Impact of the Use of a Larger Forearm Artery on the Efficacy and Safety of Transradial and Transulnar Access: A Randomized Trial with Preprocedural Ultrasonography
Abstract
1. Introduction
2. Materials and Methods
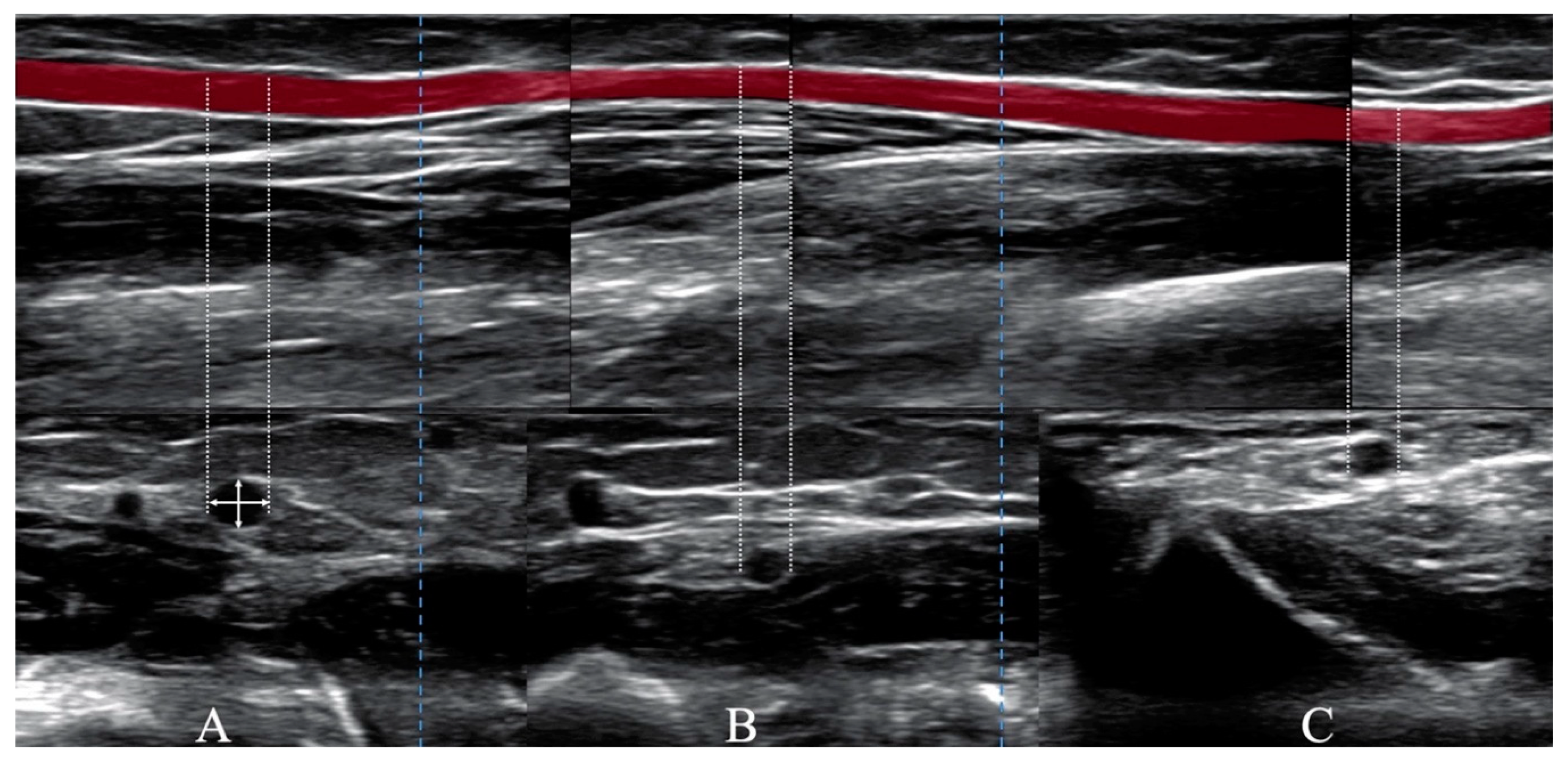
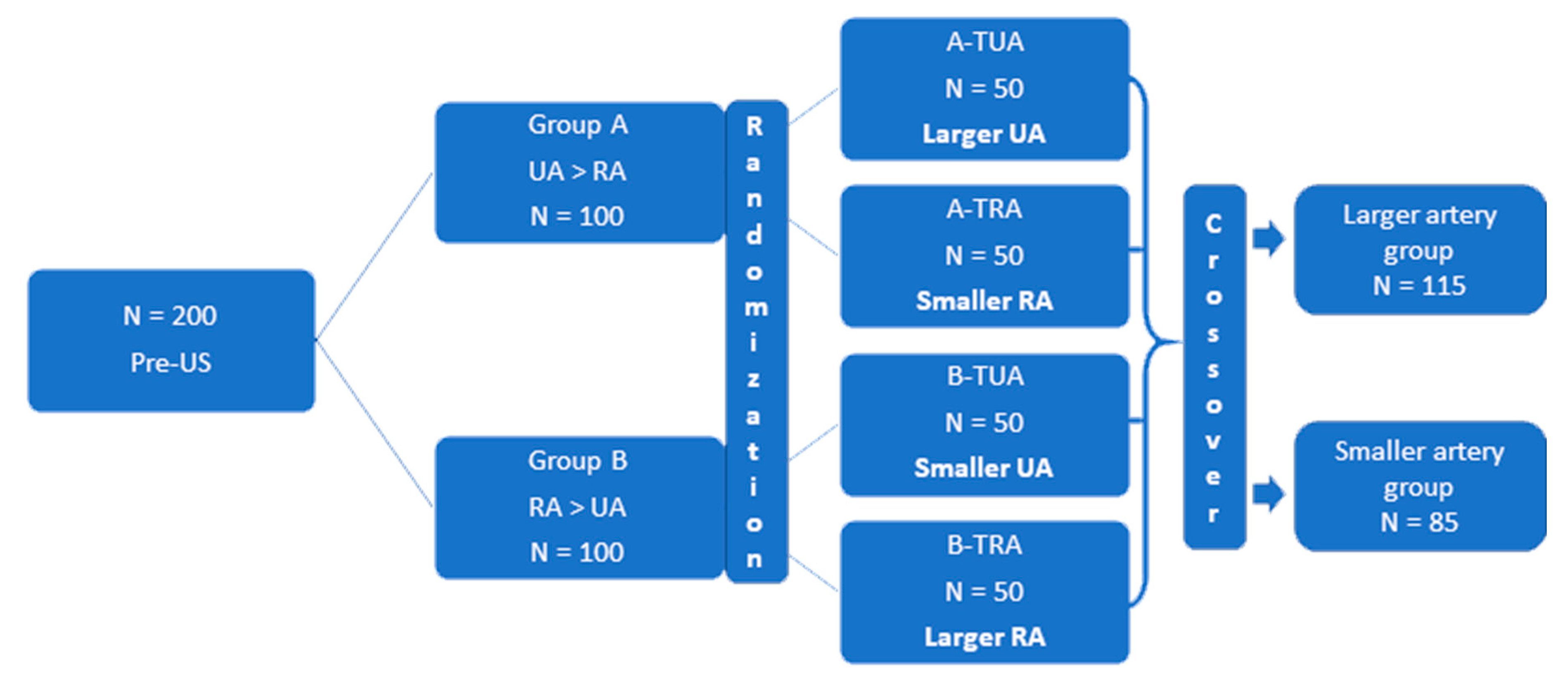
2.1. Study Design
2.1.1. Efficacy of Vascular Access
2.1.2. Safety of Vascular Access
2.2. Statistical Methods
3. Results
3.1. Efficacy: Intention to Treat Analysis
3.2. Safety
4. Discussion
4.1. Comparison with Previous Studies
4.1.1. TRA vs. TUA for CAG/PCI
4.1.2. Preprocedural Ultrasonographic Examination
4.1.3. Efficacy and Safety of TRA and TUA
4.1.4. Forearm Artery Perforation after CAG/PCI
4.1.5. The Use of UA as Vascular Access
4.2. Impact on Daily Practice
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Agostoni, P.; Biondi-Zoccai, G.G.; de Benedictis, M.L.; Rigattieri, S.; Turri, M.; Anselmi, M.; Vassanelli, C.; Zardini, P.; Louvard, Y.; Hamon, M. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures; Systematic overview and meta-analysis of randomized trials. J. Am. Coll. Cardiol. 2004, 44, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Jolly, S.S.; Yusuf, S.; Cairns, J.; Niemelä, K.; Xavier, D.; Widimsky, P.; Budaj, A.; Niemelä, M.; Valentin, V.; Lewis, B.S.; et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): A randomized, parallel group, multicentre trial. Lancet 2011, 377, 1409–1420. [Google Scholar] [CrossRef]
- Pristipino, C.; Trani, C.; Nazzaro, M.S.; Berni, A.; Patti, G.; Patrizi, R.; Pironi, B.; Mazzarotto, P.; Gioffrè, G.; Biondi-Zoccai, G.G.; et al. Prospective registry of vascular access in interventions in Lazio Region Study Group. Major improvement of percutaneous cardiovascular procedure outcomes with radial artery catheterization: Results from the PREVAIL study. Heart 2009, 95, 476–482. [Google Scholar] [CrossRef] [PubMed]
- De Andrade, P.B.; Tebet, M.A.; Nogueira, E.F.; Esteves, V.C.; De Andrade, M.V.A.; Labrunie, A.; Mattos, L.A.P.E. Transulnar approach as an alternative access site for coronary invasive procedures after transradial approach failure. Am. Heart J. 2012, 164, 462–467. [Google Scholar] [CrossRef]
- Hahalis, G.; Tsigkas, G.; Xanthopoulou, I.; Deftereos, S.G.; Ziakas, A.; Raisakis, K.; Pappas, C.; Sourgounis, A.; Grapsas, N.; Davlouros, P.; et al. Transulnar compared with transradial artery approach as a default strategy for coronary procedures: A randomized trial. Circ. Cardiovasc. Interv. 2013, 6, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Gokhroo, R.; Bisht, D.; Padmanabhan, D.; Gupta, S.; Kishor, K.; Ranwa, B. Feasibility of ulnar artery for cardiac catheterization: AJmer ULnar ARtery (AJULAR) catheterization study. Catheter. Cardiovasc. Interv. 2015, 86, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Geng, W.; Fu, X.; Gu, X.; Jiang, Y.; Fan, W.; Wang, Y.; Li, W.; Xing, K.; Liu, C. Safety and feasibility of transulnar versus transradial artery approach for coronary catheterization in non-selective patients. Chin. Med. J. 2014, 127, 1222–1228. [Google Scholar]
- Uhlemann, M.; Möbius-Winkler, S.; Mende, M.; Eitel, I.; Fuernau, G.; Sandri, M.; Adams, V.; Thiele, H.; Linke, A.; Schuler, G.; et al. The Leipzig prospective vascular ultrasound registry in radial artery catheterization: Impact of sheath size on vascular complications. JACC Cardiovasc. Interv. 2012, 5, 36–43. [Google Scholar] [CrossRef]
- Sinha, S.K.; Jha, M.J.; Mishra, V.; Thakur, R.; Goel, A.; Kumar, A.; Singh, A.K.; Sachan, M.; Varma, C.M.; Krishna, V. Radial artery occlusion—Incidence, predictors and long-term outcome after TRAnsradial Catheterization: Clinico-Doppler ultrasound-based study (RAIL-TRAC study). Acta Cardiol. 2017, 72, 318–327. [Google Scholar] [CrossRef] [PubMed]
- Shroff, A.; Gulati, R.; Drachman, D.E.; Feldman, D.N.; Gilchrist, I.C.; Kaul, P.; Lata, K.; Pancholy, S.B.; Panetta, C.J.; Seto, A.H.; et al. SCAI expert consensus statement update on best practices for transradial angiography and intervention. Catheter. Cardiovasc. Interv. 2020, 95, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, O.F.; De Larochellière, R.; Rodés-Cabau, J.; Proulx, G.; Gleeton, O.; Nguyen, C.M.; Déry, J.-P.; Barbeau, G.; Noël, B.; LaRose, E.; et al. Early discharge after transradial stenting of coronary arteries study investigators. A randomized study comparing same-day home discharge and abciximab bolus only to overnight hospitalization and abciximab bolus and infusion after transradial coronary stent implantation. Circulation 2006, 114, 2636–2643. [Google Scholar]
- Mehran, R.; Rao, S.V.; Bhatt, D.L.; Gibson, C.M.; Caixeta, A.; Eikelboom, J.; Kaul, S.; Wiviott, S.D.; Menon, V.; Nikolsky, E.; et al. Standardized bleeding definitions for cardiovascular clinical trials: A consensus report from the bleeding academic research consortium. Circulation 2011, 123, 2736–2747. [Google Scholar] [CrossRef]
- Dahal, K.; Rijal, J.; Lee, J.; Korr, K.S.; Azrin, M. Transulnar versus transradial access for coronary angiography or percutaneous coronary intervention: A meta-analysis of randomized controlled trials. Catheter. Cardiovasc. Interv. 2016, 87, 857–865. [Google Scholar] [CrossRef]
- Fernandez, R.; Zaky, F.; Ekmejian, A.; Curtis, E.; Lee, A. Safety and efficacy of ulnar artery approach for percutaneous cardiac catheterization: Systematic review and meta-analysis. Catheter. Cardiovasc. Interv. 2018, 91, 1273–1280. [Google Scholar] [CrossRef]
- Chugh, S.K.; Chugh, S.; Chugh, Y.; Rao, S.V. Feasibility and utility of pre-procedure ultrasound imaging of the arm to facilitate transradial coronary diagnostic and interventional procedures (PRIMAFACIE-TRI). Catheter. Cardiovasc. Interv. 2013, 82, 64–73. [Google Scholar] [CrossRef]
- Pacha, H.M.; Alahdab, F.; Al-Khadra, Y.; Idris, A.; Rabbat, F.; Darmoch, F.; Soud, M.; Zaitoun, A.; Kaki, A.; Rao, S.V.; et al. Ultrasound-guided versus palpation-guided radial artery catheterization in adult population: A systematic review and meta-analysis of randomized controlled trials. Am. Heart J. 2018, 204, 1–8. [Google Scholar] [CrossRef]
- Pancholy, S.B.; Heck, L.A.; Patel, T. Forearm arterial anatomy and flow characteristics: A prospective observational study. J. Invasive Cardiol. 2015, 27, 218–221. [Google Scholar] [PubMed]
- Saito, S.; Ikei, H.; Hosokawa, G.; Tanaka, S. Influence of the ratio between radial artery inner diameter and sheath outer diameter on radial artery flow after transradial coronary intervention. Catheter. Cardiovasc. Interv. 1999, 46, 173–178. [Google Scholar] [CrossRef]
- Costa, F.; Daemen, J.; Diletti, R.; Kauer, F.; Van Geuns, R.-J.M.; Ligthart, J.; Witberg, K.; Zijlstra, F.; Valgimigli, M.; Van Mieghem, N.M.; et al. The Rotterdam Radial Access Research: Ultrasound-based radial artery evaluation for diagnostic and therapeutic coronary procedures. Circ. Cardiovasc. Interv. 2016, 9, e003129. [Google Scholar] [CrossRef]
- Goel, S.; Cordeiro, N.; Friedman, M. Radial artery perforation complicating percutaneous coronary intervention. Cardiovasc. Revascularization Med. 2019, 20, 26–27. [Google Scholar] [CrossRef]
- Rashid, M.; Kwok, C.S.; Pancholy, S.; Chugh, S.; Kedev, S.A.; Bernat, I.; Ratib, K.; Large, A.; Fraser, D.; Nolan, J.; et al. Radial artery occlusion after transradial interventions: A systematic review and meta-analysis. J. Am. Heart Assoc. 2016, 5, e002686. [Google Scholar] [CrossRef]
- Calviño-Santos, R.A.; Vázquez-Rodríguez, J.M.; Fernández, J.S.; Vázquez-González, N.; Fernández, R.P.; Vázquez-Rey, E.; Castro-Beiras, A. Management of iatrogenic radial artery perforation. Catheter. Cardiovasc. Interv. 2004, 61, 74–78. [Google Scholar] [CrossRef]
- Baumann, F.; Roberts, J.S. Evolving techniques to improve radial/ulnar artery access: Crossover rate of 0.3% in 1000 consecutive patients undergoing cardiac catheterization and/or percutaneous coronary intervention via the wrist. J. Interv. Cardiol. 2015, 28, 396–404. [Google Scholar] [CrossRef]

| Larger UA/RA (n = 115) | Smaller UA/RA (n = 85) | p-Value | |
|---|---|---|---|
| Age, years (mean ± SD) | 68 ± 8 | 68.5 ± 7 | 0.45 |
| Male, n (%) | 64 (56) | 43 (51) | 0.5 |
| BMI, kg/m2 (mean ± SD) | 28.5 ± 4.6 | 28.5 ± 5.5 | 0.73 |
| BSA, m2 (mean ± SD) | 1.95 ± 0.25 | 1.94 ± 0.2 | 0.95 |
| Medical history | |||
| Smoking, n (%) | 28 (24) | 24 (28) | 0.53 |
| Hypertension, n (%) | 113 (98) | 82 (96) | 0.65 |
| Hypercholesterolemia, n (%) | 112 (97) | 79 (92) | 0.17 |
| Peripheral artery disease, n (%) | 23 (20) | 11 (13) | 0.19 |
| Diabetes, n (%) | 38 (33) | 24 (28) | 0.46 |
| Stroke, n (%) | 4 (3) | 4 (5) | 0.72 |
| Renal insufficiency, n (%) | 20 (17) | 10 (12) | 0.27 |
| Myocardial Infarction, n (%) | 22 (19) | 14 (16) | 0.62 |
| CABG, n (%) | 4 (3) | 3 (4) | 1.0 |
| Prior CAG or PCI, n (%) | 28 (29) | 21 (25) | 0.53 |
| Diagnosis upon admission | |||
| Suspected CAD, n (%) | 106 (92) | 78 (92) | 0.9 |
| CHF, n (%) | 3 (3) | 2 (2) | 1.0 |
| Ventricular arrythmia, n (%) | 6 (5) | 5 (6) | 0.83 |
| Preprocedure medications | |||
| Aspirin, n (%) | 112 (97) | 84 (99) | 0.63 |
| Clopidogrel, n (%) | 110 (96) | 82 (96) | 1.0 |
| Warfarin, n (%) | 9 (8) | 4 (5) | 0.56 |
| NOAC, n (%) | 6 (5) | 6 (7) | 0.58 |
| Statin, n (%) | 107 (93) | 80 (94) | 0.76 |
| β-Blocker, n (%) | 107 (93) | 77 (91) | 0.52 |
| Larger UA/RA (n = 115) | Smaller UA/RA (n = 85) | p-Value | |
|---|---|---|---|
| Angiography alone, n (%) | 68 (59) | 57 (67) | 0.25 |
| Angiography and FFR, n (%) | 5 (4) | 1 (1) | 0.19 |
| PCI ad hoc, n (%) | 31 (27) | 24 (28) | 0.84 |
| Elective PCI, n (%) | 11 (10) | 3 (4) | 0.98 |
| TRA, n (%) | 58 (50.4) | 43 (50.6) | 0.91 |
| TUA, n (%) | 57 (49.6) | 42 (50.4) | 0.98 |
| Right radial or ulnar access, n (%) | 101 (88) | 70 (82) | 0.27 |
| Left radial or ulnar access, n (%) | 14 (12) | 15 (18) | 0.27 |
| Fluoroscopy time (min) (mean ± SD) | 5.4 ± 5.2 | 4.9 ± 4.2 | 0.49 |
| Contrast medium (mL) (mean ± SD) | 149 ± 94 | 143 ± 41 | 0.63 |
| Radiation dose of X-ray (mSv) (mean ± SD) | 281 ± 281 | 246 ± 197 | 0.64 |
| Time of compression, (min) (mean ± SD) | 147 ± 31 | 149 ± 33 | 0.49 |
| Nitroglycerin (dose 200 ug) ia, n (%) | 115 (100) | 82 (96) | 1.0 |
| Dose of heparin (IU) (mean ± SD) | 6008 ± 1600 | 5900 ± 1544 | 0.6 |
| Arterial sheath size | |||
| 6-Fr, n (%) | 115 (100) | 85 (100) | 1.0 |
| Diagnostic catheter size | |||
| 6-Fr, n (%) 5-Fr, n (%) | 105 (91) 2 (1.8) | 80 (94) 2 (2) | 0.45 |
| Catheter used for PCI, n (%) | 47 (40) | 32 (37) | |
| 6-Fr, n (%) | 47 (100) | 32 (100) | 1.0 |
| Group A (UA > RA), n = 100 | Group B (RA > UA), n = 100 | |||
|---|---|---|---|---|
| UA | RA | RA | UA | |
| 1st diam. (mm) (mean ± SD) | 2.3 ± 0.4 | 1.9 ± 0.3 | 2.3 ± 0.4 | 1.8 ± 0.3 |
| 2nd diam. (mm) (mean ± SD) | 2.5 ± 0.4 | 2.0 ± 0.4 | 2.4 ± 0.4 | 1.9 ± 0.3 |
| 3rd diam. (mm) (mean ± SD) | 3.0 ± 0.5 | 2.2 ± 0.4 | 2.7 ± 0.5 | 2.4 ± 0.6 |
| Index IxD (mm) (mean ± SD) | 2.6 ± 0.4 | 2.0 ± 0.3 | 2.5 ± 0.3 | 2.0 ± 0.3 |
| PSV (cm/s) (mean ± SD) | 44 ± 11 | 40 ± 11 | 40 ± 12 | 39 ± 11 |
| EDV (cm/s) (mean ± SD) | 6 ± 7 | 6 ± 8 | 6 ± 6 | 5 ± 6 |
| Anatomical abnormalities * n (%) | 3(3) | 8(8) | 6(6) | 7(7) |
| Parameters | Larger UA/RA n = 100 | Smaller UA/RA n = 100 | p-Value |
|---|---|---|---|
| CAG/PCI success n (%) | 98 (98) | 83 (83) | 0.001 |
| Necessity of crossover n (%) | 2 (2) | 17 (17) | 0.001 |
| Necessity of crossover n (%) | 2 (2) | 17 (17) | 0.001 |
| Parameters | Larger UA/RA n = 100 | Smaller UA/RA n = 100 | p-Value |
|---|---|---|---|
| Vessel spasm, n (%) | 0 | 5 (5) | 0.059 |
| Impalpable pulse, n (%) | 0 | 3 (3) | 0.246 |
| Prolonged procedure, n (%) | 2 (2) | 4 (4) | 0.683 |
| Painful procedure, n (%) | 0 | 1 (1) | 0.9 |
| No blood outflow after puncture, n (%) | 0 | 0 | 1.0 |
| Impossible artery puncture, n (%) | 1 (1) | 5 (5) | 0.2 |
| Impossible wire insertion into artery, n (%) | 1 (1) | 11 (11) | 0.005 |
| 24 h Follow-Up | Larger UA/RA (n = 115) | Smaller UA/RA (n = 85) | p-Value |
|---|---|---|---|
| RAO/UAO, n (%) † | 1 (0.9) | 9 (11) | 0.002 * |
| Hematoma (grade 4 in EASY scale), n (%) | 4 (3.5) | 3 (3.5) | 1.0 |
| Stroke/TIA, n (%) | 0 | 1 (1) | 0.2 * |
| Major bleeding, n (%) | 0 | 0 | |
| IPA, n (%) | 1 (1) | 3 (4) | 0.3 ** |
| a-v fistula, n (%) | 2 (2) | 2 (3) | 1.0 ** |
| Significant stenosis of used artery, n (%) | 5 (4) | 8 (9) | 0.2 ** |
| Intra-arterial complications | |||
| Perforation of artery in angiography, n (%) | 10 (9) | 10 (12) | 0.47 |
| 30 day follow-up | |||
| RAO/UAO, n (%) † | 2 (1.7) | 13 (15) | 0.001 ** |
| Hematoma (grade 4 in EASY scale), n (%) | 3 (2.6) | 1 (1.2) | 0.5 |
| Stroke/TIA, n (%) | 0 | 0 | |
| Major bleeding, n (%) | 0 | 0 | |
| IPA, n (%) | 0 | 0 | |
| a-v fistula, n (%) | 0 | 1 | 1.0 |
| Significant stenosis of used artery, n (%) | 7 (6) | 12 (14) | 0.056 * |
| 24 h Follow-Up | OR (95% CI) | p-Value |
|---|---|---|
| Larger UA/RA | 0.07 (0.09–0.61) | 0.016 |
| Perforation of the artery | 7.24 (1.68–31.05) | 0.008 |
| 24 h 30 day follow-up | ||
| Larger UA/RA | 0.025 (0.05–0.12) | 0.001 |
| Perforation of the artery | 10.38 (2.46–43.68) | 0.001 |
| Use of TRA | 9.05 (1.75–46.85) | 0.009 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lewandowski, P.; Zuk, A.; Slomski, T.; Maciejewski, P.; Ramotowski, B.; Budaj, A. Impact of the Use of a Larger Forearm Artery on the Efficacy and Safety of Transradial and Transulnar Access: A Randomized Trial with Preprocedural Ultrasonography. J. Clin. Med. 2020, 9, 3607. https://doi.org/10.3390/jcm9113607
Lewandowski P, Zuk A, Slomski T, Maciejewski P, Ramotowski B, Budaj A. Impact of the Use of a Larger Forearm Artery on the Efficacy and Safety of Transradial and Transulnar Access: A Randomized Trial with Preprocedural Ultrasonography. Journal of Clinical Medicine. 2020; 9(11):3607. https://doi.org/10.3390/jcm9113607
Chicago/Turabian StyleLewandowski, Pawel, Anna Zuk, Tomasz Slomski, Pawel Maciejewski, Bogumil Ramotowski, and Andrzej Budaj. 2020. "Impact of the Use of a Larger Forearm Artery on the Efficacy and Safety of Transradial and Transulnar Access: A Randomized Trial with Preprocedural Ultrasonography" Journal of Clinical Medicine 9, no. 11: 3607. https://doi.org/10.3390/jcm9113607
APA StyleLewandowski, P., Zuk, A., Slomski, T., Maciejewski, P., Ramotowski, B., & Budaj, A. (2020). Impact of the Use of a Larger Forearm Artery on the Efficacy and Safety of Transradial and Transulnar Access: A Randomized Trial with Preprocedural Ultrasonography. Journal of Clinical Medicine, 9(11), 3607. https://doi.org/10.3390/jcm9113607






