Rationale and Design of the Future Optimal Research and Care Evaluation in Patients with Acute Coronary Syndrome (FORCE-ACS) Registry: Towards “Personalized Medicine” in Daily Clinical Practice
Abstract
1. Introduction
2. Methods
2.1. Study Objectives
2.2. Study Design and Population
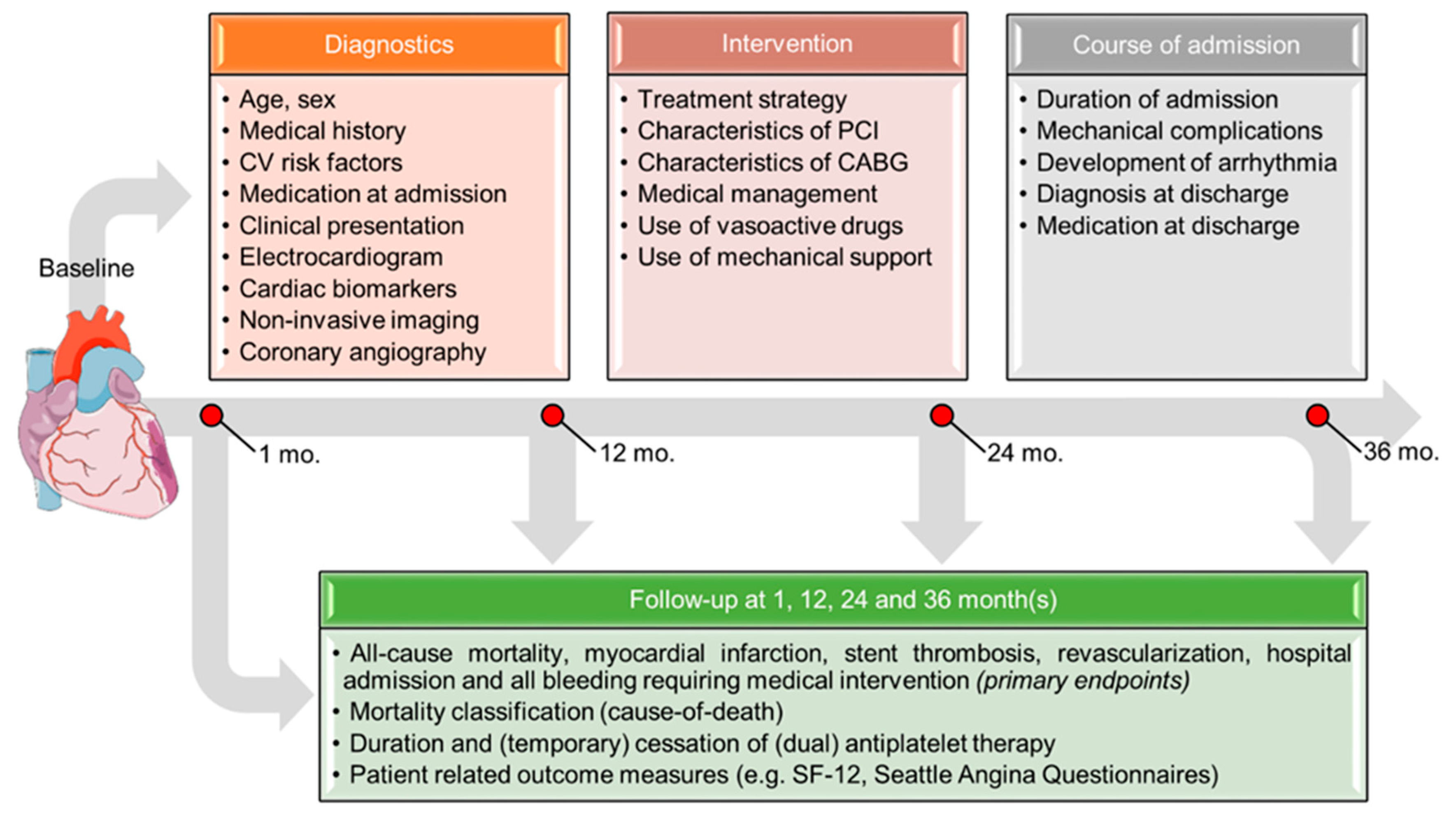
2.3. Data Collection
2.4. Study End Points
2.5. Sample Size and Statistical Analysis
2.6. Quality Control
2.7. Regulation Statement and Informed Consent
2.8. The FORCE-ACS Database Framework
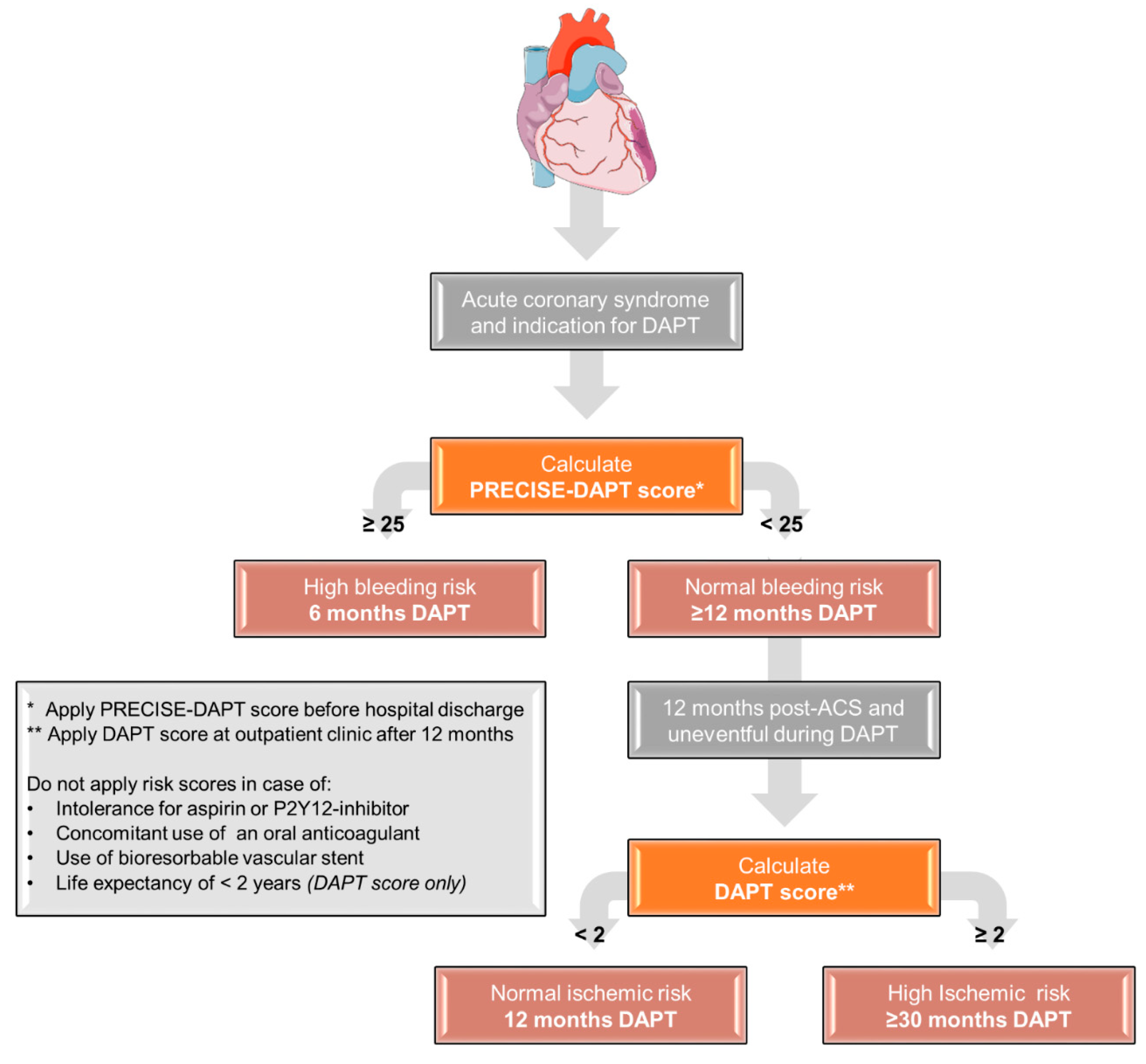
- Standard treatment group: DAPT duration not based on risk scores
- Risk score-guided group: DAPT duration based on risk scores using the following treatment scheme (see Figure 3)
3. Discussion
Future Perspective
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Szummer, K.; Wallentin, L.; Lindhagen, L.; Alfredsson, J.; Erlinge, D.; Held, C.; James, S.; Kellerth, T.; Lindahl, B.; Ravn-Fischer, A.; et al. Improved outcomes in patients with ST-elevation myocardial infarction during the last 20 years are related to implementation of evidence-based treatments: Experiences from the SWEDEHEART registry 1995–2014. Eur. Heart J. 2017, 38, 3056–3065. [Google Scholar] [CrossRef] [PubMed]
- Szummer, K.; Wallentin, L.; Lindhagen, L.; Alfredsson, J.; Erlinge, D.; Held, C.; James, S.; Kellerth, T.; Lindahl, B.; Ravn-Fischer, A.; et al. Relations between implementation of new treatments and improved outcomes in patients with non-ST-elevation myocardial infarction during the last 20 years: Experiences from SWEDEHEART registry 1995 to 2014. Eur. Heart J. 2018, 39, 3766–3776. [Google Scholar] [CrossRef]
- Fox, K.A.A.; Carruthers, K.F.; Dunbar, D.R.; Graham, C.; Manning, J.R.; De Raedt, H.; Buysschaert, I.; Lambrechts, D.; Van De Werf, F. Underestimated and under-recognized: The late consequences of acute coronary syndrome (GRACE UK-Belgian Study). Eur. Heart J. 2010, 31, 2755–2764. [Google Scholar] [CrossRef] [PubMed]
- Jernberg, T.; Hasvold, P.; Henriksson, M.; Hjelm, H.; Thuresson, M.; Janzon, M. Cardiovascular risk in post-myocardial infarction patients: Nationwide real world data demonstrate the importance of a long-term perspective. Eur. Heart J. 2015, 36, 1163–1170. [Google Scholar] [CrossRef] [PubMed]
- Simonsson, M.; Wallentin, L.; Alfredsson, J.; Erlinge, D.; Hellstrom Angerud, K.; Hofmann, R.; Kellerth, T.; Lindhagen, L.; Ravn-Fischer, A.; Szummer, K.; et al. Temporal trends in bleeding events in acute myocardial infarction: Insights from the SWEDEHEART registry. Eur. Heart J. 2020, 41, 833–843. [Google Scholar] [CrossRef]
- Valgimigli, M.; Bueno, H.; Byrne, R.A.; Collet, J.-P.; Costa, F.; Jeppsson, A.; Juni, P.; Kastrati, A.; Kolh, P.; Mauri, L.; et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2018, 39, 213–260. [Google Scholar] [CrossRef]
- Costa, F.; van Klaveren, D.; James, S.; Heg, D.; Räber, L.; Feres, F.; Pilgrim, T.; Hong, M.K.; Kim, H.S.; Colombo, A.; et al. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: A pooled analysis of individual-patient datasets from clinical trials. Lancet 2017, 389, 1025–1034. [Google Scholar] [CrossRef]
- Yeh, R.W.; Secemsky, E.A.; Kereiakes, D.J.; Normand, S.L.T.; Gershlick, A.H.; Cohen, D.J.; Spertus, J.A.; Steg, P.G.; Cutlip, D.E.; Rinaldi, M.J.; et al. Development and validation of a prediction rule for benefit and harm of dual antiplatelet therapy beyond 1 year after percutaneous coronary intervention. JAMA 2016, 315, 1735–1749. [Google Scholar] [CrossRef]
- Alexander, K.P.; Newby, L.K.; Cannon, C.P.; Armstrong, P.W.; Gibler, W.B.; Rich, M.W.; Van de Werf, F.; White, H.D.; Weaver, W.D.; Naylor, M.D.; et al. Acute coronary care in the elderly, part I: Non-ST-segment-elevation acute coronary syndromes: A scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: In collaboration with the Society of Geriatric Cardiology. Circulation 2007, 115, 2549–2569. [Google Scholar] [CrossRef]
- GRACE Investigators. Rationale and design of the GRACE (Global Registry of Acute Coronary Events) Project: A multinational registry of patients hospitalized with acute coronary syndromes. Am. Heart J. 2001, 141, 190–199. [Google Scholar] [CrossRef]
- Aliprandi-Costa, B.; Ranasinghe, I.; Turnbull, F.; Brown, A.; Kritharides, L.; Patel, A.; Chew, D.; Walters, D.; Rankin, J.; Ilton, M.; et al. The design and rationale of the Australian Cooperative National Registry of Acute Coronary care, Guideline Adherence and Clinical Events (CONCORDANCE). Heart. Lung Circ. 2013, 22, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Hao, Y.; Liu, J.; Liu, J.; Smith, S.C.J.; Huo, Y.; Fonarow, G.C.; Ma, C.; Ge, J.; Taubert, K.A.; Morgan, L.; et al. Rationale and design of the Improving Care for Cardiovascular Disease in China (CCC) project: A national effort to prompt quality enhancement for acute coronary syndrome. Am. Heart J. 2016, 179, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Alegre, O.; Ariza-Sole, A.; Vidan, M.T.; Formiga, F.; Martinez-Selles, M.; Bueno, H.; Sanchis, J.; Lopez-Palop, R.; Abu-Assi, E.; Cequier, A. Impact of frailty and other geriatric syndromes on clinical management and outcomes in elderly patients with non-ST-segment elevation Acute Coronary Syndromes: Rationale and design of the LONGEVO-SCA registry. Clin. Cardiol. 2016, 39, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Fokkema, M.L.; James, S.K.; Albertsson, P.; Aasa, M.; Akerblom, A.; Calais, F.; Eriksson, P.; Jensen, J.; Schersten, F.; de Smet, B.J.; et al. Outcome after percutaneous coronary intervention for different indications: Long-term results from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR). EuroIntervention 2016, 12, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Roffi, M.; Patrono, C.; Collet, J.P.; Mueller, C.; Valgimigli, M.; Andreotti, F.; Bax, J.J.; Borger, M.A.; Brotons, C.; Chew, D.P.; et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent st-segment elevation: Task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2016, 37, 267–315. [Google Scholar] [CrossRef]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society. Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef]
- Neumann, F.-J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.-P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Ware, J.J.; Kosinski, M.; Keller, S.D. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef]
- Spertus, J.A.; Winder, J.A.; Dewhurst, T.A.; Deyo, R.A.; Prodzinski, J.; McDonell, M.; Fihn, S.D. Development and evaluation of the Seattle Angina Questionnaire: A new functional status measure for coronary artery disease. J. Am. Coll. Cardiol. 1995, 25, 333–341. [Google Scholar] [CrossRef]
- Mehran, R.; Rao, S.V.; Bhatt, D.L.; Gibson, C.M.; Caixeta, A.; Eikelboom, J.; Kaul, S.; Wiviott, S.D.; Menon, V.; Nikolsky, E.; et al. Standardized bleeding definitions for cardiovascular clinical trials: A consensus report from the bleeding academic research consortium. Circulation 2011, 123, 2736–2747. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Garcia, H.M.; McFadden, E.P.; Farb, A.; Mehran, R.; Stone, G.W.; Spertus, J.; Onuma, Y.; Morel, M.-A.; van Es, G.-A.; Zuckerman, B.; et al. Standardized end point definitions for coronary intervention trials: The Academic Research Consortium-2 consensus document. Circulation 2018, 137, 2635–2650. [Google Scholar] [CrossRef] [PubMed]
- Taqueti, V.R. Sex differences in the coronary system. Adv. Exp. Med. Biol. 2018, 1065, 257–278. [Google Scholar] [CrossRef] [PubMed]
- Tra, J.; van der Wulp, I.; Appelman, Y.; de Bruijne, M.C.; Wagner, C. Adherence to guidelines for the prescription of secondary prevention medication at hospital discharge after acute coronary syndrome: A multicentre study. Neth. Heart J. 2015, 23, 214–221. [Google Scholar] [CrossRef]

| Hospital (Location) | Hospital Type | Start Inclusion |
|---|---|---|
| Coordinating study sites | ||
| 1. St. Antonius Hospital (Nieuwegein, the Netherlands) | Interventional cardiac center | 2015 |
| 2. Amsterdam UMC, location AMC (Amsterdam, the Netherlands) | Interventional cardiac center | 2019 |
| 3. Hospital Gelderse Vallei (Ede, the Netherlands) | Non-interventional cardiac center | 2018 |
| 4. Rijnstate Hospital (Arnhem, the Netherlands) | Interventional cardiac center | 2019 |
| 5. Gelre Hospitals (Apeldoorn, the Netherlands) | Non-interventional cardiac center | 2018 |
| 6. Rivierenland Hospital (Tiel, the Netherlands) | Non-interventional cardiac center | 2018 |
| 7. Amsterdam UMC, location VUmc (Amsterdam, the Netherlands) | Interventional cardiac center | 2020 |
| 8. Tergooi Hospital (Hilversum, the Netherlands) | Interventional cardiac center | 2020 |
| 9. University Medical Center Utrecht (Utrecht, the Netherlands) | Interventional cardiac center | 2020 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chan Pin Yin, D.R.P.P.; Vos, G.-J.A.; van der Sangen, N.M.R.; Walhout, R.; Tjon Joe Gin, R.M.; Nicastia, D.M.; Langerveld, J.; Claassens, D.M.F.; Gimbel, M.E.; Azzahhafi, J.; et al. Rationale and Design of the Future Optimal Research and Care Evaluation in Patients with Acute Coronary Syndrome (FORCE-ACS) Registry: Towards “Personalized Medicine” in Daily Clinical Practice. J. Clin. Med. 2020, 9, 3173. https://doi.org/10.3390/jcm9103173
Chan Pin Yin DRPP, Vos G-JA, van der Sangen NMR, Walhout R, Tjon Joe Gin RM, Nicastia DM, Langerveld J, Claassens DMF, Gimbel ME, Azzahhafi J, et al. Rationale and Design of the Future Optimal Research and Care Evaluation in Patients with Acute Coronary Syndrome (FORCE-ACS) Registry: Towards “Personalized Medicine” in Daily Clinical Practice. Journal of Clinical Medicine. 2020; 9(10):3173. https://doi.org/10.3390/jcm9103173
Chicago/Turabian StyleChan Pin Yin, Dean R. P. P., Gert-Jan A. Vos, Niels M. R. van der Sangen, Ronald Walhout, R. Melvyn Tjon Joe Gin, Deborah M. Nicastia, Jorina Langerveld, Daniël M. F. Claassens, Marieke E. Gimbel, Jaouad Azzahhafi, and et al. 2020. "Rationale and Design of the Future Optimal Research and Care Evaluation in Patients with Acute Coronary Syndrome (FORCE-ACS) Registry: Towards “Personalized Medicine” in Daily Clinical Practice" Journal of Clinical Medicine 9, no. 10: 3173. https://doi.org/10.3390/jcm9103173
APA StyleChan Pin Yin, D. R. P. P., Vos, G.-J. A., van der Sangen, N. M. R., Walhout, R., Tjon Joe Gin, R. M., Nicastia, D. M., Langerveld, J., Claassens, D. M. F., Gimbel, M. E., Azzahhafi, J., Bor, W. L., Oirbans, T., Dekker, J., Vlachojannis, G. J., van Bommel, R. J., Appelman, Y., Henriques, J. P. S., Kikkert, W. J., & ten Berg, J. M. (2020). Rationale and Design of the Future Optimal Research and Care Evaluation in Patients with Acute Coronary Syndrome (FORCE-ACS) Registry: Towards “Personalized Medicine” in Daily Clinical Practice. Journal of Clinical Medicine, 9(10), 3173. https://doi.org/10.3390/jcm9103173






