The 10-Year Study of the Impact of Particulate Matters on Mortality in Two Transit Cities in North-Eastern Poland (PL-PARTICLES)
Abstract
1. Introduction
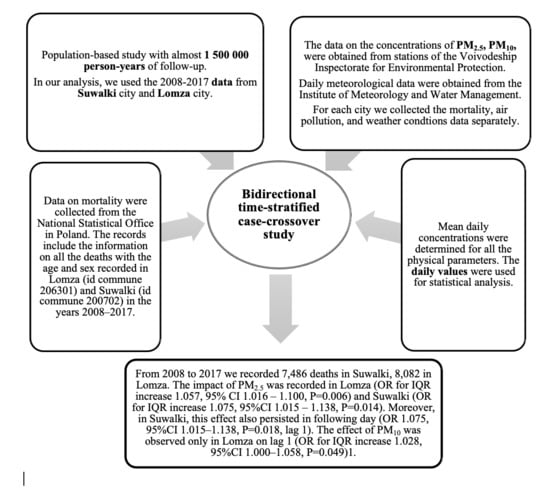
2. Patients and Methods
2.1. Study Design
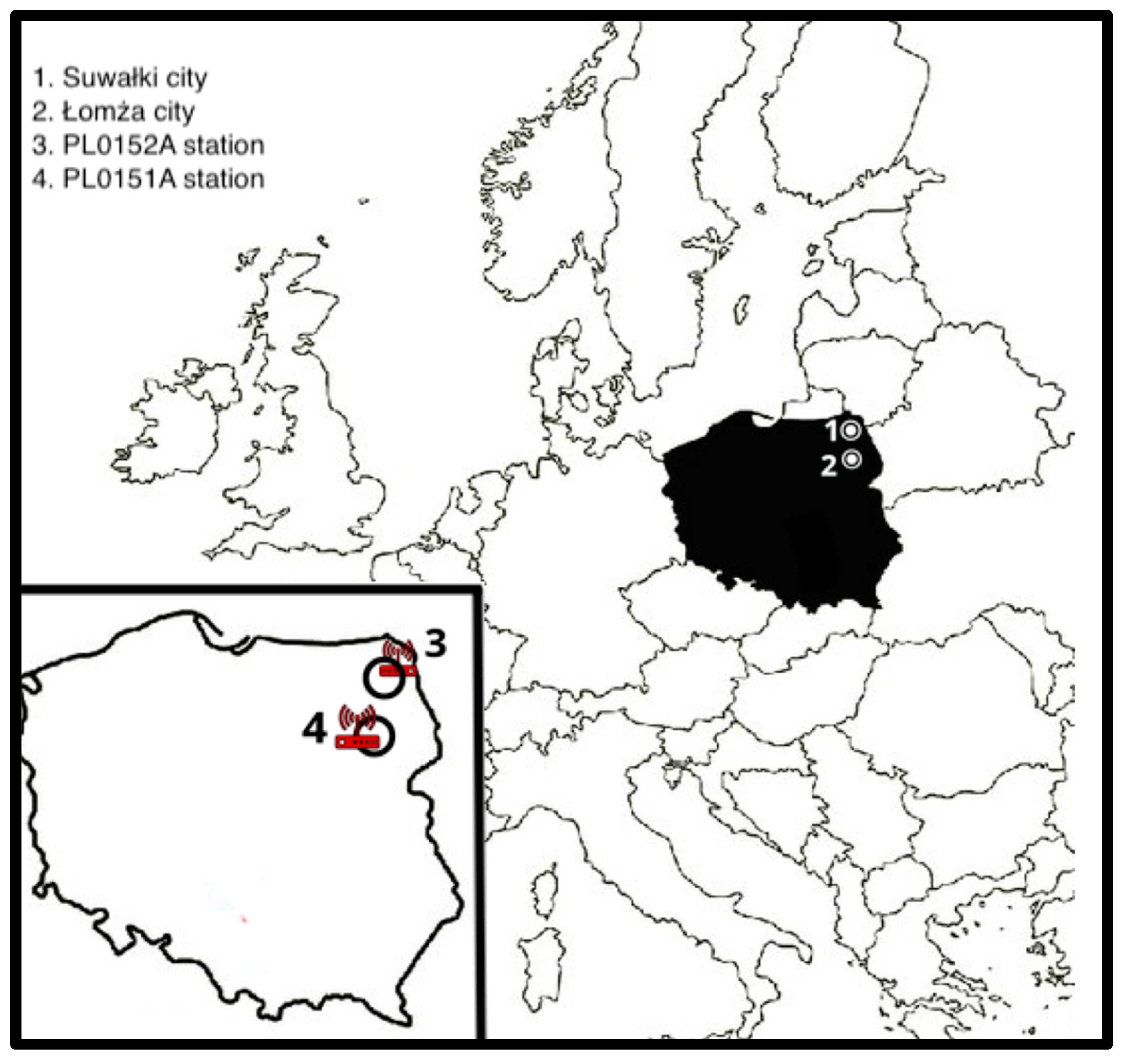
2.2. Region′s Characteristics
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Conflicts of Interest
References
- Bae, S.; Kwon, H.J. Current State of Research on the Risk of Morbidity and Mortality Associated with Air Pollution in Korea. Yonsei Med. J. 2019, 60, 243–256. [Google Scholar] [CrossRef] [PubMed]
- Mokoena, K.K.; Ethan, C.J.; Yu, Y.; Shale, K.; Liu, F. Ambient air pollution and respiratory mortality in Xi’an, China: A time-series analysis. Respir. Res. 2019, 20, 139. [Google Scholar] [CrossRef]
- Carugno, M.; Consonni, D.; Randi, G.; Catelan, D.; Grisotto, L.; Bertazzi, P.A.; Biggeri, A.; Baccini, M. Air pollution exposure, cause-specific deaths and hospitalizations in a highly polluted Italian region. Environ. Res. 2016, 147, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Sanyal, S.; Rochereau, T.; Maesano, C.N.; Com-Ruelle, L.; Annesi-Maesano, I. Long-Term Effect of Outdoor Air Pollution on Mortality and Morbidity: A 12-Year Follow-Up Study for Metropolitan France. Int. J. Environ. Res. Public Health 2018, 15, 2487. [Google Scholar] [CrossRef]
- Anderson, J.O.; Thundiyil, J.G.; Stolbach, A. Clearing the air: A review of the effects of particulate matter air pollution on human health. J. Med. Toxicol. 2012, 8, 166–175. [Google Scholar] [CrossRef]
- Jiang, X.Q.; Mei, X.D.; Feng, D. Air pollution and chronic airway diseases: What should people know and do? J. Thorac. Dis. 2016, 8, E31–E40. [Google Scholar] [CrossRef]
- Chin, M.T. Basic mechanisms for adverse cardiovascular events associated with air pollution. Heart 2015, 101, 253–256. [Google Scholar] [CrossRef]
- Stanaway, J.D.; Afshin, A.; Gakidou, E.; Lim, S.S.; Abate, D.; Abate, K.H.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef]
- Mills, N.L.; Donaldson, K.; Hadoke, P.W.; A Boon, N.; MacNee, W.; Cassee, F.R.; Sandström, T.; Blomberg, A.; E Newby, D. Adverse cardiovascular effects of air pollution. Nat. Clin. Pract. Cardiovasc. Med. 2009, 6, 36–44. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Revision of the European Standard Population Report of Eurostat’s Task Force. Available online: https://ec.europa.eu/eurostat/documents/3859598/5926869/KS-RA-13-028-EN.PDF/e713fa79-1add-44e8-b23d-5e8fa09b3f8f (accessed on 1 July 2020).
- World Health Organization. Ambient (Outdoor) Air Quality and Health (Updated 2 May 2018). Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 1 July 2020).
- Maclure, M. The case-crossover design: A method for studying transient effects on the risk of acute events. Am. J. Epidemiol. 1991, 133, 144–153. [Google Scholar] [CrossRef]
- Janes, H.; Sheppard, L.; Lumley, T. Case-crossover analyses of air pollution exposure data: Referent selection strategies and their implications for bias. Epidemiology 2005, 16, 717–726. [Google Scholar] [CrossRef] [PubMed]
- Altman, D.G.; Bland, J.M. Statistics Notes Interaction revisited: The difference between two estimates. BMJ 2003, 326, 219. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Eurostat: Causes and Occurrence of Deaths in the EU. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/DDN-20190716-1 (accessed on 5 September 2020).
- Feng, B.; Li, L.; Xu, H. PM 2.5-bound polycyclic aromatic hydrocarbons (PAHs) in Beijing: Seasonal variations, sources, and risk assessment. J. Environ. Sci. 2019, 77, 11–19. [Google Scholar] [CrossRef]
- Al-Naiema, I.M.; Yoon, S.; Wang, Y.Q. Source apportionment of fine particulate matter organic carbon in Shenzhen, China by chemical mass balance and radiocarbon methods. Environ. Pollut. 2018, 240, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Park, C.G.; Cho, H.K.; Shin, H.J. Comparison of Mutagenic Activities of Various Ultra-Fine Particles. Toxicol. Res. 2018, 34, 163–172. [Google Scholar] [CrossRef]
- Cho, H.K.; Park, C.G.; Shin, H.J. Comparison of the in vitro toxicological activity of various particulate matter. Toxicol. Ind. Health 2018, 34, 99–109. [Google Scholar] [CrossRef]
- Campen, M.J.; Lund, A.K.; Doyle-Eisele, M.L. A comparison of vascular effects from complex and individual air pollutants indicates a role for monoxide gases and volatile hydrocarbons. Environ. Health Perspect. 2010, 118, 921–927. [Google Scholar] [CrossRef]
- Yorifuji, T.; Kashima, S.; Doi, H. Fine-particulate Air Pollution from Diesel Emission Control and Mortality Rates in Tokyo: A Quasi-experimental Study. Epidemiology 2016, 27, 769–778. [Google Scholar] [CrossRef]
- Wilker, E.H.; Preis, S.R.; Beiser, A.S. Long-term exposure to fine particulate matter, residential proximity to major roads and measures of brain structure. Stroke 2015, 46, 1161–1166. [Google Scholar] [CrossRef]
- Zeng, W.; Zhang, Y.; Wang, L. Ambient fine particulate pollution and daily morbidity of stroke in Chengdu, China. PLoS ONE 2018, 13, e0206836. [Google Scholar] [CrossRef]
- Zhang, R.; Liu, G.; Jiang, Y. Acute Effects of Particulate Air Pollution on Ischemic Stroke and Hemorrhagic Stroke Mortality. Front. Neurol. 2018, 9, 827. [Google Scholar] [CrossRef]
- Shi, Y.; Matsunaga, T.; Yamaguchi, Y. Long-term trends and spatial patterns of PM 2.5-induced premature mortality in South and Southeast Asia from 1999 to 2014. Sci. Total. Environ. 2018, 631–632, 1504–1514. [Google Scholar] [CrossRef]
- Kowalska, M.; Kocot, K. Short-term exposure to ambient fine particulate matter (PM2.5 and PM10) and the risk of heart rhythm abnormalities and stroke. Postepy Hig. Med. Dosw. 2016, 70, 1017–1025. [Google Scholar] [CrossRef]
- Shah, A.S.; Lee, K.K.; McAllister, D.A. Short term exposure to air pollution and stroke: Systematic review and meta-analysis. BMJ 2015, 350, h1295. [Google Scholar] [CrossRef]
- Li, W.; Cao, Y.; Li, R. The spatial variation in the effects of air pollution on cardiovascular mortality in Beijing, China. J. Expo. Sci. Environ. Epidemiol. 2018, 28, 297–304. [Google Scholar] [CrossRef]
- Pun, V.C.; Kazemiparkouhi, F.; Manjourides, J. Long-Term PM2.5 Exposure and Respiratory, Cancer, and Cardiovascular Mortality in Older US Adults. Am. J. Epidemiol. 2017, 186, 961–969. [Google Scholar] [CrossRef]
- Liu, C.; Chen, R.; Sera, F. Ambient Particulate Air Pollution and Daily Mortality in 652 Cities. N. Engl. J. Med. 2019, 381, 705–715. [Google Scholar] [CrossRef]
- Li, M.H.; Fan, L.C.; Mao, B. Short-term Exposure to Ambient Fine Particulate Matter Increases Hospitalizations and Mortality in COPD: A Systematic Review and Meta-analysis. Chest 2016, 149, 447–458. [Google Scholar] [CrossRef]
- Xing, Y.F.; Xu, Y.H.; Shi, M.H. The impact of PM2.5 on the human respiratory system. J. Thorac. Dis. 2016, 8, E69–E74. [Google Scholar] [CrossRef]
- Wang, L.; Cheng, H.; Wang, D. Airway Microbiome Is Associated with Respiratory Functions and Responses to Ambient Particulate Matter Exposure. Ecotoxicol. Environ. Saf. 2019, 167, 269–277. [Google Scholar] [CrossRef]
- Atkinson, R.W.; Kang, S.; Anderson, H.R. Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions: A systematic review and meta-analysis. Thorax 2014, 69, 660–665. [Google Scholar] [CrossRef]
- Kim, S.Y.; Peel, J.L.; Hannigan, M.P. The temporal lag structure of short-term associations of fine particulate matter chemical constituents and cardiovascular and respiratory hospitalizations. Environ. Health Perspect. 2012, 120, 1094–1099. [Google Scholar] [CrossRef] [PubMed]
- Guaita, R.; Pichiule, M.; Maté, T. Short-term impact of particulate matter (PM(2.5)) on respiratory mortality in Madrid. Int. J. Environ. Health Res. 2011, 21, 260–274. [Google Scholar] [CrossRef] [PubMed]
- Meister, K.; Johansson, C.; Forsberg, B. Estimated short-term effects of coarse particles on daily mortality in Stockholm, Sweden. Environ. Health Perspect. 2012, 120, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Janssen, N.A.; Fischer, P.; Marra, M. Short-term effects of PM2.5, PM10 and PM2.5-10 on daily mortality in The Netherlands. Sci. Total. Environ. 2013, 463–464, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, R.W.; Fuller, G.W.; Anderson, H.R. Urban ambient particle metrics and health: A time-series analysis. Epidemiology 2010, 21, 501–511. [Google Scholar] [CrossRef]
- Choi, Y.; Kim, H.; Lee, J.T. Temporal variability of short term effects of PM 10 on mortality in Seoul, Korea. Sci. Total. Environ. 2018, 644, 122–128. [Google Scholar] [CrossRef]
- Renzi, M.; Forastiere, F.; Calzolari, R. Short-term effects of desert and non-desert PM 10 on mortality in Sicily, Italy. Environ. Int. 2018, 120, 472–479. [Google Scholar] [CrossRef]
- Yoo, S.E.; Park, J.S.; Lee, S.H. Comparison of Short-Term Associations between PM 2.5 Components and Mortality across Six Major Cities in South Korea. Int. J. Environ. Res. Public Health 2019, 16, 2872. [Google Scholar] [CrossRef]
- Wang, Y.; Shi, Z.; Shen, F. Associations of daily mortality with short-term exposure to PM2.5 and its constituents in Shanghai, China. Chemosphere 2019, 233, 879–887. [Google Scholar] [CrossRef]
- Liu, M.; Xue, X.; Zhou, B. Population susceptibility differences and effects of air pollution on cardiovascular mortality: Epidemiological evidence from a time-series study. Environ. Sci. Pollut. Res. Int. 2019, 26, 15943–15952. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Russell, A.; Mulholland, J. Using cell phone location to assess misclassification errors in air pollution exposure estimation. Environ. Pollut. 2018, 233, 261–266. [Google Scholar] [CrossRef] [PubMed]
| Suwałki | Łomża | p | |
|---|---|---|---|
| Total deaths, N | 7486 | 8082 | |
| Male, % (N) | 54.1 (4055) | 54.5 (4408) | 0.640 |
| Mean age (SD) | 71.7 (16.6) | 72.7 (15.7) | <0.001 |
| CDR (100,000 population/year) | 1079.5 | 1288.1 | <0.001 |
| SDR (100,000 population/year) | 1638.1 | 1944.6 | <0.001 |
| Suwałki | Łomża | p | |
|---|---|---|---|
| All, % (N) | 100 (7486) | 100 (8082) | N/A |
| Cardiovascular deaths, % (N) | 36.4 (2724) | 41.2 (3328) | <0.001 |
| Pulmonary deaths, % (N) | 7.3 (549) | 6.5 (528) | <0.001 |
| Chronic ischemic heart disease, % (N) | 8.5 (633) | 9.1 (733) | 0.176 |
| Cerebral infarction, % (N) | 5.8 (432) | 9.2 (744) | <0.001 |
| Heart disease-unspecified, % (N) | 5.0 (372) | 3.5 (285) | <0.001 |
| Myocardial infarction, % (N) | 3.1 (232) | 3.9 (315) | 0.007 |
| Intracerebral hemorrhage, % (N) | 2.3 (174) | 2.7 (219) | 0.126 |
| Hypertensive heart disease, % (N) | 2.2 (168) | 1.8 (144) | 0.040 |
| Heart failure, % (N) | 1.9 (141) | 3.4 (276) | <0.001 |
| Malignant neoplasm of bronchus and lung, % (N) | 8.0 (597) | 6.4 (518) | <0.001 |
| Instantaneous death, % (N) | 2.6 (196) | 2.8 (225) | 0.524 |
| Chronic obstructive pulmonary disease, % (N) | 2.6 (193) | 3.2 (258) | 0.022 |
| Pneumonia, % (N) | 2.5 (188) | 2.3 (183) | 0.313 |
| Diabetes mellitus, % (N) | 2.1 (160) | 2.6 (206) | 0.090 |
| Malignant neoplasm of breast, % (N) | 2.1 (157) | 1.6 (127) | 0.014 |
| Malignant neoplasm of colon, % (N) | 2.0 (152) | 1.9 (152) | 0.121 |
| Malignant neoplasm of prostate, % (N) | 2.0 (148) | 1.7 (137) | 0.190 |
| Senility, % (N) | 1.9 (139) | 2.2 (176) | 0.155 |
| Suicide, % (N) | 1.8 (132) | 0.8 (62) | <0.001 |
| Atherosclerosis, % (N) | 1.7 (125) | 1.8 (146) | 0.515 |
| Malignant neoplasm of gastric, % (N) | 1.6 (116) | 1.4 (115) | 0.514 |
| Other, % (N) | 40.5 (3031) | 37.9 (3061) | <0.001 |
| Variables | PM2.5 µg/m3 | PM10 µg/m3 | Temp. °C | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Suwałki | Łomża | p | Suwałki | Łomża | p | Suwałki | Łomża | p | |
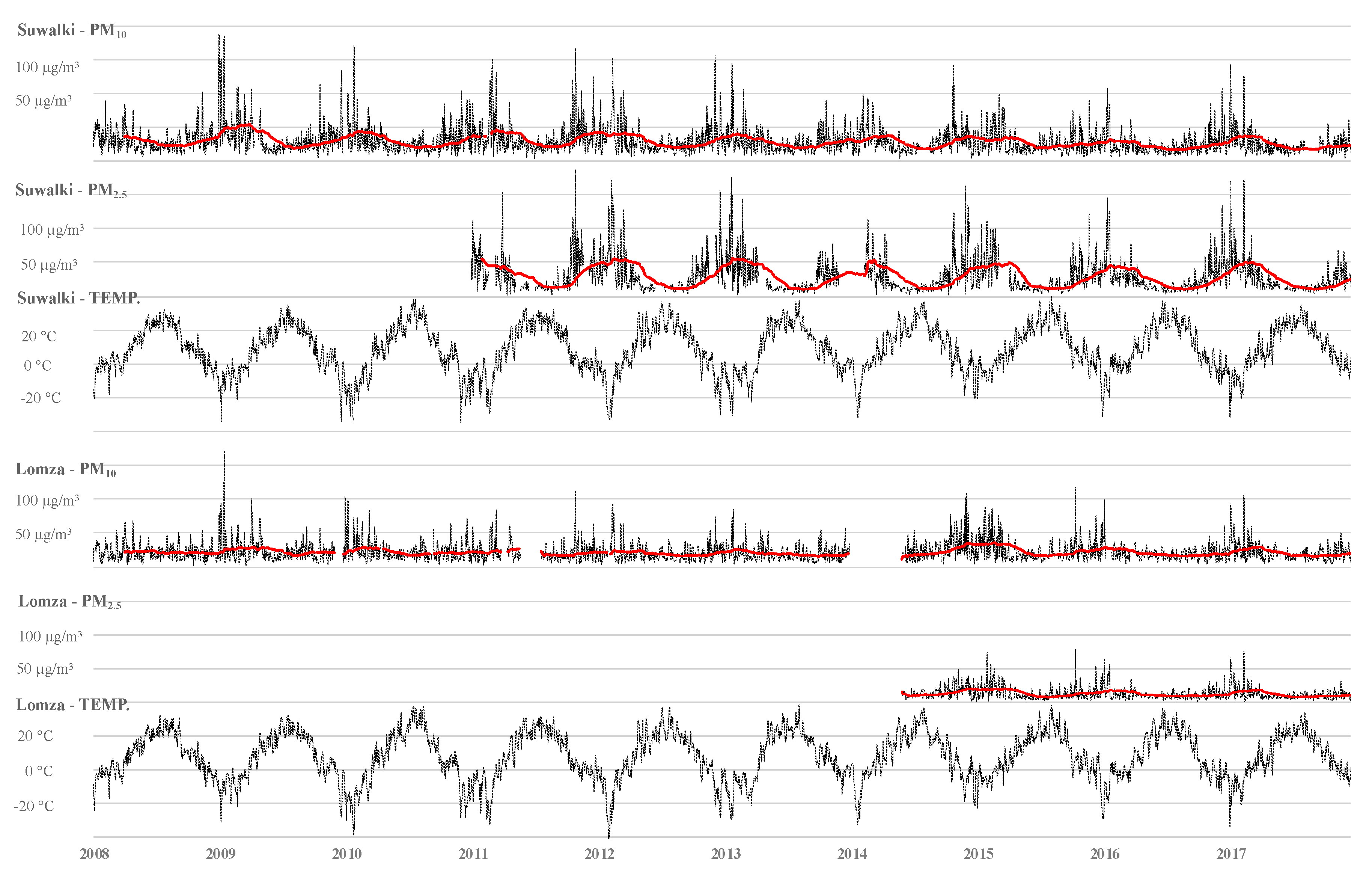
| Days with observation; N, (%) | 1309 (35.8) | 2230 (61.1) | <0.001 | 3313 (90.7) | 3533 (96.7) | <0.001 | 3653 (100) | 3653 (100) | N/A |
| 2008; mean/day (SD) | N/D | N/D | N/A | 21.5 (11.6) | 31.2 (19.1) | <0.001 | 8.0 (7.2) | 8.5 (7.3) | 0.346 |
| 2009; mean/day (SD) | N/D | N/D | N/A | 23.7 (18.2) | 34.1 (25.1) | <0.001 | 6.9 (8.6) | 7.2 (8.6) | 0.559 |
| 2010; mean/day (SD) | N/D | N/D | N/A | 22.1 (13.3) | 29.9 (19.8) | <0.001 | 6.3 (10.7) | 6.5 (10.5) | 0.754 |
| 2011; mean/day (SD) | N/D | 33.02 (25.6) | N/A | 21.4 (14.2) | 34.0 (23.8) | <0.001 | 7.4 (9.0) | 8.1 (8.9) | 0.346 |
| 2012; mean/day (SD) | N/D | 33.2 (29.4) | N/A | 20.2 (12.8) | 29.9 (20.1) | <0.001 | 6.6 (9.8) | 7.3 (9.9) | 0.350 |
| 2013; mean/day (SD) | N/D | 27.9 (24.7) | N/A | 19.1 (11.2) | 27.1 (15.7) | <0.001 | 7.2 (9.1) | 7.7 (9.0) | 0.535 |
| 2014; mean/day (SD) | 15.1 (8.7) | 28.0 (24.5) | <0.001 | 25.9 (16.8) | 29.4 (18.0) | 0.007 | 7.8 (8.8) | 8.2 (8.7) | 0.551 |
| 2015; mean/day (SD) | 13.2 (10.8) | 26.6 (21.8) | <0.001 | 24.22 (16.72) | 26.1 (15.6) | 0.004 | 8.3 (7.4) | 9.1 (7.7) | 0.218 |
| 2016; mean/day (SD) | 11.6 (8.02) | 25.9 (21.2) | <0.001 | 19.3 (10.0) | 23.6 (14.5) | <0.001 | 7.6 (8.5) | 8.2 (8.4) | 0.272 |
| 2017; mean/day (SD) | 11.4 (8.5) | 25.6 (21.8) | <0.001 | 21.0 (13.2) | 24.8 (16.7) | <0.001 | 7.5 (7.9) | 8.4 (8.1) | 0.108 |
| Total; mean/day (SD) | 12.6 (9.2) | 28.4 (24.3) | <0.001 | 21.7 (14.0) | 29.0 (19.4) | <0.001 | 7.4 (8.8) | 7.9 (8.8) | 0.009 |
| 1st quartile | 6.6 | 12.2 | <0.001 | 12.5 | 16.9 | <0.001 | 1.2 | 1.6 | 0.009 |
| Daily median | 9.9 | 20.0 | <0.001 | 18.1 | 24.0 | <0.001 | 7.2 | 7.7 | 0.009 |
| 3rd quartile | 15.5 | 37.4 | <0.001 | 27.0 | 35.0 | <0.001 | 14.6 | 15.3 | 0.009 |
| IQR | 9.0 | 25.2 | <0.001 | 14.5 | 18.0 | <0.001 | 13.4 | 13.7 | 0.009 |
| Exceed daily mean WHO guideline; N (%) | 110 (8.4) | 908 (40.7) | <0.001 | 139 (4.2) | 345 (9.8) | <0.001 | N/A | N/A | N/A |
| PM2.5 µg/m3 | r = 0.518; p < 0.001 | r = −0.608; p < 0.001 |
| r = 0.668; p < 0.001 | PM10 µg/m3 | r = −0.303; p < 0.001 |
| r = −0.268; p < 0.001 | r = −0.243; p < 0.001 | Temperature °C |
| Variables | Suwałki | Łomża | Ratio of Odds Ratio | |||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | ROR (95% CI) | p | |||
| Total mortality | LAG 0 | PM2.5 | 1.044 (1.001–1.089) | 0.04 | 1.061 (1.017–1.105) | 0.006 | 0.984 (0.972–1.044) | 0.29 |
| PM10 | 1.024 (0.995–1.054) | 0.10 | 1.018 (0.991–1.047) | 0.21 | 1.005 (0.966–1.047) | 0.38 | ||
| LAG 1 | PM2.5 | 1.027 (0.981–1.075) | 0.27 | 1.029 (0.988–1.071) | 0.17 | 0.998 (0.339–1.061) | 0.48 | |
| PM10 | 1.006 (0.978–1.036) | 0.66 | 1.028 (1.000–1.058) | 0.049 | 0.977 (0.939–1.017) | 0.14 | ||
| LAG 2 | PM2.5 | 1.005 (0.961–1.052) | 0.83 | 1.036 (0.995–1.078) | 0.82 | 0.971 (0.913–1.032) | 0.17 | |
| PM10 | 1.034 (1.005–1.064) | 0.02 | 1.030 (1.001–1.060) | 0.04 | 1.004 (0.965–1.045) | 0.43 | ||
| Cardiovascular mortality | LAG 0 | PM2.5 | 1.085 (1.005–1.171) | 0.04 | 1.086 (1.020–1.156) | 0.01 | 0.999 (0.905–1.103) | 0.50 |
| PM10 | 1.056 (1.006–1.107) | 0.03 | 1.022 (0.979–1.067) | 0.33 | 1.033 (0.972–1.098) | 0.15 | ||
| LAG 1 | PM2.5 | 1.034 (0.957–1.116) | 0.39 | 1.029 (0.967–1.095) | 0.37 | 1.005 (0.910–1.109) | 0.46 | |
| PM10 | 1.004 (0.957–1.054) | 0.86 | 1.034 (0.991–1.080) | 0.13 | 0.971 (0.909–1.036) | 0.19 | ||
| LAG 2 | PM2.5 | 1.014 (0.939–1.094) | 0.73 | 0.992 (0.932–1.056) | 0.80 | 0.981 (0.898–1.071) | 0.33 | |
| PM10 | 1.025 (0.977–1.076) | 0.31 | 1.008 (0.965–1.053) | 0.72 | 1.017 (0.952–1.085) | 0.31 | ||
| Pulmonary mortality | LAG 0 | PM2.5 | 1.161 (0.987–1.365) | 0.072 | 1.130 (0.967–1.320) | 0.12 | 1.027 (0.821–1.286) | 0.41 |
| PM10 | 1.023 (0.916–1.141) | 0.68 | 1.011 (0.906–1.128) | 0.87 | 1.012 (0.866–1.181) | 0.44 | ||
| LAG 1 | PM2.5 | 1.040 (0.885–1.221) | 0.64 | 1.163 (1.021–1.380) | 0.03 | 0.894 (0.717–1.115) | 0.16 | |
| PM10 | 0.979 (0.879–1.091) | 0.69 | 1.013 (0.904–1.135) | 0.82 | 0.966 (0.826–1.131) | 0.33 | ||
| LAG 2 | PM2.5 | 0.898 (0.759–1.062) | 0.21 | 1.073 (0.921–1.251) | 0.37 | 0.837 (0.667–1.050) | 0.06 | |
| PM10 | 0.951 (0.850–1.064) | 0.38 | 1.044 (0.933–1.168) | 0.45 | 0.911 (0.779–1.064) | 0.12 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuźma, Ł.; Dąbrowski, E.J.; Kurasz, A.; Bachórzewska-Gajewska, H.; Dobrzycki, S. The 10-Year Study of the Impact of Particulate Matters on Mortality in Two Transit Cities in North-Eastern Poland (PL-PARTICLES). J. Clin. Med. 2020, 9, 3445. https://doi.org/10.3390/jcm9113445
Kuźma Ł, Dąbrowski EJ, Kurasz A, Bachórzewska-Gajewska H, Dobrzycki S. The 10-Year Study of the Impact of Particulate Matters on Mortality in Two Transit Cities in North-Eastern Poland (PL-PARTICLES). Journal of Clinical Medicine. 2020; 9(11):3445. https://doi.org/10.3390/jcm9113445
Chicago/Turabian StyleKuźma, Łukasz, Emil Julian Dąbrowski, Anna Kurasz, Hanna Bachórzewska-Gajewska, and Sławomir Dobrzycki. 2020. "The 10-Year Study of the Impact of Particulate Matters on Mortality in Two Transit Cities in North-Eastern Poland (PL-PARTICLES)" Journal of Clinical Medicine 9, no. 11: 3445. https://doi.org/10.3390/jcm9113445
APA StyleKuźma, Ł., Dąbrowski, E. J., Kurasz, A., Bachórzewska-Gajewska, H., & Dobrzycki, S. (2020). The 10-Year Study of the Impact of Particulate Matters on Mortality in Two Transit Cities in North-Eastern Poland (PL-PARTICLES). Journal of Clinical Medicine, 9(11), 3445. https://doi.org/10.3390/jcm9113445