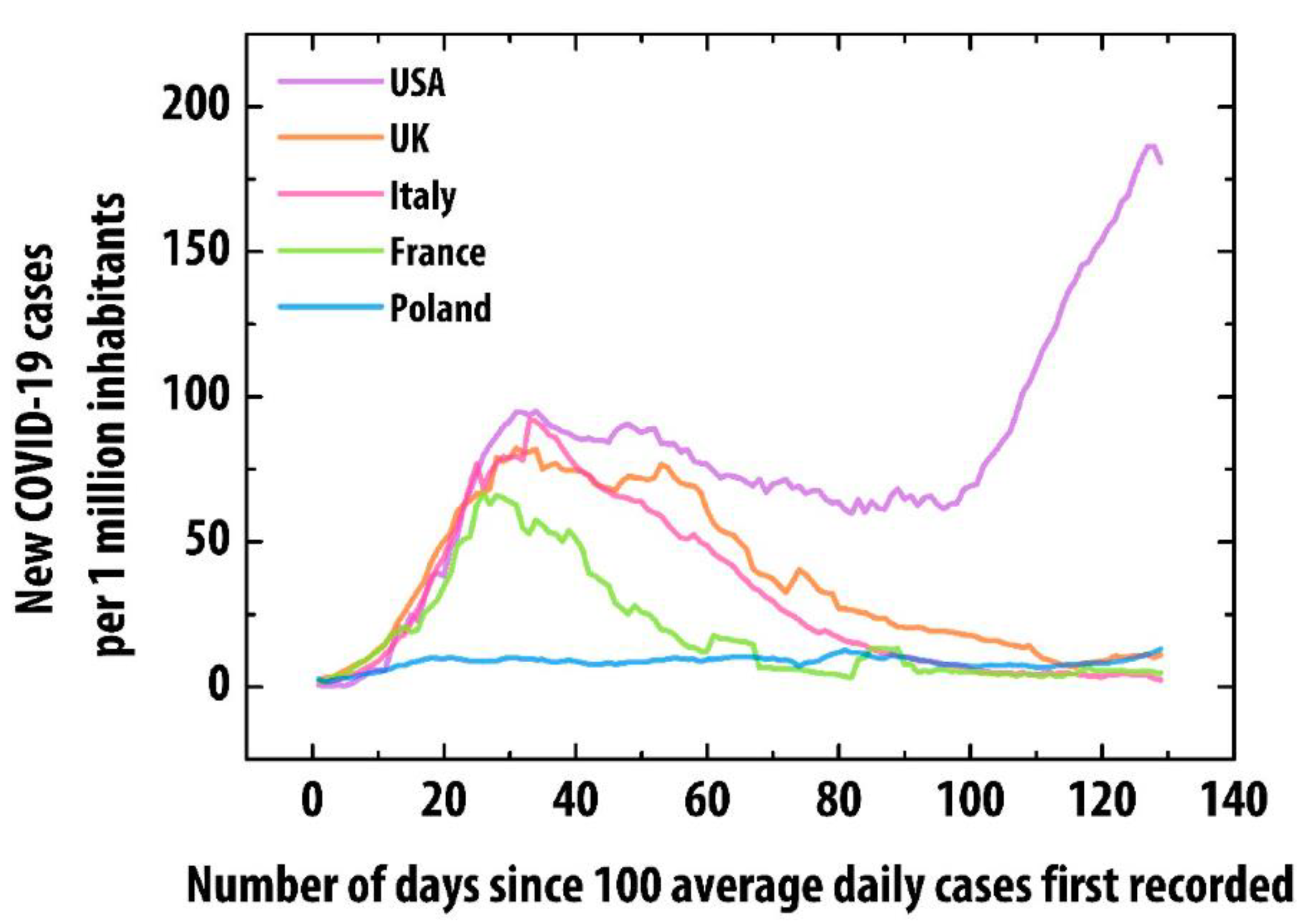
Pediatric Inflammatory Multisystem Syndrome (PIMS) Did Occur in Poland during Months with Low COVID-19 Prevalence, Preliminary Results of a Nationwide Register
Abstract
:1. Introduction
2. Experimental Section
- Patients who required hospitalization since 4 March. The end of the study will be defined by the declaration of the end of the COVID-19 pandemic by the World Health Organization; 0–18 years old;
- Diagnosed Kawasaki disease (KD) or incomplete (atypical) Kawasaki disease (aKD) or toxic shock syndrome (TSS) or macrophage activation syndrome (MAS) or unspecified inflammatory syndrome;
- Exclusion of other infectious and non-infectious causes that could be responsible for the disease;
- SARS-CoV-2 polymerase chain reaction (PCR) or serology result could have been positive or negative. Due to the limited availability and reliability of serologic testing, a proven or likely COVID-19 criterion was not a condition determining inclusion to the registry.
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Riphagen, S.; Gomez, X.; Gonzalez-Martinez, C.; Wilkinson, N.; Theocharis, P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 2020, 395, 1607–1608. [Google Scholar] [CrossRef]
- Verdoni, L.; Mazza, A.; Gervasoni, A.; Martelli, L.; Ruggeri, M.; Ciuffreda, M.; Bonanomi, E.; D’Antiga, L. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: An observational cohort study. Lancet 2020, 395, 1771–1778. [Google Scholar] [CrossRef]
- Whittaker, E.; Bamford, A.; Kenny, J.; Kaforou, M.; Jones, C.E.; Shah, P.; Ramnarayan, P.; Fraisse, A.; Miller, O.; Davies, P.; et al. Clinical Characteristics of 58 Children With a Pediatric Inflammatory Multisystem Syndrome Temporally Associated With SARS-CoV-2. JAMA 2020, 324, 259–269. [Google Scholar] [CrossRef]
- Toubiana, J.; Poirault, C.; Corsia, A.; Bajolle, F.; Fourgeaud, J.; Angoulvant, F.; Debray, A.; Basmaci, R.; Salvador, E.; Biscardi, S.; et al. Kawasaki-like multisystem inflammatory syndrome in children during the covid-19 pandemic in Paris, France: Prospective observational study. BMJ 2020, 369, m2094. [Google Scholar] [CrossRef]
- Dufort, E.M.; Koumans, E.H.; Chow, E.J.; Rosenthal, E.M.; Muse, A.; Rowlands, J.; Barranco, M.A.; Maxted, A.M.; Rosenberg, E.S.; Easton, D.; et al. Multisystem Inflammatory Syndrome in Children in New York State. N. Engl. J. Med. 2020, 383, 347–358. [Google Scholar] [CrossRef] [PubMed]
- Feldstein, L.R.; Rose, E.B.; Horwitz, S.M.; Collins, J.P.; Newhams, M.M.; Son, M.B.F.; Newburger, J.W.; Kleinman, L.C.; Heidemann, S.M.; Martin, A.A.; et al. Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. N. Engl. J. Med. 2020, 383, 334–346. [Google Scholar] [CrossRef] [PubMed]
- Belot, A.; Antona, D.; Renolleau, S.; Javouhey, E.; Hentgen, V.; Angoulvant, F.; Delacourt, C.; Iriart, X.; Ovaert, C.; Bader-Meunier, B.; et al. SARS-CoV-2-related paediatric inflammatory multisystem syndrome, an epidemiological study, France, 1 March to 17 May 2020. Eurosurveillance 2020, 25, 2001010. [Google Scholar] [CrossRef] [PubMed]
- Belhadjer, Z.; Méot, M.; Bajolle, F.; Khraiche, D.; Legendre, A.; Abakka, S.; Auriau, J.; Grimaud, M.; Oualha, M.; Beghetti, M.; et al. Acute heart failure in multisystem inflammatory syndrome in children (MIS-C) in the context of global SARS-CoV-2 pandemic. Circulation 2020, 142, 429–436. [Google Scholar] [CrossRef] [PubMed]
- Davies, P.; Evans, C.; Kanthimathinathan, H.K.; Lillie, J.; Brierley, J.; Waters, G.; Johnson, M.; Griffiths, B.; du Pré, P.; Mohammad, Z.; et al. Intensive care admissions of children with paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) in the UK: A multicentre observational study. Lancet Child Adolesc Health 2020, 4, 669–677. [Google Scholar] [CrossRef]
- Health Policy Team. Guidance—Paediatric Multisystem Inflammatory Syndrome Temporally Associated with COVID-19. Royal College of Paediatrics and Child Health: London, UK. Available online: https://www.rcpch.ac.uk/resources/guidance-paediatric-multisystem-inflammatory-syndrome-temporally-associated-covid-19 (accessed on 29 July 2020).
- Centers for Disease Control and Prevention (CDC). Information for Healthcare Providers about Multisystem Inflammatory Syndrome in Children (MIS-C). CDC: Atlanta, GA, USA. Available online: https://www.cdc.gov/mis-c/hcp/ (accessed on 29 July 2020).
- World Health Organization (WHO). Multisystem Inflammatory Syndrome in Children and Adolescents Temporally Related to COVID-19. WHO: Geneva, Switzerland, 15 May 2020. Available online: https://www.who.int/news-room/commentaries/detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19 (accessed on 29 July 2020).
- European Centre for Disease Prevention and Control (ECDC). Rapid Risk Assessment: Paediatric Inflammatory Multisystem Syndrome and SARS -CoV-2 Infection in Children. ECDC: Stockholm, Sweden, 2020. Available online: https://www.ecdc.europa.eu/en/publications-data/paediatric-inflammatory-multisystem-syndrome-and-sars-cov-2-rapid-risk-assessment (accessed on 29 July 2020).
- European Centre for Disease Prevention and Control (ECDC). COVID-19 Situation Update for the EU/EEA and the UK. ECDC: Stockholm, Sweden. Available online: https://www.ecdc.europa.eu/en/cases-2019-ncov-eueea (accessed on 29 July 2020).
- Coronavirus Update (Live). Worldometers.info. Available online: https://www.worldometers.info/coronavirus/ (accessed on 29 July 2020).
- Raciborski, F.; Pinkas, J.; Jankowski, M.; Sierpiński, R.; Zgliczyński, W.S.; Szumowski, Ł.; Rakocy, K.; Wierzba, W.; Gujski, M. Dynamics of COVID-19 outbreak in Poland: An epidemiological analysis of the first two months of the epidemic. Pol. Arch. Intern. Med. 2020, 130, 615–621. [Google Scholar] [CrossRef] [PubMed]
- McCrindle, B.W.; Rowley, A.H.; Newburger, J.W.; Burns, J.C.; Bolger, A.F.; Gewitz, M.; Baker, A.L.; Jackson, M.A.; Takahashi, M.; Shah, P.B.; et al. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals from the American Heart Association. Circulation 2017, 135, e927–e999. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Streptococcal Toxic Shock Syndrome (STSS) (Streptococcus pyogenes) 2010 Case Definition. CDC: Atlanta, GA, USA. Available online: https://wwwn.cdc.gov/nndss/conditions/streptococcal-toxic-shock-syndrome/case-definition/2010/ (accessed on 29 July 2020).
- Centers for Disease Control and Prevention (CDC). Toxic Shock Syndrome (Other Than Streptococcal) (TSS) 2011 Case Definition. CDC: Atlanta, GA, USA. Available online: https://wwwn.cdc.gov/nndss/conditions/toxic-shock-syndrome-other-than-streptococcal/case-definition/2011/ (accessed on 29 July 2020).
- Minoia, F.; Bovis, F.; Davì, S.; Horne, A.; Fischbach, M.; Frosch, M.; Huber, A.; Jelusic, M.; Sawhney, S.; McCurdy, D.K.; et al. Development and initial validation of the MS score for diagnosis of macrophage activation syndrome in systemic juvenile idiopathic arthritis. Ann. Rheum. Dis. 2019, 78, 1357–1362. [Google Scholar] [CrossRef] [PubMed]
- Tracewski, P.; Ludwikowska, K.M.; Szenborn, L.; Kusa, J. The first case of pediatric inflammatory multisystem syndrome (PIMS-TS) in Poland, complicated by giant coronary artery aneurysms. Kardiol. Pol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.; Cantor, A.; Zachariah, P.; Ahn, D.; Martinez, M.; Margolis, K. Gastrointestinal symptoms as a major presentation component of a novel multisystem inflammatory syndrome in children (MIS-C) that is related to COVID-19: A single center experience of 44 cases. Gastroenterology 2020, 159, 1571–1574. [Google Scholar] [CrossRef] [PubMed]
- Pouletty, M.; Borocco, C.; Ouldali, N.; Caseris, M.; Basmaci, R.; Lachaume, N.; Bensaid, P.; Pichard, S.; Kouider, H.; Morelle, G.; et al. Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 mimicking Kawasaki disease (Kawa-COVID-19): A multicentre cohort. Ann. Rheum. Dis. 2020, 79, 999–1006. [Google Scholar] [CrossRef]
- Ibarrondo, F.J.; Fulcher, J.A.; Goodman-Meza, D.; Elliott, J.; Hofmann, C.; Hausner, M.A.; Ferbas, K.G.; Tobin, N.H.; Aldrovandi, G.M.; Yang, O.O. Rapid Decay of Anti–SARS-CoV-2 Antibodies in Persons with Mild Covid-19. N. Engl. J. Med. 2020, 383, 1085–1087. [Google Scholar] [CrossRef]
- Long, Q.X.; Tang, X.J.; Shi, Q.L.; Li, Q.; Deng, H.J.; Yuan, J.; Hu, J.L.; Xu, W.; Zhang, Y.; Lv, F.J.; et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat. Med. 2020, 26, 1200–1204. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.M.; Thornburg, N.J.; Stubblefield, W.B.; Talbot, H.K.; Coughlin, M.M.; Feldstein, L.R.; Self, W.H. Change in Antibodies to SARS-CoV-2 Over 60 Days Among Health Care Personnel in Nashville, Tennessee. JAMA 2020. [Google Scholar] [CrossRef] [PubMed]
- Deeks, J.J.; Dinnes, J.; Takwoingi, Y.; Davenport, C.; Spijker, R.; Taylor-Phillips, S.; Adriano, A.; Beese, S.; Dretzke, J.; di Ruffano, L.F.; et al. Antibody tests for identification of current and past infection with SARS-CoV-2. Cochrane Database Syst. Rev. 2020, 6, CD013652. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Interim Guidelines for COVID-19 Antibody Testing. CDC: Atlanta, GA, USA. Available online: https://www.cdc.gov/coronavirus/2019-ncov/lab/resources/antibody-tests-guidelines.html (accessed on 10 August 2020).
- Ellinghaus, D.; Degenhardt, F.; Bujanda, L.; Buti, M.; Albillos, A.; Invernizzi, P.; Fernández, J.; Prati, D.; Baselli, G.; Asselta, R.; et al. Genomewide Association Study of Severe Covid-19 with Respiratory Failure. N. Engl. J. Med. 2020, 383, 1522–1534. [Google Scholar] [CrossRef]

| Study Inclusion Criteria: Age, Disease Severity, Timing, Diagnosis Criterion and Exclusion of Other Causes Must Be Fulfilled. |
|---|
| Age: 0–18 years |
| Disease severity: requiring hospitalization |
| Time frame: since 4 March 2020 (ongoing) |
| Diagnosis: Kawasaki disease (KD) OR incomplete (atypical) Kawasaki disease (aKD) OR toxic shock syndrome (TSS) OR macrophage activation syndrome (MAS) OR unspecified inflammatory syndrome |
| Kawasaki disease (KD) case definition |
Fever for at least 5 days and 4 from the following symptoms:
|
| Incomplete (atypical) Kawasaki disease (aKD) case definition: |
Fever for at least 5 days and 2 or 3 from the above symptoms OR infant with unexplained fever for at least 7 days AND CRP ≥ 3 mg/dl and/or ESR ≥ 40 mm/h AND
|
| Toxic shock syndrome (TSS) case definition: |
|
| Macrophage activation syndrome (MAS) case definition: |
Febrile patient with:
|
| Inflammatory syndrome case definition: |
|
| Exclusion of other infectious and non-infectious causes that could be responsible for the disease |
| SARS-CoV-2 testing may be positive or negative. |
| Characteristics | Overall (N = 39) | <5 Years (N = 25) | ≥5 Years (N = 14) | p-Value | SARS-CoV-2 History Positive (N = 9) | SARS-CoV-2 History Unknown (N = 18) | SARS-CoV-2 History and Results Negative (N = 12) | p-Value |
|---|---|---|---|---|---|---|---|---|
| n, n/N or Med (% or IQR) | n, n/N or Med (% or IQR) | n, n/N or Med (% or IQR) | n, n/N or Med (% or IQR) | n, n/N or Med (% or IQR) | n, n/N or Med (% or IQR) | |||
| Age [years] | 3.1 (1.4–6.6) | 1.8 (0.85–2.8) | 9.15 (6.4–12.15) | <0.01 * | 10.5 (7–13.4) | 3.3 (1.9–5.4) | 1.2 (0.5–1.6) | <0.01 * |
| Male sex | 29 (74%) | 21 (84%) | 8 (57%) | 0.42 | 4 (44%) | 13 (72%) | 12 (100%) | 0.047 * |
| Any comorbidities | 6/39 (15%) | 3/25 (12%) | 3/14 (21%) | 0.37 | 2/9 (22%) | 3/18 (17%) | 1/12 (8%) | 0.62 |
| Clinical features | ||||||||
| Any dermatologic | 37 (94%) | 20 (80%) | 13 (93%) | 0.39 | 7 (78%) | 17 (94%) | 11 (97%) | 0.39 |
| Rash | 34 (87%) | 22 (88%) | 12 (86%) | 0.60 | 6 (67%) | 17 (94%) | 11 (97%) | 0.11 |
| Hands and feet erythema or swelling | 23 (59%) | 13 (52%) | 10 (71%) | 0.20 | 7 (78%) | 11 (61%) | 5 (42%) | 0.24 |
| Any mucocutaneous | 30 (77%) | 23 (92%) | 10 (71%) | 0.11 | 5 (56%) | 15 (83%) | 10 (83%) | 0.22 |
| Conjunctivitis | 26 (67%) | 17 (68%) | 9 (64%) | 0.54 | 4 (44%) | 13 (72%) | 9 (75%) | 0.27 |
| Mucosal changes | 27 (69%) | 18 (72%) | 9 (64%) | 0.43 | 4 (44%) | 15 (83%) | 8 (67%) | 0.12 |
| Lymphadenopathy | 20 (51%) | 15 (60%) | 5 (36%) | 0.13 | 3 (33%) | 9 (50%) | 8 (67%) | 0.32 |
| Any musculoskeletal | 15 (39%) | 6 (24%) | 9 (64%) | 0.01 * | 5 (56%) | 6 (33%) | 4 (33%) | 0.48 |
| Arthritis (swollen joints) | 8 (21%) | 2 (8%) | 6 (43%) | 0.01 * | 4 (44%) | 3 (17%) | 1 (8%) | 0.11 |
| Arthralgia (without swelling) | 9 (23%) | 2 (8%) | 7 (50%) | <0.01 * | 3 (33%) | 5 (28%) | 1 (8%) | 0.33 |
| Myalgia | 7 (18%) | 3 (12%) | 4 (29%) | 0.19 | 3 (33%) | 1 (6%) | 3 (25%) | 0.15 |
| Any gastrointestinal | 24 (62%) | 13 (52%) | 11 (79%) | 0.09 | 7 (78%) | 10 (56%) | 7 (56%) | 0.52 |
| Nausea or vomiting | 15 (40%) | 6 (24%) | 9 (64%) | 0.02 * | 5 (56%) | 6 (33%) | 4 (33%) | 0.48 |
| Abdominal pain | 16 (42%) | 6 (24%) | 10 (71%) | <0.01 * | 5 (56%) | 7 (39%) | 4 (33%) | 0.22 |
| Diarrhea | 13 (33%) | 8 (32%) | 5 (36%) | 0.54 | 5 (56%) | 4 (22%) | 4 (33%) | 0.22 |
| Any neurologic | 30 (77%) | 21 (84%) | 10 (71%) | 0.29 | 5 (56%) | 13 (72%) | 11 (92%) | 0.16 |
| Neck stiffness | 3 (8%) | 2 (8%) | 1 (7%) | 0.71 | 1 (11%) | 0 | 2 (17%) | 0.61 |
| Somnolence | 17 (44%) | 12 (48%) | 5 (36%) | 0.34 | 4 (44%) | 6 (33%) | 7 (58%) | 0.39 |
| Headache | 6 (15%) | 0 | 6 (43%) | 0.001 * | 5 (56%) | 1 (6%) | 0 | <0.01 * |
| Any respiratory | 16 (41%) | 14 (56%) | 4 (29%) | 0.09 | 4 (44%) | 5 (28%) | 7 (58%) | 0.24 |
| Cough | 6 (15%) | 4 (16%) | 2 (14%) | 0.63 | 2 (22%) | 2 (11%) | 2 (17%) | 0.74 |
| Chest pain | 1 (3%) | 0 | 1 (7%) | - | 1 (11%) | 0 | 0 | - |
| Dyspnea | 4 (10%) | 2 (8%) | 2 (14%) | 0.45 | 2 (22%) | 0 | 2 (17%) | 0.42 |
| Characteristics | Overall (N = 39) | <5 Years (N = 25) | ≥5 Years (N = 14) | p-Value | SARS-CoV-2 History Positive (N = 9) | SARS-CoV-2 History Unknown (N = 18) | SARS-CoV-2 History and Results Negative (N = 12) | p-Value |
|---|---|---|---|---|---|---|---|---|
| n, n/N or Med (% or IQR) | n, n/N or Med (% or IQR) | n, n/N or Med (% or IQR) | n, n/N or Med (% or IQR) | n, n/N or Med (% or IQR) | n, n/N or Med (% or IQR) | |||
| Time from symptom onset to hospital admission [days] | 4.0 (2.0–7.5) | 5.0 (2.0–9.0) | 4.0 (2.5–6.0) | 0.37 | 4.0 (2.0–6.0) | 5.0 (2.25–9.0) | 4.5 (2.75–5.25) | 0.56 |
| SARS-CoV-2 epidemiological data | ||||||||
| Confirmed contact with COVID-19 | 6/29 (21%) | 0/17 | 6/12 (50%) | <0.01 * | 6/8 (75%) | 0/12 | 0/9 | - |
| SARS CoV2 RT-PCR test positive | 1/34 (3%) | 0/21 | 1/13 (8%) | - | 1/9 (11%) | 0/13 | 0/12 | - |
| SARS CoV-2 serology test positive a | 6/21 (29%) | 1/13 (8%) | 5/8 (63%) | 0.011 * | 6/9 (67%) | 0/0 | 0/12 | - |
| Diagnosis | ||||||||
| Classic KD | 20 (51%) | 13 (33%) | 7 (50%) | 0.58 | 4 (44%) | 10 (56%) | 6 (50%) | 0.85 |
| Incomplete (atypical) KD | 14 (36%) | 10 (26%) | 4 (29%) | 0.36 | 3 (33%) | 6 (33%) | 5 (42%) | 0.88 |
| MAS | 10 (26%) | 3 (12%) | 7 (50%) | 0.014 * | 5 (56%) | 4 (22%) | 1 (8%) | 0.04 * |
| Inflammatory syndrome | 5 (13%) | 2 (8%) | 3 (21%) | 0.24 | 2 (22%) | 2 (11%) | (8%) | 0.61 |
| Therapy | ||||||||
| Intensive care treatment | 1 (3%) | 0 | 1 (7%) | - | 1 (11%) | 0 | 0 | - |
| High-flow nasal cannula | 5 (13%) | 3 (12%) | 2 (14%) | 0.60 | 3 (33%) | 0 | 2 (17%) | 0.17 |
| IVIG | 35 (90%) | 24 (96%) | 11 (79%) | 0.12 | 7 (78%) | 16 (89%) | 12 (100%) | 0.61 |
| GCS | 15 (39%) | 5 (20%) | 10 (71%) | <0.01 * | 7 (78%) | 6 (33%) | 2 (17%) | 0.02 * |
| GCS and IVIG | 14 (36%) | 5 (20%) | 9 (64%) | <0.01 * | 6 (67%) | 6 (33%) | 2 (17%) | 0.06 |
| Cyclosporine A | 4 (10%) | 1 (4%) | 3 (21%) | 0.12 | 2 (22%) | 2 (11%) | 0 | 0.61 |
| Etoposide | 1 (3%) | 0 | 1 (7%) | - | 0 | 1 (6%) | 0 | - |
| ASA | 33 (85%) | 24 (96%) | 9 (64%) | 0.016 * | 6 (67%) | 15 (83%) | 12 (100%) | 0.29 |
| Heparin | 2 (5%) | 1 (4%) | 1 (7%) | 0.59 | 1 (11%) | 1 (6%) | 0 | - |
| Warfarin | 1 (3%) | 1 (4%) | 0 | - | 1 (11%) | 0 | 0 | - |
| Clinical course and outcome | ||||||||
| Shock | 1 (3%) | 0 | 1 (7%) | - | 1 (11%) | 0 | 0 | - |
| Coronary arteries dilations or aneurysms b | 6 (15%) | 3 (12%) | 3 (21%) | 0.36 | 3 (33%) | 2 (11%) | 1 (8%) | 0.23 |
| Discharged without complications c | 30 (77%) | 19 (76%) | 11 (79%) | 0.57 | 4 (44%) | 15 (78%) | 11 (92%) | 0.03 * |
| Characteristics a | Overall (N = 39) | <5 Years (N = 25) | ≥5 Years (N = 14) | p-Value | SARS-CoV-2 History Positive (N = 9) | SARS-CoV-2 History Unknown (N = 18) | SARS-CoV-2 History and Results Negative (N = 12) | p-Value | |
|---|---|---|---|---|---|---|---|---|---|
| Med (IQR) | Med (IQR) | Med (IQR) | Med (IQR) | Med (IQR) | Med (IQR) | ||||
| White-cell count [×109/L] | Min | 8.0 (5.4–10.6) | 8.2 (6.5–11.0) | 5.5 (4.1–8.6) | <0.01 * | 6.5 (4.0–10.4) | 7.0 (5.6–9.3) | 9.2 (7.0–11.1) | 0.77 |
| Max | 18.0 (4.6–22.6) | 17.8 (15.2–22.6) | 18.1 (10.9–23.2) | 0.96 | 18.0 (14.8–23.9) | 17.9 (13.0–20.4) | 18.4 (15.3–23.2) | 0.89 | |
| Lymphocytes count [×109/L] | 2.0 (1.05–3.5) | 3.1 (2.0–4.94) | 0.9 (0.6–1.1) | <0.01 * | 0.8 (0.6–1.1) | 2.0 (1.1–2.8) | 4.5 (2.8–5.7) | <0.01 * | |
| Platelet count [×109/L] | Min | 236.0 (150.0–465.0) | 306.0 (203.0–530.0) | 175.5 (125.5–298.0) | 0.07 | 164.0 (124.0–180.0) | 296.0 (195.3–455.8) | 359.5 (225.5–549.0) | 0.15 |
| Max | 637.0 (495.0–830.5) | 693.0 (530.0–862.0) | 558.0 (413.0–727.6) | 0.16 | 488.0 (328.0–522.0) | 668.5 (541.6–769.5) | 768.5 (616.3–980.6) | 0.04 * | |
| CRP [mg/dL] | 129.2 (76.7–177.9) | 128.4 (100.9–161.5) | 132.0 (74.3–202.0) | 0.53 | 190.0 (131.0–246.9) | 107.0 (72.5–134.5) | 128.8 (89.9–175.8) | 0.03 * | |
| Ferritin [ng/mL] | 352.6 (156.2–1867.8) | 164.0 (90.7–565.0) | 1335.0 (352.6–9230.5) | 0.02 * | 1314.0 (330.0–3097.0) | 1458.0 (133.9–27908.0) | 175.5 (119.0–355.8) | 0.37 | |
| D-dimer [mg/L] | 3.6 (2.3–7.8) | 3.5 (1.6–4.9) | 2.9 (2.3–23.4) | 0.36 | 2.9 (2.5–48.3) | 2.3 (1.4–5.6) | 4.2 (3.4–5.2) | 0.38 | |
| Albumin [g/dL] | 3.1 (2.6–3.5) | 3.1 (2.8–3.4) | 3.3 (2.5–3.5) | 0.87 | 2.9 (2.4–3.5) | 3.3 (3.1–3.6) | 3.0 (2.7–3.2) | 0.09 | |
| ALT [U/L] | 32.0 (16.0–96.0) | 19.0 (15.0–55.0) | 69.5 (27.5–214.8) | 0.04 * | 32.0 (16.0–178.0) | 51.5 (19.0–100.5) | 23.0 (14.5–57.7) | 0.27 | |
| Sodium [mmol/L] | 135.0 (132.0–136.0) | 135.3 (132.0–136.0) | 134.5 (129.5–138.3) | 0.43 | 131.0 (129.0–134.0) | 136.0 (132.3–139.0) | 135.5 (133.0–136.0) | 0.01 * | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okarska-Napierała, M.; Ludwikowska, K.M.; Szenborn, L.; Dudek, N.; Mania, A.; Buda, P.; Książyk, J.; Mazur-Malewska, K.; Figlerowicz, M.; Szczukocki, M.; et al. Pediatric Inflammatory Multisystem Syndrome (PIMS) Did Occur in Poland during Months with Low COVID-19 Prevalence, Preliminary Results of a Nationwide Register. J. Clin. Med. 2020, 9, 3386. https://doi.org/10.3390/jcm9113386
Okarska-Napierała M, Ludwikowska KM, Szenborn L, Dudek N, Mania A, Buda P, Książyk J, Mazur-Malewska K, Figlerowicz M, Szczukocki M, et al. Pediatric Inflammatory Multisystem Syndrome (PIMS) Did Occur in Poland during Months with Low COVID-19 Prevalence, Preliminary Results of a Nationwide Register. Journal of Clinical Medicine. 2020; 9(11):3386. https://doi.org/10.3390/jcm9113386
Chicago/Turabian StyleOkarska-Napierała, Magdalena, Kamila M. Ludwikowska, Leszek Szenborn, Natalia Dudek, Anna Mania, Piotr Buda, Janusz Książyk, Katarzyna Mazur-Malewska, Magdalena Figlerowicz, Maciej Szczukocki, and et al. 2020. "Pediatric Inflammatory Multisystem Syndrome (PIMS) Did Occur in Poland during Months with Low COVID-19 Prevalence, Preliminary Results of a Nationwide Register" Journal of Clinical Medicine 9, no. 11: 3386. https://doi.org/10.3390/jcm9113386
APA StyleOkarska-Napierała, M., Ludwikowska, K. M., Szenborn, L., Dudek, N., Mania, A., Buda, P., Książyk, J., Mazur-Malewska, K., Figlerowicz, M., Szczukocki, M., Kucińska, B., Werner, B., Stopyra, L., Czech, A., Berdej-Szczot, E., Gawlik, A., Opalińska, P., Mazur, A., Januszkiewicz-Lewandowska, D., ... Kuchar, E. (2020). Pediatric Inflammatory Multisystem Syndrome (PIMS) Did Occur in Poland during Months with Low COVID-19 Prevalence, Preliminary Results of a Nationwide Register. Journal of Clinical Medicine, 9(11), 3386. https://doi.org/10.3390/jcm9113386












