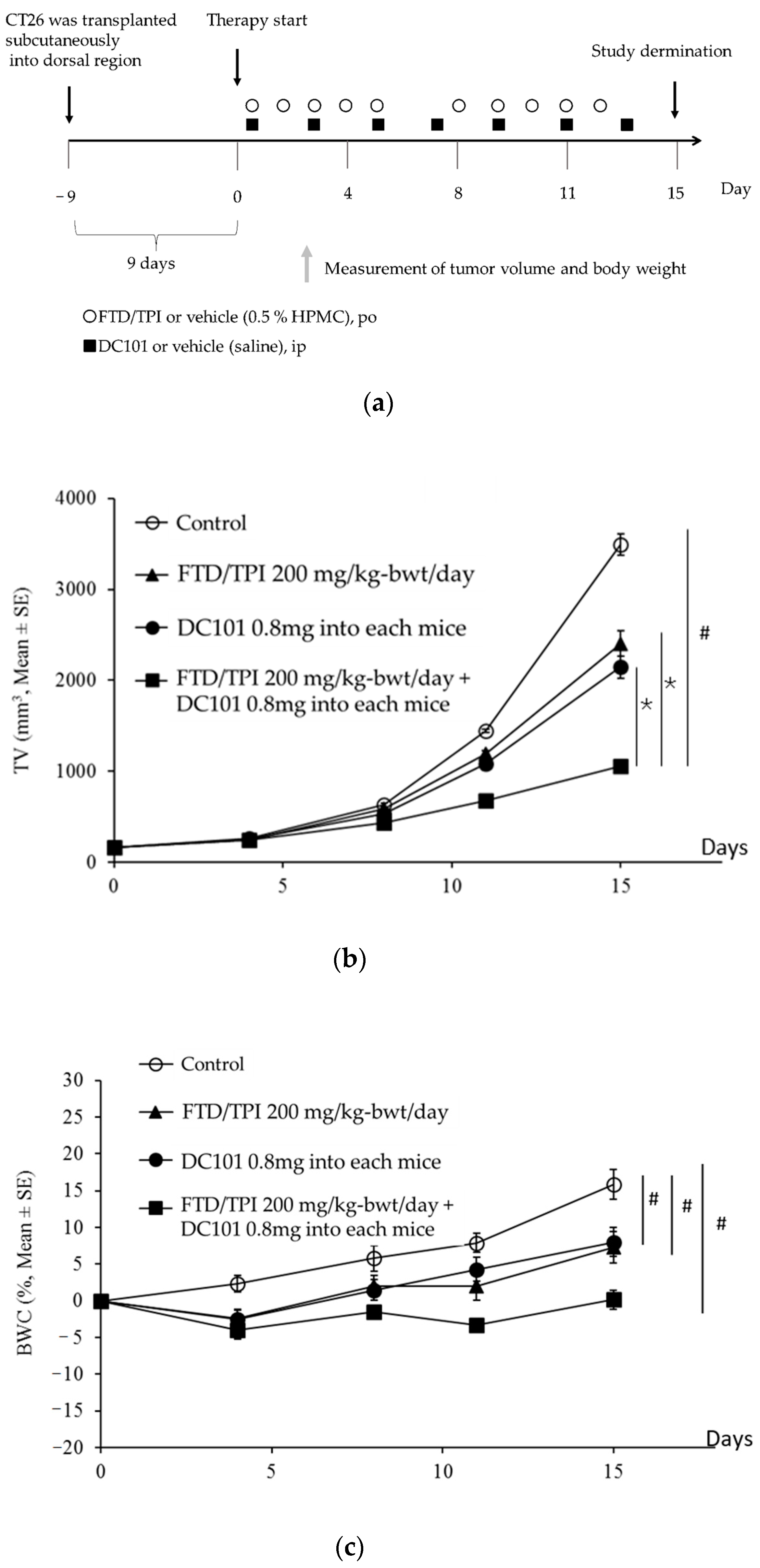


| Drug | Schedule Route | Number of Animals | TV (a) (mm3, Mean ± SE) | p-Value Aspin–Welch | TGI (b) | BWC (c) (%, Mean ± SE) | ||
|---|---|---|---|---|---|---|---|---|
| Control | FTD/TPI | DC101 | ||||||
| Control | Days 1–5 and 8–12 (sid, po) + Days 1, 3, 5, 7, 9, 11, and 13(sid, ip) | 6 | 3491.8 ± 120.7 | 15.8 ± 2.0 | ||||
| FTD/TPI 200 mg/kg-bwt/day | Days 1–5 and 8–12 (sid, po) | 6 | 2404.9 ± 141.8 | <0.001 | 30.6 | 7.3 ± 2.2 | ||
| DC101 0.8 mg into each mouse | Days 1, 3, 5, 7, 9, 11, and 13 (sid, ip) | 6 | 2145.2 ± 123.8 | <0.001 | 38.0 | 8.0 ± 2.0 | ||
| FTD/TPI 200 mg/kg-bwt/day + DC101 0.8 mg into each mouse | Days 1–5 and 8–12 (sid, po) + Days 1, 3, 5, 7, 9, 11, and 13 (sid, ip) | 6 | 1052.3 ± 67.5 | <0.001 | <0.001 | <0.001 | 69.3 | 0.1 ± 1.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsunekuni, K.; Kawakami, H.; Matsuoka, K.; Nagase, H.; Mitani, S.; Nakagawa, K. Efficacy of Combination Chemotherapy Using a Novel Oral Chemotherapeutic Agent, FTD/TPI, with Ramucirumab Murine Version DC101 in a Mouse Syngeneic Cancer Transplantation Model. J. Clin. Med. 2020, 9, 4050. https://doi.org/10.3390/jcm9124050
Tsunekuni K, Kawakami H, Matsuoka K, Nagase H, Mitani S, Nakagawa K. Efficacy of Combination Chemotherapy Using a Novel Oral Chemotherapeutic Agent, FTD/TPI, with Ramucirumab Murine Version DC101 in a Mouse Syngeneic Cancer Transplantation Model. Journal of Clinical Medicine. 2020; 9(12):4050. https://doi.org/10.3390/jcm9124050
Chicago/Turabian StyleTsunekuni, Kenta, Hisato Kawakami, Kazuaki Matsuoka, Hideki Nagase, Seiichiro Mitani, and Kazuhiko Nakagawa. 2020. "Efficacy of Combination Chemotherapy Using a Novel Oral Chemotherapeutic Agent, FTD/TPI, with Ramucirumab Murine Version DC101 in a Mouse Syngeneic Cancer Transplantation Model" Journal of Clinical Medicine 9, no. 12: 4050. https://doi.org/10.3390/jcm9124050
APA StyleTsunekuni, K., Kawakami, H., Matsuoka, K., Nagase, H., Mitani, S., & Nakagawa, K. (2020). Efficacy of Combination Chemotherapy Using a Novel Oral Chemotherapeutic Agent, FTD/TPI, with Ramucirumab Murine Version DC101 in a Mouse Syngeneic Cancer Transplantation Model. Journal of Clinical Medicine, 9(12), 4050. https://doi.org/10.3390/jcm9124050





