Efficacy and Patient’s Acceptance of Alternative Methods for Caries Removal—A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.1.1. Types of Studies
2.1.2. Types of Participants
2.1.3. Types of Interventions
- (1)
- Dental caries treatment with conventional mechanical methods (control), using high-speed rotary instruments, excavators, or both.
- (2)
- Dental caries treatment with chemomechanical methods, comprising Brix 3000, Carie-Care, Carisolv or Papacarie, in combination with blunt excavators.
- (3)
- Dental caries treatment with laser systems, comprising Er:YAG or Er,Cr:YSGG lasers.
- (4)
- Dental caries treatment with air- and/or sono-abrasion systems, using the Vector System (VS, Duerr Dental, Bietigheim-Bissingen, Germany).
2.1.4. Types of Outcome Measures
Primary Outcomes
Secondary Outcomes
2.2. Search Strategy
2.2.1. Electronic Search
2.2.2. Searching Other Sources
2.3. Data Collection, Extraction, and Analysis
2.3.1. Selection of Studies
2.3.2. Data Extraction and Management
2.3.3. Assessment of Risk of Bias in the Included Studies
3. Results
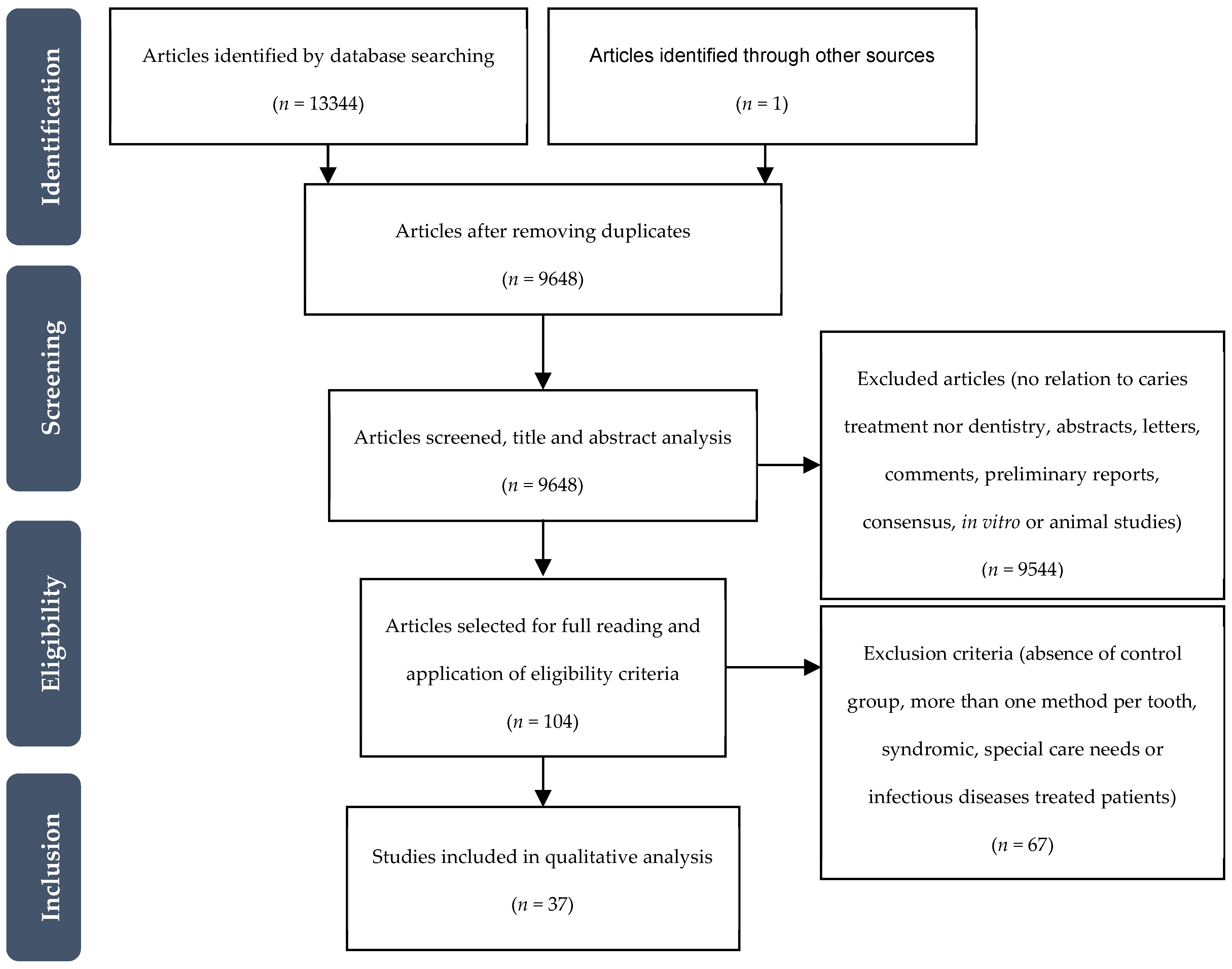
3.1. Search Results
3.2. Included Studies
3.2.1. Design
3.2.2. Participants
3.2.3. Interventions
3.2.4. Outcomes
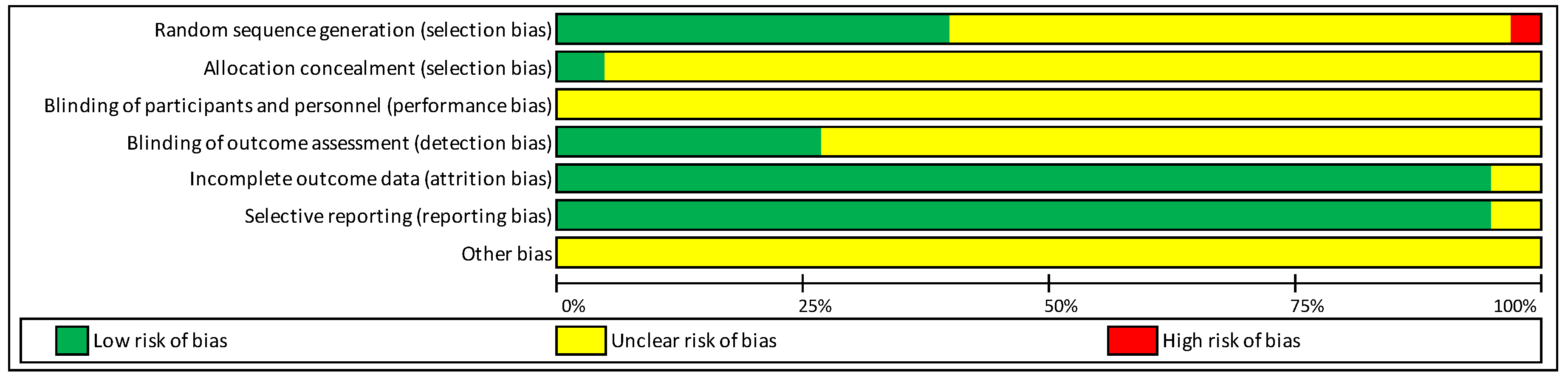
3.2.5. Risk of Bias in the Included Studies
3.2.6. Effects of Interventions
Chemomechanical versus Control
Laser versus Control
VS versus Control
Carisolv versus Papacarie versus Control
Carisolv versus Papacarie versus Er: YAG Laser versus Control
Sodium Hypochlorite Gel versus Brix 3000 versus Control
4. Discussion
4.1. Summary of Main Findings
4.2. Overall Completeness and Applicability of Evidence
4.3. Quality of Evidence
4.4. Potential Biases in the Review Process
5. Conclusions
5.1. Implications for Practice
5.2. Implications for Research
Author Contributions
Funding
Conflicts of Interest
Appendix A
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
| ? | ? | ? | ? | + | + | ? | Chomyszyn-Gajewska et al., 2006 [55] |
| ? | ? | ? | ? | + | + | ? | Fure et al., 2000 [51] |
| + | ? | ? | + | + | + | ? | Lozano-Chourio et al., 2006 [26] |
| ? | ? | ? | ? | + | + | ? | Pandit et al., 2007 [53] |
| ? | ? | ? | ? | + | + | ? | Subramaniam et al., 2008 [29] |
| ? | ? | ? | ? | + | + | ? | Mizuno et al., 2011 [30] |
| ? | ? | ? | ? | + | + | ? | Anegundi et al., 2012 [12] |
| ? | ? | ? | ? | + | + | ? | Rajakumar et al., 2013 [35] |
| + | ? | ? | + | + | + | ? | Motta et al., 2013 [34] |
| + | ? | ? | ? | + | + | ? | Matsumoto et al., 2013 [33] |
| + | ? | ? | ? | + | + | ? | Soni et al., 2014 [48] |
| ? | ? | ? | + | + | ? | Hegde et al., 2014 [36] | |
| + | ? | ? | + | + | + | ? | Motta et al., 2014 [37] |
| + | ? | ? | ? | + | + | ? | Motta et al., 2014 [38] |
| ? | ? | ? | ? | + | + | ? | Goyal et al., 2015 [27] |
| + | + | ? | ? | + | + | ? | Khalek et al., 2017 [45] |
| + | ? | ? | + | + | + | ? | Bottega et al., 2018 [59] |
| ? | ? | ? | ? | + | + | ? | Ismail et al., 2019 [43] |
| ? | ? | ? | + | + | + | ? | Sontakke et al., 2019 [50] |
| + | ? | ? | + | + | + | ? | Hadley et al., 2000 [52] |
| ? | ? | ? | + | ? | ? | ? | DenBesten et al., 2000 [46] |
| ? | ? | ? | + | ? | ? | ? | DenBesten et al., 2001 [47] |
| + | ? | ? | ? | + | + | ? | Liu et al., 2006 [28] |
| ? | ? | ? | ? | + | + | ? | Hjertton et al., 2013 [32] |
| x | ? | ? | ? | + | + | ? | Eren et al., 2013 [31] |
| ? | ? | ? | ? | + | + | ? | Zhegova et al., 2014 [39] |
| ? | ? | ? | ? | + | + | ? | Belcheva et al., 2014 [57] |
| ? | ? | ? | ? | + | + | ? | Belcheva et al., 2014 [58] |
| + | ? | ? | + | + | + | ? | Valério et al., 2015 [42] |
| ? | ? | ? | ? | + | + | ? | Zhegova et al., 2015 [40] |
| + | + | ? | + | + | + | ? | Sarmadi et al., 2018 [10] |
| + | ? | ? | ? | + | + | ? | Polizeli et al., 2019 [44] |
| ? | ? | ? | ? | + | + | ? | Kochhar et al., 2011 [54] |
| ? | ? | ? | ? | + | + | ? | Bohari et al., 2012 [56] |
| ? | ? | ? | ? | + | + | ? | Ammari et al., 2014 [15] |
| + | ? | ? | ? | + | + | ? | Hegde et al., 2016 [41] |
| + | ? | ? | ? | + | + | ? | Alkhouli et al., 2020 [49] |
References
- Hon, L.; Mohamed, A.; Lynch, E. Reliability of colour and hardness clinical examinations in detecting dentine caries severity: A systematic review and meta-analysis. Sci. Rep. 2019, 9, 6533. [Google Scholar] [CrossRef] [PubMed]
- Gannam, C.V.; Chin, K.L.; Gandhi, R.P. Caries risk assessment. Gen. Dent. 2018, 66, 12–17. [Google Scholar] [PubMed]
- Rathee, M.; Sapra, A. Dental Caries. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2020. [Google Scholar]
- Maru, V.P.; Shakuntala, B.S.; Nagarathna, C. Caries Removal by Chemomechanical (Carisolv (TM)) vs. Rotary Drill: A Systematic Review. Open Dent. J. 2015, 9, 462–472. [Google Scholar] [CrossRef] [PubMed]
- Dorri, M.; Martinez-Zapata, M.J.; Walsh, T.; Marinho, V.C.; Sheiham, A.; Zaror, C. Atraumatic restorative treatment versus conventional restorative treatment for managing dental caries. Cochrane Database Syst. Rev. 2017, 2017. [Google Scholar] [CrossRef]
- Muntean, A.; Mesaros, A.S.; Festila, D.; Mesaroș, M. Modern management of dental decay in children and adolescents—A review. Clujul Med. 2015, 88, 137–139. [Google Scholar] [CrossRef] [PubMed]
- Sugars and Dental Caries. Available online: https://apps.who.int/iris/bitstream/handle/10665/259413/WHO-NMH-NHD-17.12-eng.pdf?sequence=1 (accessed on 5 August 2020).
- Mathur, V.P.; Dhillon, J.K. Dental Caries: A Disease Which Needs Attention. Indian J. Pediatr. 2017, 85, 202–206. [Google Scholar] [CrossRef]
- Kutsch, V.K. Dental caries: An updated medical model of risk assessment. J. Prosthet. Dent. 2014, 111, 280–285. [Google Scholar] [CrossRef]
- Sarmadi, R.; Andersson, E.V.; Lingström, P.; Gabre, P. A Randomized Controlled Trial Comparing Er:YAG Laser and Rotary Bur in the Excavation of Caries–Patients’ Experiences and the Quality of Composite Restoration. Open Dent. J. 2018, 12, 443–454. [Google Scholar] [CrossRef]
- Philip, N.; Suneja, B.; Walsh, L.J. Ecological Approaches to Dental Caries Prevention: Paradigm Shift or Shibboleth? Caries Res. 2018, 52, 153–165. [Google Scholar] [CrossRef]
- Anegundi, R.T.; Patil, S.B.; Shetty, S.D.; Tegginmani, V. A comparative microbiological study to assess caries excavation by conventional rotary method and a chemo-mechanical method. Contemp. Clin. Dent. 2012, 3, 388–392. [Google Scholar] [CrossRef]
- Tanboga, I.; Eren, F.; Altınok, B.; Peker, S.; Ertugral, F. The effect of low level laser therapy on pain during dental tooth-cavity preparation in children. Eur. Arch. Paediatr. Dent. 2011, 12, 93–95. [Google Scholar] [CrossRef] [PubMed]
- Zinck, J.H.; McInnes-Ledoux, P.; Capdeboscq, C.; Weinberg, R. Chemomechanical caries removal?A clinical evaluation. J. Oral Rehabil. 1988, 15, 23–33. [Google Scholar] [CrossRef]
- Ammari, M.M.; Moliterno, L.F.M.; Junior, R.H.; Séllos, M.C.; Soviero, V.M.; Filho, W.P.C. Efficacy of chemomechanical caries removal in reducing cariogenic microbiota: A randomized clinical trial. Braz. Oral Res. 2014, 28, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Anyunes, L.A.; Pierro, V.; Maia, L. Case Report: Air Abrasion Cavity Preparation for Caries Removal in Paediatric Dentistry. Eur. Arch. Paediatr. Dent. 2007, 8, 12–14. [Google Scholar] [CrossRef]
- Hamama, H.H.; Yiu, C.; Burrow, M.F. Current update of chemomechanical caries removal methods. Aust. Dent. J. 2014, 59, 446–456. [Google Scholar] [CrossRef] [PubMed]
- Maragakis, G.; Hahn, P.; Hellwig, E. Chemomechanical caries removal: A comprehensive review of the literature. Int. Dent. J. 2001, 51, 291–299. [Google Scholar] [CrossRef]
- Jingarwar, M.M.; Bajwa, N.K.; Pathak, A. Minimal Intervention Dentistry—A New Frontier in Clinical Dentistry. J. Clin. Diagn. Res. 2014, 8, ZE04–ZE08. [Google Scholar] [CrossRef]
- Montedori, A.; Abraha, I.; Orso, M.; D’Errico, P.G.; Pagano, S.; Lombardo, G. Lasers for caries removal in deciduous and permanent teeth. Cochrane Database Syst. Rev. 2016, 9, CD010229. [Google Scholar] [CrossRef]
- Wong, Y.J. Caries removal using lasers. Evid. Based Dent. 2018, 19, 45. [Google Scholar] [CrossRef]
- Ntovas, P.; Doukoudakis, S.; Tzoutzas, J.; Lagouvardos, P. Evidence provided for the use of oscillating instruments in restorative dentistry: A systematic review. Eur. J. Dent. 2017, 11, 268–273. [Google Scholar] [CrossRef][Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho, A.P.V.; Silva, V.; Grande, A.J. Avaliação do risco de viés de ensaios clínicos randomizados pela ferramenta da colaboração Cochrane. Diagn. Trat. 2013, 18, 38–44. [Google Scholar]
- Lozano-Chourio, M.A.; Zambrano, O.; Gonzalez, H.; Quero, M. Clinical randomized controlled trial of chemomechanical caries removal (Carisolvtm). Int. J. Paediatr. Dent. 2006, 16, 161–167. [Google Scholar] [CrossRef]
- Goyal, P.A.; Kumari, R.; Kannan, V.P.; Madhu, S. Efficacy and Tolerance of Papain Gel with Conventional Drilling Method: A Clinico-Microbiological Study. J. Clin. Pediatr. Dent. 2015, 39, 109–112. [Google Scholar] [CrossRef]
- Liu, J.-F.; Lai, Y.-L.; Shu, W.-Y.; Lee, S.-Y.; Lee, S.-Y. Acceptance and Efficiency of Er:YAG Laser for Cavity Preparation in Children. Photomed. Laser Surg. 2006, 24, 489–493. [Google Scholar] [CrossRef]
- Subramaniam, P.; Babu, K.L.G.; Neeraja, G. Comparison of the Antimicrobial Efficacy of Chemomechanical Caries Removal (carisolv (TM)) with that of Conventional Drilling in Reducing Cariogenic Flora. J. Clin. Pediatr. Dent. 2008, 32, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Mizuno, D.; Guedes, C.; Hermida Bruno, L.; Motta, L.; Santos, E.; Bussadori, S. Análisis clínico y radiográfico de las técnicas ART y remoción químico- mecánica de caries: Estudio piloto. Odontoestomatología 2011, 13, 29–35. [Google Scholar]
- Eren, F.; Altinok, B.; Ertugral, F.; Tanboga, I. The effect of erbium, chromium:yttrium-scandium-gallium-garnet (Er,Cr:YSGG) laser therapy on pain during cavity preparation in paediatric dental patients: A pilot study. Oral Health Dent. Manag. 2013, 12, 80–84. [Google Scholar]
- Hjertton, P.M.; Bågesund, M. Er:YAG laser or high-speed bur for cavity preparation in adolescents. Acta Odontol. Scand. 2012, 71, 610–615. [Google Scholar] [CrossRef]
- Matsumoto, S.F.; Motta, L.; Alfaya, T.; Guedes, C.; Fernandes, K.P.; Bussadori, S. Assessment of chemomechanical removal of carious lesions using Papacarie Duo™: Randomized longitudinal clinical trial. Indian J. Dent. Res. 2013, 24, 488–492. [Google Scholar] [PubMed]
- Motta, L.J.; Bussadori, S.K.; Campanelli, A.P.; Da Silva, A.L.; Alfaya, T.A.; De Godoy, C.H.L.; Navarro, M.F.D.L. Pain during Removal of Carious Lesions in Children: A Randomized Controlled Clinical Trial. Int. J. Dent. 2013, 2013, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Rajakumar, S.; Mungara, J.; Joseph, E.; Philip, J.; Guptha, V.; Pally, S.M. Evaluation of Three Different Caries Removal Techniques in Children: A Comparative Clinical Study. J. Clin. Pediatr. Dent. 2013, 38, 23–26. [Google Scholar] [CrossRef]
- Hegde, A.M.; Preethy, V.C.; Shetty, A.; Shetty, S. Clinical Evaluation of Chemo-Bechanical Caries Removal Using Carie-Care System Among School Children. J. Health Allied Sci. NU 2014, 4, 080–084. [Google Scholar] [CrossRef]
- Motta, L.J.; Bussadori, S.K.; Campanelli, A.P.; Da Silva, A.L.; Alfaya, T.A.; De Godoy, C.H.L.; Navarro, M.F.D.L. Randomized controlled clinical trial of long-term chemo-mechanical caries removal using PapacarieTM gel. J. Appl. Oral Sci. 2014, 22, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Motta, L.J.; Bussadori, S.K.; Campanelli, A.P.; da Silva, A.L.; Alfaya, T.A.; de Godoy, C.H.L.; Navarro, M.F.D. Efficacy of Papacarie (R) in reduction of residual bacteria in deciduous teeth: A randomized, controlled clinical trial. Clinics 2014, 69, 319–322. [Google Scholar] [CrossRef]
- Zhegova, G.G.; Rashkova, M.R.; Yordanov, B.I. Perception Of Er-Yag Laser Dental Caries Treatment In Adolescents—A Clinical Evaluation. J. IMAB Annu. Proceeding Sci. Pap. 2014, 20, 500–503. [Google Scholar] [CrossRef][Green Version]
- Zhegova, G.G.; Rashkova, M.R. Er-Yag Laser And Dental Caries Treatment Of Permanent Teeth In Childhood. J. IMAB Annu. Proceeding Sci. Pap. 2014, 21, 699–704. [Google Scholar] [CrossRef]
- Hegde, S.; Kakti, A.; Bolar, D.R.; Bhaskar, S.A. Clinical Efficiency of Three Caries Removal Systems: Rotary Excavation, Carisolv, and Papacarie. J. Dent. Child. (Chicago, Ill.) 2016, 83, 22–28. [Google Scholar]
- Valério, R.A.; Borsatto, M.C.; Serra, M.C.; Polizeli, S.A.F.; Nemezio, M.A.; Galo, R.; Aires, C.P.; Dos Santos, A.C.; Corona, S.A.M. Caries removal in deciduous teeth using an Er:YAG laser: A randomized split-mouth clinical trial. Clin. Oral Investig. 2015, 20, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Ismail, M.M.; Al Haidar, A.H.M.J. Evaluation of the efficacy of caries removal using papain gel (Brix 3000) and smart preparation bur(in vivo comparative study). J. Pharm. Sci. Res. 2019, 11, 444–449. [Google Scholar]
- Polizeli, S.A.F.; Curylofo-Zotti, F.A.; Valério, R.A.; Nemezio, M.A.; Souza-Gabriel, A.E.; Borsatto, M.C.; Corona, S.A.M. Selective Removal of Necrotic Dentin in Primary Teeth Using Laser Irradiation: One-Year Clinical Evaluation of Composite Restorations. J. Lasers Med. Sci. 2019, 10, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Khalek, A.A.; Elkateb, M.A.; Aziz, W.E.A.; El Tantawi, M. Effect of Papacarie and Alternative Restorative Treatment on Pain Reaction during Caries Removal among Children: A Randomized Controlled Clinical Trial. J. Clin. Pediatr. Dent. 2017, 41, 219–224. [Google Scholar] [CrossRef]
- DenBesten, P.K.; White, J.M.; Pelino, J.; Lee, K.; Parkins, F. A randomized prospective parallel controlled study of the safety and effectiveness of Er: YAG laser use in children for caries removal. In Proceedings of the BiOS 2000: The International Symposium on Biomedical Optics, San Jose, CA, USA, 22–28 January 2000; pp. 171–174. [Google Scholar]
- DenBesten, P.K.; White, J.M.; Pelino, J.E.; Furnish, G.; Silveira, A.; Parkins, F.M. The Safety and Effectiveness of an Er:YAG Laser for Caries Removal and Cavity Preparation in Children. Med. Laser Appl. 2001, 16, 215–222. [Google Scholar] [CrossRef]
- Soni, H.K.; Sharma, A.; Sood, P.B. A comparative clinical study of various methods of caries removal in children. Eur. Arch. Paediatr. Dent. 2014, 16, 19–26. [Google Scholar] [CrossRef]
- Alkhouli, M.; Al Nesser, S.F.; Bshara, N.G.; Almidani, A.N.; Comisi, J.C. Comparing the efficacies of two chemo-mechanical caries removal agents (2.25% sodium hypochlorite gel and brix 3000), in caries removal and patient cooperation: A randomized controlled clinical trial. J. Dent. 2020, 93, 103280. [Google Scholar] [CrossRef] [PubMed]
- Sontakke, P.; Jain, P.; Patil, A.D.; Biswas, G.; Yadav, P.; Makkar, D.K.; Jeph, V.; Sakina, B.P. A comparative study of the clinical efficiency of chemomechanical caries removal using Carie-Care gel for permanent teeth of children of age group of 12–15 years with that of conventional drilling method: A randomized controlled trial. Dent. Res. J. 2019, 16, 42. [Google Scholar] [CrossRef]
- Fure, S.; Lingstrom, P.; Birkhed, D. Evaluation of Carisolv (TM) for the chemo-mechanical removal of primary root caries in vivo. Caries Res. 2000, 34, 275–280. [Google Scholar] [CrossRef]
- Hadley, J.; Young, D.A.; Eversole, L.R.; Gornbein, J.A. A laser-powered hydrokinetic system—For caries removal and cavity preparation. J. Am. Dent. Assoc. 2000, 131, 777–785. [Google Scholar] [CrossRef]
- Pandit, I.K.; Srivastava, N.; Gugnani, N.; Gupta, M.; Verma, L. Various methods of caries removal in children: A comparative clinical study. J. Indian Soc. Pedod. Prev. Dent. 2007, 25, 93–96. [Google Scholar]
- Kochhar, G.K.; Srivastava, N.; Pandit, I.K.; Gugnani, N.; Gupta, M. An Evaluation of Different Caries Removal Techniques in Primary Teeth: A Comparitive Clinical Study. J. Clin. Pediatr. Dent. 2011, 36, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Chomyszyn-Gajewska, M.; Kwapinska, H.; Zarzecka, J. Pain perception in children during caries removal with the Vector® system: A pilot study. Eur. Arch. Paediatr. Dent. 2006, 1, 38–41. [Google Scholar] [CrossRef] [PubMed]
- Bohari, M.R.; Chunawalla, Y.K.; Ahmed, B.M.N. Clinical Evaluation of Caries Removal in Primary Teeth using Conventional, Chemomechanical and Laser Technique: An in vivo Study. J. Contemp. Dent. Pract. 2012, 13, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Belcheva, A.; Shindova, M.P. Subjective acceptance of pediatric patients during cavity preparation with Er:YAG laser and conventional rotary instruments. J. IMAB Annu. Proceeding Sci. Pap. 2014, 20, 631–637. [Google Scholar] [CrossRef][Green Version]
- Belcheva, A.; Shindova, M.P. Pain Perception Of Pediatric Patients During Cavity Preparation With Er:Yag Laser And Conventional Rotary Instruments. J. IMAB Annu. Proceeding Sci. Pap. 2014, 20, 634–637. [Google Scholar] [CrossRef][Green Version]
- Bottega, F.; Bussadori, S.K.; Battisti, I.D.E.; Vieira, E.P.; Pompeo, T.S.; Winkelmann, E.R. Costs and benefits of Papacarie in pediatric dentistry: A randomized clinical trial. Sci. Rep. 2018, 8, 17908. [Google Scholar] [CrossRef] [PubMed]
- Kapur, A.; Kapur, V. Conscious Sedation in Dentistry. Ann. Maxillofac. Surg. 2018, 8, 320–323. [Google Scholar] [CrossRef]
- Beaudette, J.R.; Fritz, P.C.; Sullivan, P.J.; Ward, W.E. Oral Health, Nutritional Choices, and Dental Fear and Anxiety. Dent. J. 2017, 5, 8. [Google Scholar] [CrossRef]
- Carter, A.E.; Carter, G.; Boschen, M.; AlShwaimi, E.; George, R. Pathways of fear and anxiety in dentistry: A review. World J. Clin. Cases 2014, 2, 642–653. [Google Scholar] [CrossRef]
- Inglehart, M.R.; Habil, P.; Peters, M.C.; Flamenbaum, M.H.; Eboda, N.N.; Feigal, R.J. Chemomechanical caries removal in childrenAn operator’s and pediatric patients’ responses. J. Am. Dent. Assoc. 2007, 138, 47–55. [Google Scholar] [CrossRef]
- Yun, J.; Shim, Y.-S.; Park, S.-Y.; An, S.-Y. New treatment method for pain and reduction of local anesthesia use in deep caries. J. Dent. Anesth. Pain Med. 2018, 18, 277–285. [Google Scholar] [CrossRef]
- Lussi, A.; Hibst, R.; Paulus, R. DIAGNOdent: An Optical Method for Caries Detection. J. Dent. Res. 2004, 83, 80–83. [Google Scholar] [CrossRef] [PubMed]
- Ricketts, D.; Pitts, N. Novel Operative Treatment Options. Monogr. Oral Sci. 2009, 21, 174–187. [Google Scholar] [CrossRef] [PubMed]
| Criteria | Description |
|---|---|
| P (population) | Deciduous and permanent decayed teeth |
| I (intervention) | Alternative caries removal (chemomechanical methods, laser, sono-/air-abrasion) |
| C (comparison) | Conventional mechanical methods for caries removal (rotary or hand instruments) |
| O (outcome) | Efficacy for caries removal (time for treatment, caries removal, anesthesia and colony forming units count) |
| Inclusion criteria | Controlled trials |
| Primary caries lesion(s) treatment in healthy patients | |
| Caries lesion on primary or permanent dentition | |
| Cavitated dentin lesions | |
| One treatment per tooth | |
| Exclusion criteria | Abstracts, letters, comments, preliminary reports, consensus recommendations, in vitro or animal studies |
| Secondary caries lesion | |
| More than one technique applied per tooth, including the opening of the cavity with a different technique from that of caries removal | |
| Atraumatic restorative treatment (with no complete removal of decayed tissue), hall technique, non-restorative caries treatment, and related treatment approaches | |
| Specific populations (special care needs, infectious diseases, syndromic patients) |
| Database | Search Strategy |
|---|---|
| Cochrane Library | #1 MeSH descriptor: [Dental Caries] explode all trees |
| #2 carie* | |
| #3 cavit* | |
| #4 decay | |
| #5 #1 OR #2 OR #3 OR #4 | |
| #6 alternative | |
| #7 clean* | |
| #8 removal | |
| #9 laser | |
| #10 Er-YAG | |
| #11 Er:YAG | |
| #12 GK-101* | |
| #13 NMG | |
| #14 papain | |
| #15 brix 3000 | |
| #16 biosolv | |
| #17 solvent* | |
| #18 carie-care | |
| #19 papacarie | |
| #20 carisolv | |
| #21 n-monochloroglycine | |
| #22 caridex | |
| #23 ozone | |
| #24 “sono abrasion” | |
| #25 “air polishing” | |
| #26 photo-ablative | |
| #27 enzyme* | |
| #28 chloramine | |
| #29 “toluidine blue” | |
| #30 #6 OR #7 OR #8 OR #9 OR #10 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 | |
| #31 #5 AND #30 | |
| Embase | (cavit* OR decay OR carie* OR ‘dental caries’/exp OR ‘dental caries’) AND ((removal OR clean* OR alternative OR ‘laser’ OR ‘laser’/exp OR laser OR ‘er yag’ OR ‘er:yag’ OR ‘gk 101*’ OR nmg OR ‘papain’ OR ‘papain’/exp OR papain OR brix) AND 3000 OR biosolv OR solvent* OR ‘carie care’ OR ‘papacarie’ OR ‘papacarie’/exp OR papacarie OR ‘carisolv’ OR ‘carisolv’/exp OR carisolv OR ‘n-monochloroglycine’ OR caridex OR ‘ozone’ OR ‘ozone’/exp OR ozone OR ‘sono abrasion’ OR ‘air abrasion’ OR ‘air polishing’ OR ‘photo ablative’ OR enzyme* OR ‘chloramine’ OR ‘chloramine’/exp OR chloramine OR ‘toluidine blue’/exp OR ‘toluidine blue’) AND (humans)/lim AND (clinical study)/lim |
| Medline/Pubmed | ((((cavit* OR decay OR carie* OR “Dental Caries”(Mesh)) AND (removal OR clean* OR alternative OR laser OR Er-YAG OR ER:YAG OR GK-101* OR NMG OR papain OR brix 3000 OR biosolv OR solvent* OR carie-care OR papacarie OR carisolv OR n-monochloroglycine OR caridex OR ozone OR “sono abrasion” OR “air abrasion” OR “air polishing” OR photo-ablative OR enzyme* OR chloramine OR “toluidine blue”)))) AND Clinical Trial(ptyp)) |
| Web of Science | (TS = (“dental decay” OR “tooth decay” OR carie*) AND TS = (removal OR clean* OR alternative OR laser OR “Er-YAG” OR “ER:YAG” OR GK-101* OR NMG OR papain OR “brix 3000” OR biosolv OR solvent* OR “carie-care” OR papacarie OR carisolv OR “n-monochloroglycine” OR caridex OR ozone OR “sono abrasion” OR “air abrasion” OR “air polishing” OR “photo-ablative” OR enzyme* OR chloramine OR “toluidine blue”)) AND DOCUMENT TYPES: (Article) |
| ClinicalTrials.gov | #1 Dental Caries |
| Filters: Clinical trials, completed and with results. |
| Author, Year, Study Design | Dentition, Groups (n) | Treatment Time (Mean ± SD) | Caries Removal | Anesthesia | Restoration | Patients Pain Perception/Behavior |
|---|---|---|---|---|---|---|
| Fure et al., 2000 [51] 1 or more txt/patient | PD C: Bur (26) T1: Carisolv (34) | C = 4.5 ± 2.0 T1 = 5.9 ± 2.2 (min), C < T1 * | Remaining caries: C = 1 Final cavity: C > T1 | C = 6 T1 = 4 | At 12 m follow-up Restorations lost: C = 2/24, T1 = 2/31; Secondary caries: C = 1/24; Marginal discoloration: C = 3/21, T1 = 4/29 | Acceptance: 29/34 T1; T1: 64% did not find treatment times different and 23% found it faster than C; Better txt experience with T1 *** |
| Lozano-Chourio et al., 2006 [26] Cross-over | DD C: Bur (40) T1: Carisolv (40) | C = 2.47 ± 1.83 T1 = 7.51 ± 2.10 (min), C < T1 ** | Final cavity dimension: C > T1 ***; Tissue removed: C > T1*** | C = 2 | Pain during txt: C = 40%, T1 = 17.5%; C > T1 *; More positive behavior in T1 **; Acceptance *: T1 = 71% | |
| Pandit et al., 2007 [53] 1 or more txt/patient | DD C1: Excavator (50) C2: Bur (50) T1: Carisolv (50) | C1 = 424.6 ± 224.8 s C2 = 257.4 ± 100.6 s T1 = 534.8 ± 227.3 s C2 < C1 < T1 | Efficacy C2 > C1, T1 | VAS and VPS: C2 > C1 > T1 | ||
| Subramaniam et al., 2008 [29] Split-mouth | DD C: Bur (20) T1: Carisolv (20) | |||||
| Mizuno et al., 2011 [30] Split-mouth | DD C: Excavator (8) T1: Papacarie (8) | At 6 m follow-up Success: C = 5/6, T = 6/6 | ||||
| Anegundi et al., 2012 [12] Not clear | DD C: Bur (30) T1: Papacarie (30) | C = 280.89 s T1 = 1077.60 s C < T1 ** | Final cavity dimension: C > T1 *** | No pain: C = 50%, T1 = 86.5%; Slight pain: C = 46.7%, T1 = 10%; Unspecified pain: C = 3.3%, T1 = 3.3%; More pain induced by C **; Acceptance: C = 36.7% and T1 = 60% | ||
| Rajakumar et al., 2013 [35] Split-mouth | DD C1: Excavator (20) C2: Bur (20) T1: Carie care (20) | C1 = 44.43 ± 5.05 s C2 = 30.39 ± 8.95 s T1 = 96.45 ± 10.99 s C2 < C1 < T1 *** | Efficacy C2 > T1 > C1 | VPS and WBFPS: C1 > C2 > T1 ** | ||
| Motta et al., 2013 [34] Split-mouth | DD C: Bur (20) T1: Papacarie (20) | C = 1 | Pain: C > T1 * | |||
| Matsumoto et al., 2013 [33] Split mouth | DD C: Bur (20) T1: Papacarie Duo (20) | C = 1.43 ± 1.18 T1 = 2.45 ± 0.48 (min), C < T1 | C = 1 | At 30 d follow-up Restorations success: C∼T1 (p = 0.713) | Pain experience C∼T1 (p = 0.585) | |
| Soni et al., 2014 [48] 1 txt/patient | DD and PD C1: Bur (30) C2: Excavator (30) C3: Polymer burs (30) T1: Carisolv (30) | C1 = 232 ± 21.99 s C2 = 480 ± 33.38 s C3 = 354 ± 23.21 s T1 = 697 ± 30.17 s C1 < C3 < C2 < T1 (intergroup comparison *) | Efficacy (dental explorer): C1 > C3 > T1 > C2. Efficacy (caries detector dye): C1 > T1 > C3 > C2. Intergroup comparison *: C1/C2, C2/T1, C2/C3 | VAS and VPS: C1 > C2 > C3 > T1 (intergroup comparison *, except C3/T1) | ||
| Hegde et al., 2014 [36] Split-mouth | DD and PD C: Bur (16 each) T1: Carie-care (16 each) | DD C = 4.9; T1 = 7.0 (min), C < T1 PD C = 7.5; T1 = 10.4 (min), C < T1 | At 12 m follow-up All restorations intact; amalgam restorations with better retention than Ketac molar. Ketac molar with more success in T1 | T1 was more pleasant and accepted | ||
| Motta et al., 2014 [37] Split-mouth | DD C: Bur (20) T1: Papacarie (20) | C = 3.30 ± 2.03 T1 = 4.66 ± 3.13 (min), C < T1 | C = 1 | Success At 1 m follow-up: C = 100%, T1 = 100%; At 6 m follow-up: C = 90%, T1 = 95%; At 18 m follow-up: C = 80%, T1 = 95% | ||
| Motta et al., 2014 [38] Split-mouth | DD C: Bur (20) T1: Papacarie (20) | |||||
| Goyal et al., 2015 [27] Cross-over | DD C: Bur (25) T1: Papacarie (25) | C = 6.99 ± 1.7 T1 = 7.41 ± 1.62 (min), C < T1 | Mean pulse rate: C raised but reduced after txt; T1 reduced during and after txt ***; WBFPS: C raised during and after txt; T1 reduced **; Acceptance: C = 2/25, T1 = 20/25 | |||
| Khalek et al., 2017 [45] Two parallel-arms | DD C: Excavator (25) T1: Papacarie (25) | C = 4.8 ± 1.0 T1= 5.8 ± 1.2 (min), C < T1* | Signs of pain/discomfort: Sound: C > T ****; Eye: C > T **; Motor: C > T *** | |||
| Bottega et al., 2018 [59] Not clear | DD and PD C: Bur (12) T1: Papacarie (12) | C = 10.5, T1 = 12.5 (min, median) C < T1 | At 30 d follow-up T1 = 1/26 lost restorations | Heart rate rise during txt, maintaining after txt in C and T1 | ||
| Ismail et al., 2019 [43] Split mouth | PD C: Bur (30) T1: Brix 3000 (30) | C = 23.53 ± 6.04 T1 = 37.67 ± 10.21 (min), C < T1 *** | Sound, eye and motor signs ****: Comfort: C = 3.3%, T1 = 30%; Mild discomfort: C = 6.6%, T1 = 50%; Moderately painful: C = 70%, T1 = 20%; Painful: C= 20% | |||
| Sontakke et al., 2019 [50] 1 txt/patient | PD C: Bur (30) T1: Carie-care (30) | C = 11.5 ± 2.83 T1 = 18.9 ± 3.78 (min), C < T1 **** | Pain: C > T1 **** |
| Author, Year, Study Design | Dentition, Groups (n) | Treatment Time (Mean ± SD) | Caries Removal | Anesthesia | Restoration | Patients Pain Perception/Behavior |
|---|---|---|---|---|---|---|
| Hadley et al., 2000 [52] 1 or more txt/patient | PD C: Bur (66) T1: Er,Cr:YSGG laser (66) | At 30 d follow-up C: 1/66 restorations with partial loss; At 6 m follow-up C/T1: 66/66 restorations with no secondary caries | Discomfort: during txt C = 12.1%, T1 = 1.5%, C > T1 **; after txt C = 9.1%, T1 = 1.5%, C > T1 * | |||
| DenBesten et al., 2000 [46] 1 txt/patient | DD and PD C: Bur (41) T1: Er:YAG laser (82) | T1: txt energy for DD < PD *** | C = 25% T1 = 7% | Without discomfort (without anesthesia): C = 50%, T1 = 100% | ||
| DenBesten et al., 2001 [47] 1 txt/patient | C: Bur (42) T1: Er:YAG laser (82) | C = 6.6 T1 = 7.7 (min), C < T1 | T1: txt energy for DD < PD *; energy for cavity preparation < caries removal * | C = 11/42 T1 = 4/82 C > T1 ** | Without discomfort (without anesthesia: C = 31, T1 = 78): C = 50%, T1 = 100% | |
| Liu et al., 2006 [28] Split-mouth | DD and PD C: Bur (40) T1: Er:YAG laser (40) | C= 41.3 ± 38.3 s T1= 97.0 ± 49.7 s C < T1 *** | More body movements during C ***; No pain: C = 17.5%, T1 = 82.5%; Mild pain: C = 40%, T1 = 12.5%; Moderate pain: C = 27.5%, T1 = 2.5%; Severe pain: C = 15%, T1 = 2.5% | |||
| Hjertton et al., 2013 [32] Split-mouth | PD C: Bur (35) T1: Er:YAG laser (35) | C = 16 ± 4 s T1= 59 ± 41 s C < T1 *** | Mean pulse raise during C and reduction during T1 *; Smell perception, comfort, acceptance: C < T1 **; Sound perception: C > T1 ** | |||
| Eren et al., 2013 [31] Split-mouth | PD C: Bur (10) T1: Er,Cr:YSGG laser (10) | C = 3.7 T1 = 7.4 (min), C < T1 | Pain: C > T1 Comfort: C < T1 | |||
| Zhegova et al., 2014 [39] Split-mouth | PD C: Bur (44) T1: Er:YAG laser (44) | No pain: C = 18.18%, T1 = 79.55%, C < T1 *; Slight discomfort: C = 9.09%, T1 = 11.36%; Mild pain: C = 20.45, T1 = 9.09%; Moderate pain: C = 43.18%; Severe pain: C = 9.09%; Acceptance: C = 2/44, T1 = 38/44 | ||||
| Belcheva et al., 2014 [57] Not clear | DD and PD C: Bur (NR) T1: Er:YAG laser (NR) | Anxiety factors Vibration: C > T1 ***; Smell: C < T1 ***; Taste: C < T1 * | ||||
| Belcheva et al., 2014 [58] Not clear | C: Bur (NR) T1: Er:YAG laser (NR) | Mild pain: C = 40%, T1 = 71.10%; Moderate pain: C = 42.20%, T1 = 26.70%; Severe pain: C = 17.80%, T1 = 2.20%; Pain: C > T1 ** | ||||
| Valério et al., 2015 [42] Split-mouth | DD C: Bur (29) T1: Er:YAG laser (29) | C= 54.96 ± 5.64 s T = 110.24 ± 9.83 s C < T1 * | Efficacy C∼T1, on pulpal walls *; C more efficient on the remaining walls **** | At 7 d and 12 m follow-up No differences | ||
| Zhegova et al., 2015 [40] Split-mouth | PD C: Bur (58) T1: Er:YAG laser (58) | At 12 m follow-up Small marginal loss: C = 2/58; T1 = 3/58; At 18 m follow-up Small marginal loss: C/T1 = 2/58; small multiple losses or marginal discoloration: C/T1: 1/58; At 24 m follow-up Small marginal loss: C = 3/58, T1 = 2/58; small multiple losses or marginal discoloration: C = 1/58, T1 = 2/58 | ||||
| Sarmadi et al., 2018 [10] Split-mouth | PD C: Bur (28) T1: Er:YAG laser (28) | C = 4.3 T1 = 13.2 (min), C < T1 **** | C = 15/28 T1 = 10/28 | At 6 m follow-up Small marginal loss: C = 2/26; Slight discoloration: C= 1/26; Initial secondary caries: C = 2/26; At 12 m follow-up Small marginal loss: C/T1 = 1/25; Dentinal exposure: C = 1/25; Slight discoloration: C = 1/25; Initial secondary caries: T1 = 1/25; Secondary caries: C/T1 = 2/25; At 24 m follow-up Small marginal loss: C = 1/20; Secondary caries: T1 = 2/20 | Discomfort after txt Immediate: C∼T1; At 7 d–C > T1 *; At 6 m–C > T1 ***; At 12 m and 24 m–C > T1 **; Acceptance: At 7 d–C < T1 ***; At 6 m, 12 m and 24 m–C < T1 ** | |
| Polizeli et al., 2019 [44] Split-mouth | DD C: Bur (20) T1: Er:YAG laser (20) | At 12 m follow-up C = 1/20 restorations were lost; Replicate SEM analysis Baseline∼6 m; after 12 m (gaps): C = 20%, T1 = 10% | Raise of salivary cortisol levels during txt and C∼T1 |
| Author, Year, Study Design | Dentition, Groups (n) | Treatment Time (Mean ± SD) | Caries Removal | Patients Pain Perception/Behavior |
|---|---|---|---|---|
| Kochhar et al., 2011 [54] 1 or more txt/patient | DD C1: Excavator (30) C2: Bur (30) T1: Carisolv (30) T2: Papacarie (30) | C1 = 535.83 ± 232.14 s C2 = 261.70 ± 86.06 s T1 = 723.73 ± 179.48 s T2 = 590.80 ± 187.00 s C2 < C1 < T2 < T1 (intergroup comparison *, except C1/T2) | Remaining caries: C2 < T2 < T1 < C1 (intergroup comparison *, except T2/C2 and T2/T1) | VAS and VPS: intergroup comparison *, except C1/C2 on VPS; VAS and VPS: C2 > C1 > T1 > T2 |
| Bohari et al., 2012 [56] Not clear | DD C: Bur (30) T1: Carisolv (30) T2: Papacarie (30) T3: Er:YAG laser (30) | C = 206.7 ± 22.1 s T1 = 474.7 ± 43.0 s T2 = 471.3 ± 68.2 s T3 = 359.9 ± 59.9 s (intergroup comparison ***, except T1/T2) | Change in DIAGNOdent values: C = 92.9 ± 9.2%; T1 = 87.7 ± 6.4%; T2 = 88.9 ± 6.0%; T3 = 93.9 ± 4.9%; (intergroup comparison *, for C/T1 and T1/T3, and **, for C/T2 and T2/T3) | FLACCS: C was more painful and uncomfortable (intergroup comparison of T1, T2, T3/C ***) |
| Ammari et al., 2014 [15] 1 or more txt/patient | DD C: Excavator (22) T1: Papacarie (25) T2: Carisolv (27) | |||
| Hegde et al., 2016 [41] Split-mouth | DD C: Bur (50) T1: Carisolv (50) T2: Papacarie (50) | C = 61.34 ± 30.43 s T1 = 341.21 ± 110.93 s T2 = 322.49 ± 91.24 s C< T1, T2 *** | Efficacy: C *** > T1, T2; T1 < T2 ** | Pain perception: C > T1 > T2, C > T1 *, C > T2 **; Worsening of behavior during C **; Acceptance *: C = 24%, T1 = 26% and T2 = 48% |
| Alkhouli et al., 2020 [49] 1 txt/patient | DD C: Bur (10) T1: 2.25% sodium hypochlorite gel (12) T2: Brix 3000 (10) | C= 1.60 ± 0.843 T1= 6.40 ± 1.838 T2= 5 ± 1.595 (min), C < T1 ***, C < T2 ** | WBFPS: C > T1 ** and C > T2 *** |
| Outcomes | Mechanical | Chemomechanical | Laser | Vector System |
|---|---|---|---|---|
| Treatment time | Conventional methods for caries removal determine faster treatment interventions [10,12,15,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59] | Brix 3000, Carie-care, Carisolv and Papacarie led to longer interventions than conventional treatments [12,26,43,45,48,49,51] | Treatment with the Er:YAG laser system increased treatment time [10,28,32,42], while treatment with the Er,Cr:YSGG did not [31] | The use of VS increased treatment time [55] |
| The use of Carisolv and Papacarie increases treatment time compared to the use of the Er:YAG laser system, and Papacarie determines faster interventions than Carisolv [56] | ||||
| Caries removal efficacy | Mechanical caries removal produces wider free-caries cavities [12,26] | Papacarie tends to be more effective in caries removal than Carisolv [41,54] | Treatment in the deciduous dentition requires less energy than treatment in the permanent dentition [46,47] | |
| Treatment with Er:YAG laser showed the highest percentage of DIAGNOdent value change, compared to Carisolv and Papacarie, and Papacarie showed higher values change than Carisolv [56] | ||||
| Anesthesia | Patients requested anesthesia more often when treated with mechanical methods [10,26,33,34,37,46,47,51] | Treatment with chemomechanical or laser methods was performed with less requests for anesthesia [10,26,33,34,37,46,47,51] | ||
| CFU count | Mechanical rotary methods are effective in reducing the cariogenic flora [12,15,27,29,38,43] | Chemomechanical methods are effective in reducing the cariogenic flora [12,15,27,29,38,43] and Brix 3000 and Papacarie may achieve higher reductions than mechanical methods [12,28,43] | ||
| Restorations | The restorations performance did not differ according to the method for caries removal [10,30,33,36,37,40,42,44,51,52,59] | |||
| Patients pain perception/behavior | Mechanical caries removal is associated with pain, more movements during treatment and is less preferred regarding future treatments [10,12,26,27,28,32,33,34,35,36,39,41,43,45,48,49,50,51,52,53,54,55,56,57,58,59] | All alternative methods induce less pain and discomfort during treatment. However, smell and taste may be appointed as negative aspects of these approaches [10,12,26,27,28,32,33,34,35,36,39,41,43,45,48,49,50,51,52,53,54,55,56,57,58,59];Alternative methods are widely accepted and preferred for future treatments, and Papacarie showed higher preference, mostly because of less induced pain [12,27,33,34,41,45,54,56,59] | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cardoso, M.; Coelho, A.; Lima, R.; Amaro, I.; Paula, A.; Marto, C.M.; Sousa, J.; Spagnuolo, G.; Marques Ferreira, M.; Carrilho, E. Efficacy and Patient’s Acceptance of Alternative Methods for Caries Removal—A Systematic Review. J. Clin. Med. 2020, 9, 3407. https://doi.org/10.3390/jcm9113407
Cardoso M, Coelho A, Lima R, Amaro I, Paula A, Marto CM, Sousa J, Spagnuolo G, Marques Ferreira M, Carrilho E. Efficacy and Patient’s Acceptance of Alternative Methods for Caries Removal—A Systematic Review. Journal of Clinical Medicine. 2020; 9(11):3407. https://doi.org/10.3390/jcm9113407
Chicago/Turabian StyleCardoso, Miguel, Ana Coelho, Rui Lima, Inês Amaro, Anabela Paula, Carlos Miguel Marto, José Sousa, Gianrico Spagnuolo, Manuel Marques Ferreira, and Eunice Carrilho. 2020. "Efficacy and Patient’s Acceptance of Alternative Methods for Caries Removal—A Systematic Review" Journal of Clinical Medicine 9, no. 11: 3407. https://doi.org/10.3390/jcm9113407
APA StyleCardoso, M., Coelho, A., Lima, R., Amaro, I., Paula, A., Marto, C. M., Sousa, J., Spagnuolo, G., Marques Ferreira, M., & Carrilho, E. (2020). Efficacy and Patient’s Acceptance of Alternative Methods for Caries Removal—A Systematic Review. Journal of Clinical Medicine, 9(11), 3407. https://doi.org/10.3390/jcm9113407









