Using the Thickness Map from Macular Ganglion Cell Analysis to Differentiate Retinal Vein Occlusion from Glaucoma
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Retinal Vein Occlusion
2.3. Primary Open-Angle Glaucoma
2.4. Spectral-Domain Optical Coherence Tomography
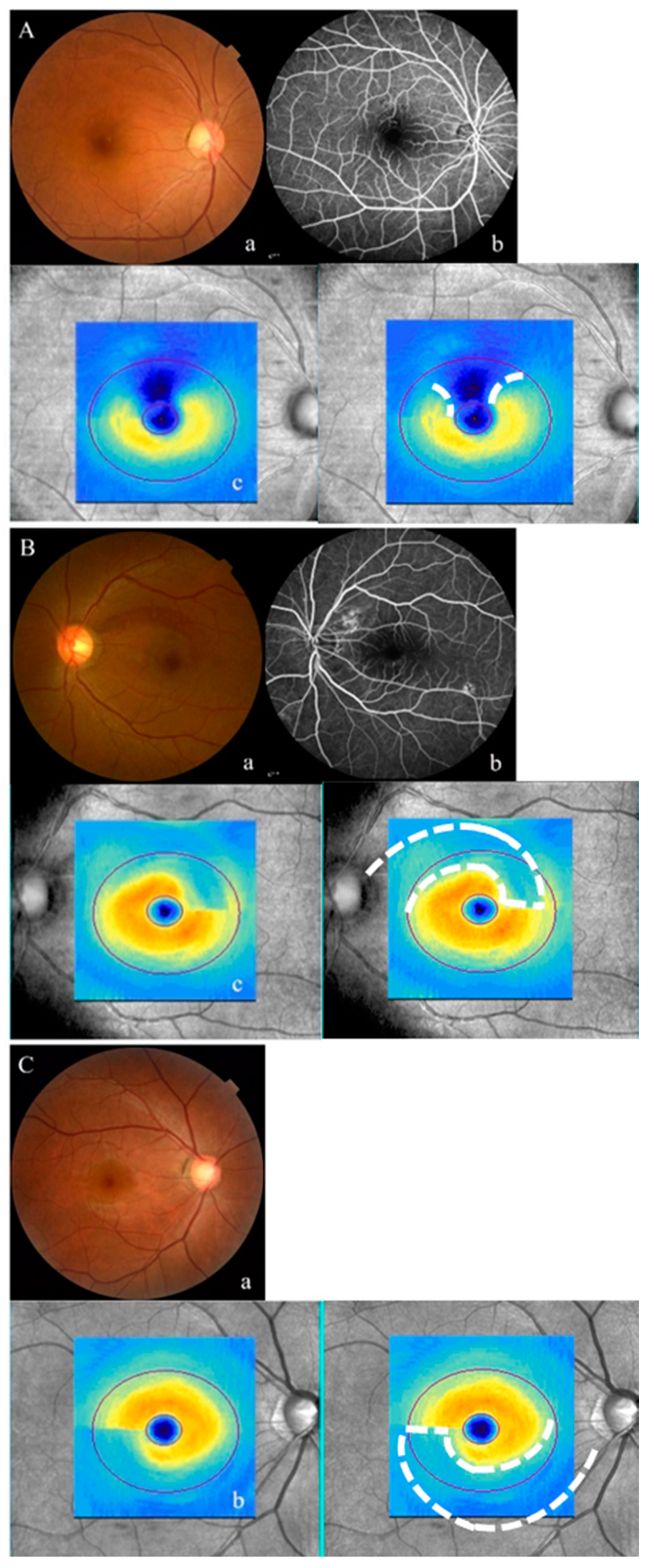
2.5. Qualitative Analysis of the Thickness Map of the GCA
2.6. Statistical Analyses
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Jaulim, A.; Ahmed, B.; Khanam, T.; Chatziralli, I.P. Branch retinal vein occlusion: Epidemiology, pathogenesis, risk factors, clinical features, diagnosis, and complications. An update of the literature. Retina 2013, 33, 901–910. [Google Scholar] [CrossRef] [PubMed]
- Aghi, M.K.; Chen, C.C.; Fleseriu, M.; Newman, S.A.; Lucas, J.W.; Kuo, J.S.; Barkhoudarian, G.; Farrell, C.J.; Sheehan, J.; Ziu, M. Congress of neurological surgeons systematic review and evidence-based guidelines on the management of patients with nonfunctioning pituitary adenomas: Executive summary. Neurosurgery 2016, 79, 521–523. [Google Scholar] [CrossRef] [PubMed]
- Micieli, J.A.; Newman, N.J.; Biousse, V. The role of optical coherence tomography in the evaluation of compressive optic neuropathies. Curr. Opin. Neurol. 2019, 32, 115–123. [Google Scholar] [CrossRef]
- Iorga, R.E.; Moraru, A.; Ozturk, M.R.; Costin, D. The role of optical coherence tomography in optic neuropathies. Rom. J. Ophthalmol. 2018, 62, 3. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.J.; Han, J.C.; Kee, C. Difference in Topographic Pattern of Prelaminar and Neuroretinal Rim Thinning Between Nonarteritic Anterior Ischemic Optic Neuropathy and Glaucoma. Investig. Ophthalmol. Vis. Sci. 2019, 60, 2461–2467. [Google Scholar] [CrossRef]
- Lee, Y.H.; Kim, K.N.; Heo, D.W.; Kang, T.S.; Lee, S.B.; Kim, C.-S. Difference in patterns of retinal ganglion cell damage between primary open-angle glaucoma and non-arteritic anterior ischaemic optic neuropathy. PLoS ONE 2017, 12, e0187093. [Google Scholar] [CrossRef]
- Lee, H.M.; Lee, W.H.; Kim, K.N.; Jo, Y.J.; Kim, J.Y. Changes in thickness of central macula and retinal nerve fibre layer in severe hypertensive retinopathy: A 1-year longitudinal study. Acta Ophthalmol. 2018, 96, e386–e392. [Google Scholar] [CrossRef]
- Lee, S.H.; Lee, W.H.; Lim, H.B.; Jo, Y.J.; Kim, J.Y. Thicknesses of central macular, retinal nerve fiber, and ganglion cell inner plexiform layers in patients with hypertension. Retina 2019, 39, 1810–1818. [Google Scholar] [CrossRef]
- Kim, C.-S.; Shin, K.-S.; Lee, H.-J.; Jo, Y.-J.; Kim, J.-Y. Sectoral retinal nerve fiber layer thinning in branch retinal vein occlusion. Retina 2014, 34, 525–530. [Google Scholar] [CrossRef]
- Baek, S.U.; Kim, K.E.; Kim, Y.K.; Park, K.H.; Jeoung, J.W. Development of topographic scoring system for identifying glaucoma in myopic eyes: A spectral-domain OCT study. Ophthalmology 2018, 125, 1710–1719. [Google Scholar] [CrossRef]
- Hwang, Y.H.; Jeong, Y.C.; Kim, H.K.; Sohn, Y.H. Macular ganglion cell analysis for early detection of glaucoma. Ophthalmology 2014, 121, 1508–1515. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.K.; Yoo, B.W.; Jeoung, J.W.; Kim, H.C.; Kim, H.J.; Park, K.H. Glaucoma-diagnostic ability of ganglion cell-inner plexiform layer thickness difference across temporal raphe in highly myopic eyes. Investig. Ophthalmol. Vis. Sci. 2016, 57, 5856–5863. [Google Scholar] [CrossRef]
- Mwanza, J.-C.; Oakley, J.D.; Budenz, D.L.; Chang, R.T.; O’Rese, J.K.; Feuer, W.J. Macular ganglion cell–inner plexiform layer: Automated detection and thickness reproducibility with spectral domain–optical coherence tomography in glaucoma. Investig. Ophthalmol. Vis. Sci. 2011, 52, 8323–8329. [Google Scholar] [CrossRef] [PubMed]
- Mwanza, J.-C.; Durbin, M.K.; Budenz, D.L.; Sayyad, F.E.; Chang, R.T.; Neelakantan, A.; Godfrey, D.G.; Carter, R.; Crandall, A.S. Glaucoma diagnostic accuracy of ganglion cell–inner plexiform layer thickness: Comparison with nerve fiber layer and optic nerve head. Ophthalmology 2012, 119, 1151–1158. [Google Scholar] [CrossRef] [PubMed]
- Jeoung, J.W.; Choi, Y.J.; Park, K.H.; Kim, D.M. Macular ganglion cell imaging study: Glaucoma diagnostic accuracy of spectral-domain optical coherence tomography. Investig. Ophthalmol. Vis. Sci. 2013, 54, 4422–4429. [Google Scholar] [CrossRef]
- Choi, Y.J.; Jeoung, J.W.; Park, K.H.; Kim, D.M. Glaucoma detection ability of ganglion cell-inner plexiform layer thickness by spectral-domain optical coherence tomography in high myopia. Investig. Ophthalmol. Vis. Sci. 2013, 54, 2296–2304. [Google Scholar] [CrossRef]
- Katz, J.; Sommer, A.; Gaasterland, D.E.; Anderson, D.R. Comparison of analytic algorithms for detecting glaucomatous visual field loss. Arch. Ophthalmol. 1991, 109, 1684–1689. [Google Scholar] [CrossRef]
- Anderson, D.R.; Patella, V.M. Automated Static Perimetry, 2nd ed.; Mosby: St Louis, MI, USA, 1999. [Google Scholar]
- Landis, J.R.; Koch, G.G. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics 1977, 33, 363–374. [Google Scholar] [CrossRef]
- David, R.; Zangwill, L.; Badarna, M.; Yassur, Y. Epidemiology of retinal vein occlusion and its association with glaucoma and increased intraocular pressure. Ophthalmologica 1988, 197, 69–74. [Google Scholar] [CrossRef]
- Beaumont, P.E.; Kang, H.K. Cup-to-disc ratio, intraocular pressure, and primary open-angle glaucoma in retinal venous occlusion. Ophthalmology 2002, 109, 282–286. [Google Scholar] [CrossRef]
- Klein, B.E.; Meuer, S.M.; Knudtson, M.D.; Klein, R. The relationship of optic disk cupping to retinal vein occlusion: The Beaver Dam Eye Study. Am. J. Ophthalmol. 2006, 141, 859–862. [Google Scholar] [CrossRef] [PubMed]
- Yin, X.; Li, J.; Zhang, B.; Lu, P. Association of glaucoma with risk of retinal vein occlusion: A meta-analysis. Acta Ophthalmol. 2019, 97, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Son, Y.; Lee, S.; Park, J. Measurement of lamina and prelaminar thicknesses of both eyes in patients with unilateral branch retinal vein occlusion. Graefe’s Arch. Clin. Exp. Ophthalmol. 2017, 255, 503–508. [Google Scholar] [CrossRef]
- Kim, S.; Sung, K.R.; Joe, S.G.; Kim, J.T.; Lee, D.H.; Lee, J.Y.; Kim, J.-G. Comparison between glaucomatous and non-glaucomatous eyes with unilateral retinal vein occlusion in the fellow eye. Korean J. Ophthalmol. 2013, 27, 440–445. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Na, K.I.; Jeoung, J.W.; Kim, Y.K.; Lee, W.J.; Park, K.H. Incidence of retinal vein occlusion in open-angle glaucoma: A nationwide, population-based study using the Korean Health Insurance Review and Assessment Database. Clin. Exp. Ophthalmol. 2018, 46, 637–644. [Google Scholar] [CrossRef]
- Park, H.-Y.L.; Jung, Y.; Han, K.; Lee, M.Y.; Park, C.K. Health care claims for primary open-angle glaucoma and retinal vein occlusion from an 11-year nationwide dataset. Sci. Rep. 2017, 7, 1–8. [Google Scholar] [CrossRef]
- Sirakaya, E.; Kucuk, B. Thickness of the Lamina Cribrosa, Retinal-Nerve Fiber Layer, and Peripapillary Choroid in Patients with Branch Retinal Vein Occlusion. Ophthalmologica 2020, 243, 288–296. [Google Scholar] [CrossRef]
- Han, J.C.; Eo, D.R.; Lee, T.K.; Shin, J.H.; Kee, C. Does glaucoma share common pathogenesis with branch retinal vein occlusion? PLoS ONE 2016, 11, e0156966. [Google Scholar] [CrossRef]
- Hoyt, W.F.; Luis, O. Visual fiber anatomy in the infrageniculate pathway of the primate: Uncrossed and crossed retinal quadrant fiber projections studied with Nauta silver stain. Arch. Ophthalmol. 1962, 68, 94–106. [Google Scholar] [CrossRef]
- Quigley, H.A.; Dunkelberger, G.R.; Green, W.R. Chronic human glaucoma causing selectively greater loss of large optic nerve fibers. Ophthalmology 1988, 95, 357–363. [Google Scholar] [CrossRef]
- Brar, M.; Sharma, M.; Grewal, S.; Grewal, D.S. Quantification of retinal microvasculature and neurodegeneration changes in branch retinal vein occlusion after resolution of cystoid macular edema on optical coherence tomography angiography. Indian J. Ophthalmol. 2019, 67, 1864. [Google Scholar] [CrossRef] [PubMed]
- Manabe, S.; Osaka, R.; Nakano, Y.; Takasago, Y.; Fujita, T.; Shiragami, C.; Hirooka, K.; Muraoka, Y.; Tsujikawa, A. Association between parafoveal capillary nonperfusion and macular function in eyes with branch retinal vein occlusion. Retina 2017, 37, 1731–1737. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |

| RVO (n = 37) | POAG (n = 74) | p-Value * | |
|---|---|---|---|
| Age (years) | 63.43 ± 10.26 | 61.81 ± 12.53 | 0.476 |
| Sex (male/female) | 13/24 | 34/40 | 0.277 |
| BCVA (decimal) | 0.94 ± 0.16 | 1.01 ± 0.24 | 0.109 |
| Axial length (mm) | 23.86 ± 0.91 | 23.59 ± 1.10 | 0.391 |
| Intraocular pressure (mmHg) | 14.97 ± 2.67 | 15.97 ± 2.82 | 0.186 |
| Damaged hemisphere (%) † | <0.001 ‡ | ||
| Superior | 24 (64.86) | 16 (21.62) | |
| Inferior | 13 (35.14) | 58 (78.38) | |
| Signal strength of optic disc scan | 9.30 ± 0.66 | 9.35 ± 0.65 | 0.675 |
| Average RNFL thickness (μm) | 84.81 ± 9.45 | 83.13 ± 8.94 | 0.376 |
| Signal strength of macular scan | 9.22 ± 0.75 | 9.00 ± 0.81 | 0.237 |
| Average GCIPL thickness (μm) | 73.43 ± 9.91 | 73.17 ± 6.40 | 0.963 |
| RVO (n = 37) | POAG (n = 74) | p-Value * | |
|---|---|---|---|
| Quadrant RNFL thickness (μm) † | |||
| Superior ‡ | 113.06 ± 10.28 | 109.66 ± 10.22 | 0.113 |
| Nasal | 63.75 ± 7.66 | 65.18 ± 7.62 | 0.371 |
| Inferior ‡ | 93.06 ± 11.98 | 89.89 ± 11.91 | 0.205 |
| Temporal | 64.94 ± 8.39 | 70.30 ± 8.35 | 0.003 |
| Minimum GCIPL thickness (μm) § | 51.50 ± 13.70 | 60.35 ± 13.60 | 0.002 |
| Sectoral GCIPL thickness (μm) § | |||
| Superotemporal # | 79.08 ± 6.06 | 76.75 ± 6.02 | 0.068 |
| Superior ‡ | 79.96 ± 5.07 | 79.36 ± 5.03 | 0.571 |
| Superonasal ¶ | 82.27 ± 6.36 | 81.89 ± 6.31 | 0.772 |
| Inferonasal ¶ | 74.45 ± 11.08 | 74.24 ± 11.00 | 0.929 |
| Inferior ‡ | 60.71 ± 13.06 | 64.78 ± 12.96 | 0.137 |
| Inferotemporal # | 61.84 ± 11.28 | 62.07 ± 11.20 | 0.922 |
| RVO (n = 37) | POAG (n = 74) | p-Value † | |
|---|---|---|---|
| Central macular thickness (μm) | 242.84 ± 20.75 | 249.57 ± 20.59 | 0.132 |
| Inner circle macular thickness (μm) | |||
| Superior * | 316.96 ± 14.41 | 319.76 ± 14.30 | 0.352 |
| Nasal | 314.88 ± 19.39 | 319.91 ± 19.25 | 0.215 |
| Inferior * | 288.55 ± 31.20 | 298.82 ± 30.97 | 0.117 |
| Temporal | 297.40 ± 17.95 | 297.79 ± 17.82 | 0.918 |
| Outer circle macular thickness (μm) | |||
| Superior * | 273.37 ± 13.69 | 271.41 ± 13.58 | 0.492 |
| Nasal | 293.90 ± 17.69 | 289.00 ± 17.56 | 0.185 |
| Inferior * | 260.88 ± 25.36 | 243.42 ± 25.17 | 0.001 |
| Temporal | 259.20 ± 13.65 | 249.28 ± 13.54 | 0.001 |
| Irregular GCA Thickness Map (n = 25) | Regular GCA Thickness Map (n = 12) | p-Value * | |
|---|---|---|---|
| Age (years) | 61.04 ± 8.64 | 68.42 ± 11.90 | 0.019 |
| Sex (male/female) | 10/15 | 3/9 | 0.476 † |
| BCVA (decimal) | 0.94 ± 0.12 | 0.93 ± 0.23 | 0.761 |
| Axial length (mm) | 24.09 ± 0.80 | 23.43 ± 0.97 | 0.094 |
| Intraocular pressure (mmHg) | 15.20 ± 2.25 | 16.58 ± 2.84 | 0.190 |
| Damaged hemisphere ‡ | 0.149 † | ||
| Superior | 14 | 10 | |
| Inferior | 11 | 2 | |
| Signal strength of optic disc scan | 9.23 ± 0.67 | 9.38 ± 0.78 | 0.394 |
| Average RNFL thickness (μm) | 85.20 ± 8.92 | 84.00 ± 10.85 | 0.723 |
| Signal strength of macular scan | 9.31 ± 0.71 | 9.01 ± 0.72 | 0.209 |
| Average GCIPL thickness (μm) | 71.60 ± 10.86 | 77.25 ± 6.37 | 0.105 |
| Irregular GCA Thickness Map (n = 25) | Regular GCA Thickness Map (n = 12) | p Value | |
|---|---|---|---|
| Quadrant RNFL thickness (μm) * | |||
| Superior ‡ | 117.54 ± 9.39 | 108.87 ± 9.67 | 0.018 |
| Nasal | 65.39 ± 3.35 | 62.77 ± 7.57 | 0.343 |
| Inferior ‡ | 92.38 ± 10.78 | 98.97 ± 11.10 | 0.109 |
| Temporal | 63.60 ± 7.88 | 68.83 ± 8.11 | 0.084 |
| Minimum GCIPL thickness (μm) † | 45.31 ± 14.35 | 67.35 ± 15.16 | <0.001 |
| Sectoral GCIPL thickness (μm) † | |||
| Superior ‡ | 80.81 ± 5.91 | 77.31 ± 6.24 | 0.138 |
| Superonasal § | 83.71 ± 8.74 | 78.86 ± 9.23 | 0.164 |
| Inferonasal § | 72.87 ± 14.70 | 80.03 ± 15.53 | 0.219 |
| Inferior ‡ | 56.11 ± 16.36 | 72.77 ± 17.29 | 0.014 |
| Inferotemporal ¶ | 58.69 ± 13.14 | 70.90 ± 13.88 | 0.023 |
| Superotemporal ¶ | 79.03 ± 8.02 | 79.44 ± 8.47 | 0.894 |
| Central macular thickness (μm) † | 240.40 ± 25.14 | 247.00 ± 26.56 | 0.504 |
| Inner circle macular thickness (μm) † | |||
| Superior ‡, | 318.47 ± 14.89 | 311.44 ± 15.73 | 0.234 |
| Nasal | 316.39 ± 24.79 | 312.01 ± 26.19 | 0.652 |
| Inferior ‡ | 279.09 ± 34.51 | 309.73 ± 36.46 | 0.029 |
| Temporal | 295.68 ± 22.96 | 302.17 ± 24.25 | 0.472 |
| Outer circle macular thickness (μm) † | |||
| Superior ‡ | 278.62 ± 12.88 | 261.46 ± 13.61 | 0.002 |
| Nasal | 295.28 ± 20.09 | 291.75 ± 21.23 | 0.654 |
| Inferior ‡ | 258.85 ± 34.92 | 270.81 ± 36.89 | 0.385 |
| Temporal | 260.56 ± 16.87 | 258.09 ± 17.82 | 0.709 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, N.H.; Park, K.S.; Lee, H.M.; Kim, J.Y.; Kim, C.-s.; Kim, K.N. Using the Thickness Map from Macular Ganglion Cell Analysis to Differentiate Retinal Vein Occlusion from Glaucoma. J. Clin. Med. 2020, 9, 3294. https://doi.org/10.3390/jcm9103294
Lee NH, Park KS, Lee HM, Kim JY, Kim C-s, Kim KN. Using the Thickness Map from Macular Ganglion Cell Analysis to Differentiate Retinal Vein Occlusion from Glaucoma. Journal of Clinical Medicine. 2020; 9(10):3294. https://doi.org/10.3390/jcm9103294
Chicago/Turabian StyleLee, Nam Ho, Kee Sup Park, Han Min Lee, Jung Yeul Kim, Chang-sik Kim, and Kyoung Nam Kim. 2020. "Using the Thickness Map from Macular Ganglion Cell Analysis to Differentiate Retinal Vein Occlusion from Glaucoma" Journal of Clinical Medicine 9, no. 10: 3294. https://doi.org/10.3390/jcm9103294
APA StyleLee, N. H., Park, K. S., Lee, H. M., Kim, J. Y., Kim, C.-s., & Kim, K. N. (2020). Using the Thickness Map from Macular Ganglion Cell Analysis to Differentiate Retinal Vein Occlusion from Glaucoma. Journal of Clinical Medicine, 9(10), 3294. https://doi.org/10.3390/jcm9103294





