Porous Tantalum vs. Titanium Implants: Enhanced Mineralized Matrix Formation after Stem Cells Proliferation and Differentiation
Abstract
1. Introduction
2. Experimental Section
2.1. Implant Materials
2.2. Culture of Human DPSC
2.3. Proliferation Assays
2.4. Scanning Electron Microscopy (SEM) and Energy Dispersion X-ray Spectroscopy (EDX)
2.5. Cell Differentiation
2.6. Extracellular Matrix Formation
2.7. Calcium Deposits
2.8. Statistical Analysis
3. Results
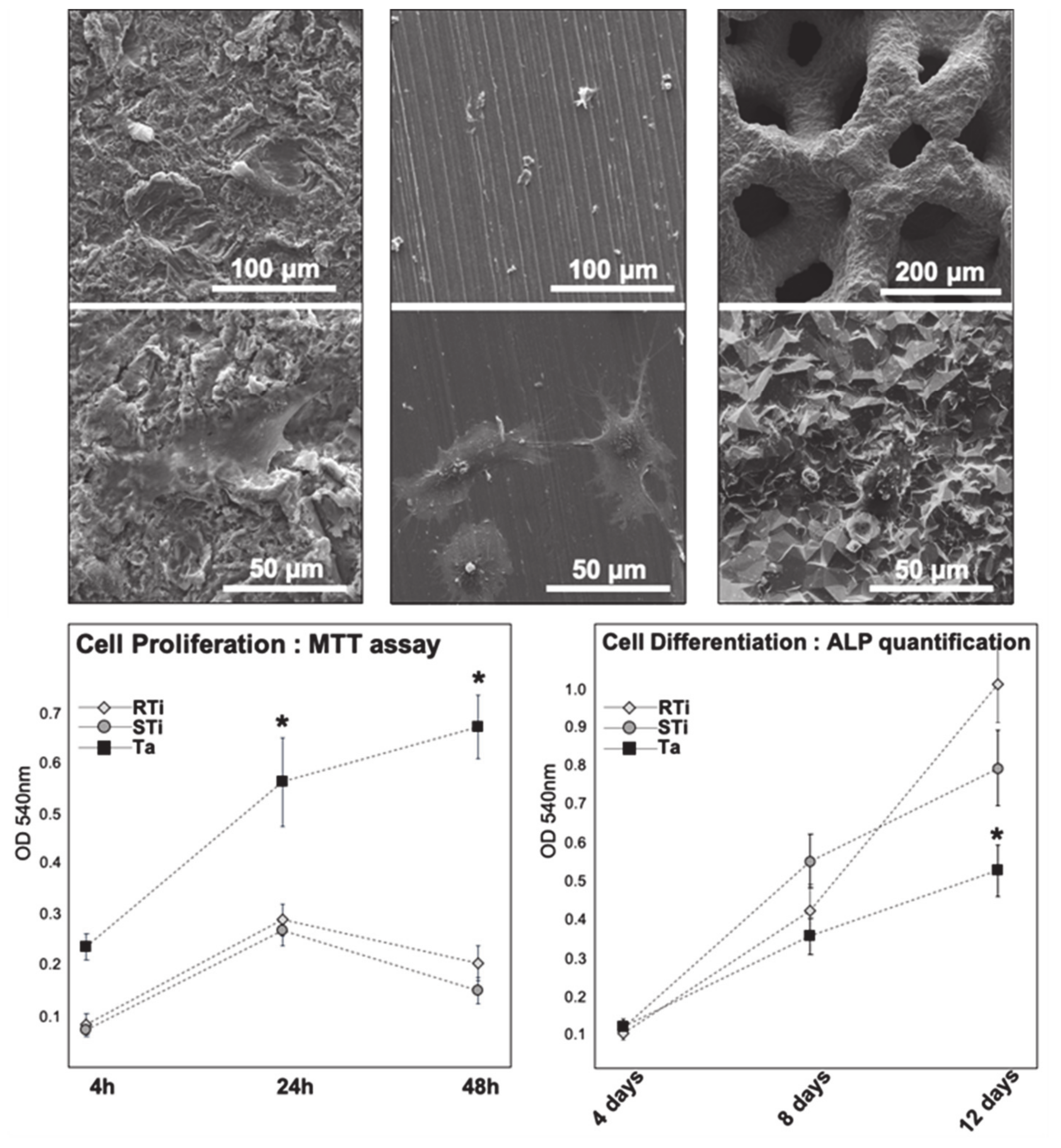
3.1. Cell Adhesion and Proliferation
3.2. Cell Osteodifferentiation
3.3. SEM and EDX
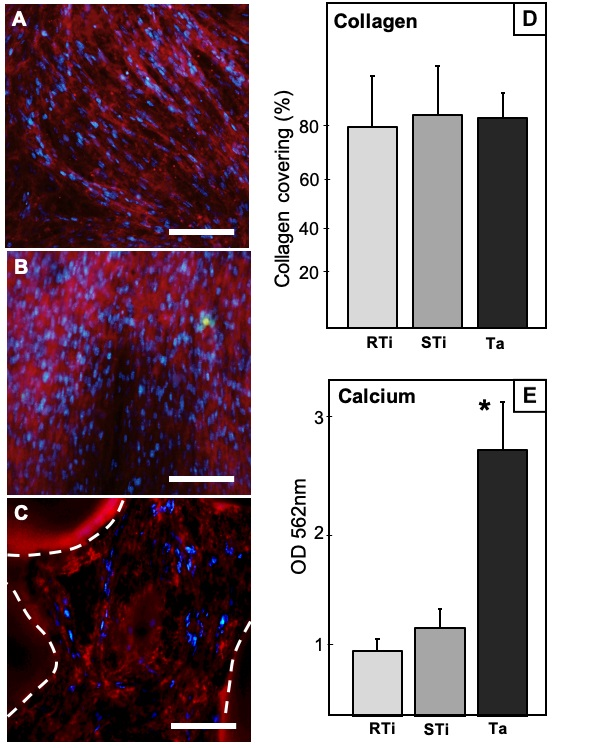
3.4. Collagen Immunostaining
3.5. Calcium Deposits Quantification
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Vos, T.; Allen, C.; Arora, M.; Barber, R.M.; Bhutta, Z.A.; Brown, A. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef]
- Rupp, F.; Liang, L.; Geis-Gerstorfer, J.; Scheideler, L.; Hüttig, F. Surface characteristics of dental implants: A review. Dent. Mater. 2018, 34, 40–57. [Google Scholar] [CrossRef]
- Junker, R.; Dimakis, A.; Thoneick, M.; Jansen, J.A. Effects of implant surface coatings and composition on bone integration: A systematic review. Clin. Oral. Implants Res. 2009, 20, 185–206. [Google Scholar] [CrossRef]
- Kasemo, B. Biocompatibility of titanium implants: Surface science aspects. J. Prosthet Dent. 1983, 49, 832–837. [Google Scholar] [CrossRef]
- Zhu, X.; Chen, J.; Scheideler, L.; Reichl, R.; Geis-Gerstorfer, J. Effects of topography and composition of titanium surface oxides on osteoblast responses. Biomaterials 2004, 25, 4087–4103. [Google Scholar] [CrossRef]
- Dohan Ehrenfest, D.M.; Coelho, P.G.; Kang, B.; Sul, Y.T.; Albrektsson, T. Classification of osseointegrated implant surfaces: Materials, chemistry and topography. Trends Biotechnol. 2010, 28, 198–206. [Google Scholar] [CrossRef]
- Smeets, R.; Stadlinger, B.; Schwarz, F.; Beck-Broichsitter, B.; Jung, O.; Precht, C.; Kloss, F.; Gröbe, A.; Heiland, M.; Ebker, T. Impact of dental implant surface modifications on osseointegration. Biomed. Res. Int. 2016, 2016, 6285620. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Reasons for failures of oral implants. J. Oral. Rehabil. 2014, 41, 443–476. [Google Scholar] [CrossRef] [PubMed]
- Wennerberg, A.; Albrektsson, T. Effects of titanium surface topography on bone integration: A systematic review. Clin. Oral. Implants Res. 2009, 20, 172–184. [Google Scholar] [CrossRef] [PubMed]
- Annunziata, M.; Guida, L. The effect of titanium surface modifications on dental implant osseointegration. Front. Oral. Biol. 2015, 17, 62–77. [Google Scholar] [CrossRef]
- Park, J.Y.; Gemmell, C.H.; Davies, J.E. Platelet interactions with titanium: Modulation of platelet activity by surface topography. Biomaterials 2001, 22, 2671–2682. [Google Scholar] [CrossRef]
- Pellegrini, G.; Francetti, L.; Barbaro, B.; del Fabbro, M. Novel surfaces and osseointegration in implant dentistry. J. Investig. Clin. Dent. 2018, 9, 12349. [Google Scholar] [CrossRef] [PubMed]
- Ghensi, P.; Bressan, E.; Gardin, C.; Ferroni, L.; Ruffato, L.; Caberlotto, M.; Soldini, C.; Zavan, B. Osteo growth induction titanium surface treatment reduces ROS production of mesenchymal stem cells increasing their osteogenic commitment. Mater. Sci Eng. C Mater. Biol. Appl. 2017, 74, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Gittens, R.A.; Olivares-Navarrete, R.; Hyzy, S.L.; Sandhage, K.H.; Schwartz, Z.; Boyan, B.D. Superposition of nanostructures on microrough titanium–aluminum–vanadium alloy surfaces results in an altered integrin expression profile in osteoblasts. Connect. Tissue Res. 2014, 55, 164–168. [Google Scholar] [CrossRef][Green Version]
- Ogle, O.E. Implant surface material, design, and osseointegration. Dent. Clin. N. Am. 2015, 59, 505–520. [Google Scholar] [CrossRef]
- Goiato, M.C.; dos Santos, D.M.; Santiago, J.F.; Moreno, A.; Pellizzer, E.P. Longevity of dental implants in type IV bone: A systematic review. Int. J. Oral. Maxillofac. Surg. 2014, 43, 1108–1116. [Google Scholar] [CrossRef]
- Todisco, M.; Trisi, P. Histomorphometric evaluation of six dental implant surfaces after early loading in augmented human sinuses. J. Oral. Implantol. 2006, 32, 153–166. [Google Scholar] [CrossRef]
- Olmedo, D.G.; Paparella, M.L.; Brandizzi, D.; Cabrini, R.L. Reactive lesions of peri-implant mucosa associated with titanium dental implants: A report of 2 cases. Int. J. Oral. Maxillofac. Surg. 2010, 39, 503–507. [Google Scholar] [CrossRef]
- Sicilia, A.; Cuesta, S.; Coma, G.; Arregui, I.; Guisasola, C.; Ruiz, E.; Maestro, A. Titanium allergy in dental implant patients: A clinical study on 1500 consecutive patients. Clin. Oral. Implants Res. 2008, 19, 823–835. [Google Scholar] [CrossRef]
- Balla, V.; Bodhak, S.; Bose, S.; Bandyopadhyay, A. Porous tantalum structures for bone implants: Fabrication, mechanical and in vitro biological properties. Acta Biomater. 2010, 6, 3349–3359. [Google Scholar] [CrossRef]
- Fohlerova, Z.; Mozalev, A. Tuning the response of osteoblast-like cells to the porous-alumina assisted mixed-oxide nano-mound arrays. J. Biomed. Mater. Res. B Appl. Biomater. 2018, 106, 1645–1654. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Bao, C.; Wismeijer, D.; Wu, G. The physicochemical/biological properties of porous tantalum and the potential surface modification techniques to improve its clinical application in dental implantology. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 49, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Pałka, K.; Pokrowiecki, R. Porous titanium implants: A review. Adv. Eng. Mater. 2018, 20, 1700648. [Google Scholar] [CrossRef]
- Wally, Z.; van Grunsven, W.; Claeyssens, F.; Goodall, R.; Reilly, G.C. Porous titanium for dental implant applications. Metals 2015, 5, 1902–1920. [Google Scholar] [CrossRef]
- Orti, V.; Collart-Dutilleul, P.Y.; Piglionico, S.; Pall, O.; Cuisinier, F.; Panayotov, I. Pulp regeneration concepts for nonvital teeth: From tissue engineering to clinical approaches. Tissue Eng. Part. B Rev. 2018, 24, 419–442. [Google Scholar] [CrossRef] [PubMed]
- Gronthos, S.; Mankani, M.; Brahim, J.; Robey, P.G.; Shi, S. Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proc. Natl. Acad. Sci. USA 2000, 97, 13625–13630. [Google Scholar] [CrossRef]
- Collart-Dutilleul, P.Y.; Chaubron, F.; De Vos, J.; Cuisinier, F.J. Allogenic banking of dental pulp stem cells for innovative therapeutics. World J. Stem. Cells 2015, 7, 1010–1021. [Google Scholar] [CrossRef]
- Collart-Dutilleul, P.Y.; Secret, E.; Panayotov, I.; Deville de Périère, D.; Martín-Palma, R.; Torres-Costa, V.; Martin, M.; Gergely, C.; Durand, J.O.; Cunin, F.; et al. Adhesion and Proliferation of Human Mesenchymal Stem Cells from Dental Pulp on Porous Silicon Scaffolds. ACS Appl. Mater. Interfaces 2014, 6, 1719–1728. [Google Scholar] [CrossRef]
- Zhang, Y.; Zheng, Y.; Li, Y.; Wang, L.; Bai, Y.; Zhao, Q.; Xiong, X.; Cheng, Y.; Tang, Z.; Deng, Y.; et al. Tantalum Nitride-Decorated Titanium with Enhanced Resistance to Microbiologically Induced Corrosion and Mechanical Property for Dental Application. PLoS ONE 2015, 10, e0130774. [Google Scholar] [CrossRef]
- Welldon, K.J.; Atkins, G.J.; Howie, D.W.; Findlay, D.M. Primary human osteoblasts grow into porous tantalum and maintain an osteoblastic phenotype. J. Biomed. Mater. Res. A 2008, 84, 691–701. [Google Scholar] [CrossRef]
- Collart-Dutilleul, P.Y.; Panayotov, I.; Secret, E.; Cunin, F.; Gergely, C.; Cuisinier, F.J.; Martin, M. Initial stem cell adhesion on porous silicon surface: Molecular architecture of actin cytoskeleton and filopodial growth. Nanoscale Res. Lett. 2014, 9, 564–574. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Song, X.; Zhang, P.; Zhu, Z.; Xu, X. Effects of nano tantalum implants on inducing osteoblast proliferation and differentiation. Exp. Ther. Med. 2016, 12, 3541–3544. [Google Scholar] [CrossRef] [PubMed]
- Stiehler, M.; Lind, M.; Mygind, T.; Baatrup, A.; Dolatshahi-Pirouz, A.; Li, H.; Foss, M.; Besenbacher, F.; Kassem, M.; Bünger, C. Morphology, proliferation, and osteogenic differentiation of mesenchymal stem cells cultured on titanium, tantalum, and chromium surfaces. J. Biomed. Mater. Res. A 2008, 86, 448–458. [Google Scholar] [CrossRef] [PubMed]
- Quarles, L.D.; Yohay, D.A.; Lever, L.W.; Caton, R.; Wenstrup, R.J. Distinct proliferative and differentiated stages of murine MC3T3-E1 cells in culture: An in vitro model of osteoblast development. J. Bone Miner. Res. 1992, 7, 683–692. [Google Scholar] [CrossRef] [PubMed]
- Vater, C.; Kasten, P.; Stiehler, M. Culture media for the differentiation of mesenchymal stromal cells. Acta Biomater. 2011, 7, 463–477. [Google Scholar] [CrossRef]
- Hanna, H.; Mir, L.M.; Andre, F.M. In vitro osteoblastic differentiation of mesenchymal stem cells generates cell layers with distinct properties. Stem Cell Res. Ther. 2018, 9, 203. [Google Scholar] [CrossRef] [PubMed]
- Miyaza, T.; Kim, H.M.; Kokubo, T.; Ohtsuki, C.; Kato, H.; Nakamura, T. Mechanism of bonelike apatite formation on bioactive tantalum metal in a simulated body fluid. Biomaterials 2002, 23, 827–832. [Google Scholar] [CrossRef]
- Wang, Q.; Qiao, Y.; Cheng, M.; Jiang, G.; He, G.; Chen, Y.; Zhang, X.; Liu, X. Tantalum implanted entangled porous titanium promotes surface osseointegration and bone ingrowth. Sci. Rep. 2016, 6, 26248. [Google Scholar] [CrossRef]
- Kim, D.G.; Huja, S.S.; Tee, B.C.; Larsen, P.E.; Kennedy, K.S.; Chien, H.H.; Lee, J.W.; Wen, H.B. Bone Ingrowth and Initial Stability of Titanium and Porous Tantalum Dental Implants: A Pilot Canine Study. Implant. Dent. 2013, 22, 399–405. [Google Scholar] [CrossRef]
- Lee, J.W.; Wen, H.B.; Battula, S.; Akella, R.; Collins, M.; Romanos, G.E. Outcome after placement of tantalum porous engineered dental implants in fresh extraction sockets: A canine study. Int. J. Oral. Maxillofac. Implants 2015, 30, 134–142. [Google Scholar] [CrossRef][Green Version]
- Hefni, E.K.; Bencharit, S.; Kim, S.J.; Byrd, K.M.; Moreli, T.; Nociti, F.H.; Offenbacher, S.; Barros, S.P. Transcriptomic profiling of tantalum metal implant osseointegration in osteopenic patients. BDJ Open 2018, 4, 17042. [Google Scholar] [CrossRef] [PubMed]
- Bencharit, S.; Morelli, T.; Barros, S.; Seagroves, J.; Kim, S.; Yu, N.; Byrd, K.; Brenes, C.; Offenbacher, S. Comparing initial wound healing and osteogenesis of porous tantalum trabecular metal and titanium alloy materials. J. Oral Implantol. 2019, 45, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wang, L.; Yu, X.; Feng, Y.; Wang, C.; Yang, K.; Su, D. Tantalum coating on porous Ti6Al4V scaffold using chemical vapor deposition and preliminary biological evaluation. Mat. Sci. Engineer. C 2013, 33, 2987–2994. [Google Scholar] [CrossRef]
- Matena, J.; Petersen, S.; Gieseke, M.; Kampmann, A.; Teske, M.; Beyerbach, M.; Murua Escobar, H.; Haferkamp, H.; Gellrich, N.C.; Nolte, I. SLM produced porous titanium implant improvements for enhanced vascularization and osteoblast seeding. Int. J. Mol. Sci. 2015, 16, 7478–7492. [Google Scholar] [CrossRef]
- Warnke, P.H.; Douglas, T.; Wollny, P.; Sherry, E.; Steiner, M.; Galonska, S.; Becker, S.T.; Springer, I.N.; Wiltfang, J.; Sivananthan, S. Rapid prototyping: Porous titanium alloy scaffolds produced by selective laser melting for bone tissue engineering. Tissue Eng. Part C Methods 2009, 15, 115–124. [Google Scholar] [CrossRef]
- Van Bael, S.; Chai, Y.C.; Truscello, S.; Moesen, M.; Kerckhofs, G.; Van Oosterwyck, H.; Kruth, J.P.; Schrooten, J. The effect of pore geometry on the in vitro biological behavior of human periosteum-derived cells seeded on selective laser-melted Ti6Al4V bone scaffolds. Acta Biomaterialia 2012, 8, 2824–2834. [Google Scholar] [CrossRef]
- Amin Yavari, S.; van der Stok, J.; Chai, Y.C.; Wauthle, R.; Birgani, Z.T.; Habibovic, P.; Mulier, M.; Schrooten, J.; Weinans, H.; Zadpoor, A.A. Bone regeneration performance of surface-treated porous titanium. Biomaterials 2014, 35, 6172–6181. [Google Scholar] [CrossRef]
- Markhoff, J.; Wieding, J.; Weissmann, V.; Pasold, J.; Jonitz-Heincke, A.; Bader, R. Influence of different three-dimensional open porous titanium scaffold designs on human osteoblasts behavior in static and dynamic cell investigations. Materials 2015, 8, 5490–5507. [Google Scholar] [CrossRef]
- Wysocki, B.; Idaszek, J.; Szlazak, K.; Strzelczyk, K.; Brynk, T.; Kurzydłowski, K.J.; Swieszkowski, W. Post processing and biological evaluation of the titanium scaffolds for bone tissue engineering. Materials 2016, 9, 197–215. [Google Scholar] [CrossRef]
- Wang, H.; Zhao, B.; Liu, C.; Wang, C.; Tan, X.; Hu, M. A comparison of biocompatibility of a titanium alloy fabricated by electron beam melting and selective laser melting. PLoS ONE 2016, 11, e0158513. [Google Scholar] [CrossRef]
- Fousová, M.; Vojtӗch, D.; Kubásek, J.; Jablonská, E.; Fojt, J. Promising characteristics of gradient porosity Ti6Al4V alloy prepared by SLM process. J. Mech. Behav. Biomed. Mater. 2017, 69, 368–376. [Google Scholar] [CrossRef]
- Wang, H.; Sua, K.; Sua, L.; Liang, P.; Jia, P.; Wang, C. Comparison of 3D-printed porous tantalum and titanium scaffolds on T osteointegration and osteogenesis. Mat. Sci. Engineer. C 2019, 104, 109908. [Google Scholar] [CrossRef]
- Bartolomeu, F.; Dourado, N.; Pereira, F.; Alves, N.; Miranda, G.; Silva, F.S. Additive manufactured porous biomaterials targeting orthopedic implants: A suitable combination of mechanical, physical and topological properties. Mat. Sci. Engineer. C 2020, 107, 110342. [Google Scholar] [CrossRef]
- Liu, F.; Ran, Q.; Zhao, M.; Zhang, T.; Zhang, D.Z.; Su, Z. Additively manufactured continuous cell-size gradient porous scaffolds: pore characteristics, mechanical properties and biological responses in vitro. Materials 2020, 13, 2589. [Google Scholar] [CrossRef]
- Schlee, M.; Pradies, G.; Mehmke, W.U.; Beneytout, A.; Stamm, M.; Meda, R.G.; Kamm, T.; Poiroux, F.; Weinlich, F.; del Canto Pingarron, M.; et al. Prospective, multicenter evaluation of trabecular metal-enhanced titanium dental Implants placed in routine dental practices: 1-Year interim report from the development period (2010 to 2011). Clin. Implant. Dent. Relat. Res. 2015, 17, 1141–1153. [Google Scholar] [CrossRef]
- Edelmann, A.R.; Patel, D.; Allen, R.K.; Gibson, C.J.; Best, A.M.; Bencharit, S. Retrospective analysis of porous tantalum trabecular metal–enhanced titanium dental implants. J. Prosthet Dent. 2019, 121, 404–410. [Google Scholar] [CrossRef]

| Crystal Structure | Ca/P Ratio | Ca/O Ratio |
|---|---|---|
| MonoCalcium Phosphate | 0.5 | 0.125 |
| DiCalcium Phosphate | 1 | 0.25 |
| OctaCalcium Phosphate | 1.33 | 0.275 |
| TriCalcium Phosphate | 1.5 | 0.375 |
| Hydroxyapatite | 1.67 | 0.55 |
| % Atomic Element | R Ti | S Ti | Ta |
|---|---|---|---|
| C | 21.4% | 24.9% | 19.7% |
| O | 65.1% | 65.2% | 57.1% |
| P | 2.7% | 2.2% | 2.0% |
| Ca | 3.5% | 2.7% | 2.6% |
| Ti | 4.2% | 2.2% | - |
| Ta | - | - | 17.0% |
| Ca/P Ratio | 1.27 | 1.21 | 1.28 |
| Reference | Pore Size Range | Porosity | Cell Type | Conclusion |
|---|---|---|---|---|
| Warnke 2009 [45] | 400–1000 µm | 70–80% | Osteoblast | Increased cell proliferation on scaffolds with 400 µm pore size |
| Van Bael 2012 [46] | 500–1000 µm | 70–80% | Periosteum Cell | Increased cell proliferation and cell osteodifferentiation on scaffolds with 500 µm pore size |
| Li 2013 [43] | 400–600 µm | 75–85% | BMMSC | Better cell adhesion and proliferation on porous scaffolds coated with tantalum. No difference of bone formation between coated and uncoated |
| Amin Yavari 2014 [47] | 500 µm | 88% | Periosteum Cell | Anodizing-heat treatment improves cell attachment and proliferation, and osteogenic markers expression. |
| Matena 2015 [44] | 250 µm | 50% | Osteoblast | Lower cell adhesion on PCL coated Ti scaffolds, but increased chemotactic behavior for endothelial cells |
| Markhoff 2015 [48] | 500–1000 µm | 50–70% | Osteoblast | SLM and EBM manufacturing techniques lead to similar cell adhesion, proliferation and osteodifferentiation |
| Wysocki 2016 [49] | 200–500 µm | 70% | MSC | Smaller pores improved cell adhesion and proliferation. |
| Wang 2016 [50] | 1000 µm | 75% | MSC | SLM and EBM porous Ti scaffolds are cytocompatible |
| Wang 2016 [38] | nd | 30–50% | MG63 Cell | Ta-coated porous Ti implants improve cell adhesion, proliferation and osteodifferentiation (compared to uncoated) |
| Fousová 2017 [51] | 1000 µm | 60–80% | Osteoblast | SLM porous Ti implants retain Ti alloy cytocompatibility |
| Wang 2019 [52] | 500 µm | 70% | BMMSC | Both porous Ta and porous Ti scaffolds were in favor of BMMSC proliferation and osteogenic differentiation |
| Bartolomeu 2020 [53] | 500–600 µm | 64–93% | Fibroblast | Porous Ti scaffolds produced by SLM did not release toxic substances and insured a suitable environment for cell proliferation |
| Liu 2020 [54] | 400–1000 µm | 70–85% | Osteoblast | All porosities (porous Ti gradients) investigated were suitable for cell adhesion and cell survival |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piglionico, S.; Bousquet, J.; Fatima, N.; Renaud, M.; Collart-Dutilleul, P.-Y.; Bousquet, P. Porous Tantalum vs. Titanium Implants: Enhanced Mineralized Matrix Formation after Stem Cells Proliferation and Differentiation. J. Clin. Med. 2020, 9, 3657. https://doi.org/10.3390/jcm9113657
Piglionico S, Bousquet J, Fatima N, Renaud M, Collart-Dutilleul P-Y, Bousquet P. Porous Tantalum vs. Titanium Implants: Enhanced Mineralized Matrix Formation after Stem Cells Proliferation and Differentiation. Journal of Clinical Medicine. 2020; 9(11):3657. https://doi.org/10.3390/jcm9113657
Chicago/Turabian StylePiglionico, Sofia, Julie Bousquet, Naveen Fatima, Matthieu Renaud, Pierre-Yves Collart-Dutilleul, and Philippe Bousquet. 2020. "Porous Tantalum vs. Titanium Implants: Enhanced Mineralized Matrix Formation after Stem Cells Proliferation and Differentiation" Journal of Clinical Medicine 9, no. 11: 3657. https://doi.org/10.3390/jcm9113657
APA StylePiglionico, S., Bousquet, J., Fatima, N., Renaud, M., Collart-Dutilleul, P.-Y., & Bousquet, P. (2020). Porous Tantalum vs. Titanium Implants: Enhanced Mineralized Matrix Formation after Stem Cells Proliferation and Differentiation. Journal of Clinical Medicine, 9(11), 3657. https://doi.org/10.3390/jcm9113657







