Effect of Gender, Age, and Ocular and Growth-Related Factors on Corneal Epithelial and Stromal Thickness in Children
Abstract
1. Introduction
2. Materials and Methods
3. Results
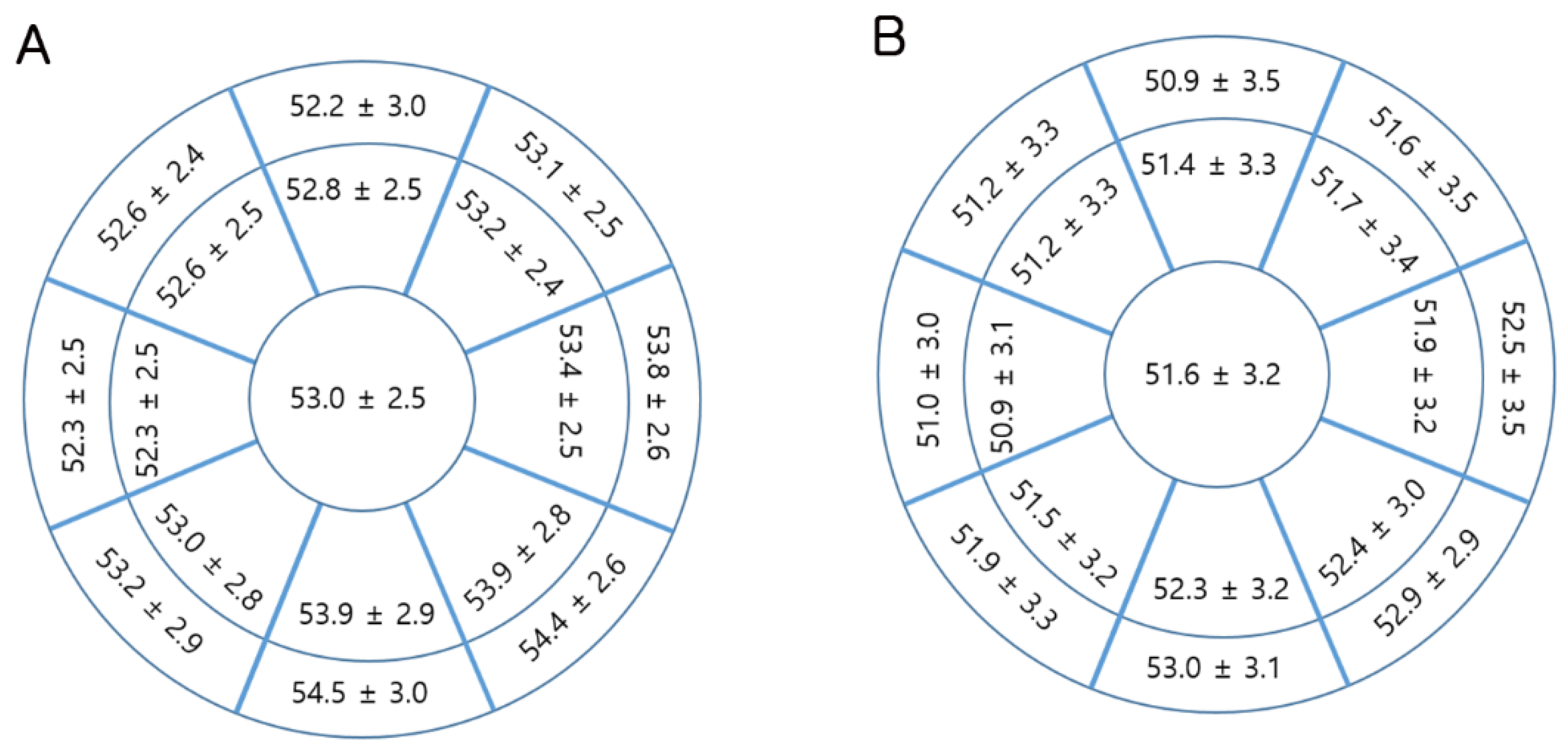
3.1. Corneal Epithelial and Stromal Thickness Profiles
3.2. Association between Ocular Measurements
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| FD-OCT | Fourier-domain optical coherence tomography |
| CCT | central corneal thickness |
| WTW | white to white corneal diameter |
| Mean K | mean keratometric value, mean corneal power |
| ACD | anterior chamber depth |
| SEQ | spherical equivalent refraction |
References
- Gromacki, S.J.; Barr, J.T. Central and peripheral corneal thickness in keratoconus and normal patient groups. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom. 1994, 71, 437–441. [Google Scholar] [CrossRef]
- Day, A.C.; Machin, D.; Aung, T.; Gazzard, G.; Husain, R.; Chew, P.T.; Khaw, P.T.; Seah, S.K.; Foster, P.J. Central corneal thickness and glaucoma in East Asian people. Investig. Ophthalmol. Vis. Sci. 2011, 52, 8407–8412. [Google Scholar] [CrossRef]
- Grewal, D.S.; Brar, G.S.; Grewal, S.P. Assessment of central corneal thickness in normal, keratoconus, and post-laser in situ keratomileusis eyes using Scheimpflug imaging, spectral domain optical coherence tomography, and ultrasound pachymetry. J. Cataract Refract. Surg. 2010, 36, 954–964. [Google Scholar] [CrossRef]
- Shah, H.; Kniestedt, C.; Bostrom, A.; Stamper, R.; Lin, S. Role of central corneal thickness on baseline parameters and progression of visual fields in open angle glaucoma. Eur. J. Ophthalmol. 2007, 17, 545–549. [Google Scholar] [CrossRef]
- Kanellopoulos, A.J.; Asimellis, G. In vivo three-dimensional corneal epithelium imaging in normal eyes by anterior-segment optical coherence tomography: A clinical reference study. Cornea 2013, 32, 1493–1498. [Google Scholar] [CrossRef]
- Ma, X.J.; Wang, L.; Koch, D.D. Repeatability of corneal epithelial thickness measurements using Fourier-domain optical coherence tomography in normal and post-LASIK eyes. Cornea 2013, 32, 1544–1548. [Google Scholar] [CrossRef] [PubMed]
- Ryu, I.H.; Kim, B.J.; Lee, J.H.; Kim, S.W. Comparison of Corneal Epithelial Remodeling After Femtosecond Laser-Assisted LASIK and Small Incision Lenticule Extraction (SMILE). J. Refract. Surg. 2017, 33, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Reinstein, D.Z.; Archer, T.J.; Gobbe, M. Corneal epithelial thickness profile in the diagnosis of keratoconus. J. Refract. Surg. 2009, 25, 604–610. [Google Scholar] [CrossRef] [PubMed]
- Reinstein, D.Z.; Gobbe, M.; Archer, T.J.; Silverman, R.H.; Coleman, D.J. Epithelial, stromal, and total corneal thickness in keratoconus: Three-dimensional display with artemis very-high frequency digital ultrasound. J. Refract. Surg. 2010, 26, 259–271. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Tan, O.; Brass, R.; Weiss, J.L.; Huang, D. Corneal epithelial thickness mapping by Fourier-domain optical coherence tomography in normal and keratoconic eyes. Ophthalmology 2012, 119, 2425–2433. [Google Scholar] [CrossRef] [PubMed]
- Reinstein, D.Z.; Archer, T.J.; Gobbe, M.; Silverman, R.H.; Coleman, D.J. Epithelial thickness in the normal cornea: Three-dimensional display with Artemis very high-frequency digital ultrasound. J. Refract. Surg. 2008, 24, 571–581. [Google Scholar] [CrossRef]
- Reinstein, D.Z.; Archer, T.J.; Dickeson, Z.I.; Gobbe, M. Transepithelial phototherapeutic keratectomy protocol for treating irregular astigmatism based on population epithelial thickness measurements by artemis very high-frequency digital ultrasound. J. Refract. Surg. 2014, 30, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Lohmann, C.P.; Reischl, U.; Marshall, J. Regression and epithelial hyperplasia after myopic photorefractive keratectomy in a human cornea. J. Cataract Refract. Surg. 1999, 25, 712–715. [Google Scholar] [CrossRef]
- Reinstein, D.Z.; Ameline, B.; Puech, M.; Montefiore, G.; Laroche, L. VHF digital ultrasound three-dimensional scanning in the diagnosis of myopic regression after corneal refractive surgery. J. Refract. Surg. 2005, 21, 480–484. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.S.Y.; Kim, S.W. Effect of Corneal Cross-linking on Epithelial Hyperplasia and Myopia Regression after Transepithelial Photorefractive Keratectomy. J. Refract. Surg. 2019, 35, 354–361. [Google Scholar] [CrossRef]
- Ryu, I.H.; Kim, W.K.; Nam, M.S.; Kim, J.K.; Kim, S.W. Reduction of corneal epithelial thickness during medical treatment for myopic regression following FS-LASIK. BMC Ophthalmol. 2020, 20, 296. [Google Scholar] [CrossRef]
- Alharbi, A.; Swarbrick, H.A. The effects of overnight orthokeratology lens wear on corneal thickness. Investig. Ophthalmol. Vis. Sci. 2003, 44, 2518–2523. [Google Scholar] [CrossRef]
- Reinstein, D.Z.; Gobbe, M.; Archer, T.J.; Couch, D.; Bloom, B. Epithelial, stromal, and corneal pachymetry changes during orthokeratology. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom. 2009, 86, E1006–E1014. [Google Scholar] [CrossRef]
- Kim, W.K.; Kim, B.J.; Ryu, I.H.; Kim, J.K.; Kim, S.W. Corneal epithelial and stromal thickness changes in myopic orthokeratology and their relationship with refractive change. PLoS ONE 2018, 13, e0203652. [Google Scholar] [CrossRef]
- Zhou, J.; Xue, F.; Zhou, X.; Naidu, R.K.; Qian, Y. Thickness profiles of the corneal epithelium along the steep and flat meridians of astigmatic corneas after orthokeratology. BMC Ophthalmol. 2020, 20, 240. [Google Scholar] [CrossRef]
- Francoz, M.; Karamoko, I.; Baudouin, C.; Labbe, A. Ocular surface epithelial thickness evaluation with spectral-domain optical coherence tomography. Investig. Ophthalmol. Vis. Sci. 2011, 52, 9116–9123. [Google Scholar] [CrossRef] [PubMed]
- Niederer, R.L.; Perumal, D.; Sherwin, T.; McGhee, C.N. Age-related differences in the normal human cornea: A laser scanning in vivo confocal microscopy study. Br. J. Ophthalmol. 2007, 91, 1165–1169. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.J.; Ryu, I.H.; Kim, S.W. Age-related differences in corneal epithelial thickness measurements with anterior segment optical coherence tomography. Jpn. J. Ophthalmol. 2016, 60, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Hong, J.; Deng, S.X.; Xu, J. Age-related changes in human corneal epithelial thickness measured with anterior segment optical coherence tomography. Investig. Ophthalmol. Vis. Sci. 2014, 55, 5032–5038. [Google Scholar] [CrossRef]
- Chang, S.W.; Tsai, I.L.; Hu, F.R.; Lin, L.L.; Shih, Y.F. The cornea in young myopic adults. Br. J. Ophthalmol. 2001, 85, 916–920. [Google Scholar] [CrossRef]
- Pedersen, L.; Hjortdal, J.; Ehlers, N. Central corneal thickness in high myopia. Acta Ophthalmol. Scand. 2005, 83, 539–542. [Google Scholar] [CrossRef]
- Prasad, A.; Fry, K.; Hersh, P.S. Relationship of age and refraction to central corneal thickness. Cornea 2011, 30, 553–555. [Google Scholar] [CrossRef]
- Wang, X.; Dong, J.; Wu, Q. Corneal thickness, epithelial thickness and axial length differences in normal and high myopia. BMC Ophthalmol. 2015, 15, 49. [Google Scholar] [CrossRef]
- Kim, B.J.; Ryu, I.H.; Lee, J.H.; Kim, S.W. Correlation of Sex and Myopia with Corneal Epithelial and Stromal Thicknesses. Cornea 2016, 35, 1078–1083. [Google Scholar] [CrossRef]
- Ma, Y.; He, X.; Zhu, X.; Lu, L.; Zhu, J.; Zou, H. Corneal Epithelium Thickness Profile in 614 Normal Chinese Children Aged 7-15 Years Old. Sci. Rep. 2016, 6, 23482. [Google Scholar] [CrossRef]
- Hahn, S.; Azen, S.; Ying-Lai, M.; Varma, R.; Los Angeles Latino Eye Study, G. Central corneal thickness in Latinos. Investig. Ophthalmol. Vis. Sci. 2003, 44, 1508–1512. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, H.; Yazdani, K.; Mehravaran, S.; KhabazKhoob, M.; Mohammad, K.; Parsafar, H.; Fotouhi, A. Corneal thickness in a population-based, cross-sectional study: The Tehran Eye Study. Cornea 2009, 28, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Shimmyo, M.; Ross, A.J.; Moy, A.; Mostafavi, R. Intraocular pressure, Goldmann applanation tension, corneal thickness, and corneal curvature in Caucasians, Asians, Hispanics, and African Americans. Am. J. Ophthalmol. 2003, 136, 603–613. [Google Scholar] [CrossRef]
- Aghaian, E.; Choe, J.E.; Lin, S.; Stamper, R.L. Central corneal thickness of Caucasians, Chinese, Hispanics, Filipinos, African Americans, and Japanese in a glaucoma clinic. Ophthalmology 2004, 111, 2211–2219. [Google Scholar] [CrossRef] [PubMed]
- Gupta, P.D.; Johar, K., Sr.; Nagpal, K.; Vasavada, A.R. Sex hormone receptors in the human eye. Surv. Ophthalmol. 2005, 50, 274–284. [Google Scholar] [CrossRef] [PubMed]
- Giuffre, G.; Di Rosa, L.; Fiorino, F.; Bubella, D.M.; Lodato, G. Variations in central corneal thickness during the menstrual cycle in women. Cornea 2007, 26, 144–146. [Google Scholar] [CrossRef]
- AlMahmoud, T.; Priest, D.; Munger, R.; Jackson, W.B. Correlation between refractive error, corneal power, and thickness in a large population with a wide range of ametropia. Investig. Ophthalmol. Vis. Sci. 2011, 52, 1235–1242. [Google Scholar] [CrossRef]
- Iribarren, R.; Fuentes Bonthoux, F.; Pfortner, T.; Chiaradia, P.; Stell, W.K. Corneal power is correlated with anterior chamber diameter. Investig. Ophthalmol. Vis. Sci. 2012, 53, 3788–3791. [Google Scholar] [CrossRef]
| Male (n = 122) | Female (n = 201) | p-Value | |
|---|---|---|---|
| Age (years) | 9.16 ± 2.04 | 9.84 ± 2.23 | 0.006 * |
| SEQ (D) | −2.29 ± 1.40 | −2.40 ± 1.34 | 0.468 |
| CCT (µm) | 540.43 ± 32.77 | 531.37 ± 32.10 | 0.015 * |
| Mean K (D) | 43.01 ± 1.33 | 43.64 ± 1.22 | <0.001 * |
| Epithelium (µm) | |||
| Central | 52.98 ± 2.50 | 51.57 ± 3.22 | <0.001 * |
| Paracentral | 53.14 ± 2.36 | 51.67 ± 3.02 | <0.001 * |
| Midperiphery | 53.79 ± 6.02 | 51.88 ± 2.81 | <0.001 * |
| Stroma (µm) | |||
| Central | 487.45 ± 32.24 | 479.80 ± 31.57 | 0.037 * |
| Paracentral | 507.30 ± 32.75 | 498.95 ± 32.34 | 0.026 * |
| Midperiphery | 528.80 ± 34.34 | 521.29 ± 32.79 | 0.051 |
| Male (n = 64) | Female (n = 101) | p-Value | |
|---|---|---|---|
| Age (years) | 9.23 ± 2.06 | 10.06 ± 2.31 | 0.021 * |
| SEQ (D) | −2.13 ± 1.27 | −2.34± 1.28 | 0.293 |
| Axial length (mm) | 24.70 ± 0.86 | 24.40 ± 0.73 | 0.020 * |
| Mean K (D) | 42.89 ± 1.37 | 43.58 ± 1.08 | 0.001 * |
| WTW (mm) | 12.02 ± 0.42 | 11.96 ± 0.41 | 0.305 |
| ACD (mm) | 3.88 ± 0.22 | 3.84 ± 0.21 | 0.312 |
| CCT (µm) | 537.44 ± 30.88 | 528.92 ± 31.81 | 0.092 |
| Epithelium (µm) | |||
| Central | 52.70 ± 2.49 | 51.54 ± 3.15 | 0.014 * |
| Paracentral | 52.86 ± 2.33 | 51.58 ± 2.99 | 0.004 * |
| Midperiphery | 53.01 ± 2.16 | 51.81 ± 2.88 | 0.005 * |
| Stroma (µm) | |||
| Central | 484.73 ± 30.46 | 477.38 ± 30.96 | 0.136 |
| Paracentral | 504.67 ± 31.54 | 497.15 ± 32.23 | 0.143 |
| Midperipheral | 528.55 ± 33.25 | 521.85 ± 32.04 | 0.199 |
| Height (cm) | 140.39 ± 14.52 | 142.78± 12.31 | 0.259 |
| Weight (kg) | 38.10 ± 13.09 | 37.24 ± 9.74 | 0.654 |
| Simple Regression | Multiple Regression | |||||
|---|---|---|---|---|---|---|
| B | R | p-Value | B | β | p-Value | |
| Central 2 mm zone epithelium | 0.467 (R) | <0.001 | ||||
| Age | 0.215 | 0.164 | 0.036 | −0.138 | −0.105 | 0.318 |
| Sex | −1.159 | 0.191 | 0.014 | −0.911 | −0.15 | 0.045 |
| Body weight | 0.079 | 0.296 | <0.001 | 0.095 | 0.356 | 0.001 |
| Height | 0.242 | 0.054 | 0.002 | |||
| WTW | −1.382 | 0.193 | 0.013 | −1.550 | −0.217 | 0.004 |
| CCT | 0.028 | 0.297 | <0.001 | 0.019 | 0.198 | 0.008 |
| SEQ | −0.071 | 0.030 | 0.698 | |||
| ACD | −0.937 | 0.068 | 0.388 | |||
| Axial length | 0.479 | 0.128 | 0.100 | |||
| Mean K | −0.306 | 0.129 | 0.099 | |||
| Stroma | 0.285 (R) | 0.003 | ||||
| Age | 2.403 | 0.175 | 0.025 | 2.715 | 0.198 | 0.011 |
| Sex | −7.358 | 0.116 | 0.136 | −10.448 | −0.165 | 0.033 |
| WTW | −12.106 | 0.162 | 0.037 | −12.490 | −0.167 | 0.029 |
| Height | 0.308 | 0.132 | 0.092 | |||
| Body weight | 0.400 | 0.144 | 0.065 | |||
| ACD | 17.84 | 0.124 | 0.114 | |||
| Axial length | 4.866 | 0.125 | 0.109 | |||
| Mean K | 0.276 | 0.011 | 0.877 | |||
| SEQ | −2.542 | 0.105 | 0.180 | |||
| Multiple Regression | Multiple Regression | |||||
|---|---|---|---|---|---|---|
| B | R/β | p-Value | B | R/β | p-Value | |
| Epithelium | Paracenter | 0.419 | <0.001 | Mid-periphery | 0.367 | <0.001 |
| Age | −0.047 | −0.038 | 0.725 | −0.010 | −0.008 | 0.942 |
| Sex | −1.135 | −0.197 | 0.011 | −1.125 | −0.205 | 0.010 |
| Body weight | 0.072 | 0.295 | 0.008 | 0.055 | 0.229 | 0.036 |
| WTW | −1.088 | −0.160 | 0.035 | −0.867 | −0.134 | 0.084 |
| CCT | 0.014 | 0.154 | 0.043 | 0.010 | 0.113 | 0.147 |
| Stroma | Paracenter | 0.301 | 0.002 | Mid-periphery | 0.330 | <0.001 |
| Age | 2.904 | 0.204 | 0.009 | 3.274 | 0.226 | 0.003 |
| Sex | −10.906 | −0.166 | 0.032 | −10.566 | −0.158 | 0.038 |
| WTW | −14.610 | −0.188 | 0.013 | −17.061 | −0.217 | 0.004 |
| SEQ | Mean K | WTW | Axial Length | ACD | Height | Body Weight | Age | |
|---|---|---|---|---|---|---|---|---|
| SEQ | 1 | |||||||
| Mean K | −0.067 | 1 | ||||||
| WTW | 0.061 | −0.378 ** | 1 | |||||
| Axial length | −0.634 ** | −0.593 ** | 0.248 ** | 1 | ||||
| ACD | −0.215 ** | 0.065 | 0.513 ** | 0.308 ** | 1 | |||
| Height | −0.332 ** | −0.155 * | −0.060 | 0.459 ** | 0.174 * | 1 | ||
| Body weight | −0.269 * | −0.205 ** | 0.118 | 0.447 ** | 0.204 ** | 0.869 ** | 1 | |
| Age | −0.275 ** | −0.031 | −0.123 | 0.367 ** | 0.133 | 0.838 ** | 0.701 ** | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, W.K.; Ryu, I.H.; Yoo, J.; Kim, S.W. Effect of Gender, Age, and Ocular and Growth-Related Factors on Corneal Epithelial and Stromal Thickness in Children. J. Clin. Med. 2020, 9, 3849. https://doi.org/10.3390/jcm9123849
Kim WK, Ryu IH, Yoo J, Kim SW. Effect of Gender, Age, and Ocular and Growth-Related Factors on Corneal Epithelial and Stromal Thickness in Children. Journal of Clinical Medicine. 2020; 9(12):3849. https://doi.org/10.3390/jcm9123849
Chicago/Turabian StyleKim, Wook Kyum, Ik Hee Ryu, Jeongseo Yoo, and Sun Woong Kim. 2020. "Effect of Gender, Age, and Ocular and Growth-Related Factors on Corneal Epithelial and Stromal Thickness in Children" Journal of Clinical Medicine 9, no. 12: 3849. https://doi.org/10.3390/jcm9123849
APA StyleKim, W. K., Ryu, I. H., Yoo, J., & Kim, S. W. (2020). Effect of Gender, Age, and Ocular and Growth-Related Factors on Corneal Epithelial and Stromal Thickness in Children. Journal of Clinical Medicine, 9(12), 3849. https://doi.org/10.3390/jcm9123849






