Radiostereometric Analysis Allows Assessment of the Stability and Inducible Displacement of Pelvic Ring Disruptions during Healing: A Case Series
Abstract
1. Introduction
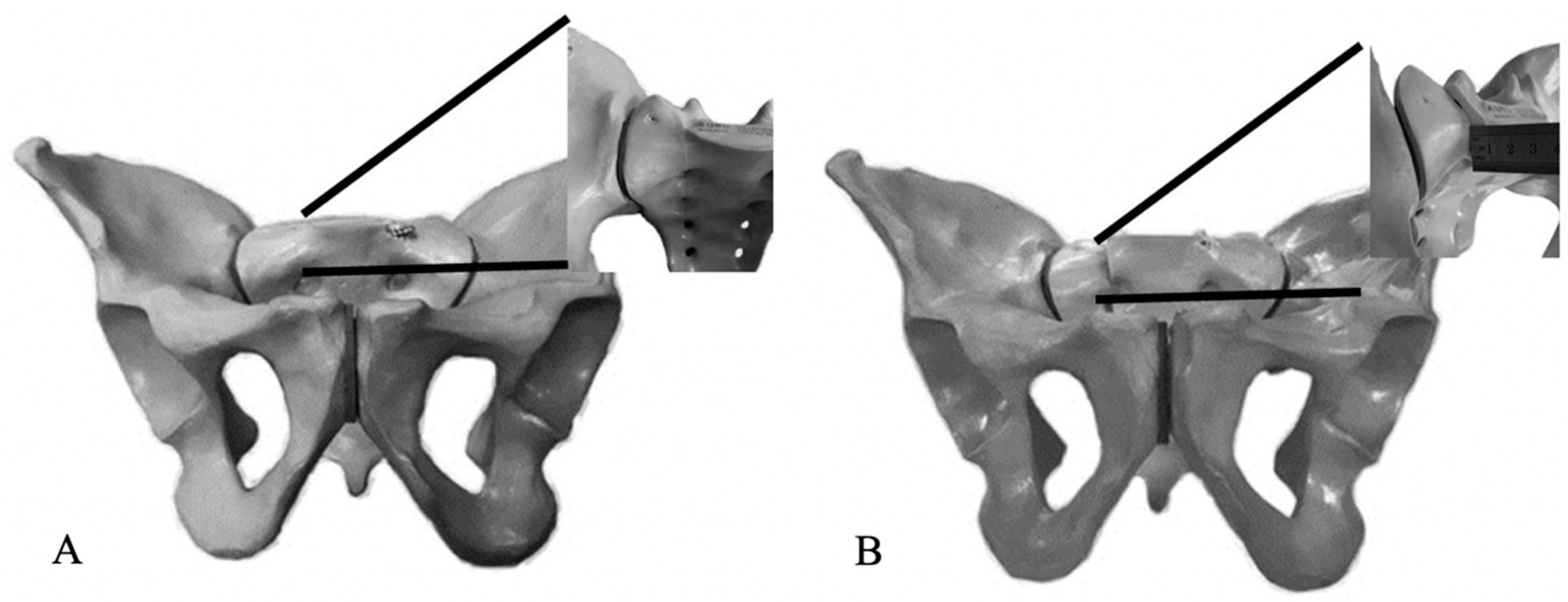
2. Experimental Section
3. Results
3.1. Demographics
3.2. Clinical Results
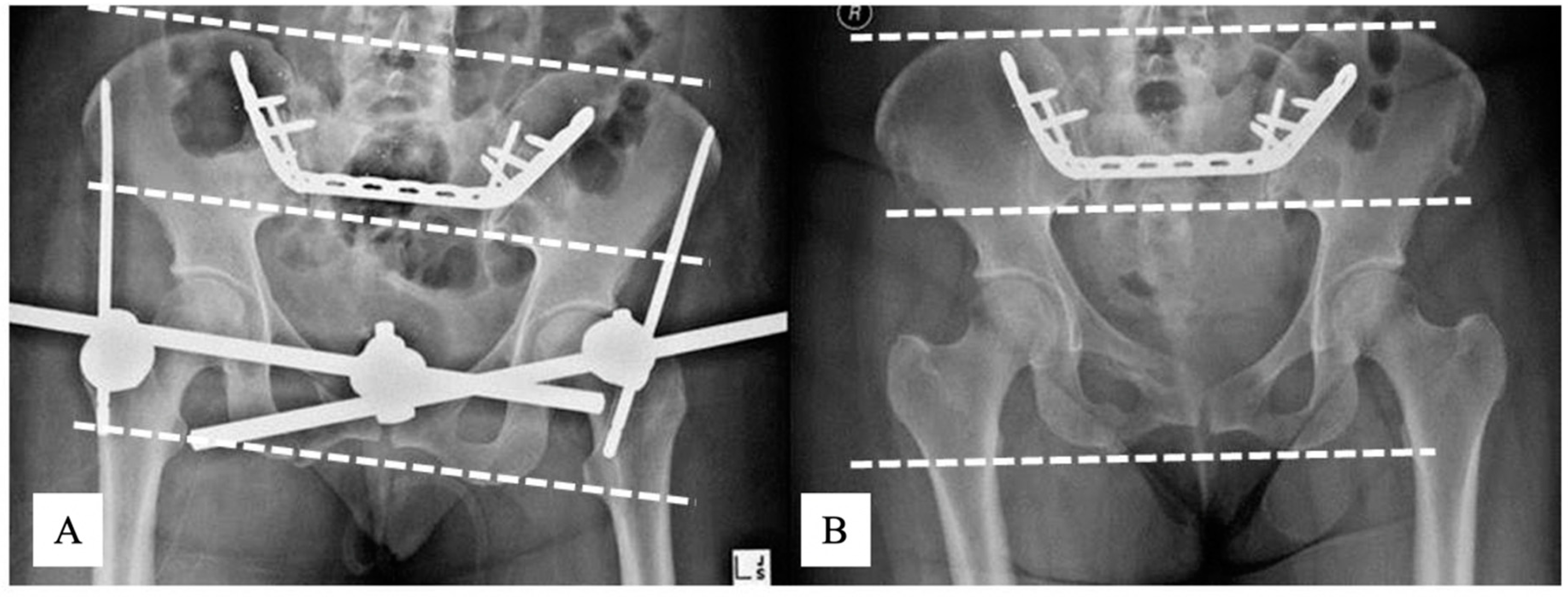
3.3. Radiographic Results
3.4. RSA
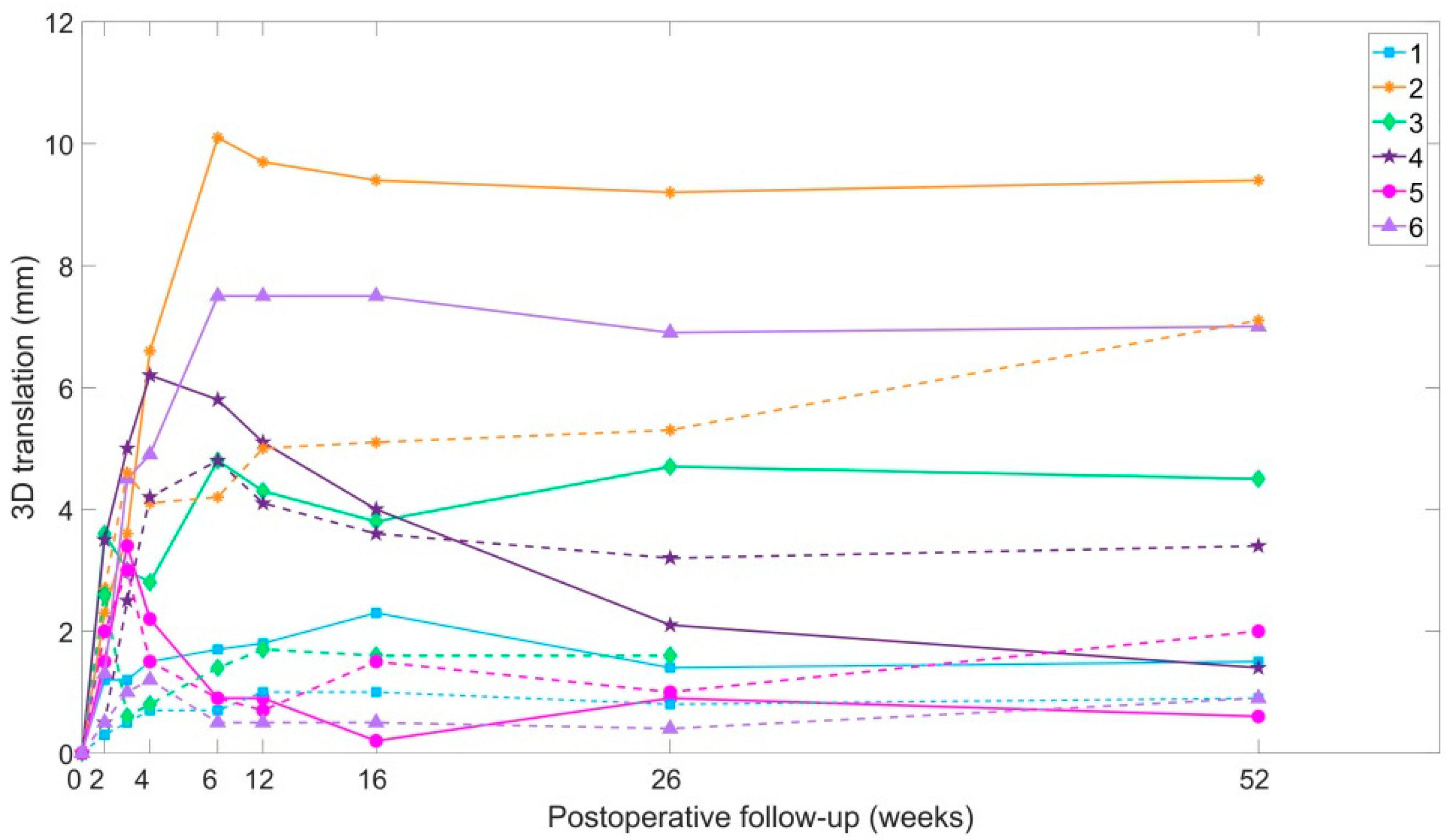
3.4.1. D Fracture Fragment Displacement over Time
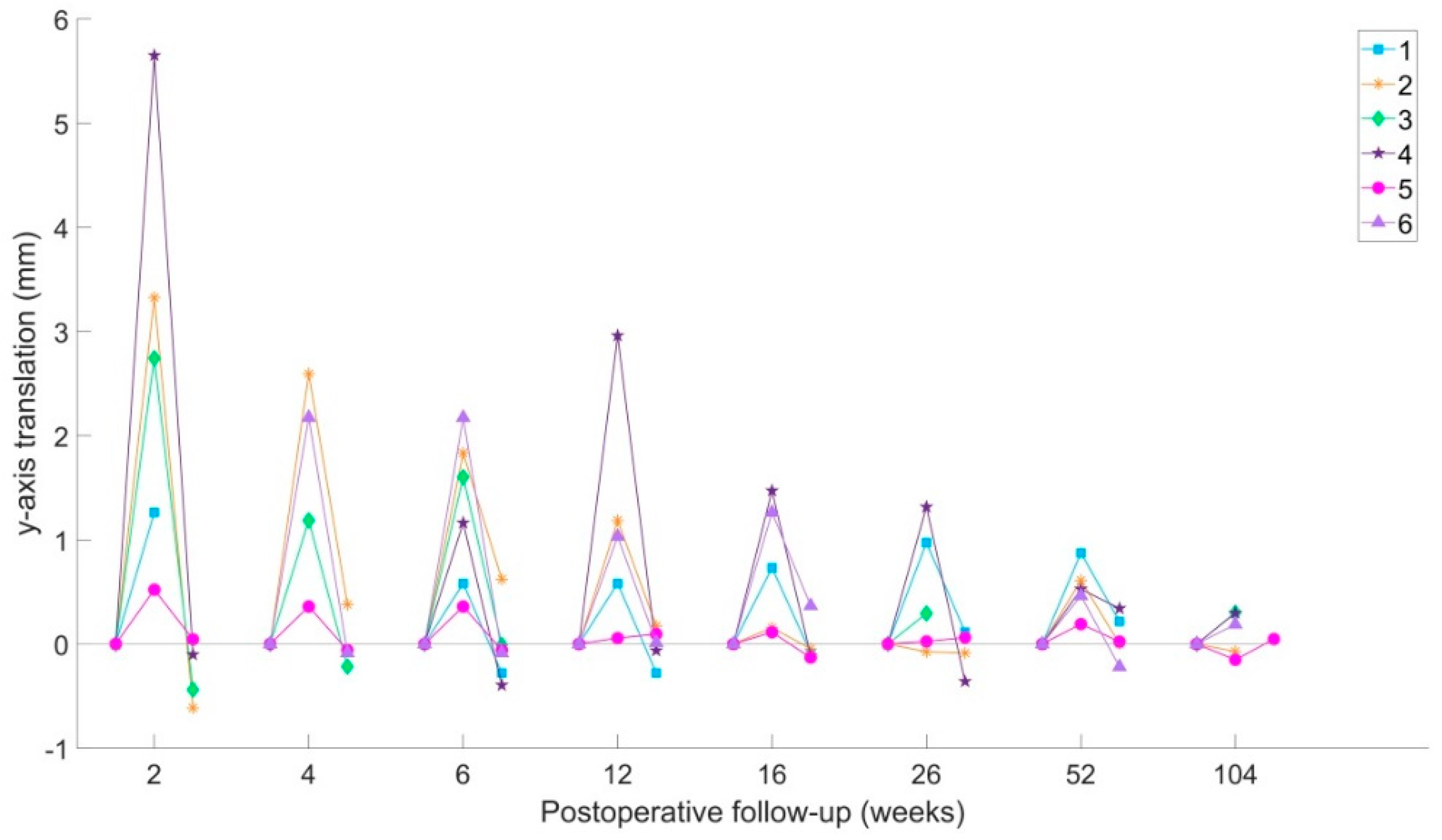
3.4.2. Y-Axis Translation
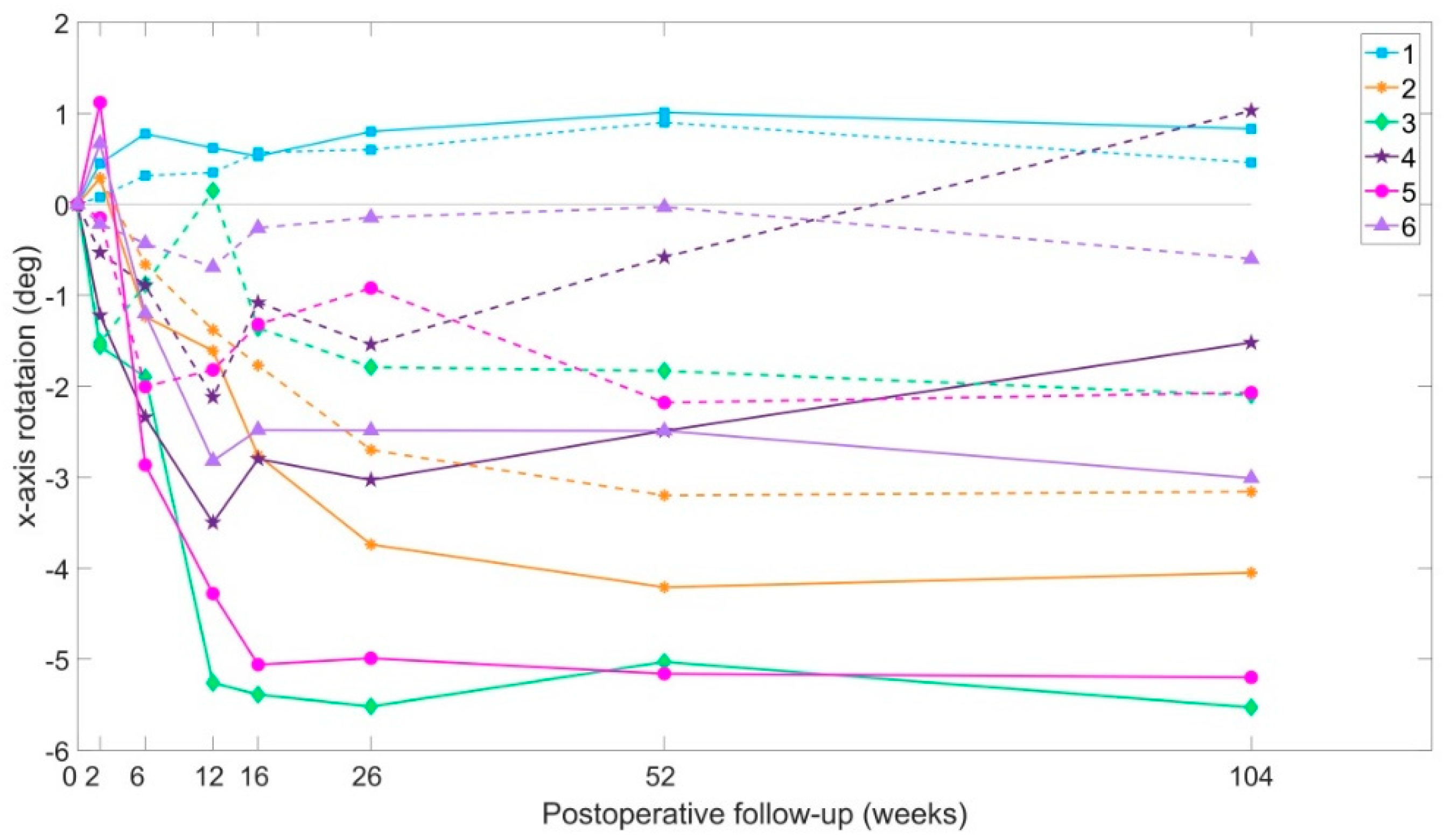
3.4.3. X-Axis Rotation
3.4.4. Pelvic Displacement Caused by the Removal of the External Fixator
3.5. DL-RSA Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Pohlemann T: Tscherne, H.; Baumgärtel, F.; Egbers, H.J.; Euler, E.; Maurer, F.; Fell, M.; Mayr, E.; Quirini, W.W.; Schlickewei, W. Pelvic fractures: Epidemiology, therapy and long-term outcome. Overview of the multicenter study of the Pelvis Study Group. Unfallchirurg 1996, 99, 160. [Google Scholar]
- Schmal, H.; Froberg, L.; Larsen, M.S.; Südkamp, N.P.; Pohlemann, T.; Aghayev, E.; Goodwin Burri, K. Evaluation of strategies for the treatment of type B and C pelvic fractures. Bone Joint J. 2018, 100, 973–983. [Google Scholar] [CrossRef] [PubMed]
- Tile, M. Pelvic ring fractures: Should they be fixed? J. Bone Joint Surg. Ser. B 1988, 70, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ochs, B.G.; Marintschev, I.; Hoyer, H.; Rolauffs, B.; Culemann, U.; Pohlemann, T.; Stuby, F.M. Changes in the treatment of acetabular fractures over 15 years: Analysis of 1266 cases treated by the German Pelvic Multicentre Study Group (DAO/DGU). Injury 2010, 41, 839–851. [Google Scholar] [CrossRef] [PubMed]
- Kerschbaum, M.; Hausmann, N.; Worlicek, M.; Pfeifer, C.; Nerlich, M.; Schmitz, P. Patient-related outcome of unstable pelvic ring fractures stabilized with a minimal invasive screw-rod system. Health Qual. Life Outcomes 2017, 15, 248. [Google Scholar] [CrossRef]
- Bott, A.; Odutola, A.; Halliday, R.; Acharya, M.R.; Ward, A.; Chesser, T.J.S. Long-Term Patient-Reported Functional Outcome of Polytraumatized Patients with Operatively Treated Pelvic Fractures. J. Orthop. Trauma 2019, 33, 64–70. [Google Scholar] [CrossRef]
- Tornetta, P.; Matta, J.M. Outcome of operatively treated unstable posterior pelvic ring disruptions. Clin. Orthop. Relat. Res. 1996, 186–193. [Google Scholar] [CrossRef]
- Lindahl, J.; Hirvensalo, E. Outcome of operatively treated type-C injuries of the pelvic ring. Acta. Orthop. 2005, 76, 667–678. [Google Scholar] [CrossRef]
- Rickman, M.; Link, B.; Solomon, L.B. Patient Weight-bearing after Pelvic Fracture Surgery-A Systematic Review of the Literature: What is the Modern Evidence Base? Strateg. Trauma Limb. Reconstr. 2019, 14, 32–39. [Google Scholar] [CrossRef]
- Parry, S.M.; Puthucheary, Z.A. The impact of extended bed rest on the musculoskeletal system in the critical care environment. Extrem. Physiol. Med. 2015, 4, 16. [Google Scholar] [CrossRef]
- Nystrom, L.M.; McKinley, T.O.; Marsh, J.L. Accuracy in radiographic assessment of pelvic ring fracture deformity: Analysis of current methods. J. Orthop. Trauma 2013, 27, 708–715. [Google Scholar] [CrossRef] [PubMed]
- Griffin, D.R.; Starr, A.J.; Reinert, C.M.; Jones, A.L.; Whitlock, S. Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: Does posterior injury pattern predict fixation failure? J. Orthop. Trauma 2006, 20, S30–S36. [Google Scholar] [CrossRef] [PubMed]
- Keating, J.F. Early fixation of the vertically unstable pelvis: The role of iliosacral screw fixation of the posterior lesion. J. Orthop. Trauma 1998, 13, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Lefaivre, K.A.; Blachut, P.A.; Starr, A.J.; Slobogean, G.P.; O’Brien, P.J. Radiographic displacement in pelvic ring disruption: Reliability of 3 previously described measurement techniques. J. Orthop. Trauma 2014, 28, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Schicho, A.; Schmidt, S.A.; Seeber, K.; Olivier, A.; Richter, P.H.; Gebhard, F. Pelvic X-ray misses out on detecting sacral fractures in the elderly—Importance of CT imaging in blunt pelvic trauma. Injury 2016, 47, 707–710. [Google Scholar] [CrossRef] [PubMed]
- Boontanapibul, K.; Harnroongroj, T.; Sudjai, N.; Harnroongroj, T. Vertical pelvic ring displacement in pelvic ring injury Measurements in pelvic outlet radiograph and in cadavers. Indian J. Orthop. 2015, 49, 425–428. [Google Scholar] [CrossRef]
- Callary, S.A.; Thewlis, D.; Rowlands, A.V.; Findlay, D.M.; Solomon, L.B. Collecting a comprehensive evidence base to monitor fracture rehabilitation: A case study. World. J. Orthop. 2013, 4, 259–266. [Google Scholar] [CrossRef]
- Chehade, M.J.; Solomon, L.B.; Callary, S.A.; Benveniste, S.H.; Pohl, A.P.; Howie, D.W. Differentially loaded radiostereometric analysis to monitor fracture stiffness: A feasibility study. Clin. Orthop. Relat. Res. 2009, 467, 1839–1847. [Google Scholar] [CrossRef][Green Version]
- Solomon, L.B.; Callary, S.A.; Stevenson, A.W.; McGee, M.A.; Chehade, M.J.; Howie, D.W. Weight-bearing-induced displacement and migration over time of fracture fragments following split depression fractures of the lateral tibial plateau: A case series with radiostereometric analysis. JBone Joint Surg. Ser. B 2011, 93, 817–823. [Google Scholar] [CrossRef]
- Valstar, E.R.; Gill, R.; Ryd, L.; Flivik, G.; Börlin, N.; Kärrholm, J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta. Orthop. 2005, 76, 563–572. [Google Scholar] [CrossRef]
- Ahn, J.M.; Suh, J.T. Anatomy, Classification and Radiology of the Pelvic Fracture. J. Korean Fract. Soc. 2013, 26, 221. [Google Scholar] [CrossRef]
- Pennal, G.F.; Tile, M.; Waddell, J.P.; Garside, H. Pelvic disruption: Assessment and classification. Clin. Orthop. Relat. Res. 1980, 12–21. [Google Scholar] [CrossRef]
- Kibsgård, T.J.; Røise, O.; Stuge, B.; Röhrl, S.M. Precision and accuracy measurement of radiostereometric analysis applied to movement of the sacroiliac joint. Clin. Orthop. Relat. Res. 2012, 470, 3187–3194. [Google Scholar] [CrossRef] [PubMed]
- Solomon, L.B.; Pohl, A.P.; Sukthankar, A.; Chehade, M.J. The subcristal pelvic external fixator: Technique, results, and rationale. J. Orthop. Trauma 2009, 23, 365–369. [Google Scholar] [CrossRef]
- Matta, J.M.; Tornetta, P. Internal fixation of unstable pelvic ring injuries. Clin. Orthop. Relat. Res. 1996, 129–140. [Google Scholar] [CrossRef]
- Lefaivre, K.A.; Slobogean, G.P.; Valeriote, J.; O’Brien, P.J.; Macadam, S.A. Reporting and interpretation of the functional outcomes after the surgical treatment of disruptions of the pelvic ring: A systematic review. J. Bone Joint Surg. Ser. B 2012, 94, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Templeman, D.; Goulet, J.; Duwelius, P.J.; Olson, S.; Davidson, M. Internal fixation of displaced fractures of the sacrum. Clin. Orthop. Relat. Res. 1996, 329, 180–185. [Google Scholar] [CrossRef]
- Kibsgård, T.J.; Røise, O.; Sturesson, B.; Röhrl, S.M.; Stuge, B. Radiosteriometric analysis of movement in the sacroiliac joint during a single-leg stance in patients with long-lasting pelvic girdle pain. Clin. Biomech. 2014, 29, 406–411. [Google Scholar] [CrossRef]
- Sturesson, B.; Udén, A.; Önsten, I. Can an external frame fixation reduce the movements in the sacroiliac joint? A radiostereometric analysis of 10 patients. Acta Orthop. Scand. 1999, 70, 42–46. [Google Scholar] [CrossRef]
- Sturesson, B.; Selvik, G.; Udén, A. Movements of the sacroiliac joints: A roentgen stereophotogrammetric analysis. Spine (Phila Pa 1976) 1989, 14, 162–165. [Google Scholar] [CrossRef]


| Number of Patients | n | 6 |
|---|---|---|
| Age (years) | Mean (Range) | 34 (18–47) |
| Gender | F:M | 4:2 |
| BMI | Mean (Range) | 23 (21–25) |
| Mechanism of injury | MVA - car vs pedestrian - car vs car - Fall from height - parachute accident - fall from horse - Work-related (hit by hay-bail) | 3 2 1 2 1 1 1 |
| Classification of injury (Tile [3]) | All patients | C1 |
| Associated injuries | Chest injury Spine fractures Head injury Abdominal organ injury Superficial soft tissue injury | 1 3 1 3 2 |
| Length of stay from initial injury (days) | Mean (Range) | 25 (16–37) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ladurner, A.; Callary, S.A.; Mitra, A.; Rickman, M.; Thewlis, D.; Solomon, L.B. Radiostereometric Analysis Allows Assessment of the Stability and Inducible Displacement of Pelvic Ring Disruptions during Healing: A Case Series. J. Clin. Med. 2020, 9, 3411. https://doi.org/10.3390/jcm9113411
Ladurner A, Callary SA, Mitra A, Rickman M, Thewlis D, Solomon LB. Radiostereometric Analysis Allows Assessment of the Stability and Inducible Displacement of Pelvic Ring Disruptions during Healing: A Case Series. Journal of Clinical Medicine. 2020; 9(11):3411. https://doi.org/10.3390/jcm9113411
Chicago/Turabian StyleLadurner, Andreas, Stuart A. Callary, Aniruddha Mitra, Mark Rickman, Dominic Thewlis, and Lucian B. Solomon. 2020. "Radiostereometric Analysis Allows Assessment of the Stability and Inducible Displacement of Pelvic Ring Disruptions during Healing: A Case Series" Journal of Clinical Medicine 9, no. 11: 3411. https://doi.org/10.3390/jcm9113411
APA StyleLadurner, A., Callary, S. A., Mitra, A., Rickman, M., Thewlis, D., & Solomon, L. B. (2020). Radiostereometric Analysis Allows Assessment of the Stability and Inducible Displacement of Pelvic Ring Disruptions during Healing: A Case Series. Journal of Clinical Medicine, 9(11), 3411. https://doi.org/10.3390/jcm9113411







