Treatment of Heart Failure Patients with Anxiolytics Is Associated with Adverse Outcomes, with and without Depression
Abstract
1. Background
2. Methods
3. Results
3.1. Clinical Parameters
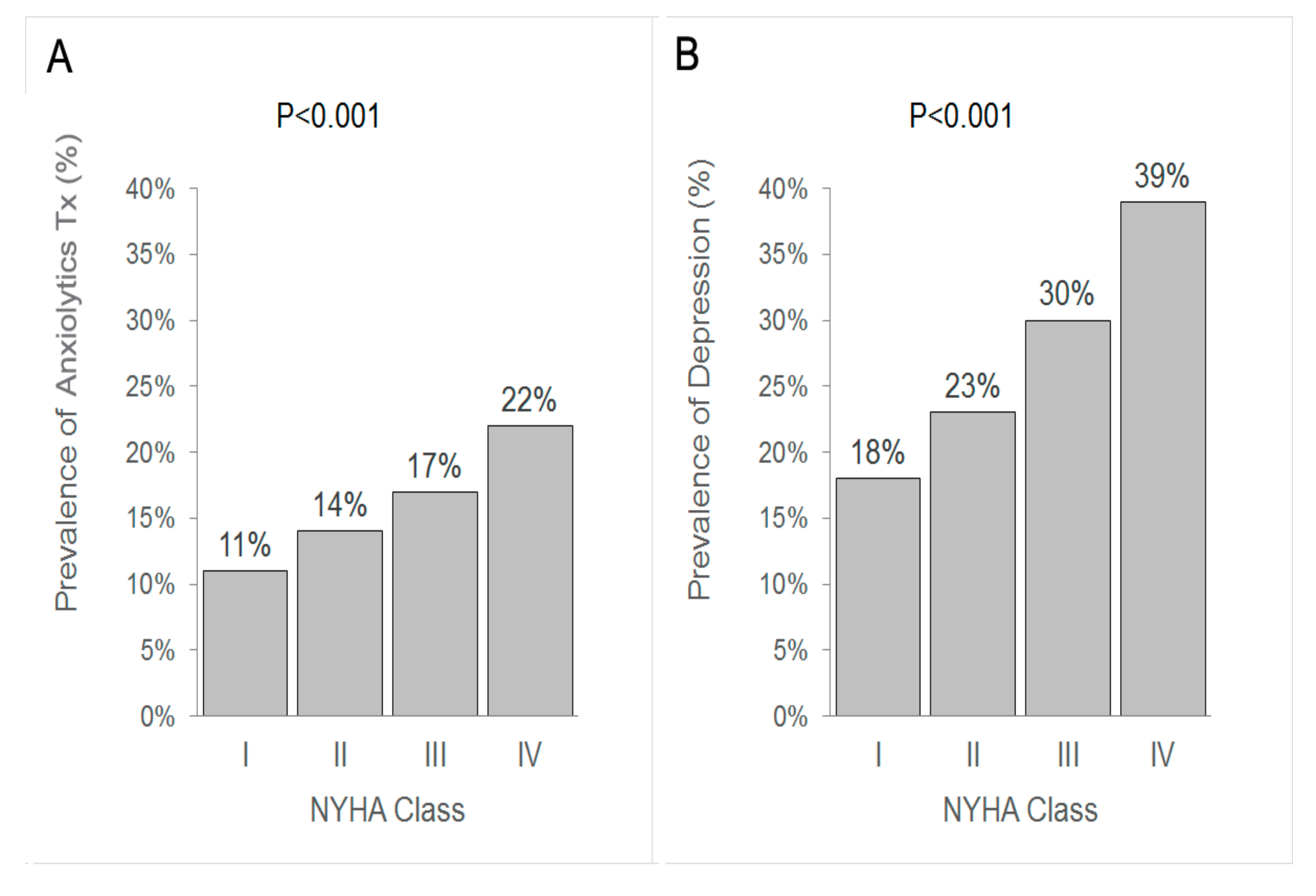
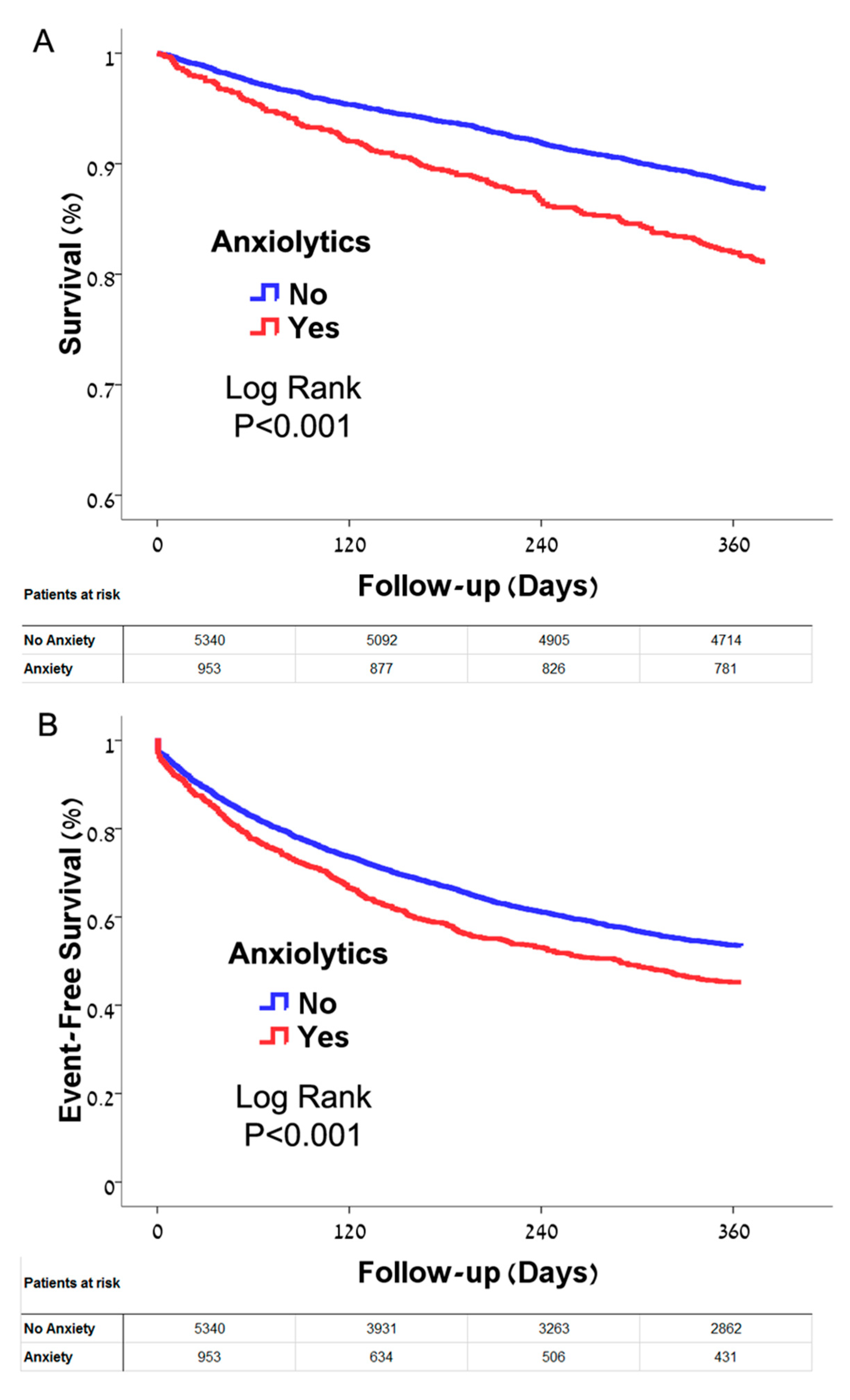
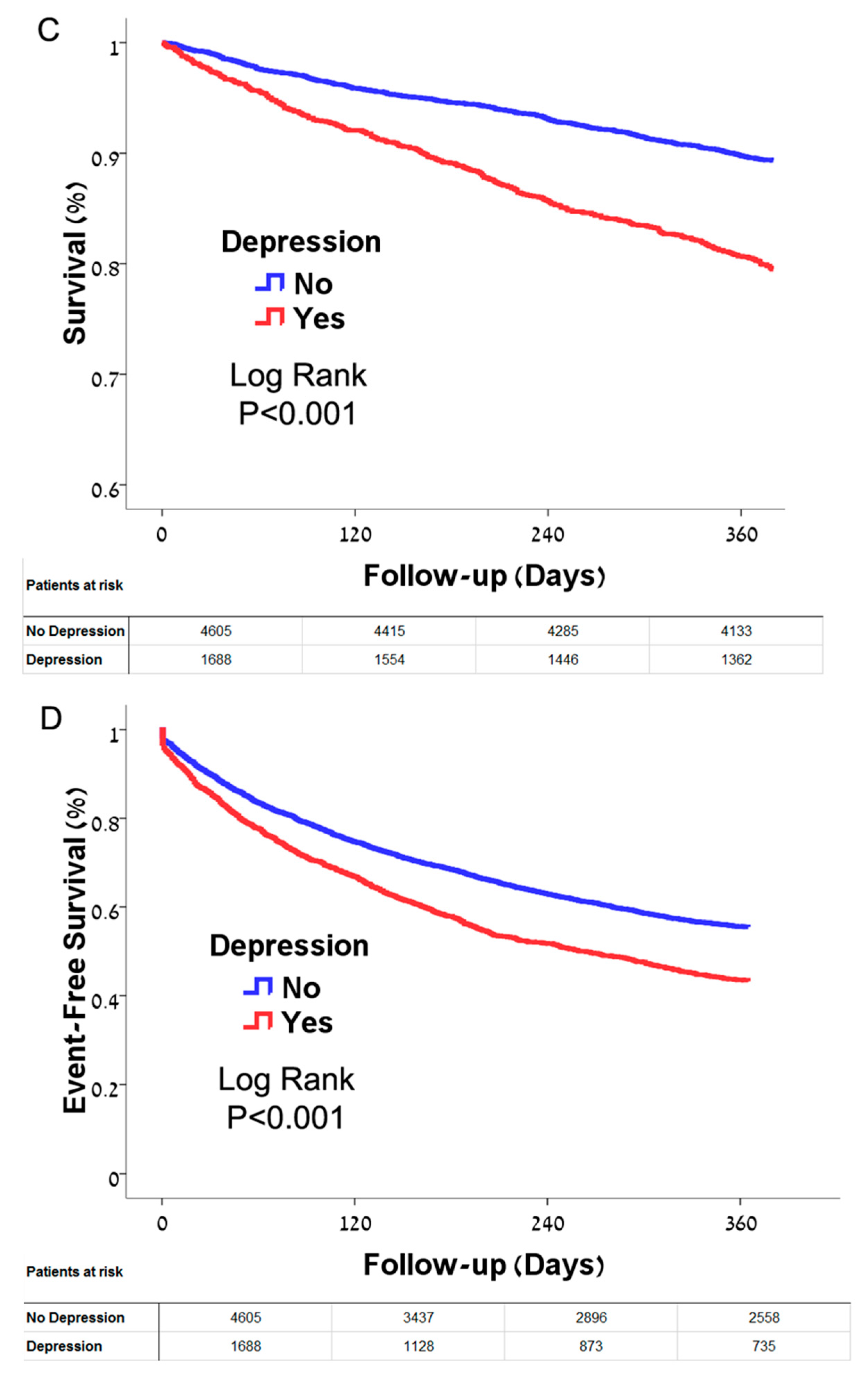
3.2. Treatment for Anxiety, Depression and Clinical Outcomes
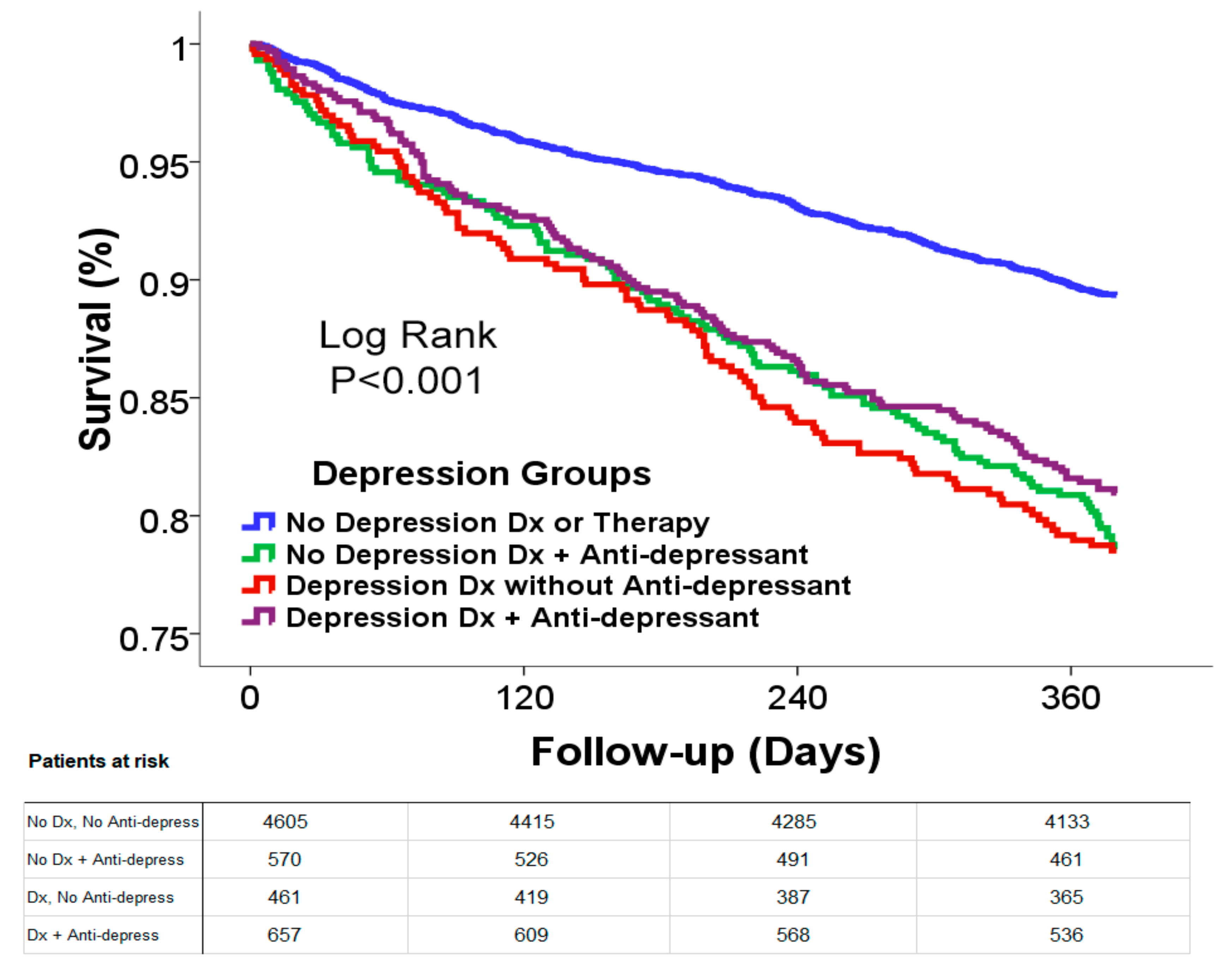
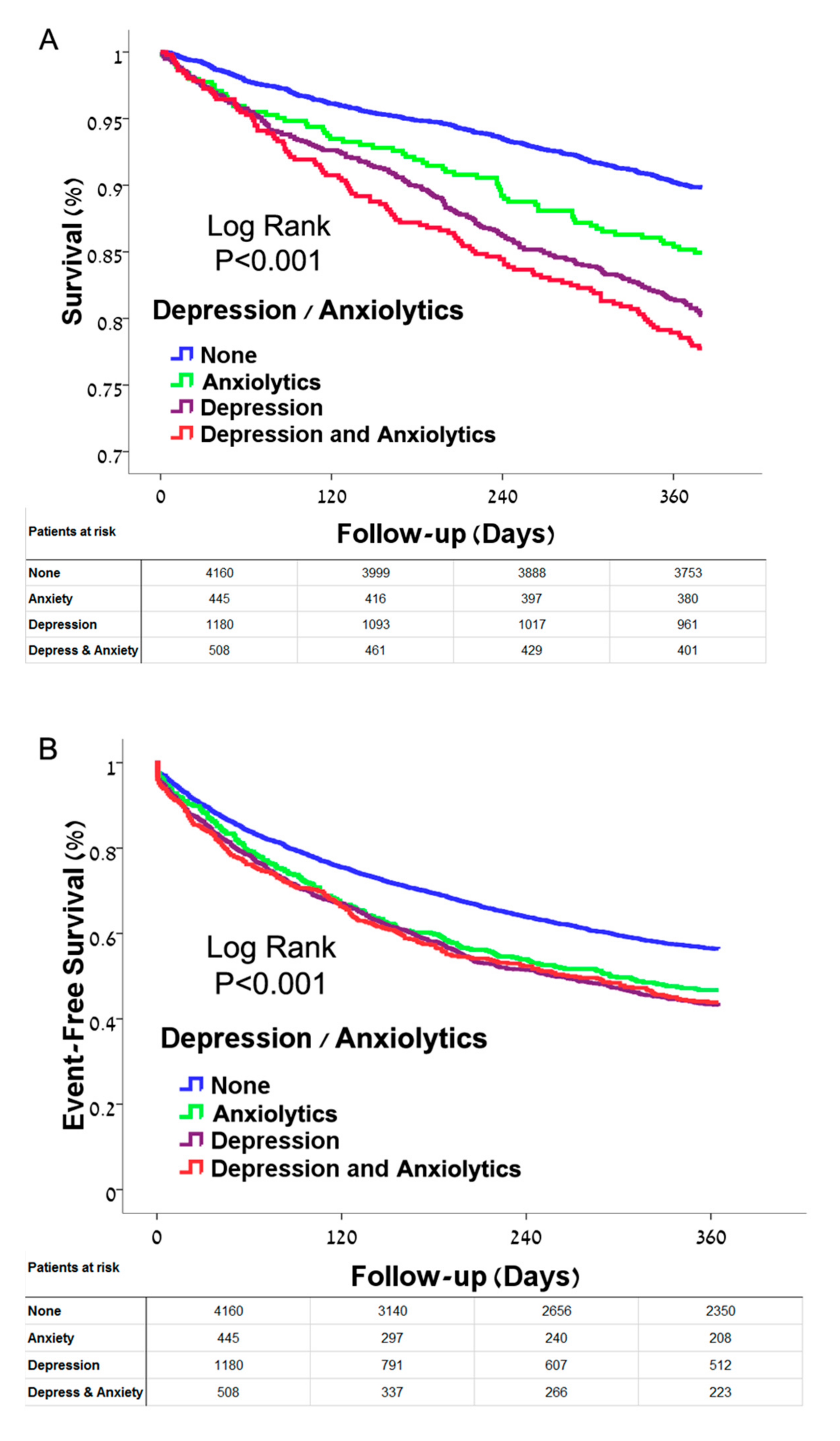
3.3. Comorbid Suspected Anxiety and Depression and Clinical Outcomes
3.4. Analysis of Anxiolytics and Depression/Antidepressant Therapy as Time-Dependent Variables
4. Discussion
Limitations
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CI | confidence intervals |
| HF | heart failure |
| HFPEF | heart failure with preserved ejection fraction |
| HFREF | heart failure with reduced ejection fraction |
| HMO | health maintenance organization |
| HR | hazard ratio |
| SSRIs | selective serotonin reuptake inhibitors |
References
- Kessler, R.C.; Petukhova, M.; Sampson, N.A.; Zaslavsky, A.M.; Wittchen, H.-U. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int. J. Methods Psychiatr. Res. 2012, 21, 169–184. [Google Scholar] [CrossRef] [PubMed]
- Hohls, J.K.; König, H.-H.; Raynik, Y.I.; Hajek, A. A systematic review of the association of anxiety with health care utilization and costs in people aged 65 years and older. J. Affect. Disord. 2018, 232, 163–176. [Google Scholar] [CrossRef] [PubMed]
- Easton, K.; Coventry, P.; Lovell, K.; Carter, L.-A.; Deaton, C. Prevalence and Measurement of Anxiety in Samples of Patients with Heart Failure Meta-analysis. J. Cardiovasc. Nurs. 2016, 31, 367–379. Available online: www.jcnjournal.com (accessed on 5 July 2020). [CrossRef] [PubMed]
- Ruscio, A.M.; Hallion, L.S.; Lim, C.C.W.; Aguilar-Gaxiola, S.; Al-Hamzawi, A.; Alonso, J.; Andrade, L.H.; Borges, G.; Bromet, E.J.; Bunting, B.; et al. Cross-sectional Comparison of the Epidemiology of DSM-5 Generalized Anxiety Disorder Across the Globe. JAMA Psychiatry 2017, 74, 465–475. [Google Scholar] [CrossRef]
- Olariu, E.; Forero, C.G.; Castro-Rodríguez, J.I.; Rodrigo-Calvo, M.T.; Alvarez, P.; Martín-López, L.M.; Sánchez-Toto, A.; Adroher, N.D.; Blasco, M.J.; Vilagut, G.; et al. detection of anxiety disorders in primary care: A meta-analysis of assisted and unassisted diagnoses. Depress. Anxiety 2015, 32, 471–484. [Google Scholar] [CrossRef]
- Alonso, J.; Liu, Z.; Evans-Lacko, S.; Mph, E.S.; A Sampson, N.; Chatterji, S.; Abdulmalik, J.; Aguilar-Gaxiola, S.; Al-Hamzawi, A.; Andrade, L.; et al. Treatment gap for anxiety disorders is global: Results of the World Mental Health Surveys in 21 countries. Depress. Anxiety 2018, 35, 195–208. [Google Scholar] [CrossRef]
- Rhee, T.G.; Rosenheck, R.A. Initiation of new psychotropic prescriptions without a psychiatric diagnosis among US adults: Rates, correlates, and national trends from 2006 to 2015. Health Serv. Res. 2018, 54, 139–148. [Google Scholar] [CrossRef]
- Jiang, W.; Kuchibhatla, M.; Cuffe, M.S.; Christopher, E.J.; Alexander, J.D.; Clary, G.L.; Blazing, M.A.; Gaulden, L.H.; Califf, R.M.; Krishnan, R.R.; et al. Prognostic Value of Anxiety and Depression in Patients With Chronic Heart Failure. Circulation 2004, 110, 3452–3456. [Google Scholar] [CrossRef]
- Sokoreli, I.; De Vries, J.J.G.; Pauws, S.; Steyerberg, E.W. Depression and anxiety as predictors of mortality among heart failure patients: Systematic review and meta-analysis. Hear. Fail. Rev. 2016, 21, 49–63. [Google Scholar] [CrossRef]
- Celano, C.M.; Villegas, A.C.; Albanese, A.M.; Gaggin, H.K.; Huffman, J.C. Depression and Anxiety in Heart Failure: A Review. Harv. Rev. Psychiatry 2018, 26, 175–184. [Google Scholar] [CrossRef]
- Vongmany, J.; Hickman, L.D.; Lewis, J.; Newton, P.J.; Phillips, J.L. Anxiety in chronic heart failure and the risk of increased hospitalisations and mortality: A systematic review. Eur. J. Cardiovasc. Nurs. 2016, 15, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.; Hsu, B.; Li, Y.; Chen, C.; Lin, J.; Chien, C.; Weng, C.-Y. Prognostic Value of Anxiety between Heart Failure with Reduced Ejection Fraction and Heart Failure with Preserved Ejection Fraction. J. Am. Hear. Assoc. 2019, 8, e010739. [Google Scholar] [CrossRef] [PubMed]
- Baldwin, D.S.; Anderson, I.M.; Nutt, D.J.; Allgulander, C.; Bandelow, B.; Boer, J.A.D.; Christmas, D.M.; Davies, S.; Fineberg, N.; Lidbetter, N.; et al. Evidence-based pharmacological treatment of anxiety disorders, post-traumatic stress disorder and obsessive-compulsive disorder: A revision of the 2005 guidelines from the British Association for Psychopharmacology. J. Psychopharmacol. 2014, 28, 403–439. [Google Scholar] [CrossRef] [PubMed]
- Bandelow, B.; Zohar, J.; Hollander, E.; Kasper, S.; Möller, H.-J.; Guide, W.T.F.O.T. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the Pharmacological Treatment of Anxiety, Obsessive-Compulsive and Post-Traumatic Stress Disorders—First Revision. World J. Biol. Psychiatry 2008, 9, 248–312. [Google Scholar] [CrossRef]
- Wang, Y.; Li, J.-Q.; Shi, J.-F.; Que, J.-Y.; Liu, J.-J.; Lappin, J.M.; Leung, J.; Ravindran, A.V.; Chen, W.-Q.; Qiao, Y.-L.; et al. Depression and anxiety in relation to cancer incidence and mortality: A systematic review and meta-analysis of cohort studies. Mol. Psychiatry 2020, 25, 1487–1499. [Google Scholar] [CrossRef]
- Vikjord, S.A.A.; Brumpton, B.M.; Mai, X.-M.; Vanfleteren, L.; Langhammer, A. The association of anxiety and depression with mortality in a COPD cohort. The HUNT study, Norway. Respir. Med. 2020, 171. [Google Scholar] [CrossRef]
- Weye, N.; Momen, N.C.; Christensen, M.K.; Iburg, K.M.; Dalsgaard, S.; Laursen, T.M.; Mortensen, P.B.; Santomauro, D.F.; Scott, J.G.; Whiteford, H.A.; et al. Association of Specific Mental Disorders With Premature Mortality in the Danish Population Using Alternative Measurement Methods. JAMA Netw. Open 2020, 3, e206646. [Google Scholar] [CrossRef]
- Kessler, R.C.; A Sampson, N.; Berglund, P.; Gruber, M.J.; Al-Hamzawi, A.; Andrade, L.; Bunting, B.; Demyttenaere, K.; Florescu, S.; De Girolamo, G.; et al. Anxious and non-anxious major depressive disorder in the World Health Organization World Mental Health Surveys. Epidemiol. Psychiatr. Sci. 2015, 24, 210–226. [Google Scholar] [CrossRef]
- Grant, B.F.; Hasin, D.S.; Stinson, F.S.; Dawson, D.A.; Ruan, W.J.; Goldstein, R.B.; Smith, S.M.; Saha, T.D.; Huang, B. Prevalence, correlates, co-morbidity, and comparative disability of DSM-IV generalized anxiety disorder in the USA: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol. Med. 2005, 35, 1747–1759. [Google Scholar] [CrossRef]
- Kessler, R.C.; Gruber, M.; Hettema, J.M.; Hwang, I.; Sampson, N.; Yonkers, K.A. Co-morbid major depression and generalized anxiety disorders in the National Comorbidity Survey follow-up. Psychol. Med. 2008, 38, 365–374. [Google Scholar] [CrossRef]
- Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corrà, U.; Cosyns, B.; Deaton, C.; Graham, I.; Stephen Hall, M.; et al. European Guidelines on Cardiovascular Disease Prevention in Clinical Practice. (The Netherlands) 6:1. 2016. Available online: http://www.escardio.org/guidelines (accessed on 4 September 2020).
- Karlsen, H.R.; Saksvik-Lehouillier, I.; Stone, K.L.; Schernhammer, E.; Yaffe, K.; Langvik, E. Anxiety as a risk factor for cardiovascular disease independent of depression: A prospective examination of community-dwelling men (the MrOS study). Psychol. Health 2020, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Todaro, J.F.; Shen, B.-J.; Raffa, S.D.; Tilkemeier, P.L.; Niaura, R. Prevalence of Anxiety Disorders in Men and Women With Established Coronary Heart Disease. J. Cardiopulm. Rehabil. Prev. 2007, 27, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Pogosova, N.; Kotseva, K.; De Bacquer, D.; Von Känel, R.; De Smedt, D.; Bruthans, J.; Dolzhenko, M. Psychosocial risk factors in relation to other cardiovascular risk factors in coronary heart disease: Results from the EUROASPIRE IV survey. A registry from the European Society of Cardiology. Eur. J. Prev. Cardiol. 2017, 24, 1371–1380. [Google Scholar] [CrossRef] [PubMed]
- Tully, P.J.; Cosh, S.M.; Baumeister, H. The anxious heart in whose mind? A systematic review and meta-regression of factors associated with anxiety disorder diagnosis, treatment and morbidity risk in coronary heart disease. J. Psychosom. Res. 2014, 77, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Smoller, J.W.; Pollack, M.H.; Wassertheil-Smoller, S.; Jackson, R.D.; Oberman, A.; Wong, N.D.; Sheps, D. Panic Attacks and Risk of Incident Cardiovascular Events Among Postmenopausal Women in the Women’s Health Initiative Observational Study. Arch. Gen. Psychiatry 2007, 64, 1153–1160. [Google Scholar] [CrossRef]
- Roest, A.M.; Martens, E.J.; Denollet, J.; De Jonge, P. Prognostic Association of Anxiety Post Myocardial Infarction With Mortality and New Cardiac Events: A Meta-Analysis. Psychosom. Med. 2010, 72, 563–569. [Google Scholar] [CrossRef]
- Li, J.; Ji, F.; Song, J.; Gao, X.; Jiang, D.; Chen, G.; Chen, S.; Lin, X.; Zhuo, C. Anxiety and clinical outcomes of patients with acute coronary syndrome: A meta-analysis. BMJ Open 2020, 10, e034135. [Google Scholar] [CrossRef]
- Volz, A.; Schmid, J.-P.; Zwahlen, M.; Kohls, S.; Saner, H.; Barth, J. Predictors of readmission and health related quality of life in patients with chronic heart failure: A comparison of different psychosocial aspects. J. Behav. Med. 2011, 34, 13–22. [Google Scholar] [CrossRef]
- Suzuki, T.; Shiga, T.; Kuwahara, K.; Kobayashi, S.; Suzuki, S.; Nishimura, K.; Suzuki, A.; Minami, Y.; Ishigooka, J.; Kasanuki, H.; et al. Impact of clustered depression and anxiety on mortality and rehospitalization in patients with heart failure. J. Cardiol. 2014, 64, 456–462. [Google Scholar] [CrossRef]
- Holwerda, S.W.; Luehrs, R.E.; Gremaud, A.L.; Wooldridge, N.A.; Stroud, A.K.; Fiedorowicz, J.G.; Abboud, F.M.; Pierce, G.L. Relative burst amplitude of muscle sympathetic nerve activity is an indicator of altered sympathetic outflow in chronic anxiety. J. Neurophysiol. 2018, 120, 11–22. [Google Scholar] [CrossRef]
- Wilson, M.A.; Liberzon, I.; Lindsey, M.L.; Lokshina, Y.; Risbrough, V.B.; Sah, R.; Wood, S.K.; Williamson, J.B.; Spinale, F.G. Common pathways and communication between the brain and heart: Connecting post-traumatic stress disorder and heart failure. Stress 2019, 22, 530–547. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, K.-I.; Shinba, T.; Yoshii, M. Psychiatric symptoms of noradrenergic dysfunction: A pathophysiological view. Psychiatry Clin. Neurosci. 2013, 68, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Zou, Z.; Zhou, B.; Huang, Y.; Wang, J.; Min, W.; Li, T. Differences in cytokines between patients with generalised anxiety disorder and panic disorder. J. Psychosom. Res. 2020, 133, 109975. [Google Scholar] [CrossRef] [PubMed]
- O’Donovan, A.; Hughes, B.M.; Slavich, G.M.; Lynch, L.; Cronin, M.-T.; O’Farrelly, C.; Malone, K.M. Clinical anxiety, cortisol and interleukin-6: Evidence for specificity in emotion–biology relationships. Brain, Behav. Immun. 2010, 24, 1074–1077. [Google Scholar] [CrossRef]
- Rasmussen, A.A.; Wiggers, H.; Jensen, M.; Berg, S.K.; Rasmussen, T.B.; Borregaard, B.; Thrysoee, L.; Thorup, C.B.; Mols, R.E.; Larsen, S.H.; et al. Patient-reported outcomes and medication adherence in patients with heart failure. Eur. Hear. J. Cardiovasc. Pharmacother. 2020. [Google Scholar] [CrossRef]
- Rao, A.; Zecchin, R.; Newton, P.J.; Phillips, J.L.; Digiacomo, M.; Denniss, A.R.; Hickman, L.D. The prevalence and impact of depression and anxiety in cardiac rehabilitation: A longitudinal cohort study. Eur. J. Prev. Cardiol. 2020, 27, 478–489. [Google Scholar] [CrossRef]
- Torii, H.; Ando, M.; Tomita, H.; Kobaru, T.; Tanaka, M.; Fujimoto, K.; Shimizu, R.; Ikesue, H.; Okusada, S.; Hashida, T.; et al. Association of Hypnotic Drug Use with Fall Incidents in Hospitalized Elderly Patients: A Case-Crossover Study. Biol. Pharm. Bull. 2020, 43, 925–931. [Google Scholar] [CrossRef]
- Hansen, R.N.; Boudreau, D.M.; Ebel, B.E.; Grossman, D.C.; Sullivan, S.D. Sedative Hypnotic Medication Use and the Risk of Motor Vehicle Crash. Am. J. Public Health 2015, 105, e64–e69. [Google Scholar] [CrossRef]
- Obiora, E.; Hubbard, R.; Sanders, R.D.; Myles, P.R. The impact of benzodiazepines on occurrence of pneumonia and mortality from pneumonia: A nested case-control and survival analysis in a population-based cohort. Thorax 2013, 68, 163–170. Available online: http://thorax.bmj.com/ (accessed on 8 September 2020). [CrossRef]
- Kripke, D.F. Mortality Risk of Hypnotics: Strengths and Limits of Evidence. Drug Saf. 2016, 39, 93–107. [Google Scholar] [CrossRef]
- Wu, C.-K.; Huang, Y.-T.; Lee, J.-K.; Juang, J.-M.J.; Tsai, C.-T.; Lai, L.-P.; Hwang, J.-J.; Chiang, F.-T.; Lin, J.-L.; Chen, P.-C.; et al. Anti-anxiety drugs use and cardiovascular outcomes in patients with myocardial infarction: A national wide assessment. Atherosclerosis 2014, 235, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Sato, Y.; Yoshihisa, A.; Hotsuki, Y.; Watanabe, K.; Kimishima, Y.; Kiko, T.; Kanno, Y.; Yokokawa, T.; Abe, S.; Misaka, T.; et al. Associations of Benzodiazepine with Adverse Prognosis in Heart Failure Patients With Insomnia. J. Am. Hear. Assoc. 2020, 9. [Google Scholar] [CrossRef] [PubMed]
- Maslej, M.M.; Bolker, B.M.; Russell, M.J.; Eaton, K.; Durisko, Z.; Hollon, S.D.; Swanson, G.M.; Thomson, J.A., Jr.; Mulsant, B.H.; Andrews, P.W. The Mortality and Myocardial Effects of Antidepressants Are Moderated by Preexisting Cardiovascular Disease: A Meta-Analysis. Psychother. Psychosom. 2017, 86, 268–282. Available online: https://www.karger.com/Article/FullText/477940 (accessed on 15 November 2020). [CrossRef] [PubMed]
- Angermann, C.E.; Gelbrich, G.; Störk, S.; Gunold, H.; Edelmann, F.; Wachter, R.; Schunkert, H.; Graf, T.; Kindermann, I.; Haass, M.; et al. Effect of escitalopram on 1–3all-Cause mortality and hospitalization in patients with heart failure and depression the mood-hf randomized clinical trial. JAMA J. Am. Med Assoc. 2016, 315, 2683–2693. Available online: https://pubmed.ncbi.nlm.nih.gov/27367876/ (accessed on 11 November 2020). [CrossRef] [PubMed]
- O’Connor, C.M.; Jiang, W.; Kuchibhatla, M.; Silva, S.G.; Cuffe, M.S.; Callwood, D.D.; Zakhary, B.; Stough, W.G.; Arias, R.M.; Rivelli, S.K.; et al. Safety and efficacy of sertraline for depression in patients with heart failure: Results of the SADHART-CHF (Sertraline against depression and heart disease in chronic heart failure) trial. J. Am. College Cardiol. 2010, 56, 692–699. Available online: https://pubmed.ncbi.nlm.nih.gov/20723799/ (accessed on 13 November 2020). [CrossRef] [PubMed]
- Fraguas, R.; Telles, R.M.D.S.; Alves, T.C.T.F.; Andrei, A.M.; Rays, J.; Iosifescu, D.V.; Wajngarten, M. A double-blind, placebo-controlled treatment trial of citalopram for major depressive disorder in older patients with heart failure: The relevance of the placebo effect and psychological symptoms. Contemp. Clin. Trials 2009, 30, 205–211. [Google Scholar] [CrossRef]
- He, W.; Zhou, Y.; Ma, J.; Wei, B.; Fu, Y. Effect of antidepressants on death in patients with heart failure: A systematic review and meta-analysis. Hear. Fail. Rev. 2019, 25, 1–8. [Google Scholar] [CrossRef]
- Brouwers, C.; Christensen, S.B.; Damen, N.L.; Denollet, J.; Madelaire, C.; Gislason, G.; Pedersen, S.S. Antidepressant use and risk for mortality in 121,252 heart failure patients with or without a diagnosis of clinical depression. Int. J. Cardiol. 2016, 203, 867–873. [Google Scholar] [CrossRef]
- Anon. FDA Drug Safety Communication: Abnormal Heart Rhythms Associated with High Doses of Celexa (Citalopram Hydrobromide) | FDA. Available online: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-abnormal-heart-rhythms-associated-high-doses-celexa-citalopram#data (accessed on 7 September 2020).
- Fernandes, N.; Prada, L.; Rosa, M.M.; Ferreira, J.J.; Costa, J.; Pinto, F.J.; Caldeira, D. The impact of SSRIs on mortality and cardiovascular events in patients with coronary artery disease and depression: Systematic review and meta-analysis. Clin. Res. Cardiol. 2020, 1–11. [Google Scholar] [CrossRef]
- Aronow, W.S.; A Shamliyan, T. Effects of antidepressants on QT interval in people with mental disorders. Arch. Med Sci. 2020, 16, 727–741. [Google Scholar] [CrossRef]
- Neutel, C.I.; Johansen, H. Benzodiazepines vs mortality-Causation or confounding? Sleep Med. 2019, 57, 151–152. [Google Scholar] [CrossRef] [PubMed]
- Walker, E.R.; Cummings, J.R.; Hockenberry, J.M.; Druss, B.G. Insurance Status, Use of Mental Health Services, and Unmet Need for Mental Health Care in the United States. Psychiatr. Serv. 2015, 66, 578–584. [Google Scholar] [CrossRef] [PubMed]
- Das, A.; Roy, B.; Schwarzer, G.; Silverman, M.G.; Ziegler, O.; Bandyopadhyay, D.; Philpotts, L.L.; Sinha, S.; Blumenthal, J.A.; Das, S. Comparison of treatment options for depression in heart failure: A network meta-analysis. J. Psychiatr. Res. 2019, 108, 7–23. [Google Scholar] [CrossRef] [PubMed]
| Variable | No. Anxiolytic (N = 5340) | Anxiolytics (N = 953) | p Value | No. Depression (N = 4605) | Depression (N = 1688) | p Value | Total (N = 6293) |
|---|---|---|---|---|---|---|---|
| Age (Years) | 75 (65–84) | 80 (69–87) | <0.001 | 74 (64–83) | 81 (72–88) | <0.001 | 76 (66–84) |
| Men | 2925 (55) | 416 (44) | <0.001) | 2664 (58) | 677 (40) | <0.001 | 3341 (53) |
| Social Status (living with spouse) | 2576 (49) | 380 (40) | <0.001 | 2371 (53) | 585 (35) | <0.001 | 2956 (48) |
| NYHA Class III/IV | 1465 (36) | 302 (44) | <0.001 | 1224 (34) | 543 (45) | <0.001 | 1767 (37) |
| HF Type | |||||||
| Reduced ejection fraction | 1493 (28%) | 250 (26%) | <0.001 | 1320 (29%) | 423 (25%) | <0.001 | 1743 (28%) |
| Preserved ejection fraction | 1992 (37%) | 401 (42%) | 1654 (36%) | 739 (44%) | 2393 (38%) | ||
| Not-specified | 1855 (35%) | 302 (32%) | 1631 (35%) | 526 (31%) | 2157 (34%) | ||
| Diabetes mellitus | 2852 (53) | 480 (50) | 0.08 | 2443 (53) | 889 (53) | 0.79 | 3332 (53) |
| Hypertension | 4326 (81) | 837 (88) | <0.001 | 3676 (80) | 1487 (88) | <0.001 | 5163 (82) |
| Hyperlipidemia | 4749 (89) | 866 (91) | 0.08 | 4075 (88) | 1540 (91) | 0.002 | 5615 (89) |
| Ischemic Heart Disease | 3495 (65) | 626 (66) | 0.89 | 3046 (66) | 1075 (64) | 0.07 | 4121 (65) |
| Prior Myocardial Infarction | 2256 (42) | 391 (41) | 0.48 | 1989 (43) | 658 (39) | 0.003 | 2647 (42) |
| Prior coronary bypass surgery | 101 (2) | 11 (1) | 0.11 | 90 (2) | 22 (1) | 0.08 | 112 (2) |
| Atrial fibrillation | 1935 (36) | 397 (42) | 0.001 | 1640 (36) | 692 (41) | <0.001 | 2332 (37) |
| Prior Stroke/transient ischemic attack | 1168 (22) | 247 (26) | 0.006 | 864 (19) | 551 (33) | <0.001 | 1415 (22) |
| Peripheral vascular disease | 716 (13) | 159 (17) | 0.007 | 570 (12) | 305 (18) | <0.001 | 875 (14) |
| Chronic obstructive lung disease | 1104 (21) | 229 (24) | 0.02 | 941 (20) | 392 (23) | 0.02 | 1333 (21) |
| Charlson Comorbidity Score | 6.0 (5.0–7.0) | 7.0 (5.0–8.0) | <0.001 | 6.0 (4.0–7.0) | 7.0 (5.0–8.0) | <0.001 | 6.0 (5.0–8.0) |
| Malignancy | 1060 (20) | 252 (26) | <0.001 | 900 (20) | 412 (24) | <0.001 | 1312 (21) |
| Dementia | 596 (11) | 199 (21) | <0.001 | 329 (7) | 466 (28) | <0.001 | 795 (13) |
| Dialysis | 256 (5) | 44 (5) | 0.81 | 231 (5) | 69 (4) | 0.13 | 300 (5) |
| Body mass index (kg/m2) | 29 (26–33) | 29 (25–33) | 0.06 | 29 (26–33) | 29 (25–33) | 0.07 | 29 (25–33) |
| Pulse (beats per minute) | 72 (65–80) | 72 (64–80) | 0.03 | 72 (64–80) | 72 (64–80) | 0.25 | 72 (64–80) |
| Systolic blood pressure (mmHg) | 128 (118–138) | 128 (117–139) | 0.65 | 128 (118–138) | 128 (116–139) | 0.72 | 128 (118–139) |
| Diastolic blood pressure (mmHg) | 72 (65–80) | 70 (63–79) | 0.21 | 72 (65–80) | 70 (63–80) | 0.14 | 72 (65–80) |
| Selected Laboratory Data | No. Anxiolytic (N = 5340) | Anxiolytics (N = 953) | p Value | No. Depression (N = 4605) | Depression (N = 1688) | p Value | Total (N = 6293) |
| Estimated glomerular filtration rate (mL/min per 1.73 m2) * | 71 (51–94) | 68 (48–88) | 0.001 | 73 (52–95) | 66 (48–88) | <0.001 | 71 (51–93) |
| Urea (mg/dL) | 44 (34–62) | 47 (34–64) | 0.05 | 44 (33–61) | 48 (35–66) | <0.001 | 45 (34–62) |
| Sodium (mEq/L) | 140 (138–142) | 140 (138–142) | 0.52 | 140 (138–142) | 140 (138–142) | 0.30 | 140 (138–142) |
| Potassium (mEql/L) | 13 (12–14) | 13 (11–14) | <0.001 | 13 (12–14) | 12 (11–14) | <0.001 | 13 (12–14) |
| Hemoglobin (g/dL) | 4.6 (4.3–4.9) | 4.6 (4.3–4.9) | 0.17 | 4.6 (4.3–5.0) | 4.6 (4.3–4.9) | 0.08 | 4.6 (4.3–4.9) |
| Red Cell Distribution Width (%) | 15 (14–16) | 15 (14–16) | <0.001 | 15 (14–16) | 15 (14–16) | <0.001 | 15 (14–16) |
| Glucose (mg/dL) | 107 (94–134) | 104 (93–126) | <0.001 | 108 (95-135) | 103 (92-129) | <0.001 | 106 (94-133) |
| Hemoglobin A1c (%) | 6.1 (5.6–7.2) | 6.0 (5.5–6.8) | <0.001 | 6.1 (5.6–7.2) | 6.0 (5.6–6.9) | <0.001 | 6.1 (5.6–7.1) |
| Uric Acid (mg/dL) | 6.2 (5.1–7.5) | 6.2 (5.0–7.5) | 0.33 | 6.2 (5.1–7.5) | 6.2 (5.1–7.5) | 0.61 | 6.2 (5.1–7.5) |
| TSH (mIU/L) | 2.2 (1.5–3.3) | 2.4 (1.5–3.6) | 0.02 | 2.2 (1.5–3.3) | 2.3 (1.5–3.4) | 0.52 | 2.2 (1.5–3.3) |
| Transferrin Saturation (%) | 17 (12–23) | 16 (12–22) | 0.17 | 17 (12–23) | 17 (12–23) | 0.44 | 17 (12–23) |
| Ferritin (ng/mL) | 81 (38–166) | 76 (36–163) | 0.53 | 81 (37–165) | 78 (39–169) | 0.68 | 80 (38–166) |
| Triglycerides (mg/dL) | 120 (89–170) | 122 (91–169) | 0.70 | 120 (88–170) | 122 (91–168) | 0.60 | 121 (89–169) |
| Low-density lipoprotein (mg/dL) | 82 (65–105) | 86 (65–108) | 0.13 | 82 (65–105) | 83 (66–108) | 0.75 | 83 (65–106) |
| Albumin (g/dL) | 4.0 (3.7–4.2) | 3.9 (3.6–4.1) | <0.001 | 4.0 (3.7–4.2) | 3.8 (3.5–4.1) | <0.001 | 3.9 (3.7–4.2) |
| C-Reactive Protein (mg/dL) | 0.6 (0.2–1.4) | 0.6 (0.2–1.8) | 0.15 | 0.5 (0.2–1.4) | 0.6 (0.2–1.6) | 0.20 | 0.6 (0.2–1.5) |
| Medication | No. Anxiolytic (N = 5340) | Anxiolytics (N = 953) | p Value | No. Depression (N = 4605) | Depression (N = 1688) | p Value | Total (N = 6293) |
| ACE-I/ARB/ARNI | 4156 (78) | 747 (78) | 0.7 | 3651 (79) | 1252 (74) | <0.001 | 4903 (78) |
| Beta blockers | 3967 (74) | 730 (77) | 0.13 | 3462 (75) | 1235 (73) | 0.1 | 4697 (75) |
| Spironolactone | 3421 (64) | 703 (74) | <0.001 | 2889 (63) | 1235 (73) | <0.001 | 4124 (66) |
| Furosemide | 1866 (35) | 370 (39) | 0.02 | 1614 (35) | 622 (37) | 0.19 | 2236 (36) |
| Thiazide | 752 (14) | 115 (12) | 0.1 | 641 (14) | 226 (13) | 0.59 | 867 (14) |
| Digoxin | 318 (6) | 65 (7) | 0.3 | 263 (6) | 120 (7) | 0.04 | 383 (6) |
| Amiodarone | 817 (15) | 169 (18) | 0.06 | 758 (16) | 228 (14) | 0.004 | 986 (16) |
| Aspirin | 153 (3) | 32 (3) | 0.41 | 129 (3) | 56 (3) | 0.28 | 185 (3) |
| New oral anticoagulants ** | 2991 (56) | 526 (55) | 0.64 | 2640 (57) | 877 (52) | <0.001 | 3517 (56) |
| Vitamin K antagonists | 223 (4) | 28 (3) | 0.07 | 199 (4) | 52 (3) | 0.03 | 251 (4) |
| Anti-Depressants | 816 (15) | 411 (43) | <0.001 | 0 | 1227 (73) | 1227 (19) | |
| Anxiolytics | 0 | 953 (100) | 445 (10) | 508 (30) | <0.001 | 953 (15) |
| Univariable | Multivariable | |||
|---|---|---|---|---|
| Hazard Ratio (95% CI) | p Value | Hazard Ratio (95% CI) | p Value | |
| Age (years) | 1.06 (1.05–1.07) | <0.001 | 1.04 (1.03–1.05) | <0.001 |
| Gender (Male) | 0.80 (0.70–0.92) | <0.001 | 1.26 (1.06–1.48) | 0.007 |
| NYHA III/IV | 1.99 (1.68–2.36) | <0.001 | 1.33 (1.11–1.60) | 0.002 |
| Diabetes Mellitus | 1.16 (1.01–1.33) | 0.003 | 1.19 (1.01–1.40) | 0.03 |
| Hypertension | 2.55 (1.99–3.26) | <0.001 | 1.24 (0.94–1.64) | 0.13 |
| Ischemic Heart Disease | 1.04 (0.90–1.20) | 0.33 | 0.87 (0.74–1.03) | 0.11 |
| Atrial Fibrillation | 1.80 (1.57–2.06) | <0.001 | 1.44 (1.24–1.68) | <0.001 |
| Body mass index * (kg/m2) | 0.13 (0.06–0.29) | <0.001 | 0.21 (0.08–0.51) | <0.001 |
| Urea (mg/dL) * | 9.18 (6.80–12.39) | <0.001 | 3.85 (2.17–6.85) | <0.001 |
| eGFR **(mL/min per 1.73 m2) | 0.84 (0.81–0.87) | <0.001 | 1.00 (0.94–1.07) | 0.95 |
| Sodium (mEq/L) | 0.95 (0.93–0.97) | <0.001 | 0.97 (0.95–0.99) | 0.007 |
| Hemoglobin (g/dL) | 0.79 (0.76–0.82) | <0.001 | 0.89 (0.85–0.93) | <0.001 |
| Treatment for Anxiety | 1.60 (1.36–1.89) | <0.001 | 1.23 (1.02–1.48) | 0.03 |
| Depression | 2.04 (1.78–2.34) | <0.001 | 1.49 (1.27–1.75) | <0.001 |
| Univariable | Multivariable | Multivariable and Drugs | ||||
|---|---|---|---|---|---|---|
| Hazard Ratio (95% CI) | p-Value | Hazard Ratio (95% CI) | p-Value | Hazard Ratio (95% CI) | p-Value | |
| Main Analysis | ||||||
| Death | ||||||
| Anxiolytics | 1.60 (1.36–1.89) | <0.001 | 1.23 (1.02–1.48) | 0.03 | 1.24 (1.03–1.50) | 0.02 |
| Depression | 2.04 (1.78–2.34) | <0.001 | 1.49 (1.27–1.75) | <0.001 | 1.46 (1.25–1.72) | <0.001 |
| Death and cardiovascular hospitalization | ||||||
| Anxiolytics | 1.28 (1.16–1.41) | <0.001 | 1.08 (0.97–1.20) | 0.17 | 1.05 (0.95–1.17) | 0.35 |
| Depression | 1.42 (1.32–1.54) | <0.001 | 1.20 (1.10–1.31) | <0.001 | 1.19 (1.09–1.30) | <0.001 |
| Additional Analysis | ||||||
| Death | ||||||
| None | 1.0 (Reference) | <0.001 | 1.0 (Reference) | <0.001 | 1.0 (Reference) | <0.001 |
| Anxiolytics (Alone) | 1.53 (1.18–1.98) 0.001 | 1.26 (0.95–1.67) 0.10 | 1.28 (0.97–1.70) 0.08 | |||
| Depression (Alone) | 2.05 (1.75–2.41) <0.001 | 1.51 (1.26–1.80) <0.001 | 1.48 (1.24–1.78) <0.001 | |||
| Depression and Anxiolytics | 2.36 (1.91–2.90) <0.001 | 1.81 (1.44–2.28) <0.001 | 1.80 (1.43–2.27) <0.001 | |||
| Death and cardiovascular hospitalization | ||||||
| None | 1.0 (Reference) | <0.001 | 1.0 (Reference) | <0.001 | 1.0 (Reference) | <0.001 |
| Anxiolytics (Alone) | 1.34 (1.17–1.53) <0.001 | 1.23 (1.06–1.41) 0.005 | 1.21 (1.04–1.39) 0.01 | |||
| Depression (Alone) | 1.47 (1.35–1.61) <0.001 | 1.27 (1.15–1.40) <0.001 | 1.26 (1.14–1.39) <0.001 | |||
| Depression and Anxiolytics | 1.46 (1.29–1.65) <0.001 | 1.20 (1.04–1.37) 0.01 | 1.15 (1.01–1.32) 0.04 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zwas, D.R.; Keren, A.; Amir, O.; Gotsman, I. Treatment of Heart Failure Patients with Anxiolytics Is Associated with Adverse Outcomes, with and without Depression. J. Clin. Med. 2020, 9, 3967. https://doi.org/10.3390/jcm9123967
Zwas DR, Keren A, Amir O, Gotsman I. Treatment of Heart Failure Patients with Anxiolytics Is Associated with Adverse Outcomes, with and without Depression. Journal of Clinical Medicine. 2020; 9(12):3967. https://doi.org/10.3390/jcm9123967
Chicago/Turabian StyleZwas, Donna R., Andre Keren, Offer Amir, and Israel Gotsman. 2020. "Treatment of Heart Failure Patients with Anxiolytics Is Associated with Adverse Outcomes, with and without Depression" Journal of Clinical Medicine 9, no. 12: 3967. https://doi.org/10.3390/jcm9123967
APA StyleZwas, D. R., Keren, A., Amir, O., & Gotsman, I. (2020). Treatment of Heart Failure Patients with Anxiolytics Is Associated with Adverse Outcomes, with and without Depression. Journal of Clinical Medicine, 9(12), 3967. https://doi.org/10.3390/jcm9123967





