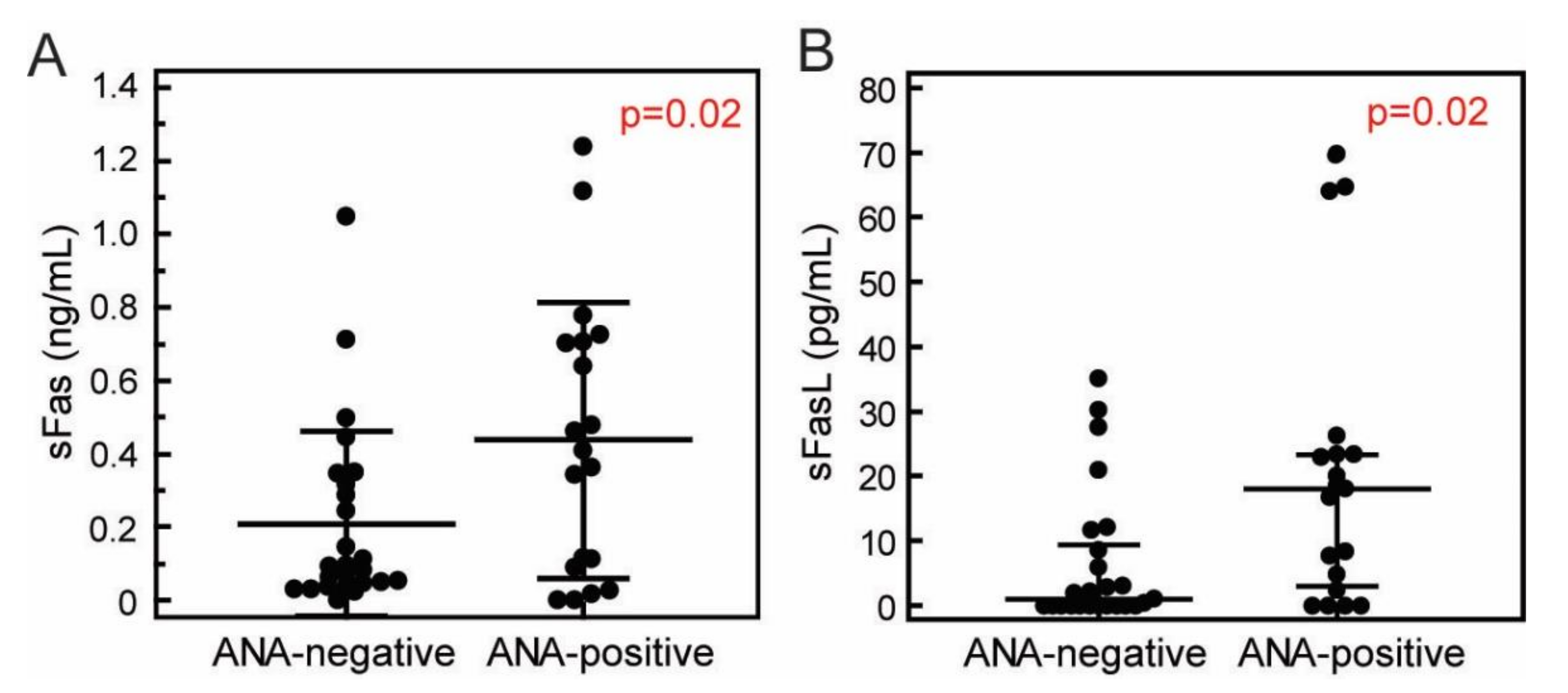
Elevated Concentrations of Soluble Fas and FasL in Multiple Sclerosis Patients with Antinuclear Antibodies
Abstract
1. Introduction
2. Materials and Methods
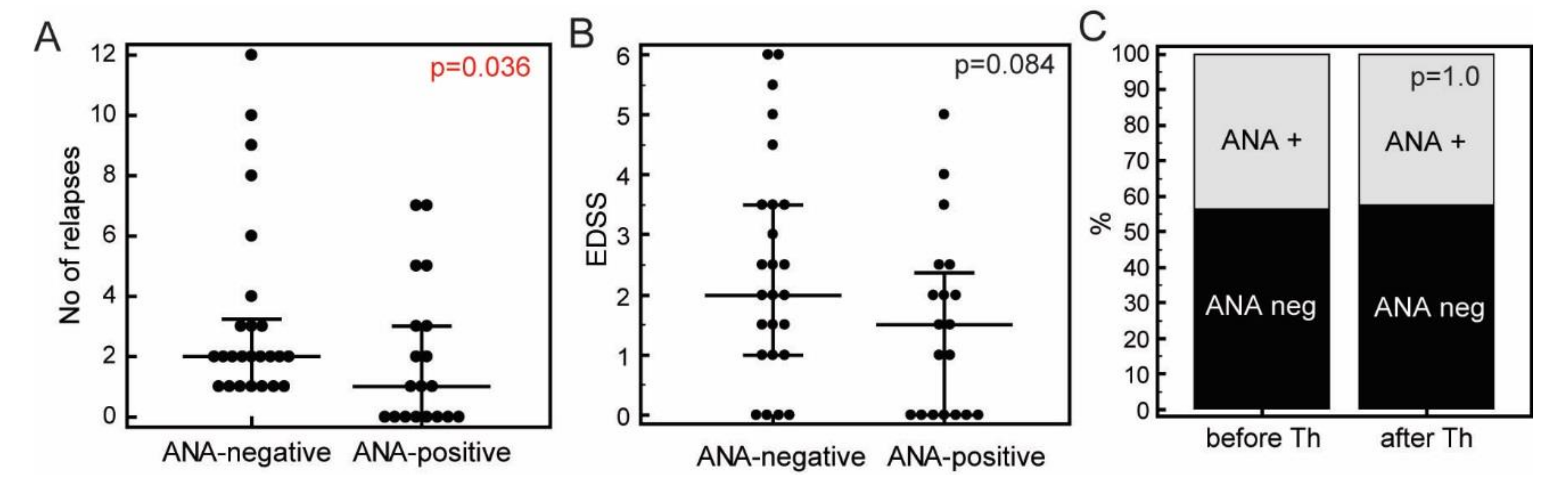
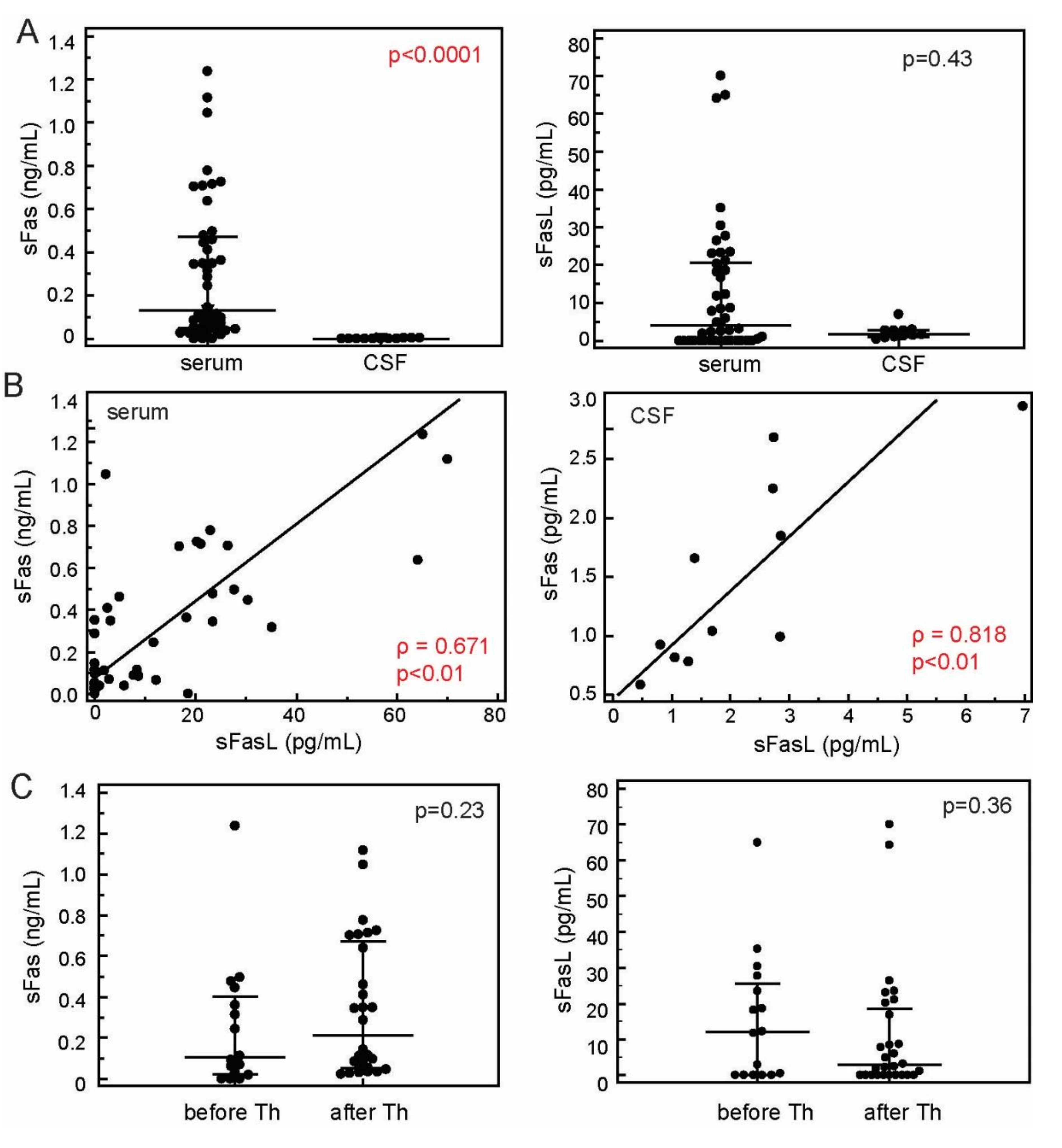
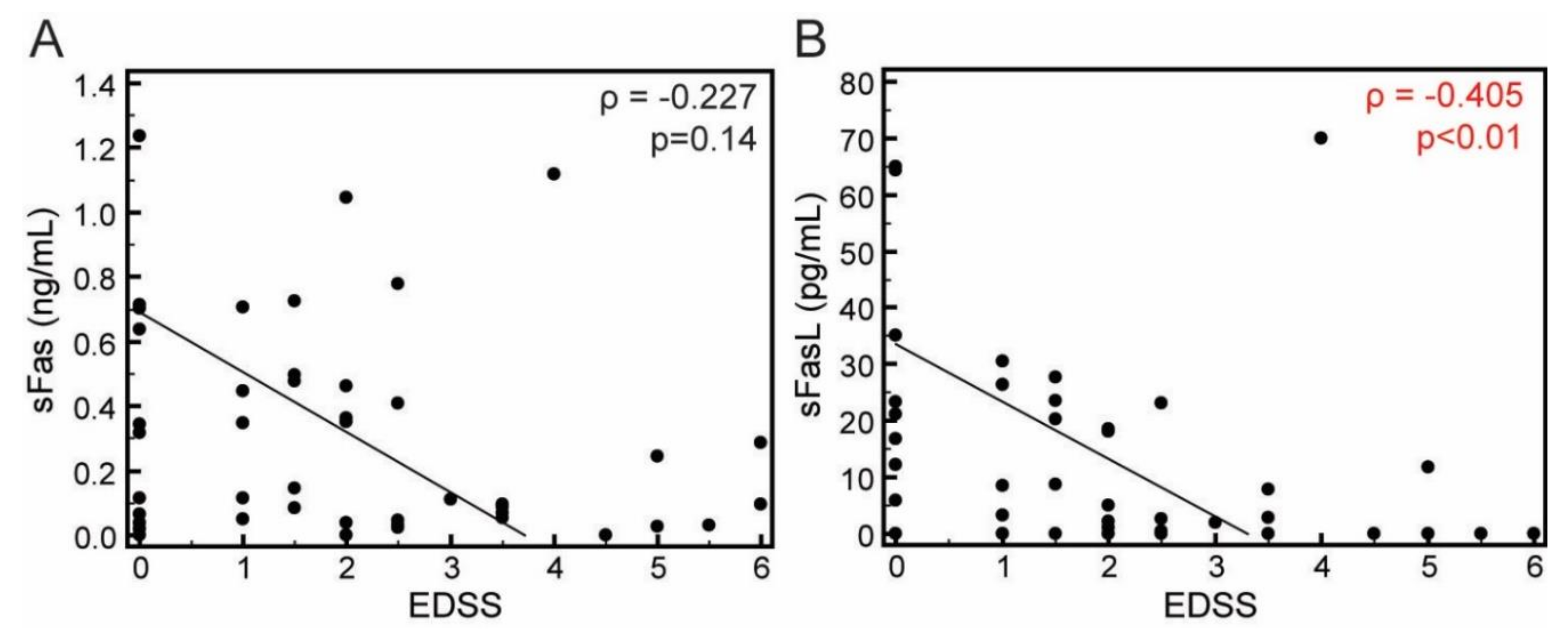
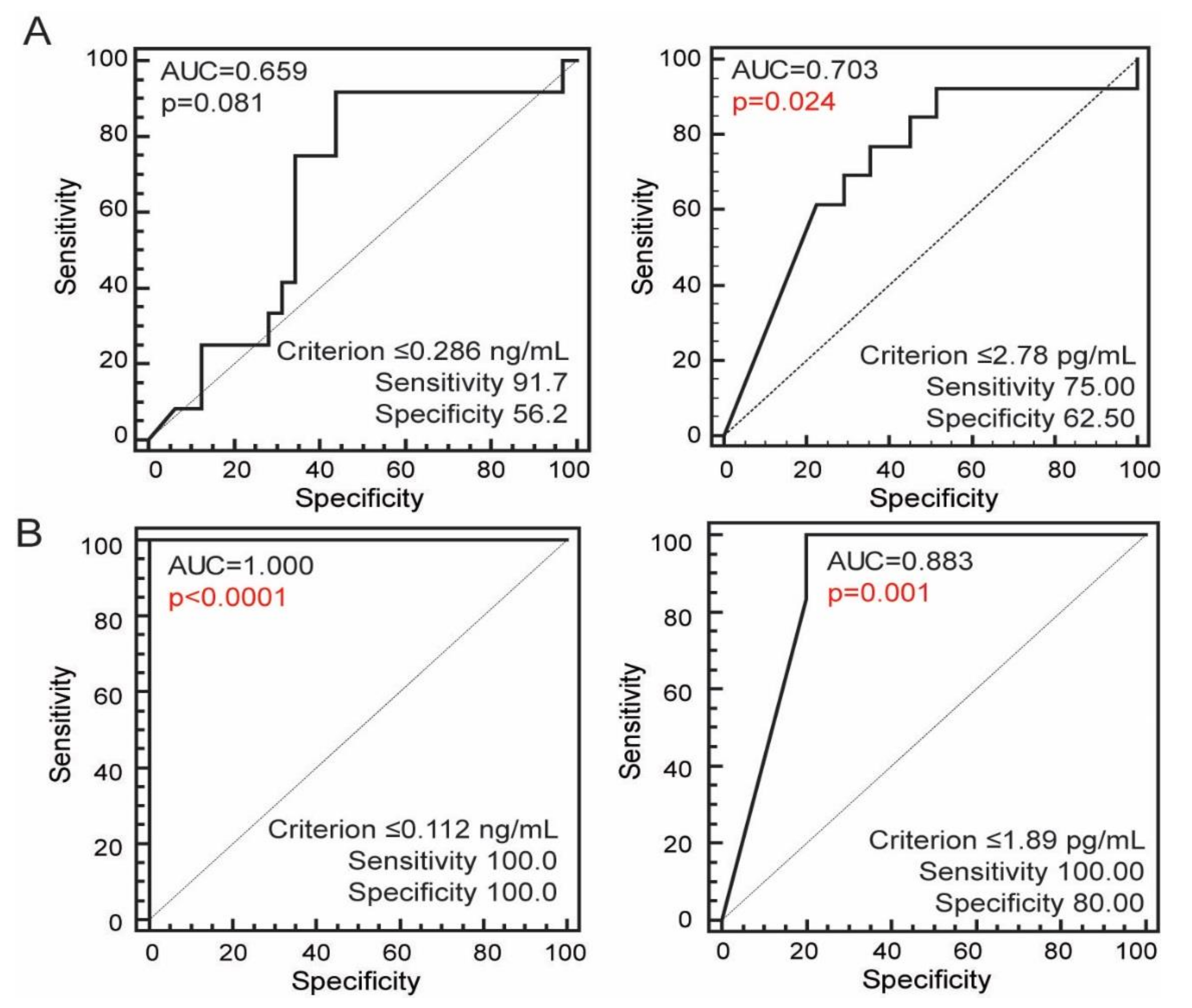
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Dendrou, C.A.; Fugger, L.; Friese, M.A. Immunopathology of multiple sclerosis. Nat. Rev. Immunol. 2015, 15, 545–558. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, H.; Williamson, D.; Ashley-Koch, A. HLA-DR15 Haplotype and Multiple Sclerosis: A HuGE Review. Am. J. Epidemiol. 2007, 165, 1097–1109. [Google Scholar] [CrossRef] [PubMed]
- Owens, G.P.; Bennett, J.L.; Lassmann, H.; O’Connor, K.C.; Bs, A.M.R.; Bs, A.S.; Lam, C.; Yu, X.; Birlea, M.; DuPree, C.; et al. Antibodies produced by clonally expanded plasma cells in multiple sclerosis cerebrospinal fluid. Ann. Neurol. 2009, 65, 639–649. [Google Scholar] [CrossRef] [PubMed]
- Brettschneider, J.; Tumani, H.; Kiechle, U.; Muche, R.; Richards, G.; Lehmensiek, V.; Ludolph, A.C.; Otto, M. IgG Antibodies against Measles, Rubella, and Varicella Zoster Virus Predict Conversion to Multiple Sclerosis in Clinically Isolated Syndrome. PLoS ONE 2009, 4, e7638. [Google Scholar] [CrossRef] [PubMed]
- Buljevac, D.; van Doornum, G.J.; Flach, H.Z.; Groen, J.; Osterhaus, A.D.; Hop, W.; van Doorn, P.A.; van der Meché, F.G.; Hintzen, R.Q. Epstein-Barr virus and disease activity in multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 2005, 76, 1377–1381. [Google Scholar] [CrossRef]
- Belogurov, A.A.; Kurkova, I.N.; Friboulet, A.; Thomas, D.; Misikov, V.K.; Zakharova, M.Y.; Suchkov, S.V.; Kotov, S.V.; Alehin, A.I.; Avalle, B.; et al. Recognition and Degradation of Myelin Basic Protein Peptides by Serum Autoantibodies: Novel Biomarker for Multiple Sclerosis. J. Immunol. 2008, 180, 1258–1267. [Google Scholar] [CrossRef] [PubMed]
- Bivona, G.; Gambino, C.M.; Iacolino, G.; Ciaccio, M. Vitamin D and the nervous system. Neurol. Res. 2019, 41, 827–835. [Google Scholar] [CrossRef]
- Kavanaugh, A.F.; Solomon, D.H. American College of Rheumatology Ad Hoc Committee on Immunologic Testing Guidelines. Guidelines for immunologic laboratory testing in the rheumatic diseases: Anti-DNA antibody tests. Arthritis Rheum. 2002, 47, 546–555. [Google Scholar] [CrossRef]
- Dore-Duffy, P.; Donaldson, J.O.; Rothman, B.L.; Zurier, R.B. Antinuclear Antibodies in Multiple Sclerosis. Arch. Neurol. 1982, 39, 504–506. [Google Scholar] [CrossRef]
- Szmyrka-Kaczmarek, M.; Pokryszko-Dragan, A.; Pawlik, B.; Gruszka, E.; Korman, L.; Podemski, R.; Wiland, P.; Szechinski, J. Antinuclear and antiphospholipid antibodies in patients with multiple sclerosis. Lupus 2011, 21, 412–420. [Google Scholar] [CrossRef] [PubMed]
- Barned, S.; Goodman, A.D.; Mattson, D.H. Frequency of anti-nuclear antibodies in multiple sclerosis. Neurology 1995, 45, 384–385. [Google Scholar] [CrossRef] [PubMed]
- Adamec, I.; Bošković, M.; Škvorc, A.; Posavec, V.; Radmilović, M.; Gabelić, T.; Habek, M. Do we need broad immunological work-up in all patients with CIS? J. Neurol. Sci. 2012, 315, 86–88. [Google Scholar] [CrossRef] [PubMed]
- Collard, R.C.; Koehler, R.P.; Mattson, D.H. Frequency and significance of antinuclear antibodies in multiple sclerosis. Neurology 1997, 49, 857–861. [Google Scholar] [CrossRef] [PubMed]
- Antigüedad, A.; Ruiz, J.; Mendibe, M.M.; Zarranz, J.J. Antinuclear antibodies in multiple sclerosis. Neurologia 1997, 12, 245–248. [Google Scholar] [PubMed]
- Negrotto, L.; Tur, C.; Tintoré, M.; Arrambide, G.; Sastre-Garriga, J.; Río, J.; Comabella, M.; Nos, C.; Galán, I.; Vidal-Jordana, A.; et al. Should we systematically test patients with clinically isolated syndrome for auto-antibodies? Mult. Scler. J. 2015, 21, 1802–1810. [Google Scholar] [CrossRef]
- Fujii, T.; Yamasaki, R.; Miyachi, Y.; Nagata, S.; Maimaitijiang, G.; Nakamura, Y.; Shinoda, K.; Matsushita, T.; Isobe, N.; Kira, J.-I. Central nervous system-specific antinuclear antibodies in patients with multiple sclerosis. J. Neurol. Sci. 2020, 409, 116619. [Google Scholar] [CrossRef]
- Weinshenker, B.G.; Wingerchuk, D.M. Neuromyelitis Spectrum Disorders. Mayo Clin. Proc. 2017, 92, 663–679. [Google Scholar] [CrossRef]
- Chen, C.; Xiaobo, S.; Yuge, W.; Yaqing, S.; Ling, F.; Lisheng, P.; Zhengqi, L.; Wei, Q. Multiple Autoantibodies and Neuromyelitis Optica Spectrum Disorders. Neuroimmunomodulation 2016, 23, 151–156. [Google Scholar] [CrossRef]
- Masuda, H.; Mori, M.; Uzawa, A.; Muto, M.; Uchida, T.; Kuwabara, S. Serum antinuclear antibody may be associated with less severe disease activity in neuromyelitis optica. Eur. J. Neurol. 2016, 23, 276–281. [Google Scholar] [CrossRef]
- Bai, Y.; Tong, Y.; Liu, Y.; Hu, H. Self-dsDNA in the pathogenesis of systemic lupus erythematosus. Clin. Exp. Immunol. 2018, 191, 1–10. [Google Scholar] [CrossRef]
- Smeenk, R.J. Antinuclear antibodies: Cause of disease or caused by disease? Rheumatology 2000, 39, 581–584. [Google Scholar] [CrossRef] [PubMed]
- Lleo, A.; Selmi, C.; Invernizzi, P.; Podda, M.; Gershwin, M.E. The consequences of apoptosis in autoimmunity. J. Autoimmun. 2008, 31, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Yonehara, S.; Ishii, A.; Yonehara, M. A cell-killing monoclonal antibody (anti-Fas) to a cell surface antigen co-downregulated with the receptor of tumor necrosis factor. J. Exp. Med. 1989, 169, 1747–1756. [Google Scholar] [CrossRef] [PubMed]
- Denault, J.B.; Salvesen, G.S. Caspases: Keys in the ignition of cell death. Chem. Rev. 2002, 102, 4489–5000. [Google Scholar] [CrossRef] [PubMed]
- Askenasy, N.; Yolcu, E.S.; Yaniv, I.; Shirwan, H. Induction of tolerance using Fas ligand: A double-edged immunomodulator. Blood 2005, 105, 1396–1404. [Google Scholar] [CrossRef]
- French, L.E.; Tschopp, J. Protein-based therapeutic approaches targeting death receptors. Cell Death Differ. 2003, 10, 117–123. [Google Scholar] [CrossRef]
- Volpe, E.; Sambucci, M.; Battistini, L.; Borsellino, G. Fas–Fas Ligand: Checkpoint of T Cell Functions in Multiple Sclerosis. Front. Immunol. 2016, 7, 382. [Google Scholar] [CrossRef]
- Griffith, T.S.; Brunner, T.; Fletcher, S.M.; Green, D.R.; Ferguson, T.A. Fas Ligand-Induced Apoptosis as a Mechanism of Immune Privilege. Science 1995, 270, 1189–1192. [Google Scholar] [CrossRef]
- Izquierdo, J.M.; Majós, N.; Bonnal, S.; Martínez, C.; Castelo, R.; Guigó, R.; Bilbao, D.; Valcárcel, J. Regulation of Fas Alternative Splicing by Antagonistic Effects of TIA-1 and PTB on Exon Definition. Mol. Cell 2005, 19, 475–484. [Google Scholar] [CrossRef]
- Cascino, I.; Papoff, G.; Eramo, A.; Ruberti, G. Soluble Fas/Apo-1 splicing variants and apoptosis. Front. Biosci. 1996, 1, 12–18. [Google Scholar]
- Guégan, J.P.; Legembre, P. Nonapoptotic functions of Fas/CD95 in the immune response. FEBS J. 2018, 285, 809–827. [Google Scholar] [CrossRef] [PubMed]
- Macchi, B.; Marino-Merlo, F.; Nocentini, U.; Pisani, V.; Cuzzocrea, S.; Grelli, S.; Mastino, A. Role of inflammation and apoptosis in multiple sclerosis: Comparative analysis between the periphery and the central nervous system. J. Neuroimmunol. 2015, 287, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Lopatinskaya, L.; Zwemmer, J.; Uitdehaag, B.; Lucas, K.; Polman, C.; Nagelkerken, L. Mediators of apoptosis Fas and FasL predict disability progression in multiple sclerosis over a period of 10 years. Mult. Scler. J. 2006, 12, 704–709. [Google Scholar] [CrossRef] [PubMed]
- Boylan, M.T.; Crockard, A.; McDonnell, G.V.; McMillan, S.A.; Hawkins, S.A. Serum and cerebrospinal fluid soluble Fas levels in clinical subgroups of multiple sclerosis. Immunol. Lett. 2001, 78, 183–187. [Google Scholar] [CrossRef]
- Thompson, A.J.; Banwell, B.L.; Barkhof, F.; Carroll, W.M.; Coetzee, T.; Comi, G.; Correale, J.; Fazekas, F.; Filippi, M.; Freedman, M.S.; et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018, 17, 162–173. [Google Scholar] [CrossRef]
- Becker, D.E. Basic and clinical pharmacology of glucocorticosteroids. Anesth Prog. 2013, 60, 25–32. [Google Scholar] [CrossRef]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef]
- Bellone, M.; Iezzi, G.; Rovere, P.; Galati, G.; Ronchetti, A.; Protti, M.P.; Davoust, J.; Rugarli, C.; Manfredi, A.A. Processing of engulfed apoptotic bodies yields T cell epitopes. J. Immunol. 1997, 159, 5391–5399. [Google Scholar]
- Rinta, S.; Kuusisto, H.; Raunio, M.; Paalavuo, R.; Levula, M.; Lehtimäki, T.; Elovaara, I. Apoptosis-related molecules in blood in multiple sclerosis. J. Neuroimmunol. 2008, 205, 135–141. [Google Scholar] [CrossRef]
- Nozawa, K.; Kayagaki, N.; Tokano, Y.; Yagita, H.; Okumura, K.; Hasimoto, H. Soluble Fas (APO-1, CD95) and soluble Fas ligand in rheumatic diseases. Arthritis Rheum. 1997, 40, 1126–1129. [Google Scholar] [CrossRef]
- Yoshimura, C.; Nomura, S.; Nagahama, M.; Ozaki, Y.; Kagawa, H.; Fukuhara, S. Plasma-soluble Fas (APO-1, CD95) and soluble Fas ligand in immune thrombocytopenic purpura. Eur. J. Haematol. 2000, 64, 219–224. [Google Scholar] [CrossRef]
- Endo, S.; Inoue, Y.; Fujino, Y.; Yamada, Y.; Sato, N.; Wakabayashi, G.; Sakamoto, T.; Ishikura, H.; Tanaka, T.; Inada, K.; et al. Soluble Fas and soluble Fas L levels in patients with acute pancreatitis. Res. Commun. Mol. Pathol. Pharmacol. 2000, 108, 179–186. [Google Scholar] [PubMed]
- Tinazzi, E.; Puccetti, A.; Gerli, R.; Rigo, A.; Migliorini, P.; Simeoni, S.; Beri, R.; Dolcino, M.; Martinelli, N.; Corrocher, R.; et al. Serum DNase I, soluble Fas/FasL levels and cell surface Fas expression in patients with SLE: A possible explanation for the lack of efficacy of hrDNase I treatment. Int. Immunol. 2009, 21, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Liphaus, B.L.; Kiss, M.H.B.; Carrasco, S.; Goldenstein-Schainberg, C.; Palmeira, P.; Carneiro-Sampaio, M. Increased serum sFas, sTRAIL, and reduced sFasL in juvenile-onset systemic lupus erythematosus. Clin. Rheumatol. 2017, 36, 2847–2852. [Google Scholar] [CrossRef] [PubMed]
| Age (years, male/female) | 38.43 ± 10.25 (33.91 ± 9.72/40.12 ± 10.07) | N = 44 |
| Disease duration (years, male/female) | 6 [1–10](5.5 [1.5–7.5]/6.5 [1–13]) * | N = 44 |
| Number of experienced relapses (male/female) | 3 [2–4](3.5 [2–5]/3 [1.5–4.0]) * | N = 44 |
| Number of relapses in first two years of the disease (male/female) | 1 [1–2](2 [1.0–2.5]/1 [1–2]) * | N = 32 |
| Annualized relapse rate (male/female) | 0.47 [0.33–1.00] (0.75 [0.44–1.25]/0.42 [0.28–0.71]) * | N = 35 |
| EDSS (male/female) | 2 [0.50–3.25] (2.0 [1.25–3.00]/1.75 [0.00–3.25]) * | N = 44 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sremec, J.; Tomasović, S.; Tomić Sremec, N.; Šućur, A.; Košćak Lukač, J.; Bačić Baronica, K.; Grčević, D.; Kovačić, N. Elevated Concentrations of Soluble Fas and FasL in Multiple Sclerosis Patients with Antinuclear Antibodies. J. Clin. Med. 2020, 9, 3845. https://doi.org/10.3390/jcm9123845
Sremec J, Tomasović S, Tomić Sremec N, Šućur A, Košćak Lukač J, Bačić Baronica K, Grčević D, Kovačić N. Elevated Concentrations of Soluble Fas and FasL in Multiple Sclerosis Patients with Antinuclear Antibodies. Journal of Clinical Medicine. 2020; 9(12):3845. https://doi.org/10.3390/jcm9123845
Chicago/Turabian StyleSremec, Josip, Sanja Tomasović, Nada Tomić Sremec, Alan Šućur, Jelena Košćak Lukač, Koraljka Bačić Baronica, Danka Grčević, and Nataša Kovačić. 2020. "Elevated Concentrations of Soluble Fas and FasL in Multiple Sclerosis Patients with Antinuclear Antibodies" Journal of Clinical Medicine 9, no. 12: 3845. https://doi.org/10.3390/jcm9123845
APA StyleSremec, J., Tomasović, S., Tomić Sremec, N., Šućur, A., Košćak Lukač, J., Bačić Baronica, K., Grčević, D., & Kovačić, N. (2020). Elevated Concentrations of Soluble Fas and FasL in Multiple Sclerosis Patients with Antinuclear Antibodies. Journal of Clinical Medicine, 9(12), 3845. https://doi.org/10.3390/jcm9123845




