Prognostic Value of Different CMR-Based Techniques to Assess Left Ventricular Myocardial Strain in Takotsubo Syndrome
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. CMR Image Acquisition and Analysis
2.3. CMR-Based Strain Analysis
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics and Routine CMR Findings
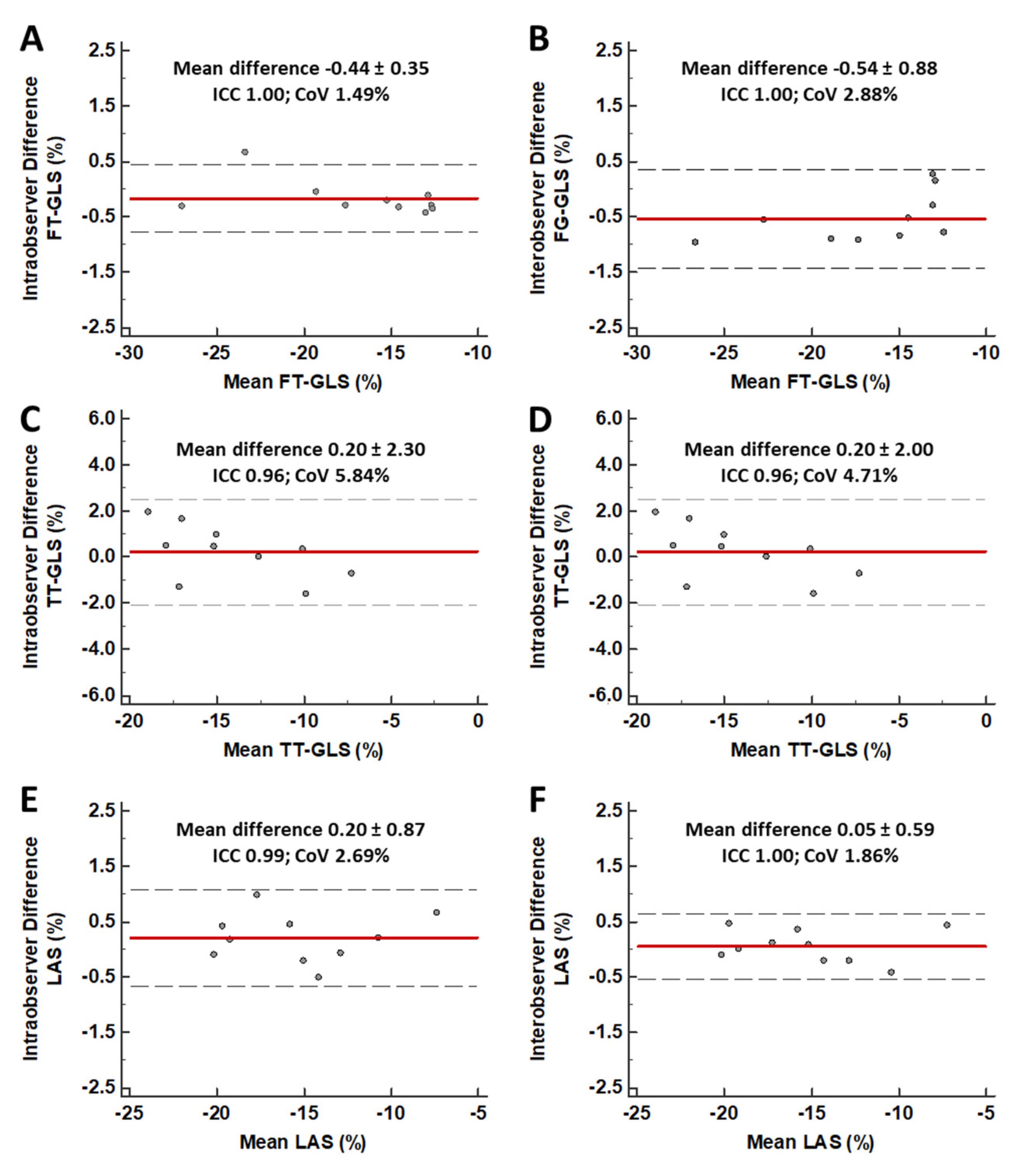
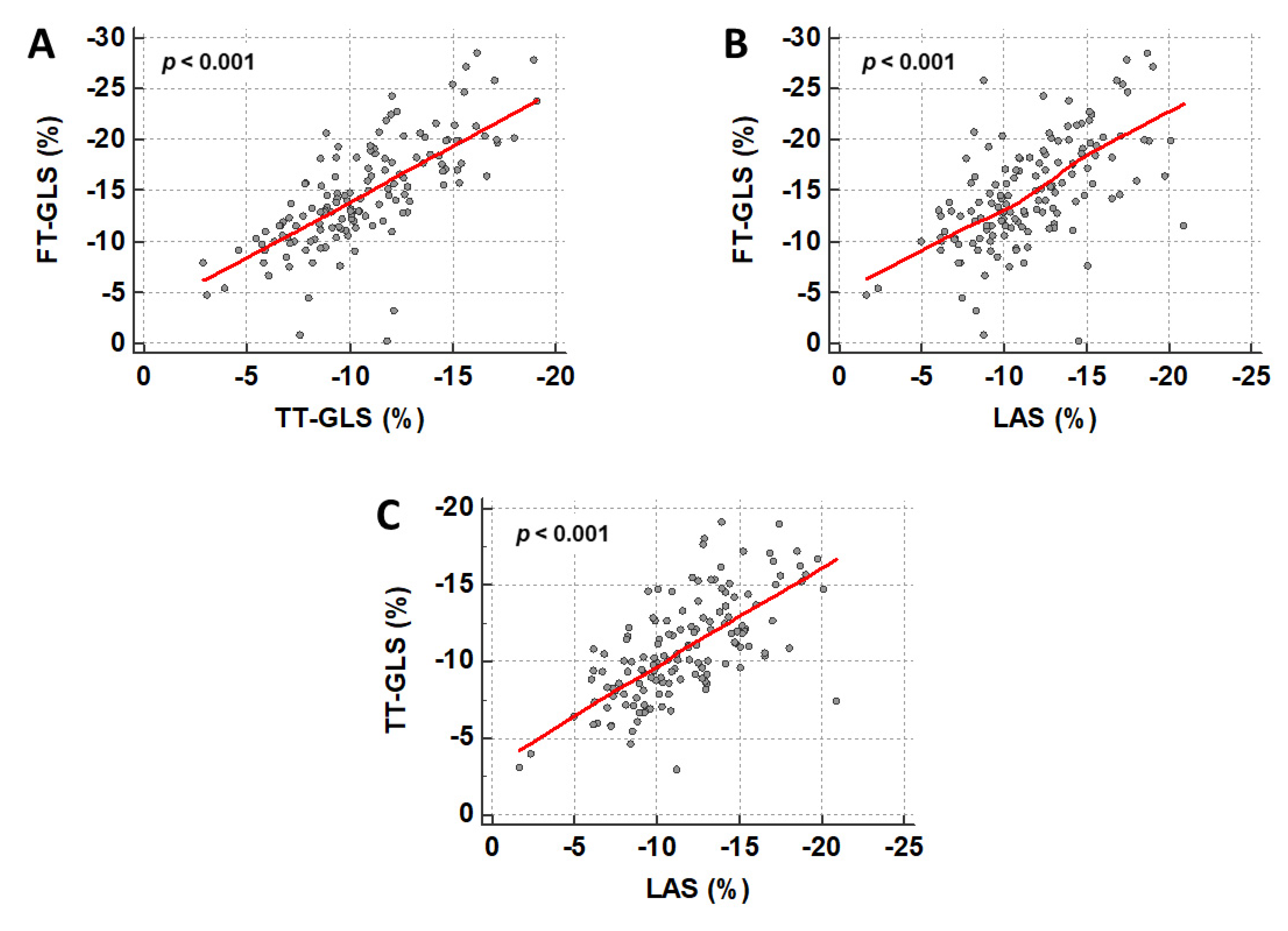
3.2. CMR-Bases Strain Analysis
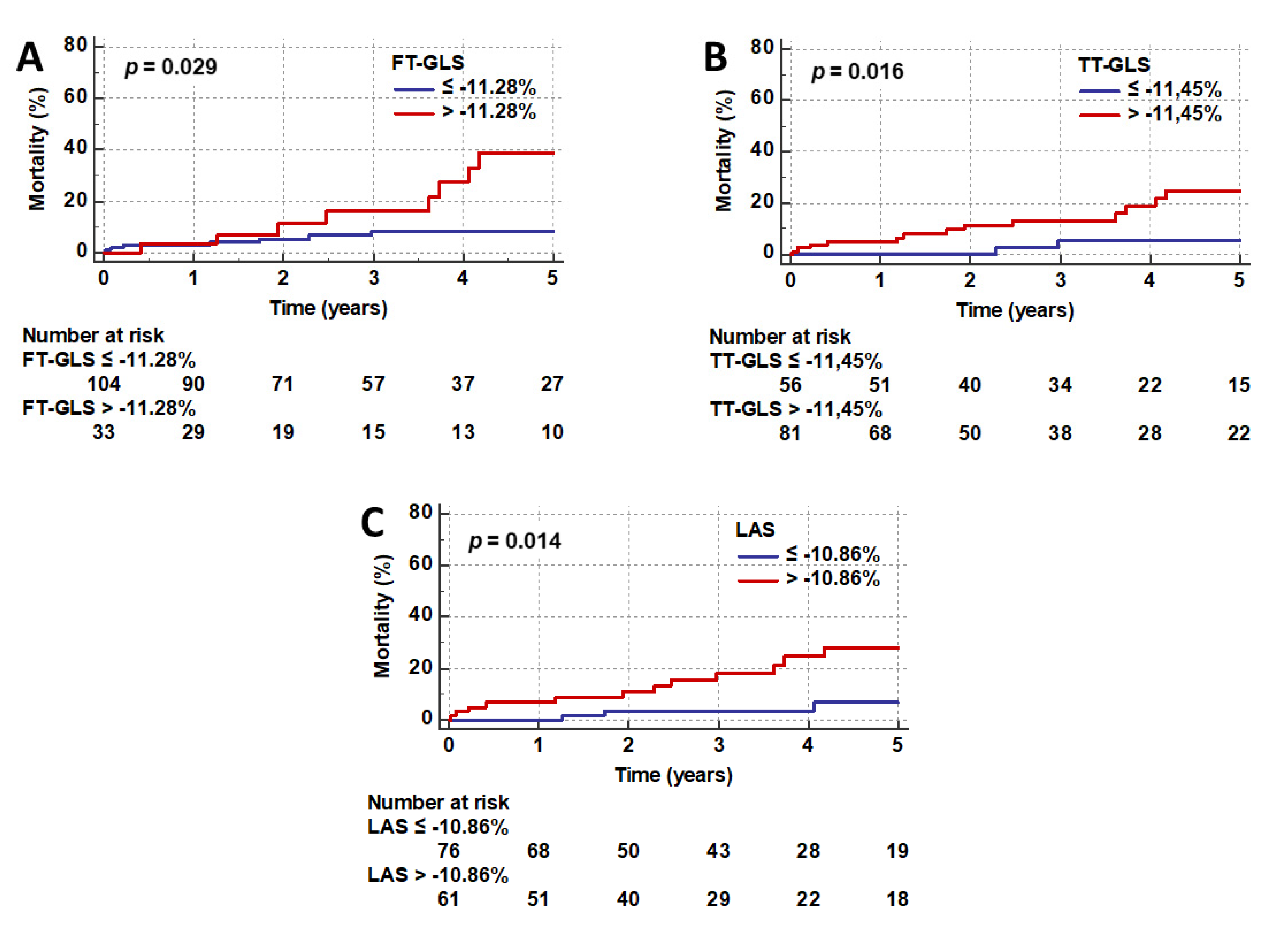
3.3. Prognostic Value of CMR-Based Strain Values
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
References
- Lyon, A.R.; Bossone, E.; Schneider, B.; Sechtem, U.; Citro, R.; Underwood, S.R.; Sheppard, M.N.; Figtree, G.A.; Parodi, G.; Akashi, Y.J.; et al. Current state of knowledge on Takotsubo syndrome: A Position Statement from the Taskforce on Takotsubo Syndrome of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2016, 18, 8–27. [Google Scholar] [CrossRef] [PubMed]
- Stiermaier, T.; Jobs, A.; de Waha, S.; Fuernau, G.; Poss, J.; Desch, S.; Thiele, H.; Eitel, I. Optimized Prognosis Assessment in ST-Segment-Elevation Myocardial Infarction Using a Cardiac Magnetic Resonance Imaging Risk Score. Circ. Cardiovasc. Imaging 2017, 10, e006774. [Google Scholar] [CrossRef] [PubMed]
- Stiermaier, T.; Moeller, C.; Oehler, K.; Desch, S.; Graf, T.; Eitel, C.; Vonthein, R.; Schuler, G.; Thiele, H.; Eitel, I. Long-term excess mortality in takotsubo cardiomyopathy: Predictors, causes and clinical consequences. Eur. J. Heart Fail. 2016, 18, 650–656. [Google Scholar] [CrossRef] [PubMed]
- Stiermaier, T.; Moller, C.; Graf, T.; Eitel, C.; Desch, S.; Thiele, H.; Eitel, I. Prognostic Usefulness of the Ballooning Pattern in Patients With Takotsubo Cardiomyopathy. Am. J. Cardiol. 2016, 118, 1737–1741. [Google Scholar] [CrossRef] [PubMed]
- Eitel, I.; von Knobelsdorff-Brenkenhoff, F.; Bernhardt, P.; Carbone, I.; Muellerleile, K.; Aldrovandi, A.; Francone, M.; Desch, S.; Gutberlet, M.; Strohm, O.; et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (takotsubo) cardiomyopathy. JAMA 2011, 306, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Eitel, I.; Stiermaier, T.; Lange, T.; Rommel, K.P.; Koschalka, A.; Kowallick, J.T.; Lotz, J.; Kutty, S.; Gutberlet, M.; Hasenfuss, G.; et al. Cardiac Magnetic Resonance Myocardial Feature Tracking for Optimized Prediction of Cardiovascular Events Following Myocardial Infarction. JACC Cardiovasc. Imaging 2018, 11, 1433–1444. [Google Scholar] [CrossRef]
- Buss, S.J.; Breuninger, K.; Lehrke, S.; Voss, A.; Galuschky, C.; Lossnitzer, D.; Andre, F.; Ehlermann, P.; Franke, J.; Taeger, T.; et al. Assessment of myocardial deformation with cardiac magnetic resonance strain imaging improves risk stratification in patients with dilated cardiomyopathy. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 307–315. [Google Scholar] [CrossRef]
- Fischer, K.; Obrist, S.J.; Erne, S.A.; Stark, A.W.; Marggraf, M.; Kaneko, K.; Guensch, D.P.; Huber, A.T.; Greulich, S.; Aghayev, A.; et al. Feature Tracking Myocardial Strain Incrementally Improves Prognostication in Myocarditis Beyond Traditional CMR Imaging Features. JACC Cardiovasc. Imaging 2020, 13, 1891–1901. [Google Scholar] [CrossRef]
- Backhaus, S.J.; Kowallick, J.T.; Stiermaier, T.; Lange, T.; Koschalka, A.; Navarra, J.L.; Lotz, J.; Kutty, S.; Bigalke, B.; Gutberlet, M.; et al. Culprit vessel-related myocardial mechanics and prognostic implications following acute myocardial infarction. Clin. Res. Cardiol. 2020, 109, 339–349. [Google Scholar] [CrossRef]
- Liu, T.; Gao, Y.; Wang, H.; Zhou, Z.; Wang, R.; Chang, S.; Liu, Y.; Sun, Y.; Rui, H.; Yang, G.; et al. Association between right ventricular strain and outcomes in patients with dilated cardiomyopathy. Heart 2020. [Google Scholar] [CrossRef]
- Secchi, F.; Monti, C.B.; Ali, M.; Carbone, F.S.; Cannao, P.M.; Sardanelli, F. Diagnostic Value of Global Cardiac Strain in Patients With Myocarditis. J. Comput. Assist. Tomogr. 2020, 44, 591–598. [Google Scholar] [CrossRef] [PubMed]
- Scally, C.; Rudd, A.; Mezincescu, A.; Wilson, H.; Srivanasan, J.; Horgan, G.; Broadhurst, P.; Newby, D.E.; Henning, A.; Dawson, D.K. Persistent Long-Term Structural, Functional, and Metabolic Changes After Stress-Induced (Takotsubo) Cardiomyopathy. Circulation 2018, 137, 1039–1048. [Google Scholar] [CrossRef] [PubMed]
- Schuster, A.; Backhaus, S.J.; Stiermaier, T.; Kowallick, J.T.; Stulle, A.; Koschalka, A.; Lotz, J.; Kutty, S.; Bigalke, B.; Gutberlet, M.; et al. Fast manual long-axis strain assessment provides optimized cardiovascular event prediction following myocardial infarction. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 1262–1270. [Google Scholar] [CrossRef] [PubMed]
- Gavara, J.; Rodriguez-Palomares, J.F.; Valente, F.; Monmeneu, J.V.; Lopez-Lereu, M.P.; Bonanad, C.; Ferreira-Gonzalez, I.; Garcia Del Blanco, B.; Rodriguez-Garcia, J.; Mutuberria, M.; et al. Prognostic Value of Strain by Tissue Tracking Cardiac Magnetic Resonance After ST-Segment Elevation Myocardial Infarction. JACC Cardiovasc. Imaging 2018, 11, 1448–1457. [Google Scholar] [CrossRef]
- Stiermaier, T.; Lange, T.; Chiribiri, A.; Moller, C.; Graf, T.; Villnow, C.; Raaz, U.; Villa, A.; Kowallick, J.T.; Lotz, J.; et al. Left ventricular myocardial deformation in Takotsubo syndrome: A cardiovascular magnetic resonance myocardial feature tracking study. Eur. Radiol. 2018, 28, 5160–5170. [Google Scholar] [CrossRef]
- Prasad, A.; Lerman, A.; Rihal, C.S. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): A mimic of acute myocardial infarction. Am. Heart J. 2008, 155, 408–417. [Google Scholar] [CrossRef]
- Citro, R.; Okura, H.; Ghadri, J.R.; Izumi, C.; Meimoun, P.; Izumo, M.; Dawson, D.; Kaji, S.; Eitel, I.; Kagiyama, N.; et al. Multimodality imaging in takotsubo syndrome: A joint consensus document of the European Association of Cardiovascular Imaging (EACVI) and the Japanese Society of Echocardiography (JSE). Eur. Heart J. Cardiovasc. Imaging 2020, 21, 1184–1207. [Google Scholar] [CrossRef]
- Gertz, R.J.; Lange, T.; Kowallick, J.T.; Backhaus, S.J.; Steinmetz, M.; Staab, W.; Kutty, S.; Hasenfuss, G.; Lotz, J.; Schuster, A. Inter-vendor reproducibility of left and right ventricular cardiovascular magnetic resonance myocardial feature-tracking. PLoS ONE 2018, 13, e0193746. [Google Scholar]
- Riffel, J.H.; Andre, F.; Maertens, M.; Rost, F.; Keller, M.G.; Giusca, S.; Seitz, S.; Kristen, A.V.; Muller, M.; Giannitsis, E.; et al. Fast assessment of long axis strain with standard cardiovascular magnetic resonance: A validation study of a novel parameter with reference values. J. Cardiovasc. Magn. Reson. 2015, 17, 69. [Google Scholar] [CrossRef]
- Santoro, F.; Nunez Gil, I.J.; Stiermaier, T.; El-Battrawy, I.; Guerra, F.; Novo, G.; Guastafierro, F.; Tarantino, N.; Novo, S.; Mariano, E.; et al. Assessment of the German and Italian Stress Cardiomyopathy Score for Risk Stratification for In-hospital Complications in Patients With Takotsubo Syndrome. JAMA Cardiol. 2019, 4, 892–899. [Google Scholar] [CrossRef]
- Redfors, B.; Vedad, R.; Angeras, O.; Ramunddal, T.; Petursson, P.; Haraldsson, I.; Ali, A.; Dworeck, C.; Odenstedt, J.; Ioaness, D.; et al. Mortality in takotsubo syndrome is similar to mortality in myocardial infarction—A report from the SWEDEHEART registry. Int. J. Cardiol. 2015, 185, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Stiermaier, T.; Eitel, C.; Desch, S.; Fuernau, G.; Schuler, G.; Thiele, H.; Eitel, I. Incidence, determinants and prognostic relevance of cardiogenic shock in patients with Takotsubo cardiomyopathy. Eur. Heart J. Acute Cardiovasc. Care 2016, 5, 489–496. [Google Scholar] [CrossRef] [PubMed]
- Almendro-Delia, M.; Nunez-Gil, I.J.; Lobo, M.; Andres, M.; Vedia, O.; Sionis, A.; Martin-Garcia, A.; Cruz Aguilera, M.; Pereyra, E.; Martin de Miguel, I.; et al. Short- and Long-Term Prognostic Relevance of Cardiogenic Shock in Takotsubo Syndrome: Results From the RETAKO Registry. JACC Heart Fail. 2018, 6, 928–936. [Google Scholar] [CrossRef] [PubMed]
- Schuster, A.; Hor, K.N.; Kowallick, J.T.; Beerbaum, P.; Kutty, S. Cardiovascular Magnetic Resonance Myocardial Feature Tracking: Concepts and Clinical Applications. Circ. Cardiovasc. Imaging 2016, 9, e004077. [Google Scholar] [CrossRef] [PubMed]
- Nazir, S.A.; Shetye, A.M.; Khan, J.N.; Singh, A.; Arnold, J.R.; Squire, I.; McCann, G.P. Inter-study repeatability of circumferential strain and diastolic strain rate by CMR tagging, feature tracking and tissue tracking in ST-segment elevation myocardial infarction. Int. J. Cardiovasc. Imaging 2020, 36, 1133–1146. [Google Scholar] [CrossRef]
- Bistoquet, A.; Oshinski, J.; Skrinjar, O. Left ventricular deformation recovery from cine MRI using an incompressible model. IEEE Trans. Med. Imaging 2007, 26, 1136–1153. [Google Scholar] [CrossRef]
- Morton, G.; Schuster, A.; Jogiya, R.; Kutty, S.; Beerbaum, P.; Nagel, E. Inter-study reproducibility of cardiovascular magnetic resonance myocardial feature tracking. J. Cardiovasc. Magn. Reson. 2012, 14, 43. [Google Scholar] [CrossRef]
- Brunetti, N.D.; Tarantino, N.; Guastafierro, F.; De Gennaro, L.; Correale, M.; Stiermaier, T.; Moller, C.; Di Biase, M.; Eitel, I.; Santoro, F. Malignancies and outcome in Takotsubo syndrome: A meta-analysis study on cancer and stress cardiomyopathy. Heart Fail. Rev. 2019, 24, 481–488. [Google Scholar] [CrossRef]
- Moller, C.; Stiermaier, T.; Graf, T.; Eitel, C.; Thiele, H.; Burgdorf, C.; Eitel, I. Prevalence and long-term prognostic impact of malignancy in patients with Takotsubo syndrome. Eur. J. Heart Fail. 2018, 20, 816–818. [Google Scholar] [CrossRef]
- Stiermaier, T.; Santoro, F.; Eitel, C.; Graf, T.; Moller, C.; Tarantino, N.; Guastafierro, F.; Di Biase, M.; Thiele, H.; Brunetti, N.D.; et al. Prevalence and prognostic relevance of atrial fibrillation in patients with Takotsubo syndrome. Int. J. Cardiol. 2017, 245, 156–161. [Google Scholar] [CrossRef]
- Stiermaier, T.; Santoro, F.; El-Battrawy, I.; Moller, C.; Graf, T.; Novo, G.; Santangelo, A.; Mariano, E.; Romeo, F.; Caldarola, P.; et al. Prevalence and Prognostic Impact of Diabetes in Takotsubo Syndrome: Insights From the International, Multicenter GEIST Registry. Diabetes Care 2018, 41, 1084–1088. [Google Scholar] [CrossRef] [PubMed]
- Nunez-Gil, I.J.; Almendro-Delia, M.; Andres, M.; Sionis, A.; Martin, A.; Bastante, T.; Cordoba-Soriano, J.G.; Linares, J.A.; Gonzalez Sucarrats, S.; Sanchez-Grande-Flecha, A.; et al. Secondary forms of Takotsubo cardiomyopathy: A whole different prognosis. Eur. Heart J. Acute Cardiovasc. Care 2016, 5, 308–316. [Google Scholar] [CrossRef] [PubMed]
- Stiermaier, T.; Eitel, C.; Denef, S.; Desch, S.; Schuler, G.; Thiele, H.; Eitel, I. Prevalence and Clinical Significance of Life-Threatening Arrhythmias in Takotsubo Cardiomyopathy. J. Am. Coll. Cardiol. 2015, 65, 2148–2150. [Google Scholar] [CrossRef] [PubMed]
- El-Battrawy, I.; Santoro, F.; Stiermaier, T.; Moller, C.; Guastafierro, F.; Novo, G.; Novo, S.; Mariano, E.; Romeo, F.; Romeo, F.; et al. Incidence and Clinical Impact of Recurrent Takotsubo Syndrome: Results From the GEIST Registry. J. Am. Heart Assoc. 2019, 8, e010753. [Google Scholar] [CrossRef] [PubMed]
- Backhaus, S.J.; Lange, T.; Beuthner, B.E.; Topci, R.; Wang, X.; Kowallick, J.T.; Lotz, J.; Seidler, T.; Toischer, K.; Zeisberg, E.M.; et al. Real-time cardiovascular magnetic resonance T1 and extracellular volume fraction mapping for tissue characterisation in aortic stenosis. J. Cardiovasc. Magn. Reson. 2020, 22, 46. [Google Scholar] [CrossRef]
- Backhaus, S.J.; Metschies, G.; Zieschang, V.; Erley, J.; Zamani, S.M.; Kowallick, J.T.; Lapinskas, T.; Pieske, B.; Lotz, J.; Kutty, S.; et al. Head-to-head comparison of cardiovascular MR feature tracking cine versus acquisition-based deformation strain imaging using myocardial tagging and strain encoding. Magn. Reson. Med. 2020. [Google Scholar] [CrossRef]

| Variable | All Patients (n = 147) | Survivors (n = 119) | Non-Survivors (n = 19) | p |
|---|---|---|---|---|
| Age (years) | 72 (61, 78) | 71 (61, 77) | 77 (72, 82) | 0.006 |
| Male sex | 13/147 (8.8) | 8/119 (6.7) | 4/19 (21.1) | 0.040 |
| Hypertension | 122/147 (83.0) | 97/119 (81.5) | 17/19 (89.5) | 0.395 |
| Diabetes mellitus | 33/147 (22.4) | 20/119 (16.8) | 8/19 (42.1) | 0.011 |
| Hypercholesterolemia | 31/147 (21.1) | 26/119 (21.8) | 5/19 (26.3) | 0.665 |
| Current smoking | 28/147 (19.0) | 23/119 (19.3) | 3/19 (15.8) | 0.714 |
| Body mass index (kg/m2) | 25 (22, 29) | 25 (22, 29) | 24 (21, 27) | 0.440 |
| Atrial fibrillation | 24/147 (16.3) | 14/119 (11.8) | 6/19 (31.6) | 0.023 |
| Malignancy | 27/147 (18.4) | 17/119 (14.3) | 8/19 (42.1) | 0.003 |
| Killip-class on admission | 0.519 | |||
| 1 | 114/147 (7.6) | 95/119 (79.8) | 14/19 (73.7) | |
| 2 | 25/147 (17.0) | 18/119 (15.1) | 5/19 (26.3) | |
| 3 | 2/147 (1.4) | 1/119 (0.8) | - | |
| 4 | 6/147 (4.1) | 5/119 (4.2) | - | |
| Days of hospitalization | 5 (3, 7) | 5 (3, 7) | 4 (3, 7) | 0.566 |
| Stressful event | 97/147 (66.0) | 75/119 (63.0) | 16/19 (84.2) | 0.070 |
| Physical trigger | 60/147 (40.8) | 42/119 (35.3) | 14/19 (73.7) | 0.002 |
| Emotional trigger | 37/147 (25.2) | 33/119 (27.7) | 2/19 (10.5) | 0.109 |
| ST-segment elevation | 50/142 (35.2) | 36/115 (31.3) | 9/19 (47.4) | 0.170 |
| Ballooning pattern | 0.165 | |||
| Apical | 96/147 (65.3) | 74/119 (62.2) | 16/19 (84.2) | |
| Midventricular | 48/147 (32.7) | 42/119 (35.3) | 3/19 (15.8) | |
| Basal | 3/147 (2.0) | 3/119 (2.5) | - | |
| Initial LV-EF * (%) | 47 (41, 53) | 48 (41, 53) | 47 (40, 49) | 0.570 |
| Follow-up LV-EF * (%) | 60 (55, 66) | 60 (55, 65) | 58 (50, 69) | 0.394 |
| Discharge medication | ||||
| Aspirin | 64/146 (43.8) | 52/119 (43.7) | 7/18 (38.9) | 0.701 |
| Clopidogrel | 16/146 (11.0) | 14/119 (11.8) | 1/18 (5.6) | 0.432 |
| Oral anticoagulation | 19/146 (13.0) | 12/119 (10.1) | 5/18 (27.8) | 0.034 |
| Beta blocker | 141/146 (96.6) | 115/119 (96.6) | 17/18 (94.4) | 0.644 |
| ACE inhibitor/AT-R blocker | 141/146 (96.6) | 114/119 (95.8) | 18/18 (100) | 0.376 |
| Aldosterone antagonist | 32/146 (21.9) | 27/119 (22.7) | 3/18 (16.7) | 0.565 |
| Diuretic | 80/146 (54.8) | 60/119 (50.4) | 14/18 (77.8) | 0.030 |
| Statin | 57/146 (39.0) | 46/119 (38.7) | 7/18 (38.9) | 0.985 |
| Variable | All Patients (n = 147) | Survivors (n = 119) | Non-Survivors (n = 19) | p |
|---|---|---|---|---|
| LV ejection fraction (%) | 48 (40, 53) | 48 (40, 53) | 47 (40, 50) | 0.678 |
| LVEDV (mL) | 132 (114, 153) | 131 (113, 151) | 140 (121, 160) | 0.200 |
| LVESV (mL) | 68 (55, 82) | 68 (53, 81) | 72 (60, 82) | 0.403 |
| FT-GLS (%) | −14.2 (−11.3, −18.2) | −14.5 (−11.5, −18.8) | −12.6 (−9.2, −16.4) | 0.097 |
| TT-GLS (%) | −10.4 (−8.6, −12.8) | −10.9 (−8.8, −13.3) | −8.9 (−7.6, −11.3) | 0.032 |
| LAS (%) | −11.2 (−9.1, −14.2) | −12.0 (−9.5, −14.5) | −10.2 (−7.7, −12.8) | 0.014 |
| Myocardial edema * | 101/125 (80.8) | 82/99 (82.8) | 12/18 (66.7) | 0.112 |
| LGE | - | - | - | |
| LV thrombus | 3/147 (2.0) | 2/119 (1.7) | 1/19 (5.3) | 0.320 |
| Pericardial effusion | 48/147 (32.7) | 37/119 (31.1) | 7/19 (36.8) | 0.618 |
| Pleural effusion | 63/147 (42.9) | 49/119 (41.2) | 11/19 (57.9) | 0.172 |
| RV involvement | 41/147 (27.9) | 30/119 (25.2) | 8/19 (42.1) | 0.126 |
| Variable | Univariate | Stepwise Multivariable | ||
|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | |
| Age (years) | 1.07 (1.02–1.12) | 0.010 | - | - |
| Male sex | 4.27 (1.36–13.48) | 0.013 | - | - |
| Diabetes mellitus | 3.06 (1.22–7.68) | 0.018 | 6.15 (2.18–17.32) | 0.001 |
| Atrial fibrillation | 3.21 (1.20–8.55) | 0.020 | 7.65 (2.21–26.51) | 0.001 |
| Malignancy | 3.17 (1.27–7.92) | 0.013 | 4.32 (1.53–12.19) | 0.006 |
| Physical trigger | 3.89 (1.40–10.80) | 0.009 | 4.77 (1.58–14.39) | 0.006 |
| Pleural effusion | 2.80 (1.07–7.32) | 0.035 | - | - |
| FT-GLS (%) | 1.10 (1.00–1.20) | 0.041 | - | - |
| TT-GLS (%) | 1.18 (1.02–1.37) | 0.026 | - | - |
| LAS (%) | 1.19 (1.03–1.36) | 0.015 | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stiermaier, T.; Busch, K.; Lange, T.; Pätz, T.; Meusel, M.; Backhaus, S.J.; Frydrychowicz, A.; Barkhausen, J.; Gutberlet, M.; Thiele, H.; et al. Prognostic Value of Different CMR-Based Techniques to Assess Left Ventricular Myocardial Strain in Takotsubo Syndrome. J. Clin. Med. 2020, 9, 3882. https://doi.org/10.3390/jcm9123882
Stiermaier T, Busch K, Lange T, Pätz T, Meusel M, Backhaus SJ, Frydrychowicz A, Barkhausen J, Gutberlet M, Thiele H, et al. Prognostic Value of Different CMR-Based Techniques to Assess Left Ventricular Myocardial Strain in Takotsubo Syndrome. Journal of Clinical Medicine. 2020; 9(12):3882. https://doi.org/10.3390/jcm9123882
Chicago/Turabian StyleStiermaier, Thomas, Kira Busch, Torben Lange, Toni Pätz, Moritz Meusel, Sören J. Backhaus, Alex Frydrychowicz, Jörg Barkhausen, Matthias Gutberlet, Holger Thiele, and et al. 2020. "Prognostic Value of Different CMR-Based Techniques to Assess Left Ventricular Myocardial Strain in Takotsubo Syndrome" Journal of Clinical Medicine 9, no. 12: 3882. https://doi.org/10.3390/jcm9123882
APA StyleStiermaier, T., Busch, K., Lange, T., Pätz, T., Meusel, M., Backhaus, S. J., Frydrychowicz, A., Barkhausen, J., Gutberlet, M., Thiele, H., Schuster, A., & Eitel, I. (2020). Prognostic Value of Different CMR-Based Techniques to Assess Left Ventricular Myocardial Strain in Takotsubo Syndrome. Journal of Clinical Medicine, 9(12), 3882. https://doi.org/10.3390/jcm9123882






