Is Interleukin 17 (IL-17) Expression A Common Point in the Pathogenesis of Depression and Obesity?
Abstract
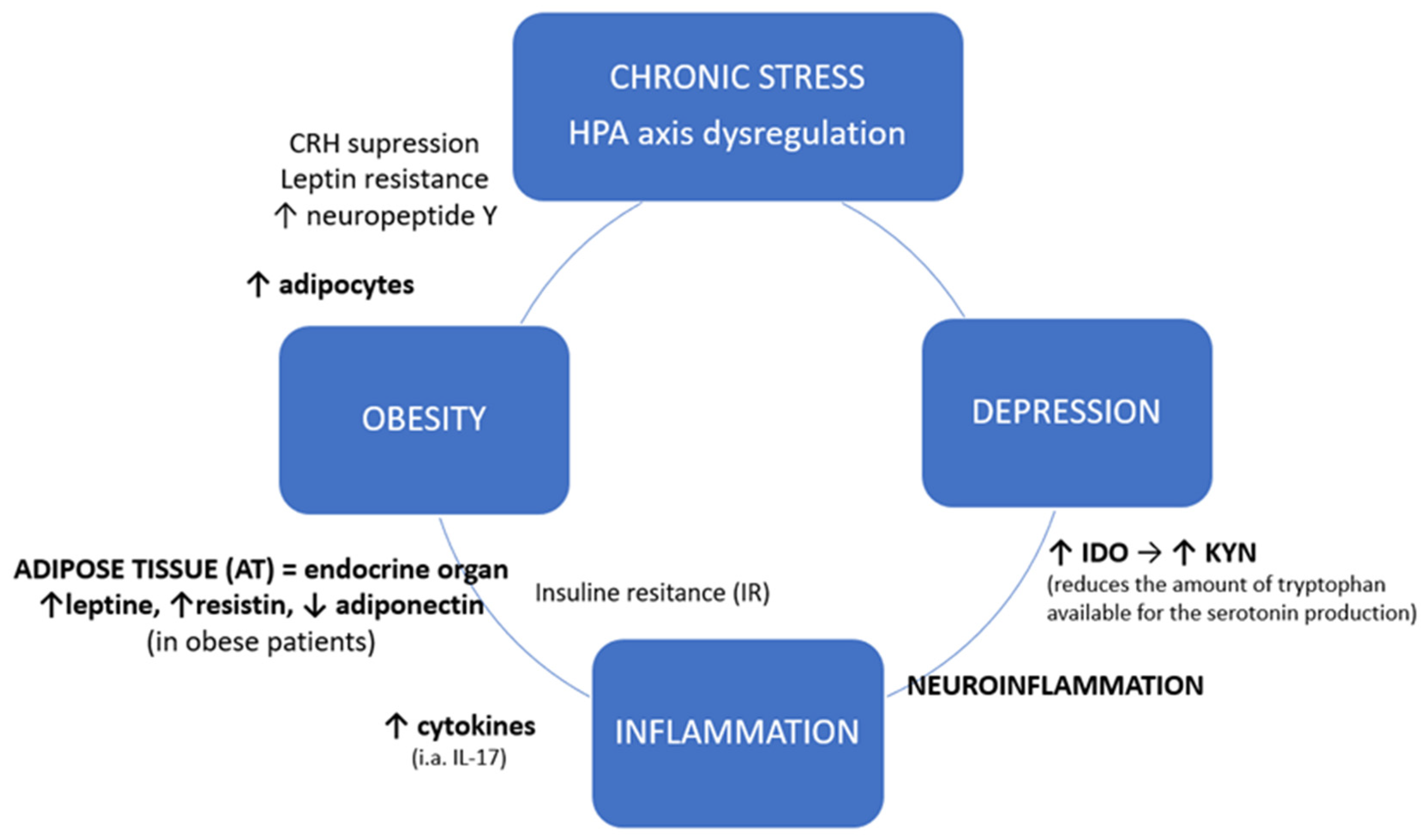
1. Introduction
2. Experimental Section
2.1. Participants and Data Collection
2.2. Interleukin 17–Protein Expression
2.2.1. Determination of Protein Concentration
2.2.2. Enzyme-Linked Immunosorbent Assay (ELISA)
2.3. Interleukin 17 Gene–mRNA Expression
2.3.1. Total RNA Isolation
2.3.2. Quality Analysis of Isolated RNA
2.3.3. RT-PCR Reverse Transcription
2.3.4. Real-Time PCR Reaction
2.4. Statistical Analysis
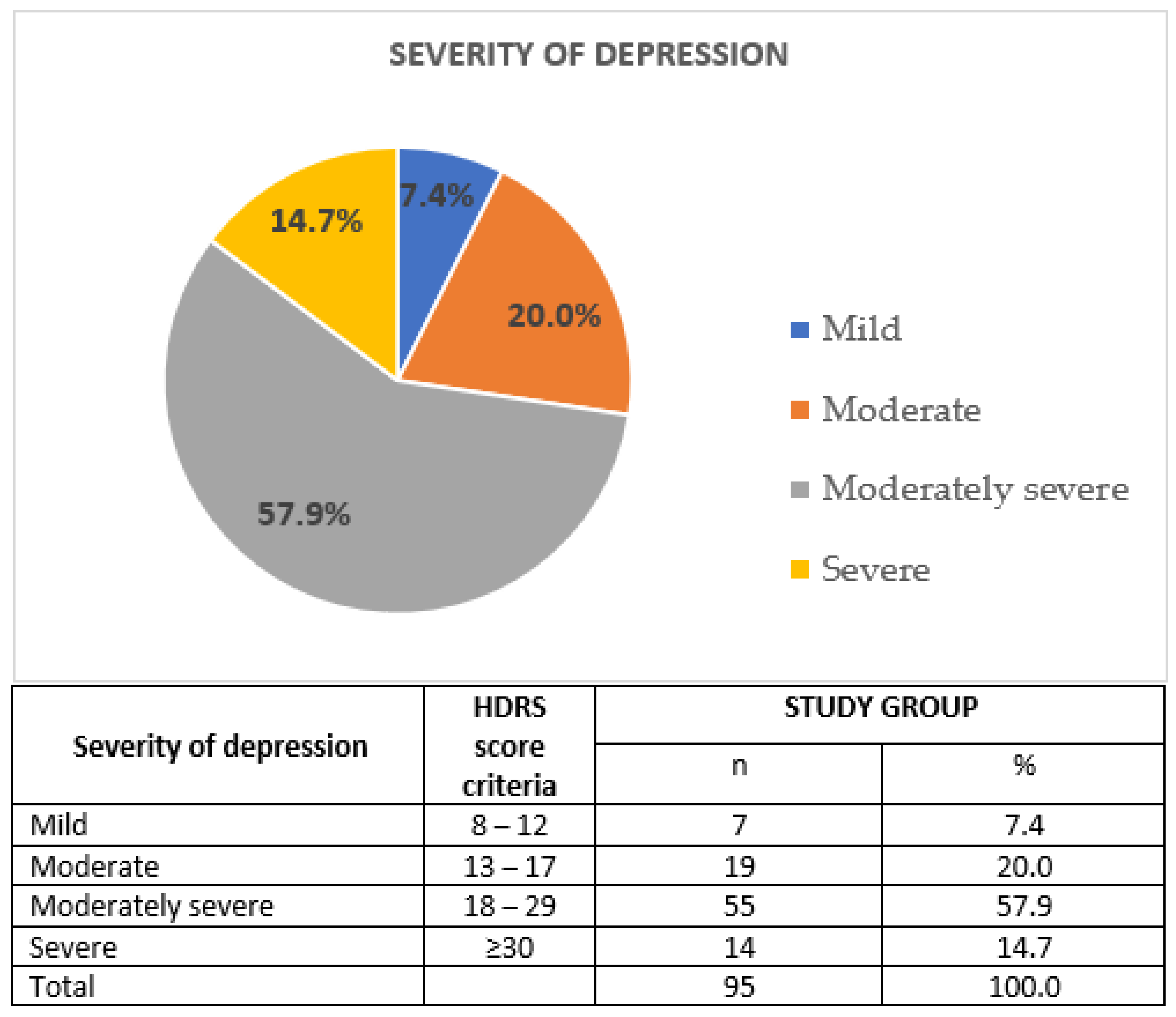
3. Results
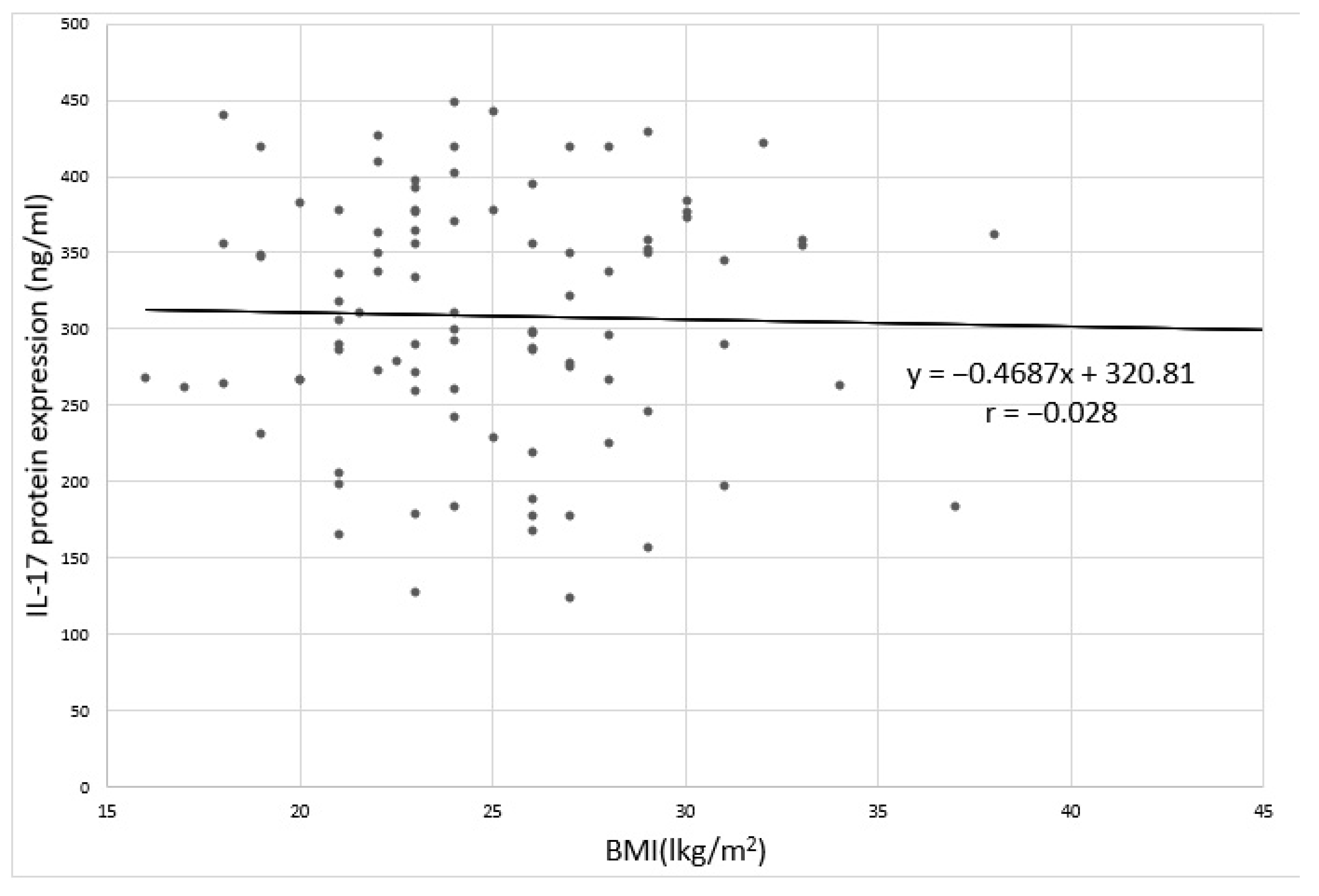
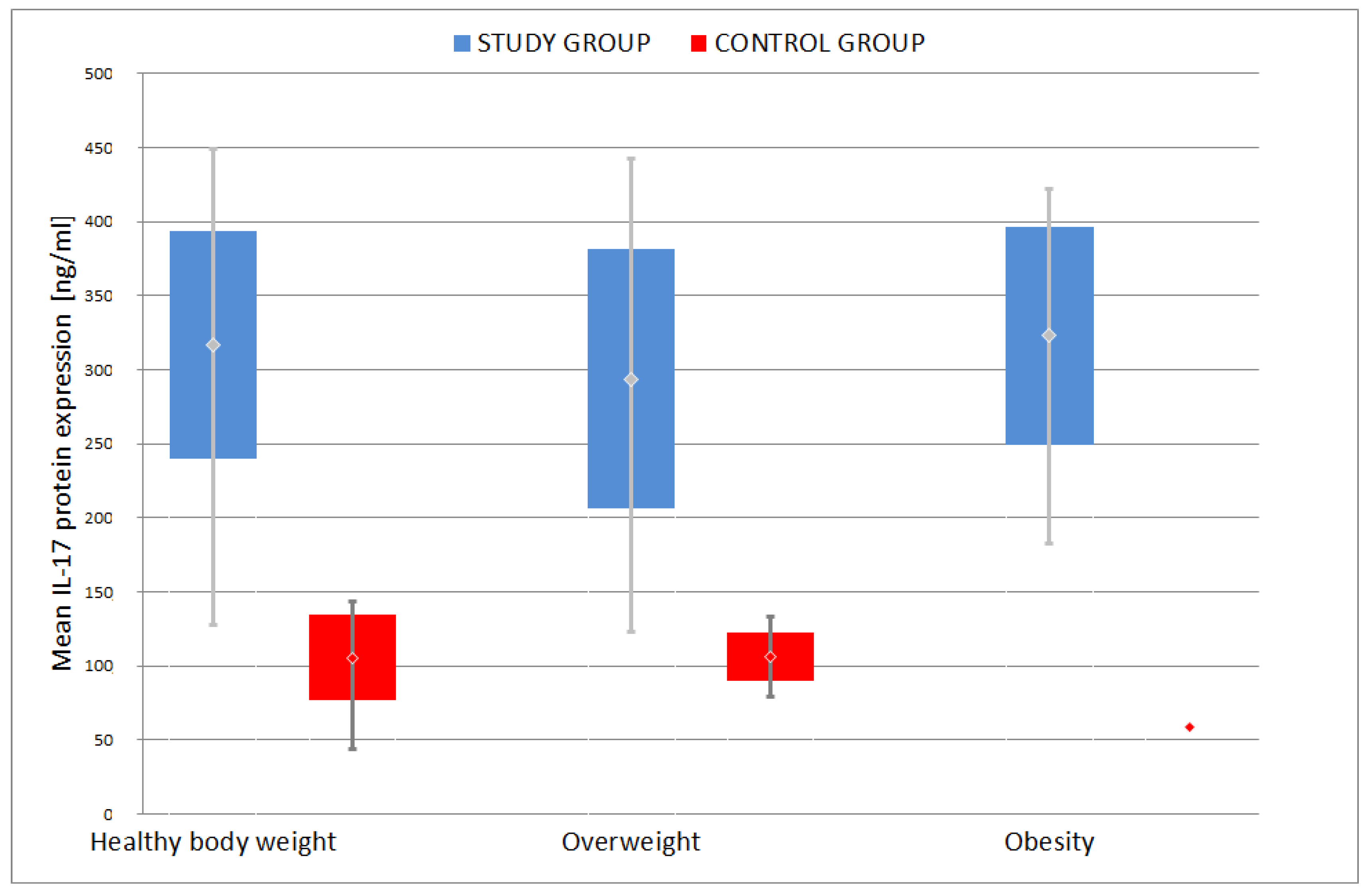
3.1. Body Mass Index (BMI)
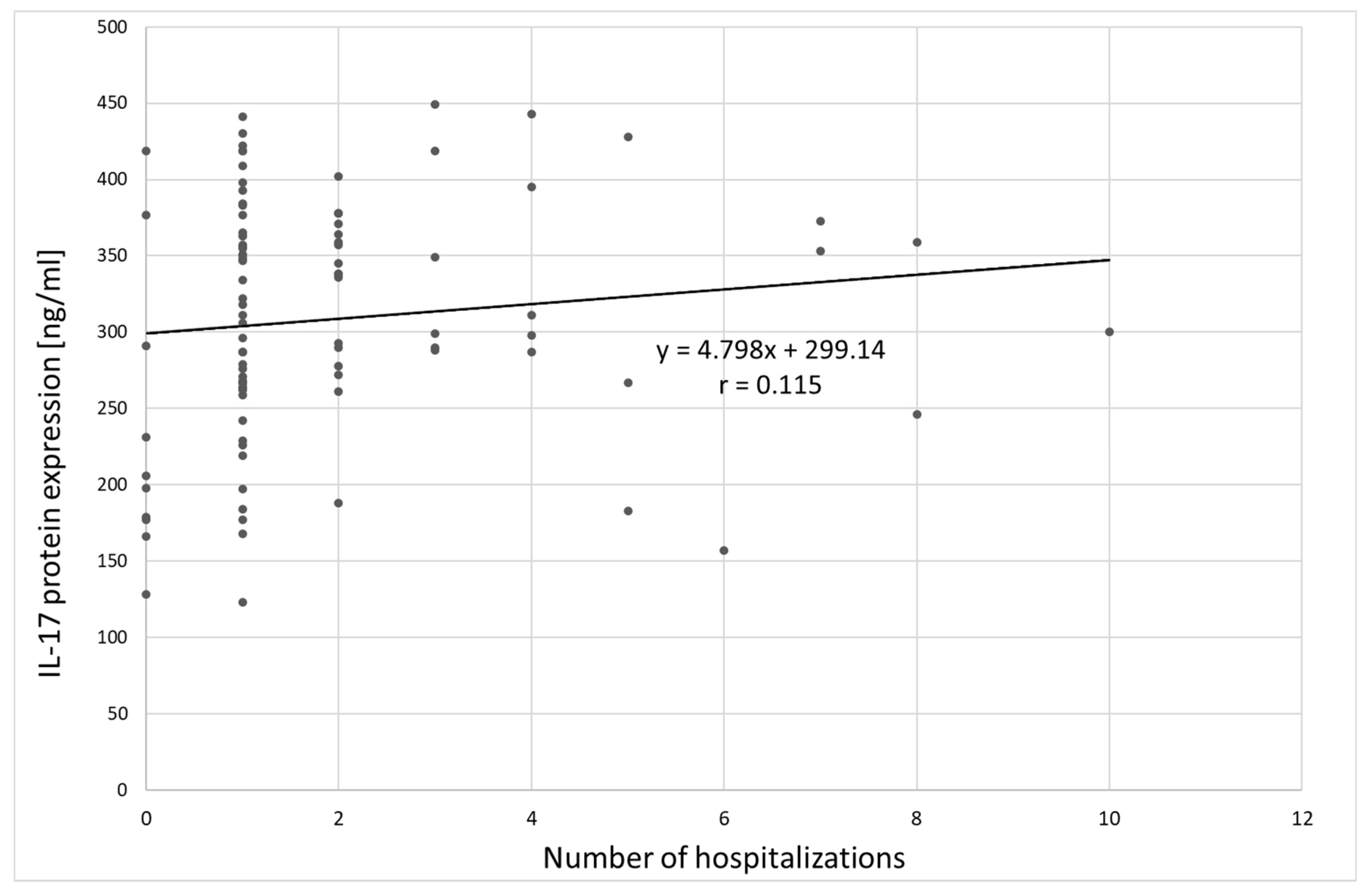
3.2. Interleukin 17 Expression
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ufnal, M.; Wolynczyk-Gmaj, D. The brain and cytokines—The mutual origin of depression, obesity and cardiovascular diseases? Postępy Hig. Med. Dosw. 2011, 65, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Nelson, J.C.; Pikalov, A.; Berman, R.M. Augmentation treatment in major depressive disorder: Focus on aripiprazole. Neuropsychiatr. Dis. Treat. 2008, 4, 937–948. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Calamaro, C.J.; Waite, R. Depression and Obesity in Adolescents. J. Nurse Pract. 2009, 5, 255–261. [Google Scholar] [CrossRef]
- Angst, J.; Gamma, A.; Sellaro, R.; Zhang, H.; Merikangas, K. Toward validation of atypical depression in the community: Results of the Zurich cohort study. J. Affect. Disord. 2002, 72, 125–138. [Google Scholar] [CrossRef]
- Thase, M.E. Atypical depression: Useful concept, but it’s time to revise the DSM-IV criteria. Neuropsychophar Macol. 2009, 34, 2633–2641. [Google Scholar] [CrossRef] [PubMed]
- Güngör, B.B.; AKGÜL, A.I.; Taymur, I.; Demirci, H.; Inel, A. Evaluation of Eating Attitudes, Anger and Impulsivity in Atypical and Non-Atypical Depression and Assessment of Comorbidity of Binge Eating. Psychiatr. Danub. 2020, 32, 105–114. [Google Scholar] [CrossRef]
- World Health Organization. Depression; Fact Sheet No. 369; World Health Organization: Geneva, Switzerland, 2012; Available online: http://wwwwhoint/mediacentre/factsheets/fs369/en/indexhtml (accessed on 30 March 2018).
- World Health Organization. Obesity and Overweight; Fact Sheet No. 311; World Health Organization: Geneva, Switzerland, 2013; Available online: http://wwwwhoint/mediacentre/factsheets/fs311/en/ (accessed on 30 March 2018).
- Karakus, M.C.; Okunade, A.A. Obesity with Comorbid Depression and Early Retirement (June 2007). In Proceedings of the IHEA 2007 6th World Congress: Explorations in Health Economics, Copenhagen, Denmark, 8–11 July 2007; Available online: https://ssrn.com/abstract=992241 (accessed on 3 March 2018).
- Fostick, L.; Silberman, A.; Beckman, M.; Spivak, B.; Amital, D. The economic impact of depression: Resistance or severity? Eur. Neuropsychopharmacol. 2010, 20, 671–675. [Google Scholar] [CrossRef]
- Garg, R.; Saxena, S.K.; Bashi, S. Is obesity a risk to depression? A cross-sectional study. Ind. Psychiatry J. 2019, 28, 130–134. [Google Scholar]
- Hryhorczuk, C.; Sharma, S.; Fulton, S.E. Metabolic disturbances connecting obesity and depression. Front. Neurosci. 2013, 7, 177. [Google Scholar] [CrossRef]
- de Melo, L.G.P.; Nunes, S.O.V.; Anderson, G.; Vargas, H.O.; Barbosa, D.S.; Galecki, P.; Carvalho, A.F.; Maes, M. Shared metabolic and immune-inflammatory, oxidative and nitrosative stress pathways in the metabolic syndrome and mood disorders. Prog. Neuro-psychopharmacol. Biol. Psychiatry 2017, 78, 34–50. [Google Scholar] [CrossRef]
- Nieuwenhuizen, A.G.; Rutters, F. The hypothalamic-pituitary-adrenal axis in the regulation of energy balance. Physiol. Behav. 2008, 94, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Kuo, L.E.; Kitlinska, J.B.; Tilan, J.U.; Li, L.; Baker, S.B.; Johnson, M.D.; Lee, E.W.; Burnett, M.S.; Fricke, S.T.; Kvetnansky, R.; et al. Neuropeptide Y acts directly in the periphery on fat tissue and mediates stress-induced obesity and metabolic syndrome. Nat. Med. 2007, 13, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Abima, R.S. Adipose tissue as an endocrine organ. Obesity (Silver Spring) 2006, 14 (Suppl. 5), 242S–249S. [Google Scholar] [CrossRef]
- Shelton, R.C.; Miller, A.H. Inflammation in depression is adiposity a cause? Dialogues Clin. Neurosci. 2011, 13, 41–53. [Google Scholar]
- Aguilar-Valles, A.; Inoue, W.; Rummel, C.; Luheshi, G.N. Obesity, adipokines and neuroinflammation. Neuropharmacology 2015, 96, 124–134. [Google Scholar] [CrossRef]
- Odegaard, J.J.; Chawla, A. Pleotropic actions of insulin resistance and inflammation in metabolic homeostatis. Science 2013, 339, 172–177. [Google Scholar] [CrossRef]
- Chehim, M.; Vidal, H.; Elijaafari, A. Pathogenic Role of IL-17-Producing Immune Cells in Obesity, and Related Inflammatory. Dis. J. Clin. Med. 2017, 6, 68. [Google Scholar] [CrossRef]
- Winer, S.; Chan, Y.; Paltser, G.; Truong, D.; Tsui, H.; Bahrami, J.; Dorfman, R.; Wang, Y.; Zielenski, J.; Mastronardi, F.; et al. Normalization of obesity-associated insulin resitance though immunotherapy. Nat. Med. 2009, 15, 921–929. [Google Scholar] [CrossRef]
- Varricchi, G.; Granata, F.; Loffredo, S.; Genovese, A.; Marone, G. Angiogenesis and lymphangiogenesis in inflammatory skin disorders. J. Am. Acad. Dermatol. 2015, 73, 144–153. [Google Scholar] [CrossRef]
- Ryan, C.; Kirby, B. Psoriasis is a systemic disease with multiple cardiovascular and metabolic comorbidities. Dermatol. Clin. 2015, 33, 41–55. [Google Scholar] [CrossRef]
- Cao, Y. Angiogenesis modulates adipogenesis and obesity. J. Clin. Investig. 2007, 117, 2362–2368. [Google Scholar] [CrossRef] [PubMed]
- Voiculescu, V.M.; Lupu, M.; Papagheorghe, L.; Giurcaneanu, C.; Micu, E. Psoriasis and Metabolic Syndrome—Scientific evidence and therapeutic implications. J. Med. Life 2014, 7, 468–471. [Google Scholar] [PubMed]
- Guillemot-Legris, O.; Muccioli, G.G. Obesity-induced neuroinflammation: Beyond the hypothalamus. Trends Neurosci. 2017, 40, 237–253. [Google Scholar] [CrossRef] [PubMed]
- Sforzini, L.; Nettis, M.A.; Mondelli, V.; Pariante, C.M. Inflammation in cancer and depression: A starring role for the kynurenine pathway. Psychopharmacology 2019, 236, 2997–3011. [Google Scholar] [CrossRef] [PubMed]
- Ogyu, K.; Kubo, K.; Noda, Y.; Iwata, Y.; Tsugawa, S.; Omura, Y.; Wada, M.; Tarumi, R.; Plitman, E.; Moriguchi, S.; et al. Kynurenine pathway in depression: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2018, 6, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Kowalczyk, M.; Szemraj, J.; Bliźniewska, K.; Maes, M.; Berk, M.; Su, K.P.; Gałecki, P. An immune gate of depression—Early neuroimmune development in the formation of the underlying depressive disorder. Pharmacol. Rep. 2019, 71, 1299–1307. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems; 10th Revision; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Lim, J.U.; Lee, J.H.; Kim, J.S.; Hwang, Y.I.; Kim, T.-H.; Lim, S.Y.; Yoo, K.H.; Jung, K.-S.; Kim, Y.K.; Rhee, C.K. Comparison of World Health Organization and Asia-Pacific body mass index classifications in COPD patients. Int. J. Chronic Obs. Pulm. Dis. 2017, 12, 2465–2475. [Google Scholar] [CrossRef]
- Patten, S. Performance of the Composite International Diagnostic Interview Short Form for major depression in community and clinical samples. Chronic Dis. Can. 1997, 3, 18–24. [Google Scholar]
- Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 56–62. [Google Scholar] [CrossRef]
- Demyttenaere, K.; De Fruyt, J. Getting what you ask for: On the selectivity of depression rating scales. Psychother. Psychosom. 2003, 72, 61–70. [Google Scholar] [CrossRef]
- Schmittgen, T.D.; Livak, K.J. Analyzing real-time PCR data by the comparative CT method. Nat. Protoc. 2008, 3, 1101–1108. [Google Scholar] [CrossRef] [PubMed]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Maes, M.; Carvalho, A.F. The Compensatory Immune-Regulatory Reflex System (CIRS) in Depression and Bipolar Disorder. Mol. Neurobiol. 2018, 55, 8885–8903. [Google Scholar] [CrossRef] [PubMed]
- Ouakinin, S.R.; Barreira, D.P.; Gois, C.J. Depression and obesity: Integrating the role of stres, neuroendorine dysfunction and inflammatory pathways. Front. Endocrinol. 2018, 9, 431. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.C.; Chou, Y.C.; Chen, H.C.; Lu, C.C.; Chang, D.M. Interleukin-6 and interleukin-17 are related to depression in patients with rheumatoid arthritis. Int. J. Rheum. Dis. 2019, 22, 980–985. [Google Scholar] [CrossRef] [PubMed]
- Tsuboi, H.; Sakakibara, H.; Minamida, Y.; Tsujiguchi, H.; Matsunaga, M.; Hara, A.; Nakamura, H. Elevated Levels of Serum IL-17A in Community-Dwelling Women with Higher Depressive Symptoms. Behav. Sci. 2018, 8, 102. [Google Scholar] [CrossRef]
- Chen, Y.; Jiang, T.; Chen, P.; Ouyang, J.; Xu, G.; Zeng, Z.; Sun, Y. Emerging tendency towards autoimmune process in major depressive patients: A novel insight from Th17 cells. Psychiatry Res. 2011, 188, 224–230. [Google Scholar] [CrossRef]
- Davami, M.H.; Baharlou, R.; Ahmadi Vasmehjani, A.; Ghanizadeh, A.; Keshtkar, M.; Dezhkam, I.; Atashzar, M.R. Elevated IL-17 and TGF-beta Serum Levels: A Positive Correlation between T-helper 17 Cell-Related Pro-Inflammatory Responses with Major Depressive Disorder. Basic Clin. Neurosci. 2016, 7, 137–142. [Google Scholar]
- Luppino, F.S.; de Wit, L.M.; Bouvy, P.F.; Stijnen, T.; Cuijpers, P.; Penninx, B.W.; Zitman, F.G. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Arch. Gen. Psychiatry 2010, 67, 220–229. [Google Scholar] [CrossRef]
- Markowitz, S.; Friedman, M.A.; Arent, S.M. Understanding the relation between obesity and depression: Causal mechanisms and implications for treatment. Clin. Psychol. Sci. Pract. 2008, 15, 1–20. [Google Scholar] [CrossRef]
- Simon, G.E.; Ludman, E.J.; Linde, J.A.; Operskalski, B.H.; Ichikawa, L.; Rohde, P.; Finch, E.A.; Jeffery, R.W. Association between obesity and depression in middle-aged women. Gen. Hosp. Psychiatry 2008, 30, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.; Gaffen, S.L. IL-17 in obesity and adipogenesis. Cytokine Growth Factor Rev. 2010, 21, 449–453. [Google Scholar] [CrossRef] [PubMed]
- Sumarac-Dumanovic, M.; Stevanovic, D.; Ljubic, A.; Jorga, J.; Simic, M.; Stamenkovic-Pejkovic, D.; Starcevic, V.; Trajkovic, V.; Micic, D. Increased activity of interleukin-23/interleukin-17 proinflammatory axis in obese women. Int. J. Obes. 2009, 33, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Bugge, E.; Wynn, R.; Mollnes, T.E.; Reitan, S.K.; Gronli, O.K. Cytokine profiles and diagnoses in elderly, hospitalized psychiatric patients. BMC Psychiatry 2018, 18, 315. [Google Scholar] [CrossRef] [PubMed]
- Benros, M.E.; Waltoft, B.L.; Nordentoft, M.; Ostergaard, S.D.; Eaton, W.W.; Krogh, J.; Mortensen, P.B. Autoimmune diseases and severe infections as risk factors for mood disorders: A nationwide study. JAMA Psychiatry 2013, 70, 812–820. [Google Scholar] [CrossRef]
- Loft, N.D.; Halling, A.-S.; Egeberg, A.; Skov, L. Efficacy of a second IL-17 inhibitor in patients with psoriasis: A systematic review and meta-analysis. J. Am. Acad. Dermatol. 2020. [Google Scholar] [CrossRef]
- Deodhar, A.; Mease, P.; McInnes, I.B.; Baraliakos, X.; Reich, K.; Blauvelt, A.; Leonardi, C.; Porter, B.; Das Gupta, A.; Widmer, A.; et al. Long-term safety of secukinumab inpatients with moderate-to-severe plaque psoriasis, psoriatic arthritis, and ankylosing spondylitis: Integrated pooled clinical trial and post-marketing surveillance data. Arthritis Res. Ther. 2019, 21, 111. [Google Scholar] [CrossRef]
- Nothdurfter, C.; Milenkovic, V.M.; Sarubin, N.; Hilbert, S.; Manook, A.; Weigl, J.; Almeqbaali, K.; Wetzel, C.H.; Rupprecht, R.; Baghai, T.C. The cytokine IL-17A as a marker of treatment resistance in major depressive disorder? Eur. J. Neurosci. 2019. [Google Scholar] [CrossRef]
- Esposito, M.; Giunta, A.; Del Duca, E.; Manfreda, V.; Troisi, A.; Bianchi, L.; Fargnoli, M.C. Long-term safety and efficacy of secukinumab in patients with psoriasis and major psychiatric disorders: A case series. Postgrad. Med. 2020, 132, 172–175. [Google Scholar] [CrossRef]
- Albeltagy, E.S.; Elaziz, S.Y.A.; Abozaid, S.Y.; El Zomor, H.M.; Elhamed, S.S.A. Interleukin 6, interleukin 17, disease-related and contextual factor association with depression, and its severity in patients with rheumatoid arthritis. Clin. Rheumatol. 2020, 13. [Google Scholar] [CrossRef]
- Krueger, J.G.; Brunner, P.M. Interleukin-17 alters the biology of many cell types involved in the genesis of psoriasis, systemic inflammation and associated comorbidities. Exp. Dermatol. 2018, 27, 115–123. [Google Scholar] [CrossRef] [PubMed]




| Variable | Group | Means Comparison | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Control | |||||||||||
| Gender | n | % | n | % | χ2 = 0.298; p = 0.585 | |||||||
| M | 27 | 28.4 | 7 | 23.3 | ||||||||
| F | 68 | 71.6 | 23 | 76.7 | ||||||||
| min | max | SD | V(%) | min | max | SD | V(%) | Z = 4.208;p= 0.000 * | ||||
| AGE [yrs] | 18 | 63 | 47.2 | 10.5 | 22.3 | 23 | 53 | 37.7 | 10.5 | 27.7 | ||
| BMI [kg/m2] | 16 | 48 | 25.1 | 4.9 | 19.5 | 19.3 | 33.9 | 24.5 | 3.9 | 15.9 | Z = 0.402; p = 0.688 | |
| Duration of depression [yrs] | 1 | 30 | 5.5 | 5.8 | 105.8 | |||||||
| No. Depressive episodes | 1 | 20 | 4.2 | 4.4 | 105.6 | |||||||
| No. hospitalizations | 0 | 10 | 1.9 | 1.9 | 100.1 | |||||||
| HDRS | 7 | 37 | 21.9 | 6.8 | 30.8 | |||||||
| Variable | Group | Means Comparison | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| STUDY | CONTROL | ||||||||||
| min | max | SD | V(%) | min | max | SD | V(%) | ||||
| IL-17 mRNA (2-Δct) | 0.201 | 0.613 | 0.518 | 0.089 | 17.2 | 0.048 | 0.393 | 0.238 | 0.070 | 29.5 | Z = 7.934; p = 0.000 * |
| IL-17 (ng/mL) | 123 | 449 | 309.1 | 79.5 | 25.7 | 44 | 143 | 104.2 | 25.1 | 24.1 | Z = 8.151; p = 0.000 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bliźniewska-Kowalska, K.; Szewczyk, B.; Gałecka, M.; Su, K.-P.; Maes, M.; Szemraj, J.; Gałecki, P. Is Interleukin 17 (IL-17) Expression A Common Point in the Pathogenesis of Depression and Obesity? J. Clin. Med. 2020, 9, 4018. https://doi.org/10.3390/jcm9124018
Bliźniewska-Kowalska K, Szewczyk B, Gałecka M, Su K-P, Maes M, Szemraj J, Gałecki P. Is Interleukin 17 (IL-17) Expression A Common Point in the Pathogenesis of Depression and Obesity? Journal of Clinical Medicine. 2020; 9(12):4018. https://doi.org/10.3390/jcm9124018
Chicago/Turabian StyleBliźniewska-Kowalska, Katarzyna, Bernadeta Szewczyk, Małgorzata Gałecka, Kuan-Pin Su, Michael Maes, Janusz Szemraj, and Piotr Gałecki. 2020. "Is Interleukin 17 (IL-17) Expression A Common Point in the Pathogenesis of Depression and Obesity?" Journal of Clinical Medicine 9, no. 12: 4018. https://doi.org/10.3390/jcm9124018
APA StyleBliźniewska-Kowalska, K., Szewczyk, B., Gałecka, M., Su, K.-P., Maes, M., Szemraj, J., & Gałecki, P. (2020). Is Interleukin 17 (IL-17) Expression A Common Point in the Pathogenesis of Depression and Obesity? Journal of Clinical Medicine, 9(12), 4018. https://doi.org/10.3390/jcm9124018







