Best Procedure for the Management of Common Bile Duct Stones via the Papilla: Literature Review and Analysis of Procedural Efficacy and Safety
Abstract
1. Introduction
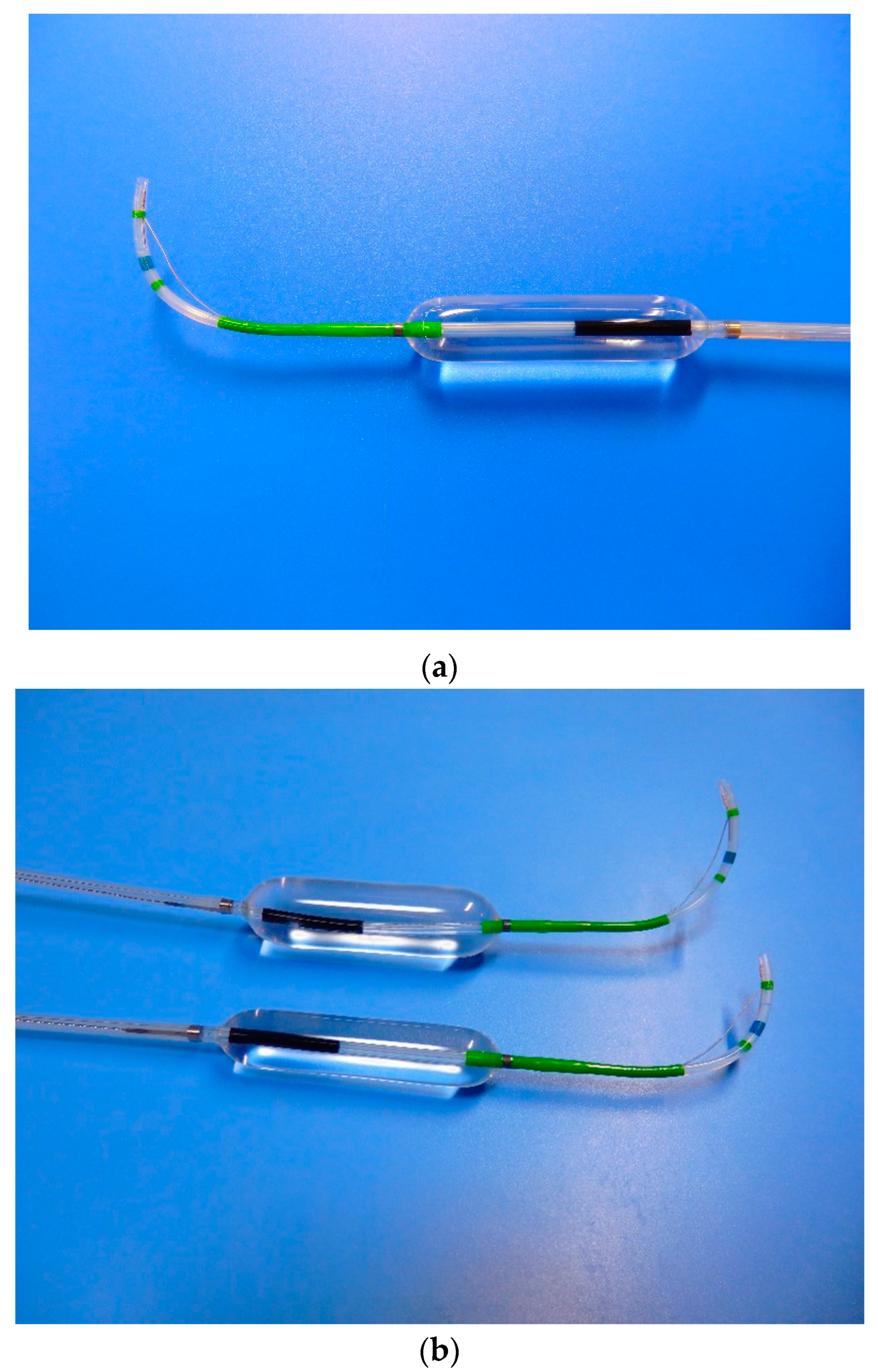
1.1. Definitions of Endoscopic Techniques
1.2. Study Selection and Data Extraction
1.3. Statistical Analyses
2. Results
2.1. Removal of Small CBDS
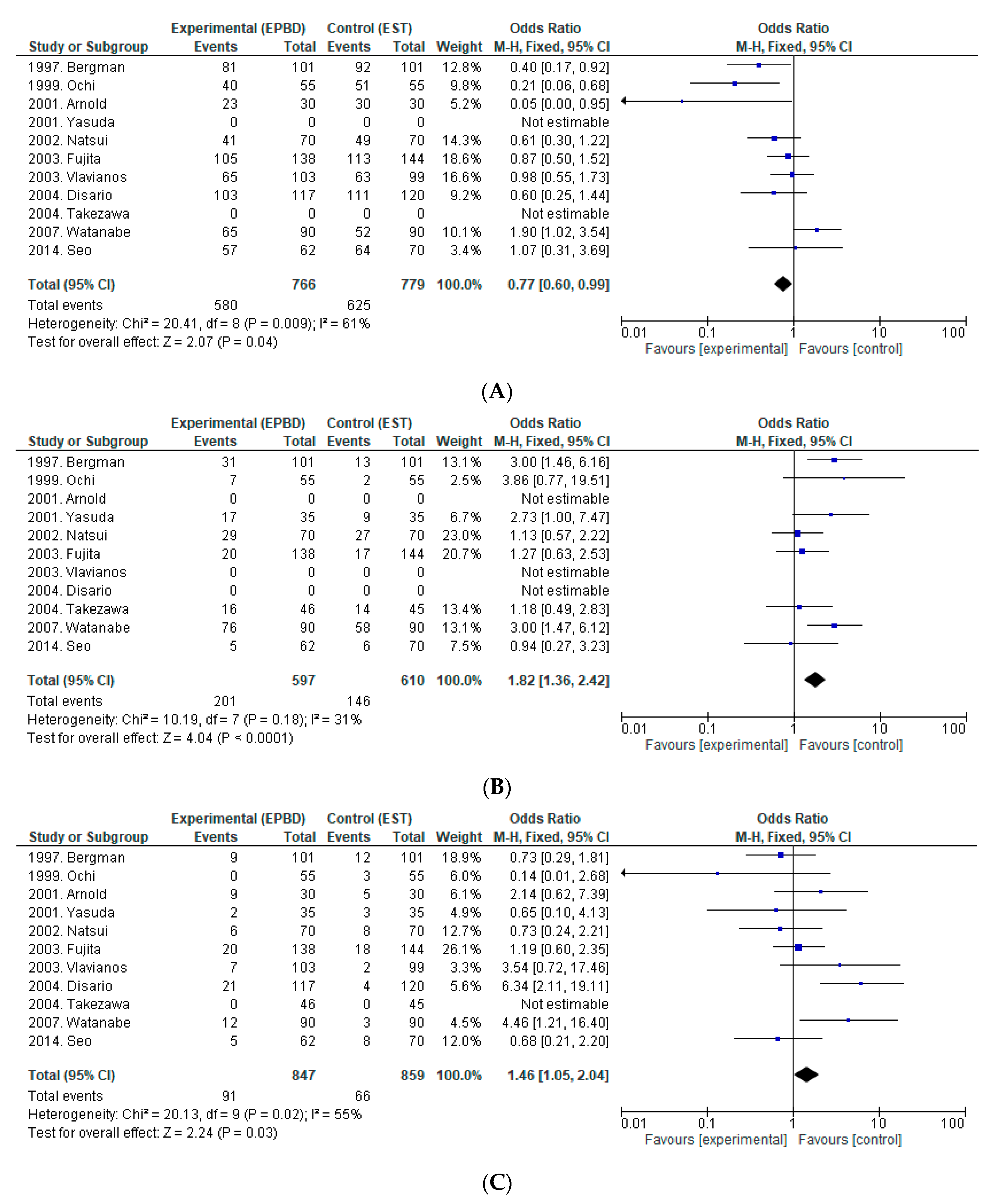
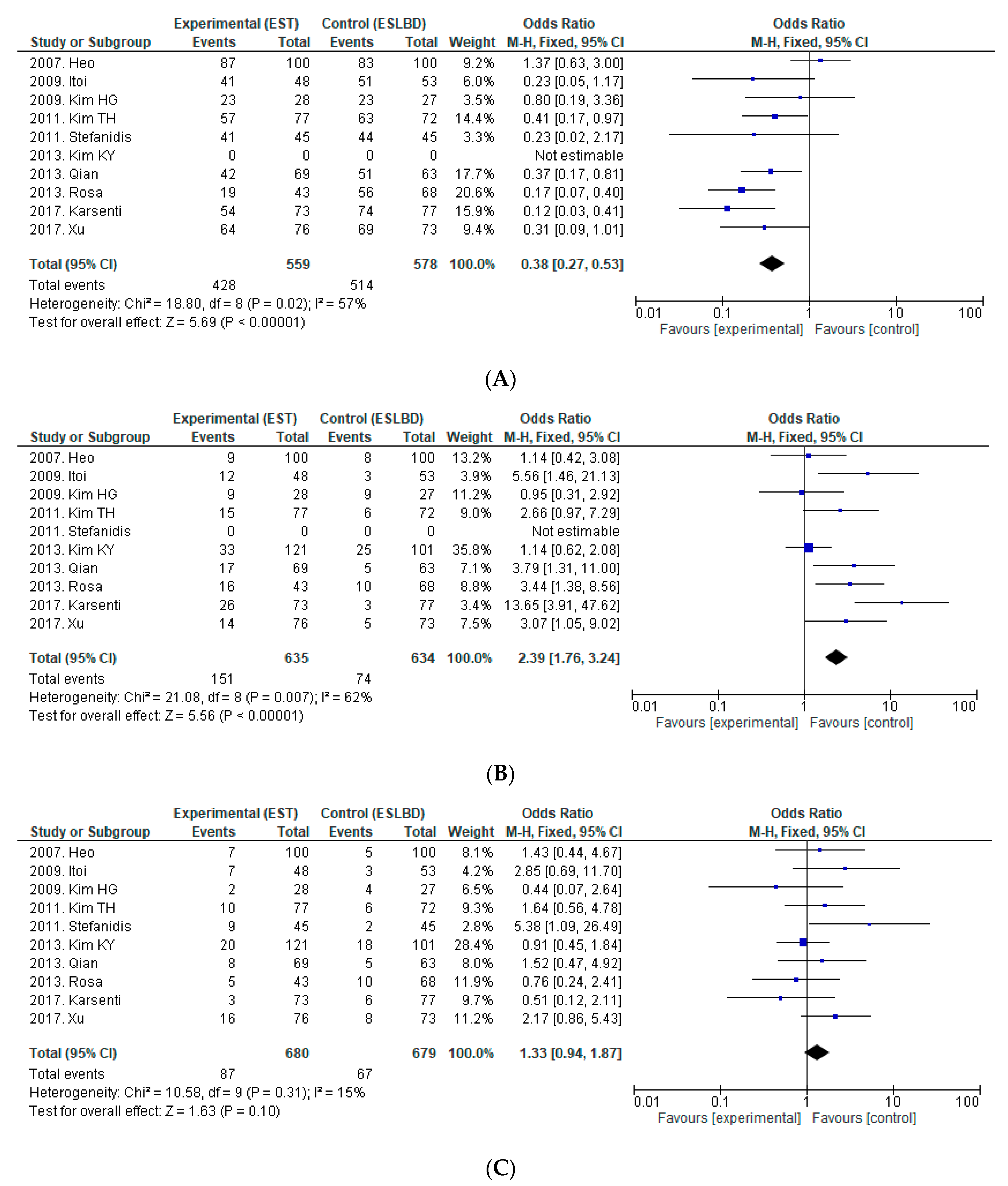
2.2. EST vs. EPBD
2.3. EST vs. ESBD
2.4. Removal of Large CBDS
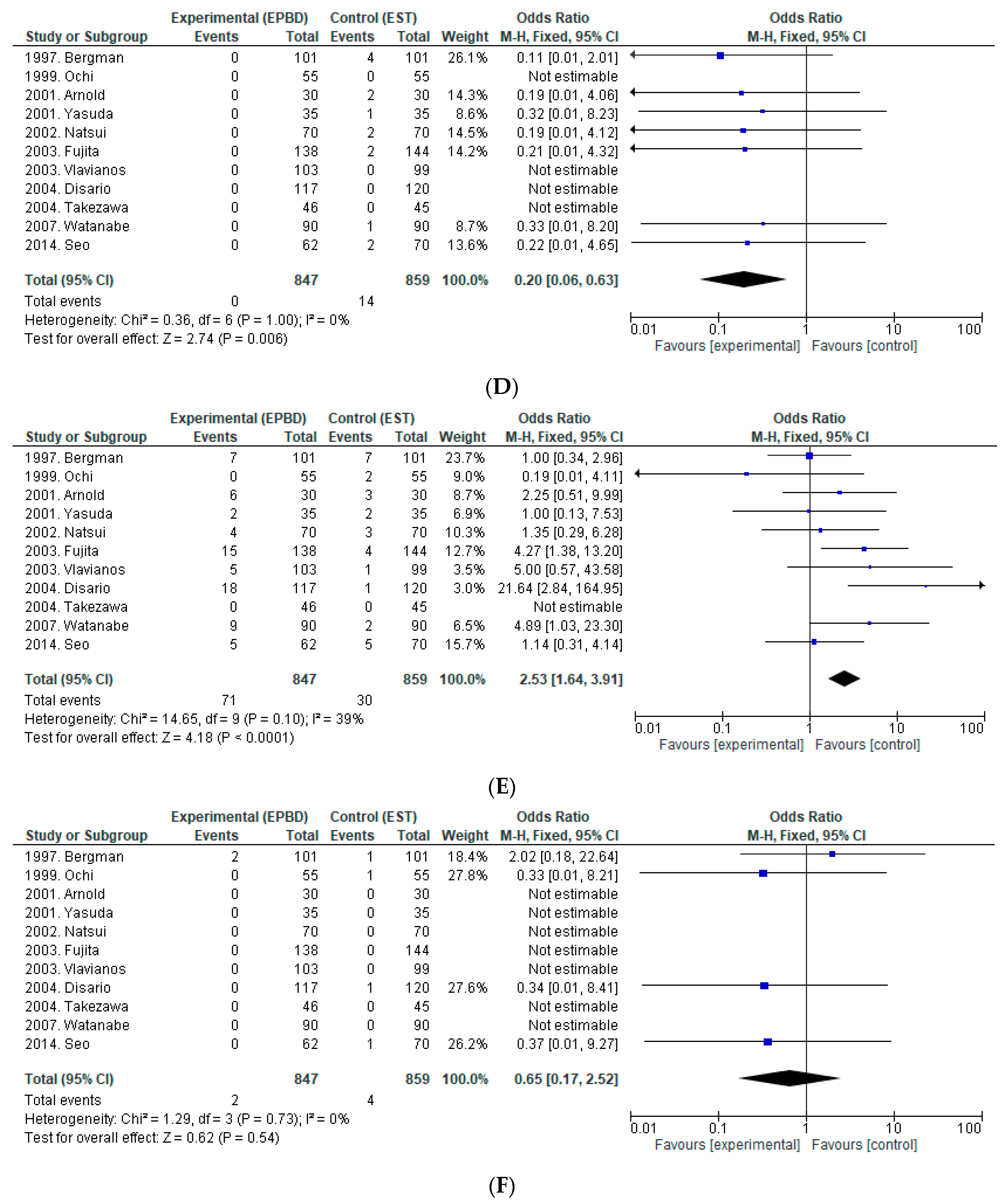
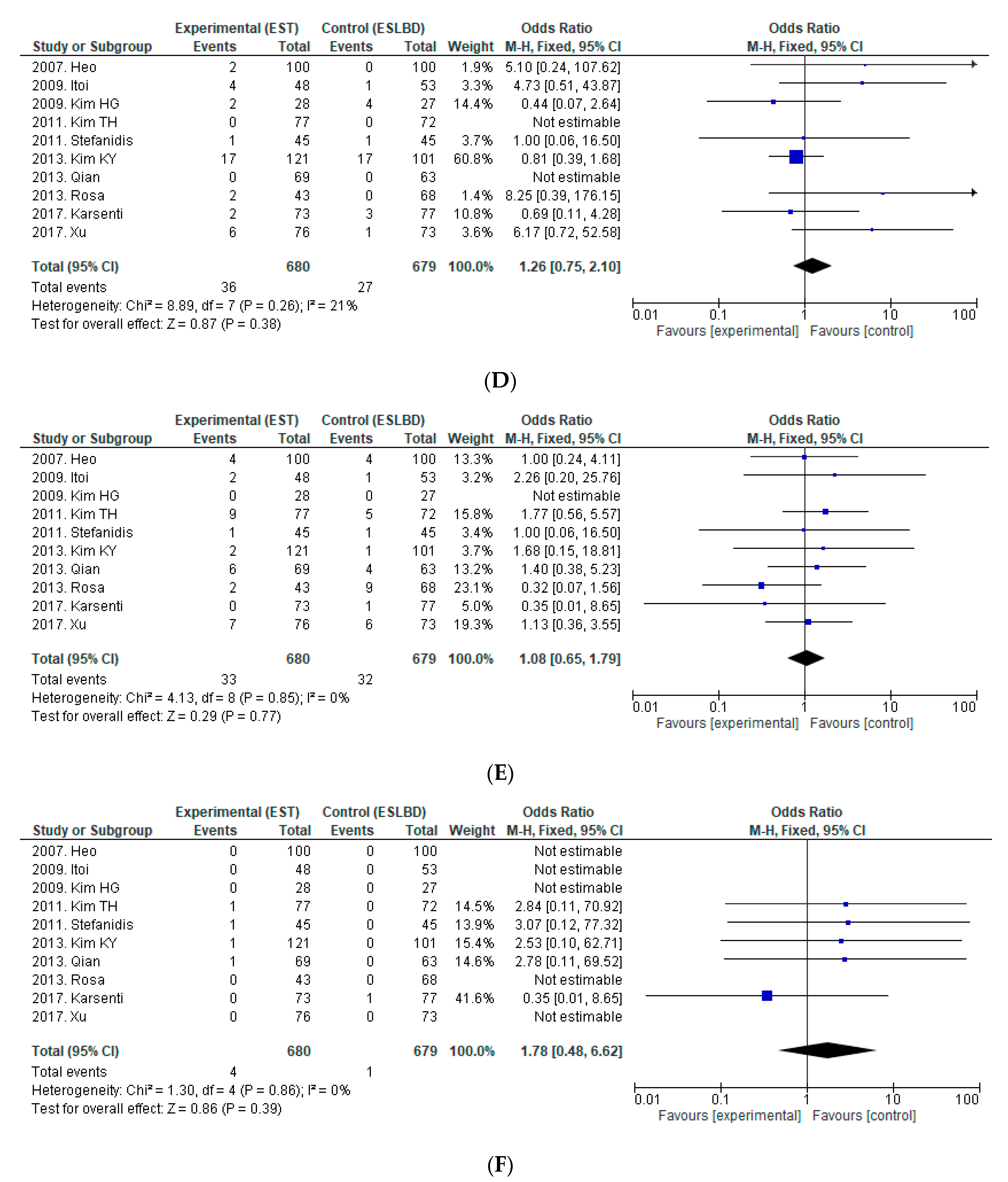
2.5. EST vs. ESLBD
2.6. EST vs. EPLBD
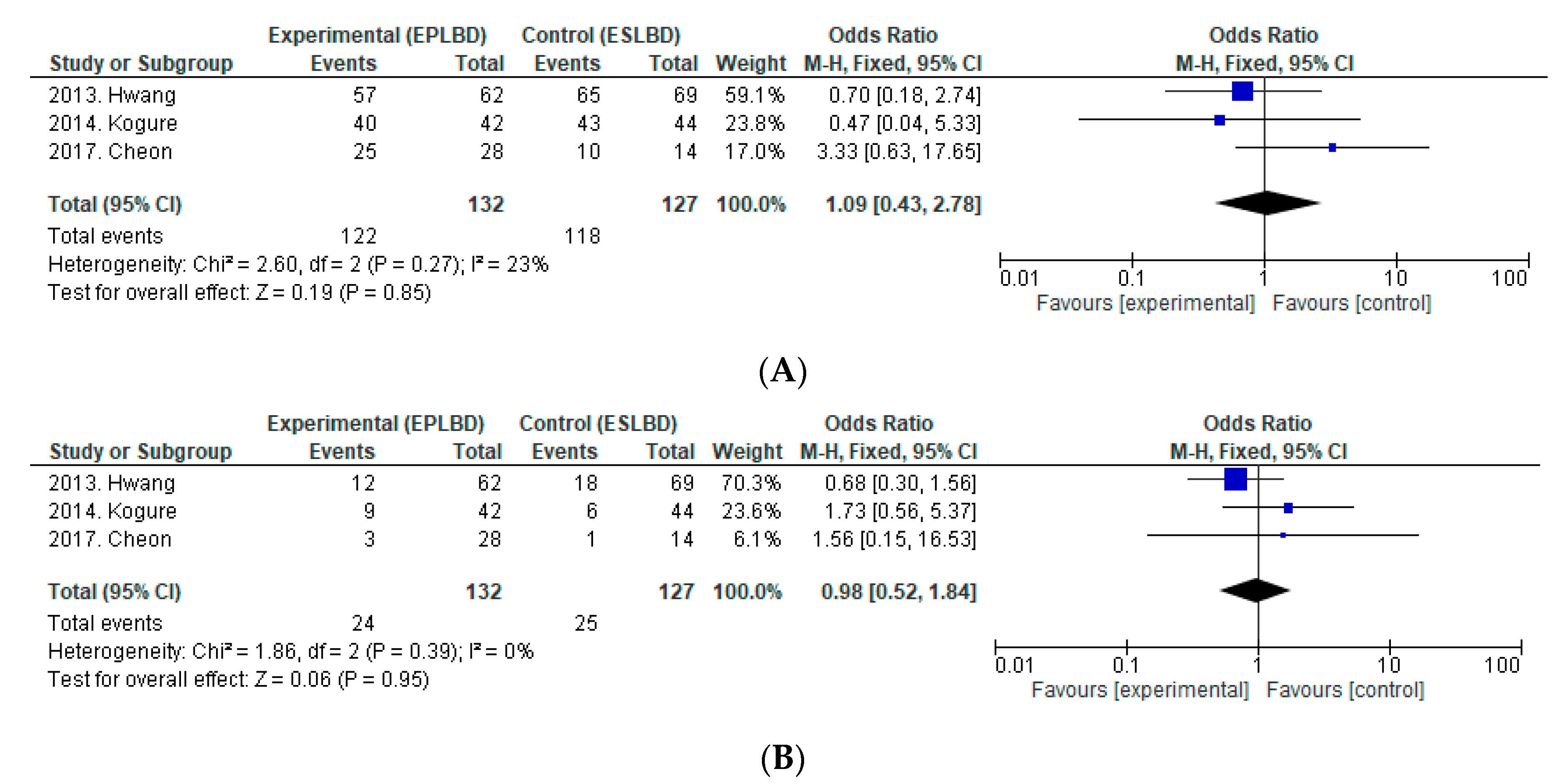
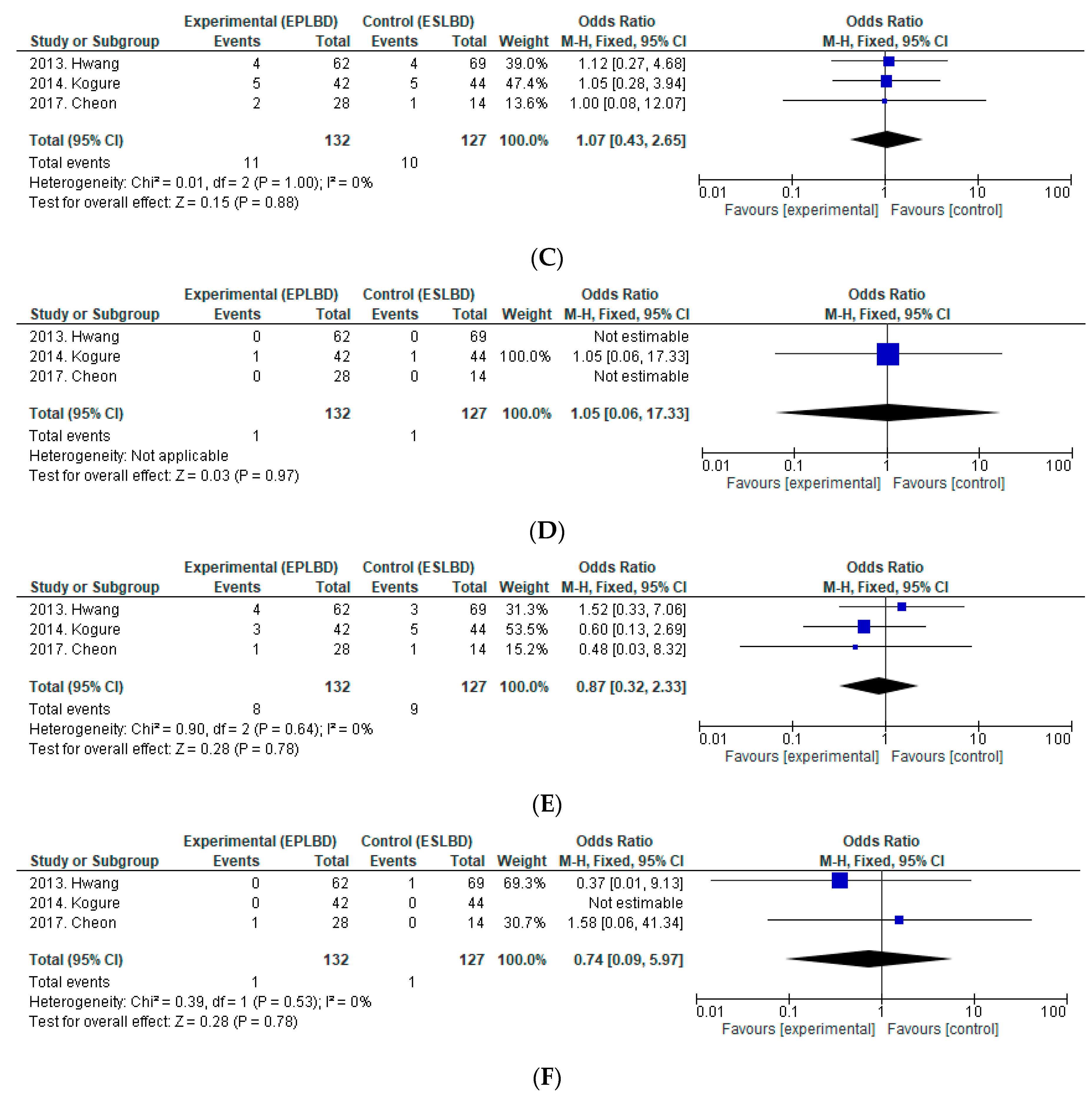
2.7. EPLBD vs. ESLBD
3. Discussion
3.1. Small CBDS
3.2. Large CBDS
4. Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Ethical Issues
Availability of Data and Material
Abbreviations
| CBDS | common bile duct stone |
| EST | endoscopic sphincterotomy |
| EPBD | endoscopic papillary balloon dilation |
| ESBD | EST followed by balloon dilation |
| EPLBD | endoscopic papillary large balloon dilation |
| ESLBD | EST followed by large balloon dilation |
| ML | mechanical lithotripsy |
| PEP | post-ERCP pancreatitis |
References
- Kawai, K. Preliminary report on endoscopic papillotomy. J. Kyoto Pref. Univ. Med. 1973, 82, 353–355. [Google Scholar]
- Staritz, M.; Ewe, K.; Meyer zum Büschenfelde, K.H. Endoscopic papillary dilation (EPD) for the treatment of common bile duct stones and papillary stenosis. Endoscopy 1983, 15 (Suppl. 1), 197–198. [Google Scholar] [CrossRef] [PubMed]
- Isayama, H.; Komatsu, Y.; Inoue, Y.; Toda, N.; Shiratori, Y.; Tsujino, T.; Yamada, H.; Saitou, K.; Kawabe, T.; Omata, M. Preserved function of the Oddi sphincter after endoscopic papillary balloon dilation. Hepato-Gastroenterology 2003, 50, 1787–1791. [Google Scholar] [PubMed]
- Fujisawa, T.; Kagawa, K.; Hisatomi, K.; Kubota, K.; Nakajima, A.; Matsuhashi, N. Is endoscopic papillary balloon dilatation really a risk factor for post-ERCP pancreatitis? World J. Gastroenterol. 2016, 22, 5909–5916. [Google Scholar] [CrossRef] [PubMed]
- Disario, J.A.; Freeman, M.L.; Bjorkman, D.J.; Macmathuna, P.; Petersen, B.T.; Jaffe, P.E.; Morales, T.G.; Hixson, L.J.; Sherman, S.; Lehman, G.A.; et al. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology 2004, 127, 1291–1299. [Google Scholar] [CrossRef]
- Tsujino, T.; Kawabe, T.; Komatsu, Y.; Yoshida, H.; Isayama, H.; Sasaki, T.; Kogure, H.; Togawa, O.; Arizumi, T.; Matsubara, S.; et al. Endoscopic papillary balloon dilation for bile duct stone: Immediate and long-term outcomes in 1000 patients. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2007, 5, 130–137. [Google Scholar] [CrossRef]
- Fujita, N.; Maguchi, H.; Komatsu, Y.; Yasuda, I.; Hasebe, O.; Igarashi, Y.; Murakami, A.; Mukai, H.; Fujii, T.; Yamao, K.; et al. Endoscopic sphincterotomy and endoscopic papillary balloon dilatation for bile duct stones: A prospective randomized controlled multicenter trial. Gastrointest. Endosc. 2003, 57, 151–155. [Google Scholar] [CrossRef]
- Ishii, S.; Fujisawa, T.; Ushio, M.; Takahashi, S.; Yamagata, W.; Takasaki, Y.; Suzuki, A.; Okawa, Y.; Ochiai, K.; Tomishima, K.; et al. Evaluation of the safety and efficacy of minimal endoscopic sphincterotomy followed by papillary balloon dilation for the removal of common bile duct stones. Saudi J. Gastroenterol. 2020. [Google Scholar] [CrossRef]
- Ersoz, G.; Tekesin, O.; Ozutemiz, A.O.; Gunsar, F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest. Endosc. 2003, 57, 156–159. [Google Scholar] [CrossRef]
- Bo, Q.J.; Hua, X.L.; Min, C.T.; Gen, G.L.; Mei, Y.Y.; Sheng, L.H. Small Endoscopic Sphincterotomy plus Large-Balloon Dilation for Removal of Large Common Bile Duct Stones during ERCP. Pak. J. Med. Sci. 2013, 29, 907–912. [Google Scholar] [CrossRef]
- Karsenti, D.; Coron, E.; Vanbiervliet, G.; Privat, J.; Kull, E.; Bichard, P.; Perrot, B.; Quentin, V.; Duriez, A.; Cholet, F.; et al. Complete endoscopic sphincterotomy with vs. without large-balloon dilation for the removal of large bile duct stones: Randomized multicenter study. Endoscopy 2017, 49, 968–976. [Google Scholar] [CrossRef] [PubMed]
- Chan, H.H.; Lai, K.H.; Lin, C.K.; Tsai, W.L.; Wang, E.M.; Hsu, P.I.; Chen, W.C.; Yu, H.C.; Wang, H.M.; Tsay, F.W.; et al. Endoscopic papillary large balloon dilation alone without sphincterotomy for the treatment of large common bile duct stones. BMC Gastroenterol. 2011, 11, 69. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.; Ki, S.H.; Lee, D.H.; Lee, J.I.; Lee, J.W.; Kwon, K.S.; Kim, H.G.; Shin, Y.W.; Kim, Y.S. Endoscopic large-balloon sphincteroplasty without preceding sphincterotomy for the removal of large bile duct stones: A preliminary study. Gastrointest. Endosc. 2009, 70, 915–922. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.C.; He, L.; Zhou, D.C.; Geng, X.P.; Pan, F.M. Meta-analysis comparison of endoscopic papillary balloon dilatation and endoscopic sphincteropapillotomy. World J. Gastroenterol. 2013, 19, 3883–3891. [Google Scholar] [CrossRef] [PubMed]
- Jin, P.P.; Cheng, J.F.; Liu, D.; Mei, M.; Xu, Z.Q.; Sun, L.M. Endoscopic papillary large balloon dilation vs endoscopic sphincterotomy for retrieval of common bile duct stones: A meta-analysis. World J. Gastroenterol. 2014, 20, 5548–5556. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Kyaw, M.H.; Tse, Y.K.; Lau, J.Y. Endoscopic sphincterotomy with large balloon dilation versus endoscopic sphincterotomy for bile duct stones: A systematic review and meta-analysis. Biomed Res. Int. 2015, 2015, 673103. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Pang, Q.; Zhang, X.; Dong, H.; Guo, R.; Zhai, H.; Dong, Y.; Jia, X. Dilation-assisted stone extraction: An alternative method for removal of common bile duct stones. Dig. Dis. Sci. 2014, 59, 857–864. [Google Scholar] [CrossRef]
- Lin, C.K.; Lai, K.H.; Chan, H.H.; Tsai, W.L.; Wang, E.M.; Wei, M.C.; Fu, M.T.; Lo, C.C.; Hsu, P.I.; Lo, G.H. Endoscopic balloon dilatation is a safe method in the management of common bile duct stones. Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver 2004, 36, 68–72. [Google Scholar] [CrossRef]
- Teoh, A.Y.; Cheung, F.K.; Hu, B.; Pan, Y.M.; Lai, L.H.; Chiu, P.W.; Wong, S.K.; Chan, F.K.; Lau, J.Y. Randomized trial of endoscopic sphincterotomy with balloon dilation versus endoscopic sphincterotomy alone for removal of bile duct stones. Gastroenterology 2013, 144, 341–345.e1. [Google Scholar] [CrossRef]
- Guo, Y.; Lei, S.; Gong, W.; Gu, H.; Li, M.; Liu, S.; Zhi, F. A Preliminary Comparison of Endoscopic Sphincterotomy, Endoscopic Papillary Large Balloon Dilation, and Combination of the Two in Endoscopic Choledocholithiasis Treatment. Med. Sci. Monit. 2015, 21, 2607–2612. [Google Scholar] [CrossRef]
- Oh, M.J.; Kim, T.N. Prospective comparative study of endoscopic papillary large balloon dilation and endoscopic sphincterotomy for removal of large bile duct stones in patients above 45 years of age. Scand. J. Gastroenterol. 2012, 47, 1071–1077. [Google Scholar] [CrossRef] [PubMed]
- Fu, B.Q.; Xu, Y.P.; Tao, L.S.; Yao, J.; Zhou, C.S. Endoscopic papillary balloon intermittent dilatation and endoscopic sphincterotomy for bile duct stones. World J. Gastroenterol. 2013, 19, 2425–2432. [Google Scholar] [CrossRef] [PubMed]
- Bergman, J.J.; Rauws, E.A.; Fockens, P.; van Berkel, A.M.; Bossuyt, P.M.; Tijssen, J.G.; Tytgat, G.N.; Huibregtse, K. Randomised trial of endoscopic balloon dilation versus endoscopic sphincterotomy for removal of bileduct stones. Lancet 1997, 349, 1124–1129. [Google Scholar] [CrossRef]
- Ochi, Y.; Mukawa, K.; Kiyosawa, K.; Akamatsu, T. Comparing the treatment outcomes of endoscopic papillary dilation and endoscopic sphincterotomy for removal of bile duct stones. J. Gastroenterol. Hepatol. 1999, 14, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Arnold, J.C.; Benz, C.; Martin, W.R.; Adamek, H.E.; Riemann, J.F. Endoscopic papillary balloon dilation vs. sphincterotomy for removal of common bile duct stones: A prospective randomized pilot study. Endoscopy 2001, 33, 563–567. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, I.; Tomita, E.; Enya, M.; Kato, T.; Moriwaki, H. Can endoscopic papillary balloon dilation really preserve sphincter of Oddi function? Gut 2001, 49, 686–691. [Google Scholar] [CrossRef]
- Natsui, M.; Narisawa, R.; Motoyama, H.; Hayashi, S.; Seki, K.; Wakabayashi, H.; Itoh, S.; Asakura, H. What is an appropriate indication for endoscopic papillary balloon dilation? Eur. J. Gastroenterol. Hepatol. 2002, 14, 635–640. [Google Scholar] [CrossRef]
- Vlavianos, P.; Chopra, K.; Mandalia, S.; Anderson, M.; Thompson, J.; Westaby, D. Endoscopic balloon dilatation versus endoscopic sphincterotomy for the removal of bile duct stones: A prospective randomised trial. Gut 2003, 52, 1165–1169. [Google Scholar] [CrossRef]
- Takezawa, M.; Kida, Y.; Kida, M.; Saigenji, K. Influence of endoscopic papillary balloon dilation and endoscopic sphincterotomy on sphincter of oddi function: A randomized controlled trial. Endoscopy 2004, 36, 631–637. [Google Scholar] [CrossRef]
- Watanabe, H.; Yoneda, M.; Tominaga, K.; Monma, T.; Kanke, K.; Shimada, T.; Terano, A.; Hiraishi, H. Comparison between endoscopic papillary balloon dilatation and endoscopic sphincterotomy for the treatment of common bile duct stones. J. Gastroenterol. 2007, 42, 56–62. [Google Scholar] [CrossRef]
- Seo, Y.R.; Moon, J.H.; Choi, H.J.; Kim, D.C.; Ha, J.S.; Lee, T.H.; Cha, S.W.; Cho, Y.D.; Park, S.H.; Kim, S.J. Comparison of endoscopic papillary balloon dilation and sphincterotomy in young patients with CBD stones and gallstones. Dig. Dis. Sci. 2014, 59, 1042–1047. [Google Scholar] [CrossRef] [PubMed]
- Heo, J.H.; Kang, D.H.; Jung, H.J.; Kwon, D.S.; An, J.K.; Kim, B.S.; Suh, K.D.; Lee, S.Y.; Lee, J.H.; Kim, G.H.; et al. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest. Endosc. 2007, 66, 720–726; quiz 768, 771. [Google Scholar] [CrossRef] [PubMed]
- Stefanidis, G.; Viazis, N.; Pleskow, D.; Manolakopoulos, S.; Theocharis, L.; Christodoulou, C.; Kotsikoros, N.; Giannousis, J.; Sgouros, S.; Rodias, M.; et al. Large balloon dilation vs. mechanical lithotripsy for the management of large bile duct stones: A prospective randomized study. Am. J. Gastroenterol. 2011, 106, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.G.; Cheon, Y.K.; Cho, Y.D.; Moon, J.H.; Park, D.H.; Lee, T.H.; Choi, H.J.; Park, S.H.; Lee, J.S.; Lee, M.S. Small sphincterotomy combined with endoscopic papillary large balloon dilation versus sphincterotomy. World J. Gastroenterol. 2009, 15, 4298–4304. [Google Scholar] [CrossRef]
- Itoi, T.; Itokawa, F.; Sofuni, A.; Kurihara, T.; Tsuchiya, T.; Ishii, K.; Tsuji, S.; Ikeuchi, N.; Moriyasu, F. Endoscopic sphincterotomy combined with large balloon dilation can reduce the procedure time and fluoroscopy time for removal of large bile duct stones. Am. J. Gastroenterol. 2009, 104, 560–565. [Google Scholar] [CrossRef]
- Kim, T.H.; Oh, H.J.; Lee, J.Y.; Sohn, Y.W. Can a small endoscopic sphincterotomy plus a large-balloon dilation reduce the use of mechanical lithotripsy in patients with large bile duct stones? Surg. Endosc. 2011, 25, 3330–3337. [Google Scholar] [CrossRef]
- Kim, K.Y.; Han, J.; Kim, H.G.; Kim, B.S.; Jung, J.T.; Kwon, J.G.; Kim, E.Y.; Lee, C.H. Late Complications and Stone Recurrence Rates after Bile Duct Stone Removal by Endoscopic Sphincterotomy and Large Balloon Dilation are Similar to Those after Endoscopic Sphincterotomy Alone. Clin. Endosc. 2013, 46, 637–642. [Google Scholar] [CrossRef]
- Rosa, B.; Moutinho Ribeiro, P.; Rebelo, A.; Pinto Correia, A.; Cotter, J. Endoscopic papillary balloon dilation after sphincterotomy for difficult choledocholithiasis: A case-controlled study. World J. Gastrointest. Endoscopy 2013, 5, 211–218. [Google Scholar] [CrossRef]
- Xu, X.D.; Chen, B.; Dai, J.J.; Qian, J.Q.; Xu, C.F. Minor endoscopic sphincterotomy followed by large balloon dilation for large choledocholith treatment. World J. Gastroenterol. 2017, 23, 5739–5745. [Google Scholar] [CrossRef]
- Hwang, J.C.; Kim, J.H.; Lim, S.G.; Kim, S.S.; Shin, S.J.; Lee, K.M.; Yoo, B.M. Endoscopic large-balloon dilation alone versus endoscopic sphincterotomy plus large-balloon dilation for the treatment of large bile duct stones. BMC Gastroenterol. 2013, 13, 15. [Google Scholar] [CrossRef]
- Cheon, Y.K.; Lee, T.Y.; Kim, S.N.; Shim, C.S. Impact of endoscopic papillary large-balloon dilation on sphincter of Oddi function: A prospective randomized study. Gastrointest. Endosc. 2017, 85, 782–790.e1. [Google Scholar] [CrossRef] [PubMed]
- Kogure, H.; Tsujino, T.; Isayama, H.; Takahara, N.; Uchino, R.; Hamada, T.; Miyabayashi, K.; Mizuno, S.; Mohri, D.; Yashima, Y.; et al. Short- and long-term outcomes of endoscopic papillary large balloon dilation with or without sphincterotomy for removal of large bile duct stones. Scand. J. Gastroenterol. 2014, 49, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Kogure, H.; Kawahata, S.; Mukai, T.; Doi, S.; Iwashita, T.; Ban, T.; Ito, Y.; Kawakami, H.; Hayashi, T.; Sasahira, N.; et al. Multicenter randomized trial of endoscopic papillary large balloon dilation without sphincterotomy versus endoscopic sphincterotomy for removal of bile duct stones: Marvelous trial. Endoscopy 2020. [Google Scholar] [CrossRef] [PubMed]
- Ding, J.; Li, F.; Zhu, H.Y.; Zhang, X.W. Endoscopic treatment of difficult extrahepatic bile duct stones, EPBD or EST: An anatomic view. World J. Gastrointest. Endosc. 2015, 7, 274–277. [Google Scholar] [CrossRef]
- Iakovou, I.; Schmidt, T.; Bonizzoni, E.; Ge, L.; Sangiorgi, G.M.; Stankovic, G.; Airoldi, F.; Chieffo, A.; Montorfano, M.; Carlino, M.; et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA 2005, 293, 2126–2130. [Google Scholar] [CrossRef]
- Mauri, L.; Hsieh, W.H.; Massaro, J.M.; Ho, K.K.; D’Agostino, R.; Cutlip, D.E. Stent thrombosis in randomized clinical trials of drug-eluting stents. N. Engl. J. Med. 2007, 356, 1020–1029. [Google Scholar] [CrossRef]
- Kuo, C.M.; Chiu, Y.C.; Liang, C.M.; Wu, C.K.; Lu, L.S.; Tai, W.C.; Kuo, Y.H.; Wu, K.L.; Chuah, S.K.; Kuo, C.H. The efficacy of limited endoscopic sphincterotomy plus endoscopic papillary large balloon dilation for removal of large bile duct stones. BMC Gastroenterol. 2019, 19, 93. [Google Scholar] [CrossRef]
| Balloon Dilation | ||||
|---|---|---|---|---|
| (-) | ≤10 mm | 12 mm≤ | ||
| Sphincterotomy | (+) | EST | ESBD | ESLBD |
| (-) | - | EPBD | EPLBD | |
| Author | Comparison | Study Design | No. of Patients | Diameter of Stones (mm) Mean ± SD or Mean (Range) | Balloon Size, mm | Procedure Time, min | ML Use % (No.) | Successful Stone Removal in the 1st Session % (No.) | Overall Uccessful Stone Removal % (No.) | Overall AEs % (No.) | Bleeding % (No.) | Perforation % (No.) | PEP % (No.) | Cholangitis % (No.) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EST vs. EPBD | ||||||||||||||
| Bergman | EST | RCT | 101 | 9 (4–27) | NA | 12.9% (13) | 91.1% (92) | 91.1% (92) | 11.9% (12) | 4% (4) | 1% (1) | 6.9% (7) | 0% (0) | |
| EPBD | RCT | 101 | 10 (3–36) | 8 | NA | 30.7% (31) | 80.2% (81) | 89.1% (90) | 8.9% (9) | 0% (0) | 2% (2) | 6.9% (7) | 0% (0) | |
| Ochi | EST | RCT | 55 | 8.8 ± 4.2 | NA | 3.7% (2) | 94.4% (51) | 98.1% (54) | 5.6% (3) | 0% (0) | 1.8% (1) | 3.6% (2) | 0% (0) | |
| EPBD | RCT | 55 | 8.1 ± 3.4 | 8 | NA | 13.7% (7) | 78.4% (40) | 92.7% (51) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | |
| Arnold | EST | RCT | 30 | 10 ± 4.7 | 17 ± 12 | NA | 100% (30) | 100% (30) | 16.7% (5) | 6.7% (2) | 0% (0) | 10% (3) | 0% (0) | |
| EPBD | RCT | 30 | 7 ± 3.5 | 8 | 29 ± 15 | NA | 76.7% (23) | 100% (30) | 30% (9) | 0% (0) | 0% (0) | 20% (6) | 10% (3) | |
| Yasuda | EST | RCT | 35 | 12.3 (5–24) | NA | 25.7% (9) | 100% (35) | 100% (35) | 8.6% (3) | 2.9% (1) | 0% (0) | 5.7% (2) | 0% (0) | |
| EPBD | RCT | 35 | 12.4 (4–24) | 8 | NA | 48.6% (17) | 100% (35) | 100% (35) | 5.7% (2) | 0% (0) | 0% (0) | 5.7% (2) | 0% (0) | |
| Natsui | EST | RCT | 70 | 9.7 (3–17) | NA | 38.6% (27) | 70% (49) | 98.6% (69) | 11.4% (8) | 2.9% (2) | 0% (0) | 4.3% (3) | 4.3% (3) | |
| EPBD | RCT | 70 | 9.2 (3–22) | 8 | NA | 41.4% (29) | 58.6% (41) | 92.9% (65) | 8.6% (6) | 0% (0) | 0% (0) | 5.7% (4) | 2.9% (2) | |
| Fujita | EST | RCT | 144 | 7.3 ± 3.4 | NA | 11.8% (17) | 78.5% (113) | 100% (144) | 12.5% (18) | 1.4% (2) | 0% (0) | 2.8% (4) | 8.3% (12) | |
| EPBD | RCT | 138 | 7 ± 3.1 | 4-8 | NA | 14.5% (20) | 76.1% (105) | 99.3% (137) | 14.5% (20) | 0% (0) | 0% (0) | 10.9% (15) | 3.6% (5) | |
| Vlavianos | EST | RCT | 99 | NA | NA | NA | 63.6% (63) | 86.9% (86) | 2% (2) | 0% (0) | 0% (0) | 1% (1) | 1% (1) | |
| EPBD | RCT | 103 | NA | 10 | NA | NA | 63.1% (65) | 87.4% (90) | 6.8% (7) | 0% (0) | 0% (0) | 4.9% (5) | 1.9% (2) | |
| Disario | EST | RCT | 120 | 5 (0.5–14) | 42 ± 19 | NA | 92.5% (111) | NA | 3.3% (4) | 0% (0) | 0.8% (1) | 0.8% (1) | 1.7% (2) | |
| EPBD | RCT | 117 | 6 (0.5–10) | ≤8 | 47 ± 25 | NA | 88% (103) | NA | 17.9% (21) | 0% (0) | 0% (0) | 15.4% (18) | 2.6% (3) | |
| Takezawa | EST | RCT | 45 | 11 (3–27) | 37.2 ± 12.4 | 31.1% (14) | NA | 100% (45) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | |
| EPBD | RCT | 46 | 10 (1–35) | 8 | 37.4 ± 13 | 34.8% (16) | NA | 100% (46) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | |
| Watanabe | EST | RCT | 90 | 7.7 ± 2.9 | NA | 64.4% (58) | 57.8% (52) | 95.6% (86) | 3.3% (3) | 1.1% (1) | 0% (0) | 2.2% (2) | 0% (0) | |
| EPBD | RCT | 90 | 8.1 ± 3.2 | 8 | NA | 84.4% (76) | 72.2% (65) | 86.7% (78) | 13.3% (12) | 0% (0) | 0% (0) | 10% (9) | 3.3% (3) | |
| Seo | EST | RCT | 70 | 7.6 ± 3.1 | NA | 8.6% (6) | 91.4% (64) | 100% (70) | 11.4% (8) | 2.9% (2) | 1.4% (1) | 7.1% (5) | 0% (0) | |
| EPBD | RCT | 62 | 7.2 ± 2.1 | 6-10 | NA | 8.1% (5) | 91.9% (57) | 98.4% (61) | 8.1% (5) | 0% (0) | 0% (0) | 8.1% (5) | 0% (0) | |
| EST vs. ESBD | ||||||||||||||
| Ishii | EST | NRCT | 114 | 5.1 ± 2.9 | 31.6 ± 16.8 | 16.7% (19) | 64.9% (74) | 100% (114) | 15.8% (18) | 9.6% (11) | 1.8% (2) | 2.6% (3) | 1.8% (2) | |
| ESBD | NRCT | 321 | 5.6 ± 3 | 8-10 | 25.8 ± 18.8 | 7.8% (25) | 87.2% (280) | 100% (321) | 4.4% (14) | 1.2% (4) | 0.3% (1) | 1.9% (6) | 0.9% (3) | |
| Author | Comparison | Study Design | No. of Patients | Diameter of Stones (mm) mean ± SD or mean (Range) | Balloon Size, mm | Procedure Time, min | ML Use % (No.) | Successful Stone Removal in the 1st Session % (No.) | Overall Uccessful Stone Removal % (No.) | Overall AEs % (No.) | Bleeding % (No.) | Perforation % (No.) | PEP % (No.) | Cholangitis % (No.) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EST vs. ESLBD | ||||||||||||||
| Heo | EST | RCT | 100 | 15 ± 0.7 | NA | 9% (9) | 87% (87) | 98% (98) | 7% (7) | 2% (2) | 0% (0) | 4% (4) | 1% (1) | |
| ESLBD | RCT | 100 | 16 ± 0.7 | 12–20 | NA | 8% (8) | 83% (83) | 97% (97) | 5% (5) | 0% (0) | 0% (0) | 4% (4) | 1% (1) | |
| Kim | EST | RCT | 28 | 21.3 ± 5.2 | 19 ± 13 | 32% (9) | 82.1% (23) | 100% (28) | 7.1% (2) | 7.1% (2) | 0% (0) | 0% (0) | 0% (0) | |
| ESLBD | RCT | 27 | 20.8 ± 4.1 | 15–18 | 18 ± 12 | 33% (9) | 85.2% (23) | 100% (27) | 14.8% (4) | 14.8% (4) | 0% (0) | 0% (0) | 0% (0) | |
| Stefanidis | EST | RCT | 45 | NA | NA | 100% (45) | 91.1% (41) | 91.1% (41) | 20% (9) | 2.2% (1) | 2.2% (1) | 2.2% (1) | 13.3% (6) | |
| ESLBD | RCT | 45 | NA | 15–20 | NA | 0% (0) | 97.7% (44) | 97.8% (44) | 4.4% (2) | 2.2% (1) | 0% (0) | 2.2% (1) | 0% (0) | |
| Qian | EST | RCT | 69 | 20.3 ± 5.3 | 15.9 ± 8.8 | 24.6% (17) | 60.9% (42) | 91.3% (63) | 11.6% (8) | 0% (0) | 1.4% (1) | 8.7% (6) | 1.4% (1) | |
| ESLBD | RCT | 63 | 20.6 ± 5.4 | 12–20 | 14.5 ± 8.4 | 7.9% (5) | 81% (51) | 95.2% (60) | 7.9% (5) | 0% (0) | 0% (0) | 6.3% (4) | 1.6% (1) | |
| Karsenti | EST | RCT | 73 | 16.2 ± 3.5 | NA | 35.6% (26) | 74% (54) | 94.5% (69) | 4.1% (3) | 2.7% (2) | 0% (0) | 0% (0) | 1.4% (1) | |
| ESLBD | RCT | 77 | 16.5 ± 3.3 | 12–20 | NA | 3.9% (3) | 96.1% (74) | 96.1% (74) | 7.8% (6) | 3.9% (3) | 1.3% (1) | 1.3% (1) | 1.3% (1) | |
| Itoi | EST | NRCT | 48 | 15.3 ± 3.2 | 40.2 ± 16.3 | 25% (12) | 85.4% (41) | 97.9% (47) | 14.6% (7) | 8.3% (4) | 0% (0) | 4.1% (2) | 2.1% (1) | |
| ESLBD | NRCT | 53 | 14.8 ± 3.5 | 15–20 | 31.6 ± 11.3 | 5.7% (3) | 96.2% (51) | 100% (53) | 5.7% (3) | 1.9% (1) | 0% (0) | 1.9% (1) | 1.9% (1) | |
| Kim KY | EST | NRCT | 121 | 10 (2–20) | NA | 27.3% (33) | NA | 100% (121) | 16.5% (20) | 14% (17) | 0.8% (1) | 1.7% (2) | 0% (0) | |
| ESLBD | NRCT | 101 | 12 (3–25) | 12– | NA | 24.8% (25) | NA | 99% (100) | 17.8% (18) | 16.8% (17) | 0% (0) | 1% (1) | 0% (0) | |
| Kim TH | EST | NRCT | 77 | NA | NA | 19.5% (15) | 74% (57) | 94.8% (73) | 13% (10) | 0% (0) | 1.3% (1) | 11.7% (9) | 0% (0) | |
| ESLBD | NRCT | 72 | NA | 12–20 | NA | 8.3% (6) | 87.5% (63) | 97.2% (70) | 8.3% (6) | 0% (0) | 0% (0) | 6.9% (5) | 1.3% (1) | |
| Xu | EST | NRCT | 76 | 16.5 ± 4.7 | 47.3 ± 11.8 | 18.4% (14) | 84.2% (64) | 100% (76) | 21.1% (16) | 7.9% (6) | 0% (0) | 9.2% (7) | 4% (3) | |
| ESLBD | NRCT | 73 | 16.9 ± 4.1 | 12–20 | 42.1 ± 13.6 | 6.8% (5) | 94.5% (69) | 100% (73) | 11% (8) | 1.4% (1) | 0% (0) | 8.2% (6) | 1.4% (1) | |
| Rosa | EST | NRCT | 43 | 16 ± 6.7 | NA | 37.2% (16) | 44.2% (19) | 69.8% (30) | 11.6% (5) | 4.7% (2) | 0% (0) | 4.7% (2) | 2.3% (1) | |
| ESLBD | NRCT | 68 | 16.8 ± 4.4 | 12-18 | NA | 14.7% (10) | 82.4% (56) | 95.6% (65) | 14.7% (10) | 0% (0) | 0% (0) | 13.2% (9) | 1.5% (1) | |
| EPLBD vs. ESLBD | ||||||||||||||
| Hwang | EPLBD | RCT | 62 | 15.7 ± 3.3 | 12–20 | NA | 19.4% (12) | 91.9% (57) | 96.8% (60) | 6.5% (4) | 0% (0) | 0% (0) | 6.5% (4) | 0% (0) |
| ESLBD | RCT | 69 | 16.5 ± 4.2 | 12–20 | NA | 26.1% (18) | 94.2% (65) | 95.7% (66) | 5.7% (4) | 0% (0) | 1.4% (1) | 4.3% (3) | 0% (0) | |
| Cheon | EPLBD | RCT | 42 | 14.4 ± 3.3 | 12– | 10.8 ± 6.9 | 21.4% (9) | 95.2% (40) | 97.6% (41) | 11.9% (5) | 2.4% (1) | 0% (0) | 7.1% (3) | 2.4% (1) |
| ESLBD | RCT | 44 | 14 ± 2.1 | 12– | 10.6 ± 5.7 | 13.6% (6) | 97.7% (43) | 100% (43) | 11.4% (5) | 2.3% (1) | 0% (0) | 11.4% (5) | 0% (0) | |
| Kogure | EPLBD | NRCT | 28 | 14 ± 4 | 12–18 | NA | 10.7% (3) | 89.3% (25) | 96.4% (27) | 7.1% (2) | 0% (0) | 3.6% (1) | 3.6% (1) | 0% (0) |
| ESLBD | NRCT | 14 | 14 ± 4 | 12–18 | NA | 7.1% (1) | 71.4% (10) | 100% (14) | 7.1% (1) | 0% (0) | 0% (0) | 7.1% (1) | 0% (0) | |
| EST vs. EPLBD | ||||||||||||||
| Kogure | EST | RCT | 85 | 14.3 ± 4.8 | 52.6 ± 58.4 | 48.2% (41) | 78.8%(67) | 95.3% (81) | 9.4% (8) | 1.2% (1) | 0% (0) | 5.9% (5) | 2.4% (2) | |
| EPLBD | 86 | 15.2 ± 4.6 | 49.6 ± 39.7 | 30.2% (26) | 90.7% (78) | 100% (86) | 9.3% (8) | 0% (0) | 0% (0) | 4.7% (4) | 3.5% (3) | |||
| Removal of Small Stones | Removal of Large Stone | |||||
|---|---|---|---|---|---|---|
| EST | EPBD | ESBD | EST | EPLBD | ESLBD | |
| Efficacy | ||||||
| Complete stone removal in initial session | 78.3% (699/893) | 75.7% (580/766) | 87.2 (280/321) | 76.6% (428/559) | 92.4% (122/132) | 89.6% (632/705) |
| Rate of ML | 22.8% (165/724) | 33.7% (201/597) | 7.8% (25/321) | 23.8% (151/635) | 18.2% (24/132) | 13.0% (99/761) |
| Safety | ||||||
| Bleeding | 2.6% (25/973) | 0% (0/847) | 1.2% (4/321) | 5.3% (36/680) | 0.8% (1/132) | 3.5% (28/806) |
| Post ERCP pancreatitis | 4.9% (48/973) | 8.4% (71/847) | 4.4% (14/321) | 4.9% (33/680) | 6.1% (8/132) | 5.1% (41/806) |
| Perforation | 0.6% (6/973) | 0.2% (2/847) | 0.3% (1/321) | 0.6% (4/680) | 0.8% (1/132) | 0.2% (2/806) |
| Removal of Small Stones | Removal of Large Stone | |||||
|---|---|---|---|---|---|---|
| EST | EPBD | ESBD | EST | EPLBD | ESLBD | |
| Efficacy | ||||||
| Complete stone removal in initial session | 2 | 1 | 3 | 1 | 3 | 3 |
| Rate of ML | 2 | 1 | 3 | 1 | 2 | 3 |
| Safety | ||||||
| Bleeding | 1 | 3 | 2 | 1 | 3 | 2 |
| Post ERCP pancreatitis | 3 | 1 | 3 | 2 | 2 | 2 |
| Perforation | 2 | 2 | 2 | 2 | 2 | 2 |
| Easiness | ||||||
| Easiness of the procedure | 1 | 3 | 2 | 1 | 3 | 2 |
| Easiness of stone extraction | 2 | 1 | 3 | 1 | 2 | 3 |
| Total score | 13 | 12 | 18 | 9 | 17 | 17 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ishii, S.; Isayama, H.; Ushio, M.; Takahashi, S.; Yamagata, W.; Takasaki, Y.; Suzuki, A.; Ochiai, K.; Tomishima, K.; Kanazawa, R.; et al. Best Procedure for the Management of Common Bile Duct Stones via the Papilla: Literature Review and Analysis of Procedural Efficacy and Safety. J. Clin. Med. 2020, 9, 3808. https://doi.org/10.3390/jcm9123808
Ishii S, Isayama H, Ushio M, Takahashi S, Yamagata W, Takasaki Y, Suzuki A, Ochiai K, Tomishima K, Kanazawa R, et al. Best Procedure for the Management of Common Bile Duct Stones via the Papilla: Literature Review and Analysis of Procedural Efficacy and Safety. Journal of Clinical Medicine. 2020; 9(12):3808. https://doi.org/10.3390/jcm9123808
Chicago/Turabian StyleIshii, Shigeto, Hiroyuki Isayama, Mako Ushio, Sho Takahashi, Wataru Yamagata, Yusuke Takasaki, Akinori Suzuki, Kazushige Ochiai, Ko Tomishima, Ryo Kanazawa, and et al. 2020. "Best Procedure for the Management of Common Bile Duct Stones via the Papilla: Literature Review and Analysis of Procedural Efficacy and Safety" Journal of Clinical Medicine 9, no. 12: 3808. https://doi.org/10.3390/jcm9123808
APA StyleIshii, S., Isayama, H., Ushio, M., Takahashi, S., Yamagata, W., Takasaki, Y., Suzuki, A., Ochiai, K., Tomishima, K., Kanazawa, R., Saito, H., Fujisawa, T., & Shiina, S. (2020). Best Procedure for the Management of Common Bile Duct Stones via the Papilla: Literature Review and Analysis of Procedural Efficacy and Safety. Journal of Clinical Medicine, 9(12), 3808. https://doi.org/10.3390/jcm9123808






