Estimating Minimal Clinically Important Differences for Knee Range of Motion after Stroke
Abstract
1. Introduction
2. Materials and Methods
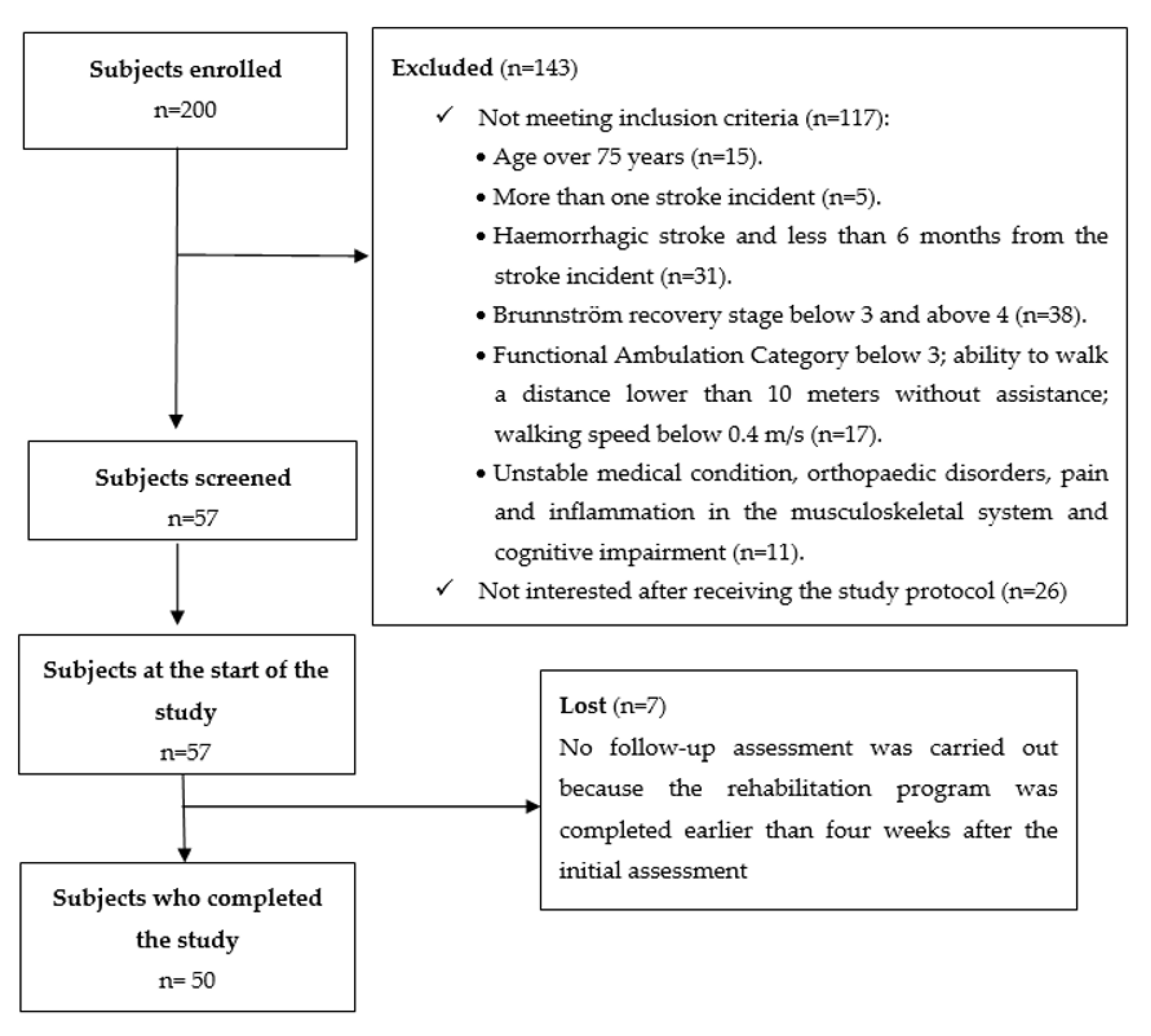
2.1. Participants
2.2. Measures
2.3. Data Analysis
2.4. Procedures
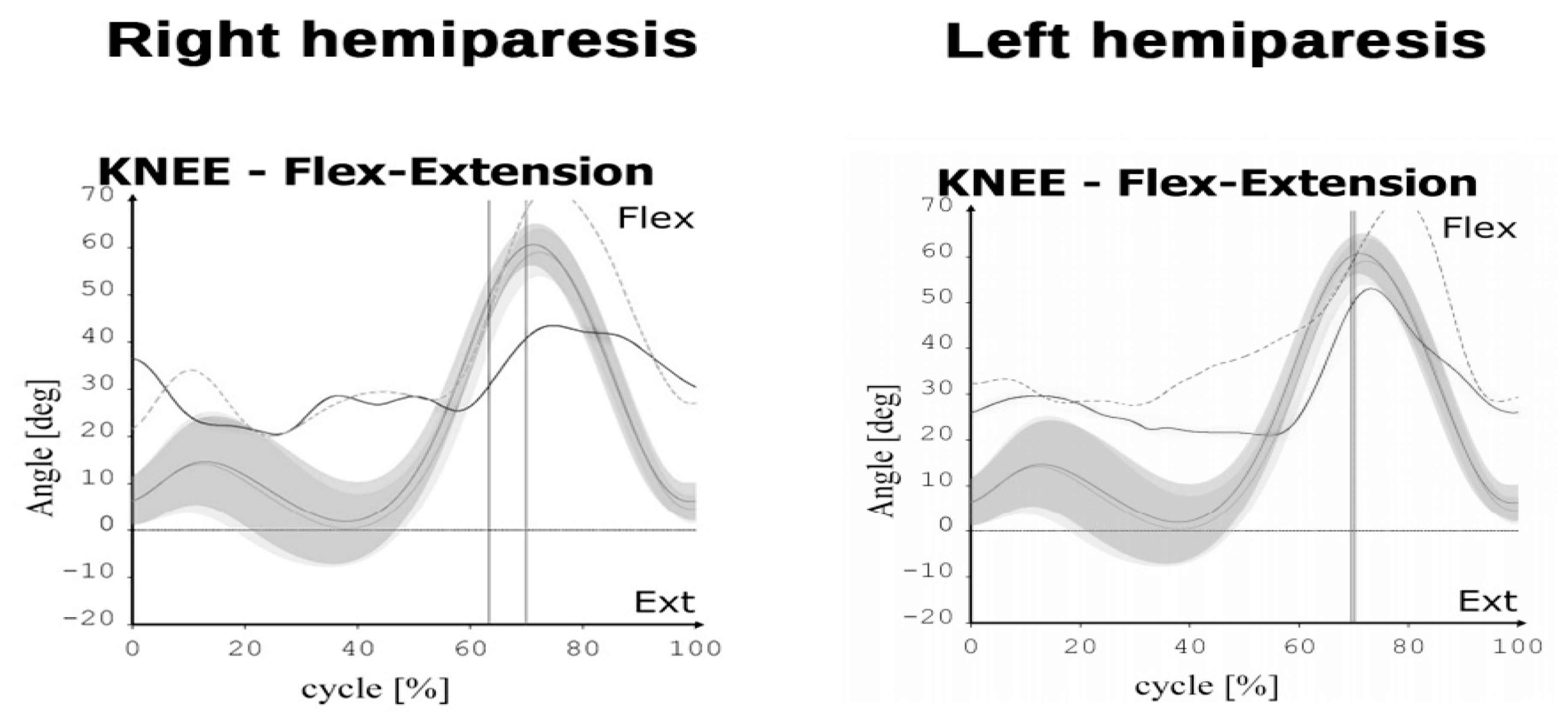
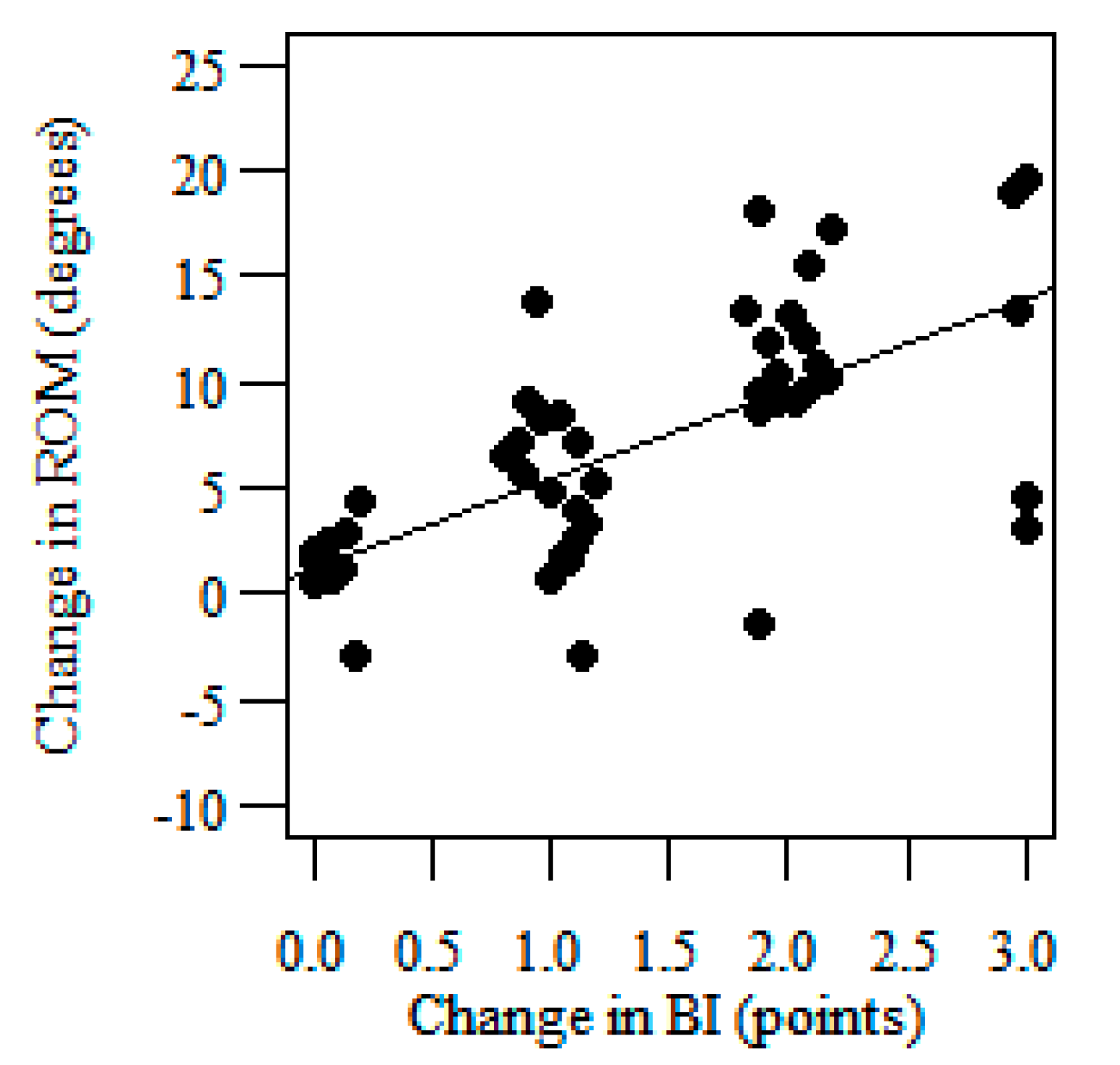
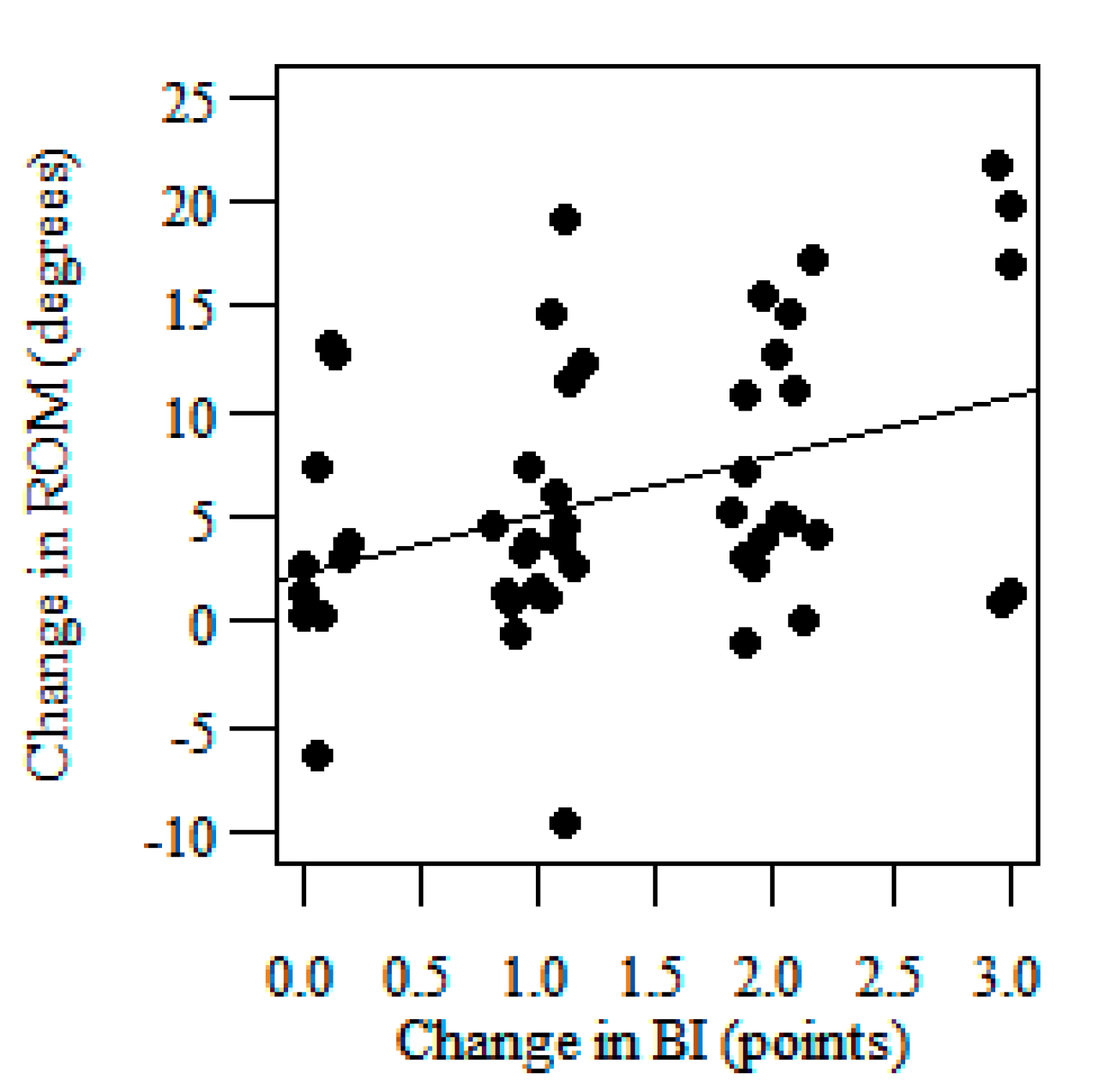
3. Results
4. Discussion
Study Limitation
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- An, S.; Lee, Y.; Shin, H.; Lee, G. Gait velocity and walking distance to predict community walking after stroke. Nurs. Health Sci. 2015, 17, 533–538. [Google Scholar] [CrossRef] [PubMed]
- van Bloemendaal, M.; van de Water, A.T.; van de Port, I.G. Walking tests for stroke survivors: A systematic review of their measurement properties. Disabil. Rehabil. 2012, 34, 2207–2221. [Google Scholar] [CrossRef] [PubMed]
- Kosak, M.; Smith, T. Comparison of the 2-, 6-, and 12-minute walk tests in patients with stroke. J. Rehabil. Res. Dev. 2005, 42, 103–107. [Google Scholar] [CrossRef] [PubMed]
- Hafsteinsdóttir, T.B.; Rensink, M.; Schuurmans, M. Clinimetric properties of the Timed Up and Go Test for patients with stroke: A systematic review. Top. Stroke. Rehabil. 2014, 21, 197–210. [Google Scholar] [CrossRef] [PubMed]
- Wonsetler, E.C.; Bowden, M.G. A systematic review of mechanisms of gait speed change post-stroke. Part 1: Spatiotemporal parameters and asymmetry ratios. Top. Stroke Rehabil. 2017, 24, 435–446. [Google Scholar] [CrossRef]
- Patterson, K.K.; Nadkarni, N.K.; Black, S.E.; McIlroy, W.E. Temporal gait symmetry and velocity differ in their relationship to age. Gait Posture 2012, 35, 590–594. [Google Scholar] [CrossRef]
- Barak, S.; Duncan, P.W. Issues in selecting outcome measures to assess functional recovery after stroke. NeuroRx 2006, 3, 505–524. [Google Scholar] [CrossRef]
- Jaeschke, R.; Singer, J.; Guyatt, G.H. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin. Trials 1989, 10, 407–415. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Andrews, A.W.; Glenney, S.S. Minimal clinically important difference for comfortable speed as a measure of gait performance in patients undergoing inpatient rehabilitation after stroke. J. Phys. Ther. Sci. 2013, 25, 1223–1225. [Google Scholar] [CrossRef]
- Bushnell, C.; Bettger, J.P.; Cockroft, K.M.; Cramer, S.C.; Edelen, M.O.; Hanley, D.; Katzan, I.L.; Mattke, S.; Nilsen, D.M.; Piquado, T.; et al. Chronic Stroke Outcome Measures for Motor Function Intervention Trials: Expert Panel Recommendations. Circ. Cardiovasc. Qual. Outcomes 2015, 8, S163–S169. [Google Scholar] [CrossRef]
- Fulk, G.D.; He, Y. Minimal Clinically Important Difference of the 6-Minute Walk Test in People with Stroke. J. Neurol. Phys. Ther. 2018, 42, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.; McGinley, J.L.; Schwartz, M.H.; Beynon, S.; Rozumalski, A.; Graham, K.; Tirosh, O. The gait profile score and movement analysis profile. Gait Posture 2009, 30, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Kazemi, M.; Dabiri, Y.; Li, L.P. Recent Advances in Computational Mechanics of the Human Knee Joint. Comput. Math. Methods. Med. 2013, 2013, 718423. [Google Scholar] [CrossRef] [PubMed]
- Reicher, M.; Bochenek, A. Human Anathomy. General Anatomy. Bones, Joints and Ligaments; PZWL Press: Warsaw, Poland, 2008. [Google Scholar]
- Perry, J.; Garret, M.; Gronley, J.K.; Mulroy, S.J. Classification of walking handicap in the stroke population. Stroke 1995, 26, 982–989. [Google Scholar] [CrossRef] [PubMed]
- McGinley, J.L.; Baker, R.; Wolfe, R.; Morris, M.E. The reliability of three-dimensional kinematic gait measurements: A systematic review. Gait Posture 2009, 29, 360–369. [Google Scholar] [CrossRef] [PubMed]
- Nadeau, S.; Betschart, M.; Bethoux, F. Gait analysis for poststroke rehabilitation: The relevance of biomechanical analysis and the impact of gait speed. Phys. Med. Rehabil. Clin. N. Am. 2013, 24, 265–276. [Google Scholar] [CrossRef] [PubMed]
- Boudarham, J.; Roche, N.; Pradon, D.; Bonnyaud, C.; Bensmail, D.; Zory, R. Variations in kinematics during clinical gait analysis in stroke patients. PLoS ONE 2013, 8, e66421. [Google Scholar] [CrossRef] [PubMed]
- Cooper, A.; Alghamdi, G.A.; Alghamdi, M.A.; Altowaijri, A.; Richardson, S. The relationship of lower limb muscle strength and knee joint hyperextension during the stance phase of gait in hemiparetic stroke patients. Physiother. Res. Int. 2012, 17, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Kaczmarczyk, K.; Wit, A.; Krawczyk, M.; Zaborski, J. Gait classification in post-stroke patients using artificial neural networks. Gait Posture 2009, 30, 207–210. [Google Scholar] [CrossRef]
- Mun, B.M.; Lee, Y.S.; Kim, T.H.; Lee, J.H.; Sim, S.M.; Park, I.M.; Seo, D.K. Study on the usefulness of sit to stand training in self-directed treatment of stroke patients. J. Phys. Ther. Sci. 2014, 26, 483–485. [Google Scholar] [CrossRef][Green Version]
- Beyaert, C.; Vasa, R.; Frykberg, G.E. Gait post-stroke: Pathophysiology and rehabilitation strategies. Neurophysiol. Clin. 2015, 45, 335–355. [Google Scholar] [CrossRef] [PubMed]
- De Quervain, I.A.; Simon, S.R.; Leurgans, S.; Pease, W.S.; McAllister, D. Gait pattern in the early recovery period after stroke. J. Bone Joint Surg. Am. 1996, 78, 1506–1514. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.M.; Eng, J.J. Magnitude and pattern of 3D kinematic and kinetic gait profiles in persons with stroke: Relationship to walking speed. Gait Posture 2004, 20, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Mulroy, S.; Gronley, J.; Weiss, W.; Newsam, C.; Perry, J. Use of cluster analysis for gait pattern classification of patients in the early and late recovery phases following stroke. Gait Posture 2003, 18, 114–125. [Google Scholar] [CrossRef]
- Olney, S.J.; Griffin, M.P.; Monga, T.N.; McBride, I.D. Work and power in gait of stroke patients. Arch. Phys. Med. Rehabil. 1991, 72, 309–314. [Google Scholar] [PubMed]
- Kinsella, S.; Moran, K. Gait pattern categorization of stroke participants with equinus deformity of the foot. Gait Posture 2008, 27, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Olney, S.J.; Griffin, M.P.; McBride, I.D. Multivariate examination of data from gait analysis of persons with stroke. Phys. Ther. 1998, 78, 814–828. [Google Scholar] [CrossRef]
- Davis, R.B.; Õunpuu, S.; Tyburski, D.; Gage, J.R. A gait analysis data collection and reduction technique. Hum. Mov. Sci. 1991, 10, 575–587. [Google Scholar] [CrossRef]
- Collin, C.; Wade, D.T.; Davies, S.; Horne, V. The Barthel ADL Index: A reliability study. Int. Disabil. Stud. 1998, 10, 61–63. [Google Scholar] [CrossRef]
- Hsueh, I.P.; Lee, M.M.; Hsieh, C.L. Psychometric characteristics of the Barthel Activities of Daily Living Index in stroke patients. J. Formos. Med. Assoc. 2001, 100, 526–532. [Google Scholar]
- Hsieh, Y.W.; Wang, C.H.; Wu, S.C.; Chen, P.C.; Sheu, C.F.; Hsieh, C.L. Establishing the minimal clinically important difference of the Barthel Index in stroke patients. Neurorehabil. Neural. Repair. 2007, 21, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Beaton, D.E.; Bombardier, C.; Katz, J.N.; Wright, J.G.; Wells, G.; Boers, M.; Strand, V.; Shea, B. Looking for important change/differences in studies of responsiveness. OMERACT MCID Working Group. Outcome Measures in Rheumatology. Minimal Clinically Important Difference. J. Rheumatol. 2001, 28, 400–405. [Google Scholar] [PubMed]
- Hagg, O.; Fritzell, P.; Nordwall, A. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur. Spine J. 2003, 12, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Lydick, E.; Epstein, R.S. Interpretation of quality of life changes. Qual. Life Res. 1993, 2, 221–226. [Google Scholar] [CrossRef]
- Wyrwich, K.W. Minimal important difference thresholds and the standard error of measurement: Is there a connection? J. Biopharm. Stat. 2004, 14, 97–110. [Google Scholar] [CrossRef]
- Crosby, R.D.; Kolotkin, R.L.; Williams, G.R. Defining clinically meaningful change in health-related quality of life. J. Clin. Epidemiol. 2003, 56, 395–407. [Google Scholar] [CrossRef]
- Hastie, T.; Tibshirani, R.; Friedman, J. The Elements of Statistical Learning: Data Mining, Inference, and Prediction; Springer Press: New York, NY, USA, 2009. [Google Scholar]
- Hoffman, J.I.E. Variations Based on Linear Regression, in Biostatistics for Medical and Biomedical Practitioners; Academic Press: London, UK, 2015. [Google Scholar]
- Beninato, M.; Gill-Body, K.M.; Salles, S.; Stark, P.C.; Black-Schaffer, R.M.; Stein, J. Determination of the minimal clinically important difference in the FIM instrument in patients with stroke. Arch. Phys. Med. Rehabil. 2006, 87, 32–39. [Google Scholar] [CrossRef]
- Stratford, P.W.; Binkley, F.M.; Riddle, D.L. Health status measures: Strategies and analytic methods for assessing change scores. Phys. Ther. 1996, 76, 1109–1123. [Google Scholar] [CrossRef]
- Guzik, A.; Drużbicki, M. Application of the Gait Deviation Index in the analysis of post-stroke hemiparetic gait. J. Biomech. 2020, 99, 109575. [Google Scholar] [CrossRef]
- Carmo, A.A.; Kleiner, A.F.; Costa, P.H.; Barros, R.M. Three-dimensional kinematic analysis of upper and lower limb motion during gait of post-stroke patients. Braz. J. Med. Biol. Res. 2012, 45, 537–545. [Google Scholar] [CrossRef]
- Drużbicki, M.; Guzik, A.; Przysada, G.; Kwolek, A.; Brzozowska-Magoń, A.; Sobolewski, M. Changes in Gait Symmetry After Training on a Treadmill with Biofeedback in Chronic Stroke Patients: A 6-Month Follow-Up from a Randomized Controlled Trial. Med. Sci. Monit. 2016, 22, 4859–4868. [Google Scholar] [CrossRef] [PubMed]
- Duncan, P.W.; Lai, S.M.; Keighley, J. Defining post-stroke recovery: Implications for design and interpretation of drug trials. Neuropharmacology 2000, 39, 835–841. [Google Scholar] [CrossRef]
- Lee, K.B.; Lim, S.H.; Kim, K.H.; Kim, K.J.; Kim, Y.R.; Chang, W.N.; Yeom, J.W.; Kim, Y.D.; Hwang, B.Y. Six-month functional recovery of stroke patients: A multi-time-point study. Int. J. Rehabil. Res. 2015, 38, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Dąbrowski, J.; Czajka, A.; Zielińska-Turek, J.; Jaroszyński, J.; Furtak-Niczyporuk, M.; Mela, A.; Poniatowski, Ł.A.; Drop, B.; Dorobek, M.; Barcikowska-Kotowicz, M.; et al. Brain Functional Reserve in the Context of Neuroplasticity after Stroke. Neural. Plast. 2019, 2019, 9708905. [Google Scholar] [CrossRef]
- Kopp, B.; Kunkel, A.; Muhlnickel, W.; Villringer, K.; Taub, E.; Flor, H. Plasticity in the motor system related to therapy-induced improvement of movement after stroke. Neuroreport 1990, 10, 807–810. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
| Group N = 50 | |
|---|---|
| Mean age, (SD) | 60.9 ± 11.2 |
| Mean time from stroke (months), range | 42 (8–120) |
| Sex (women/men) | 18/32 |
| Hemisphere lesions (right/left) | 15/35 |
| Knee Flexion/Extension Range of Motion, N = 50 | |
|---|---|
| Baseline ROM affected side (deg.), mean (SD) | 34.62 (9.71) |
| Follow-up ROM affected side (deg.), mean (SD) | 41.58 (9.52) |
| Baseline ROM unaffected side (deg.), mean (SD) | 42.33 (8.52) |
| Follow-up ROM unaffected side (deg.), mean (SD) | 48.78 (8.84) |
| Baseline ROM right side (deg.), mean (SD) | 36.9 (10.24) |
| Follow-up ROM right side (deg.), mean (SD) | 44.63 (10.2) |
| Baseline ROM left side (deg.), mean (SD) | 40.08 (9.44) |
| Follow-up ROM left side (deg.), mean (SD) | 45.43 (9.67) |
| Mean Knee Sagittal ROM—MCID Group, N = 34 | |
| Baseline ROM affected side (deg.), mean (SD) | 33.6 (9.34) |
| Follow-up ROM affected side (deg.), mean (SD) | 42.1 (9.2) |
| Baseline ROM unaffected side (deg.), mean (SD) | 41.64 (8.95) |
| Follow-up ROM unaffected side (deg.), mean (SD) | 48.45 (9.25) |
| Mean Knee Sagittal ROM—No-change Group, N = 16 | |
| Baseline ROM affected side (deg.), mean (SD) | 38.23 (11.0) |
| Follow-up ROM affected side (deg.), mean (SD) | 39.8 (11.26) |
| Baseline ROM unaffected side (deg.), mean (SD) | 44.88 (7.77) |
| Follow-up ROM unaffected side (deg.), mean (SD) | 48.6 (9.55) |
| MCID (deg.) | 95% Confidence Interval | ||
|---|---|---|---|
| Anchor-Based Method | 8.48 | 6.7 | 10.26 |
| Distribution-Based Method | 1.86 | 1.3 | 3.27 |
| Linear Regression Analysis | 7.71 | 5.22 | 10.2 |
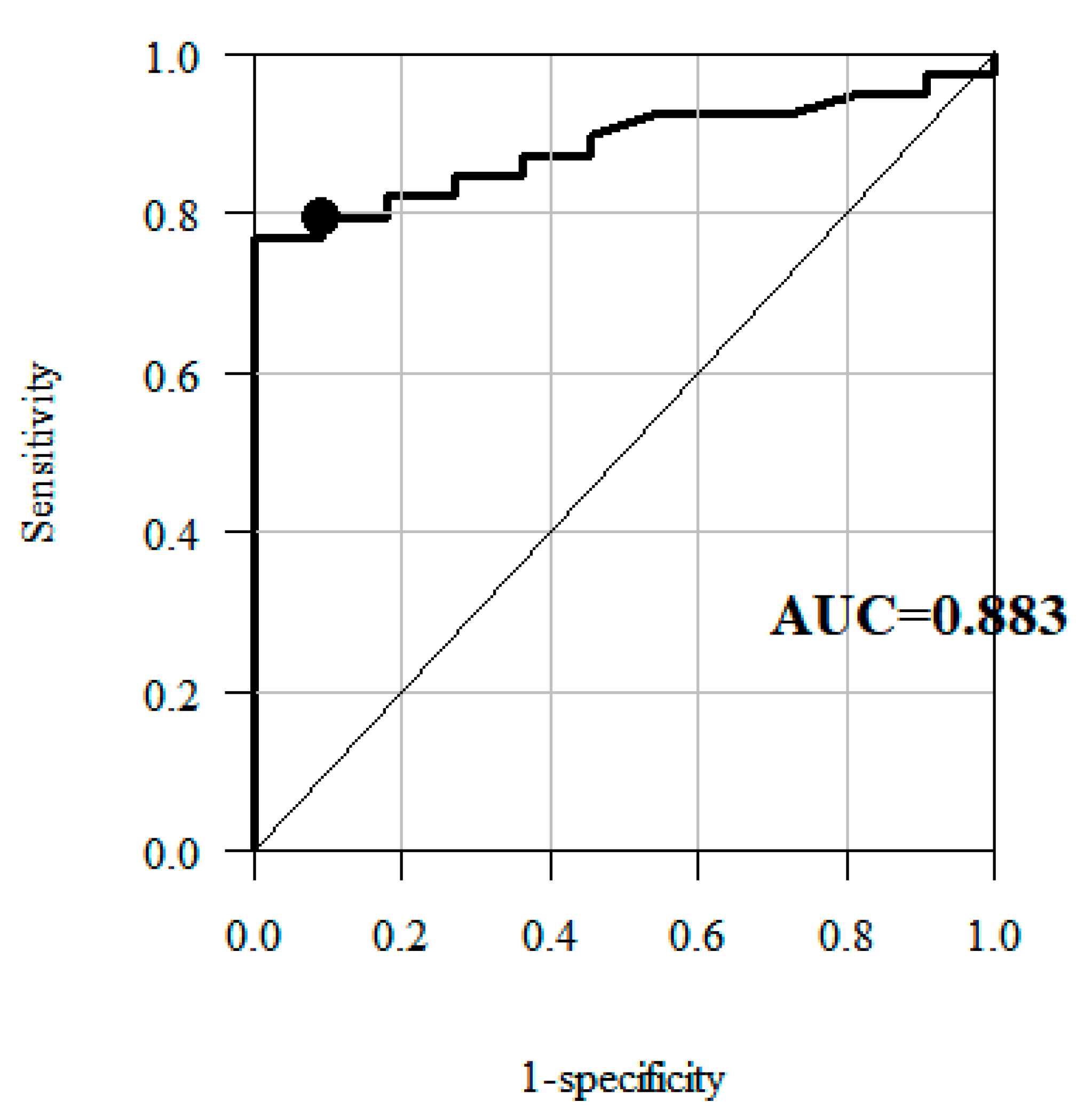
| Receiver operating characteristic Curve | 3.9 | --- | --- |
| MCID (deg.) | 95% Confidence Interval | ||
|---|---|---|---|
| Anchor-Based Method | 6.81 | 4.57 | 9.05 |
| Distribution-Based Method | 5.63 | 3.93 | 9.88 |
| Linear Regression Analysis | 4.66 | 0.95 | 8.37 |
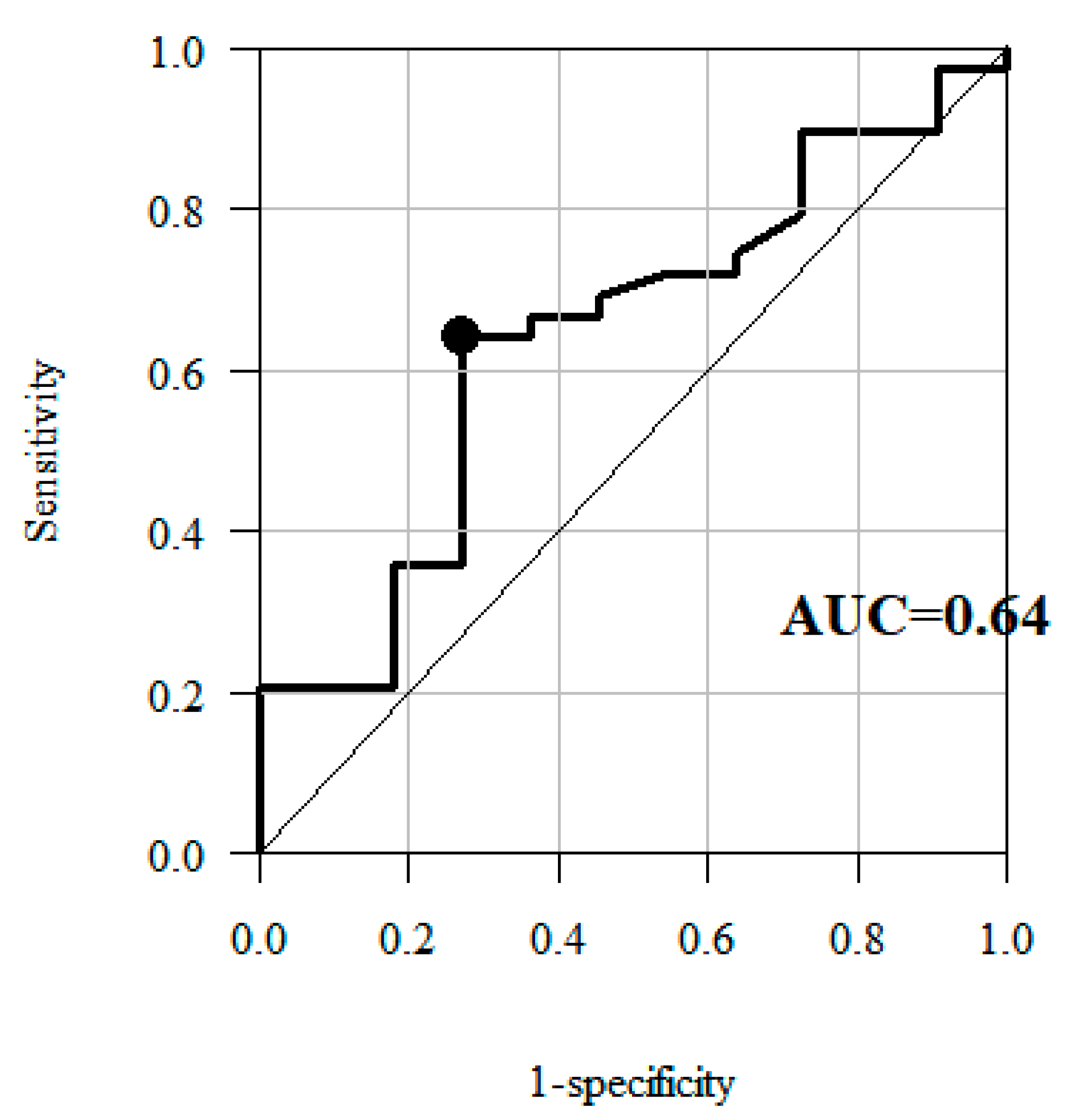
| Receiver operating characteristic Curve | 3.8 | --- | --- |
| Knee Flexion/Extension ROM (before Rehabilitation) | Age Groups (Years) | p | |||||
| Up to 50 | Over 50 | ||||||
| Mean | 95% CI | SD | Mean | 95% CI | SD | ||
| Knee flexion/extension ROM affected side (deg.) | 37.66 | 25.28–50.03 | 13.38 | 34.13 | 31.29–36.97 | 9.21 | 0.7353 |
| Knee flexion/extension ROM unaffected side (deg.) | 45.16 | 36.8–53.52 | 9.04 | 41.9 | 39.22–44.58 | 8.71 | 0.1762 |
| Knee Flexion/Extension ROM (Effects of Rehabilitation) | Age Groups (Years) | p | |||||
| Up to 50 | Over 50 | ||||||
| Mean | 95% CI | SD | Mean | 95% CI | SD | ||
| Knee flexion/extension ROM affected side (deg.) | 4.56 | 0.15–9.26 | 5.09 | 7.35 | 5.58–9.12 | 5.75 | 0.2367 |
| Knee flexion/extension ROM unaffected side (deg.) | 5.01 | 3.9–13.12 | 8.76 | 6.32 | 4.33–8.30 | 6.44 | 0.3980 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guzik, A.; Drużbicki, M.; Wolan-Nieroda, A.; Turolla, A.; Kiper, P. Estimating Minimal Clinically Important Differences for Knee Range of Motion after Stroke. J. Clin. Med. 2020, 9, 3305. https://doi.org/10.3390/jcm9103305
Guzik A, Drużbicki M, Wolan-Nieroda A, Turolla A, Kiper P. Estimating Minimal Clinically Important Differences for Knee Range of Motion after Stroke. Journal of Clinical Medicine. 2020; 9(10):3305. https://doi.org/10.3390/jcm9103305
Chicago/Turabian StyleGuzik, Agnieszka, Mariusz Drużbicki, Andżelina Wolan-Nieroda, Andrea Turolla, and Pawel Kiper. 2020. "Estimating Minimal Clinically Important Differences for Knee Range of Motion after Stroke" Journal of Clinical Medicine 9, no. 10: 3305. https://doi.org/10.3390/jcm9103305
APA StyleGuzik, A., Drużbicki, M., Wolan-Nieroda, A., Turolla, A., & Kiper, P. (2020). Estimating Minimal Clinically Important Differences for Knee Range of Motion after Stroke. Journal of Clinical Medicine, 9(10), 3305. https://doi.org/10.3390/jcm9103305







