Association of Neutrophil, Platelet, and Lymphocyte Ratios with the Prognosis in Unresectable and Metastatic Pancreatic Cancer
Abstract
1. Introduction
2. Experimental Section
3. Results
3.1. Characteristics of Patients
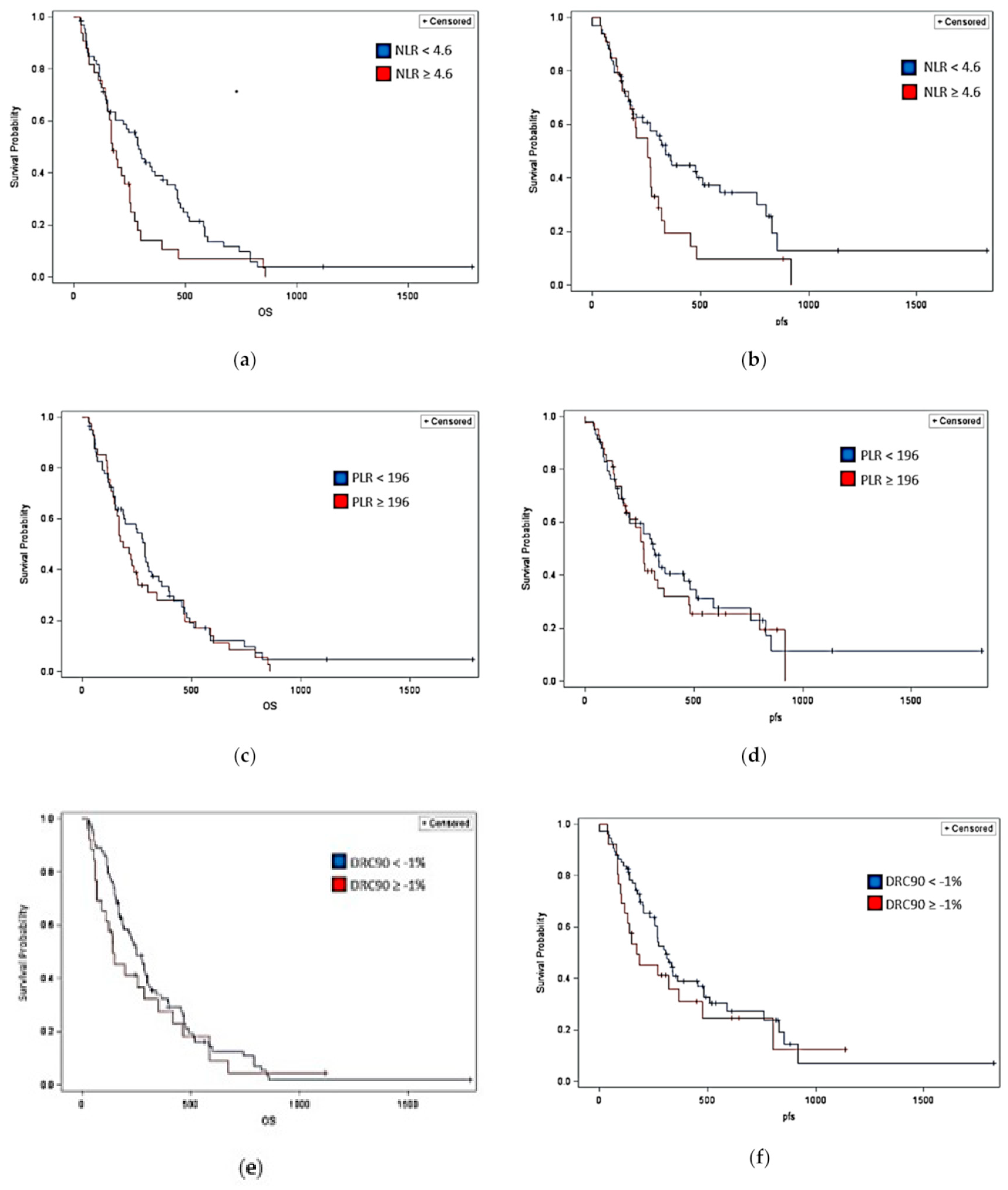
3.2. Efficacy
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Survival Rates for Pancreatic Cancer. Available online: https://www.cancer.org/cancer/pancreatic-cancer/detection-diagnosis-staging/survival-rates.html#references (accessed on 20 June 2020).
- Final Recommendation Statement: Pancreatic Cancer: Screening: United States Preventive Services Taskforce. Available online: https://www.uspreventiveservicestaskforce.org/uspstf/document/RecommendationStatementFinal/pancreatic-cancer-screening#:~:text=The%20American%20College%20of%20Gastroenterology,degree%20relative)%20and%20suggests%20that (accessed on 20 June 2020).
- Friess, H.; Demir, I.E. Pancreatic cancer—Lessons from the past decade. Indian J. Med. Paediatr. Oncol. 2015, 36, 73–76. [Google Scholar] [CrossRef] [PubMed]
- Das, A.; McNulty, M.; Higgs, D.; Rogers-Seeley, M.; Fennessy, S.; McGarvey, C.; Dean, A. Correlation of neutrophil -lymphocyte ratio, platelet -lymphocyte ratio and rate of change of CA 19-9 in predicting outcome for metastatic pancreatic cancer. In Proceedings of the World Congress on Gastrointestinal Cancer, Barcelona, Spain, 20–23 June 2019. [Google Scholar]
- DeDe, I.; Cetin, M.; Cetin, S. Prognostic value of the neutrophil-lymphocyte ratio and CA 19-9 in predicting survival in patients with metastatic pancreatic cancer. Ann. Oncol. 2018, 29, viii256. [Google Scholar] [CrossRef]
- Desai, J.R.; Colton, B.S.; Wang, H.; Marshall, J.; Kim, S.; Pishvaian, M.J. Neutrophil-to-lymphocyte ratio as a prognostic marker for metastatic pancreatic cancer. J. Clin. Oncol. 2018, 36, 251. [Google Scholar] [CrossRef]
- Mei, Z.; Shi, L.; Wang, B.; Yang, J.; Xiao, Z.; Du, P.; Wang, Q.; Yang, W. Prognostic role of pretreatment blood neutrophil-to-lymphocyte ratio in advanced cancer survivors: A systematic review and meta-analysis of 66 cohort studies. Cancer Treat. Rev. 2017, 58, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Hao, S.; Andersen, M.; Yu, H. Detection of immune suppressive neutrophils in peripheral blood samples of cancer patients. Am. J. Blood Res. 2013, 3, 239–245. [Google Scholar] [PubMed]
- Pillay, J.; Kamp, V.M.; Van Hoffen, E.; Visser, T.; Tak, T.; Lammers, J.-W.; Ulfman, L.H.; Leenen, L.P.; Pickkers, P.; Koenderman, L. A subset of neutrophils in human systemic inflammation inhibits T cell responses through Mac-1. J. Clin. Investig. 2012, 122, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Sohal, D.P.S.; Kennedy, E.B.; Khorana, A.; Copur, M.S.; Crane, C.H.; Garrido-Laguna, I.; Krishnamurthi, S.; Moravek, C.; O’Reilly, E.M.; Philip, P.A.; et al. Metastatic pancreatic cancer: ASCO clinical practice guideline update. J. Clin. Oncol. 2018, 36, 2545–2556. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | NLR < 4.6 K/µL | NLR ≥ 4.6 K/µL | PLR < 196 K/µL | PLR ≥ 196 K/µL | DRC90 < −1% | DRC90 ≥ −1% |
|---|---|---|---|---|---|---|
| Number | 66 | 35 | 59 | 43 | 66 | 36 |
| Age (median) | 65.5 | 62 | 63 | 64 | 64 | 61.5 |
| Gender (%) | ||||||
| Male | 62.0% | 60.0% | 61.0% | 62.8% | 60.6% | 63.9% |
| Female | 38.0% | 40.0% | 39.0% | 37.20% | 39.4% | 36.1% |
| Race | ||||||
| White | 57 (86.4%) | 32 (91.4%) | 53 (89.8%) | 36 (83.7%) | 60 (90.9%) | 29 (80.6%) |
| Black or African American | 2 (3.0%) | 2 (5.7%) | 2 (3.4%) | 2 (4.7%) | 0 (0.0%) | 4 (11.1%) |
| Other | 5 (7.6%) | 1 (2.9%) | 4 (6.8%) | 5 (11.6%) | 6 (9.1%) | 3 (8.3%) |
| Smoking Status | ||||||
| Yes | 27 (40.9%) | 17 (48.6%) | 30 (50.8%) | 14 (32.6%) | 40 (60.6%) | 19 (52.8%) |
| No | 37 (56.1%) | 17 (48.6%) | 27 (45.8%) | 28 (65.1%) | 25 (37.9) | 15 (41.7%) |
| ECOG Status | ||||||
| 0–1 | 60 (90.1%) | 33 (94.3%) | 54 (91.5%) | 39 (90.7%) | 60 (90.9%) | 33 (91.7%) |
| 2 or higher | 6 (9.1%) | 2 (5.7%) | 5 (8.5%) | 4 (9.3%) | 5 (7.6%) | 2 (5.6%) |
| Tumor Location | ||||||
| Head | 49 (74.2%) | 15 (42.3%) | 40 (67.8%) | 24 (55.8%) | 42 (63.6%) | 22 (61.1%) |
| Tail | 9 (13.6%) | 11 (31.4%) | 10 (16.9%) | 6 (14.0%) | 16 (24.3%) | 5 (13.9%) |
| Body | 7 (10.6%) | 9 (25.7%) | 8 (13.6%) | 13 (30.2%) | 7 (10.6%) | 9 (25.0%) |
| Neck | 1 (1.5%) | 0 (0.0%) | 1 (1.7%) | 0 (0.0%) | 1 (1.5%) | 0 (0.0%) |
| Metastatic | 46 (69.7%) | 33 (94.3%) | 46 (78.0%) | 34 (79.0%) | 54 (81.8%) | 33 (91.7%) |
| Locally Advanced | 20 (30.3%) | 2 (5.7%) | 13 (22.0%) | 9 (21.0%) | 12 (18.2%) | 3 (8.3%) |
| CA19-9 at the time of diagnosis | ||||||
| Normal (<38 U/mL) | 11 (16.7%) | 3 (8.6%) | 8 (13.6%) | 5 (11.6%) | 5 (7.6%) | 8 (22.2%) |
| Abnormal (>38 U/mL) | 54 (81.8%) | 32 (91.4%) | 51 (86.4%) | 38 (88.4%) | 61 (92.4%) | 26 (72.2%) |
| Treatment Received | ||||||
| FOLFIRINOX | 40 (60.6%) | 20 (57.1%) | 37 (62.7%) | 24 (55.8%) | 40 (60.6%) | 21 (58.3%) |
| Gemcitabine/albumin-bound Paclitaxel (Abraxane) | 16 (24.2%) | 11 (31.4%) | 13 (22.0%) | 14 (32.6%) | 18 (27.3%) | 10 (27.8%) |
| Gemcitabine | 4 (6.1%) | 0 (0.0%) | 4 (6.8%) | 0 (0.0%) | 2 (3.0%) | 2 (5.6%) |
| Other | 6 (9.1%) | 4 (11.4%) | 5 (8.5%) | 5 (11.6%) | 6 (9.1%) | 3 (8.3%) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Allen, J.; Cernik, C.; Bajwa, S.; Al-Rajabi, R.; Saeed, A.; Baranda, J.; Williamson, S.; Sun, W.; Kasi, A. Association of Neutrophil, Platelet, and Lymphocyte Ratios with the Prognosis in Unresectable and Metastatic Pancreatic Cancer. J. Clin. Med. 2020, 9, 3283. https://doi.org/10.3390/jcm9103283
Allen J, Cernik C, Bajwa S, Al-Rajabi R, Saeed A, Baranda J, Williamson S, Sun W, Kasi A. Association of Neutrophil, Platelet, and Lymphocyte Ratios with the Prognosis in Unresectable and Metastatic Pancreatic Cancer. Journal of Clinical Medicine. 2020; 9(10):3283. https://doi.org/10.3390/jcm9103283
Chicago/Turabian StyleAllen, Jessica, Colin Cernik, Suhaib Bajwa, Raed Al-Rajabi, Anwaar Saeed, Joaquina Baranda, Stephen Williamson, Weijing Sun, and Anup Kasi. 2020. "Association of Neutrophil, Platelet, and Lymphocyte Ratios with the Prognosis in Unresectable and Metastatic Pancreatic Cancer" Journal of Clinical Medicine 9, no. 10: 3283. https://doi.org/10.3390/jcm9103283
APA StyleAllen, J., Cernik, C., Bajwa, S., Al-Rajabi, R., Saeed, A., Baranda, J., Williamson, S., Sun, W., & Kasi, A. (2020). Association of Neutrophil, Platelet, and Lymphocyte Ratios with the Prognosis in Unresectable and Metastatic Pancreatic Cancer. Journal of Clinical Medicine, 9(10), 3283. https://doi.org/10.3390/jcm9103283





